Investigating the Prognostic Role of Peripheral Inflammatory Markers in Mild Cognitive Impairment
Abstract
:1. Introduction
2. Materials and Methods
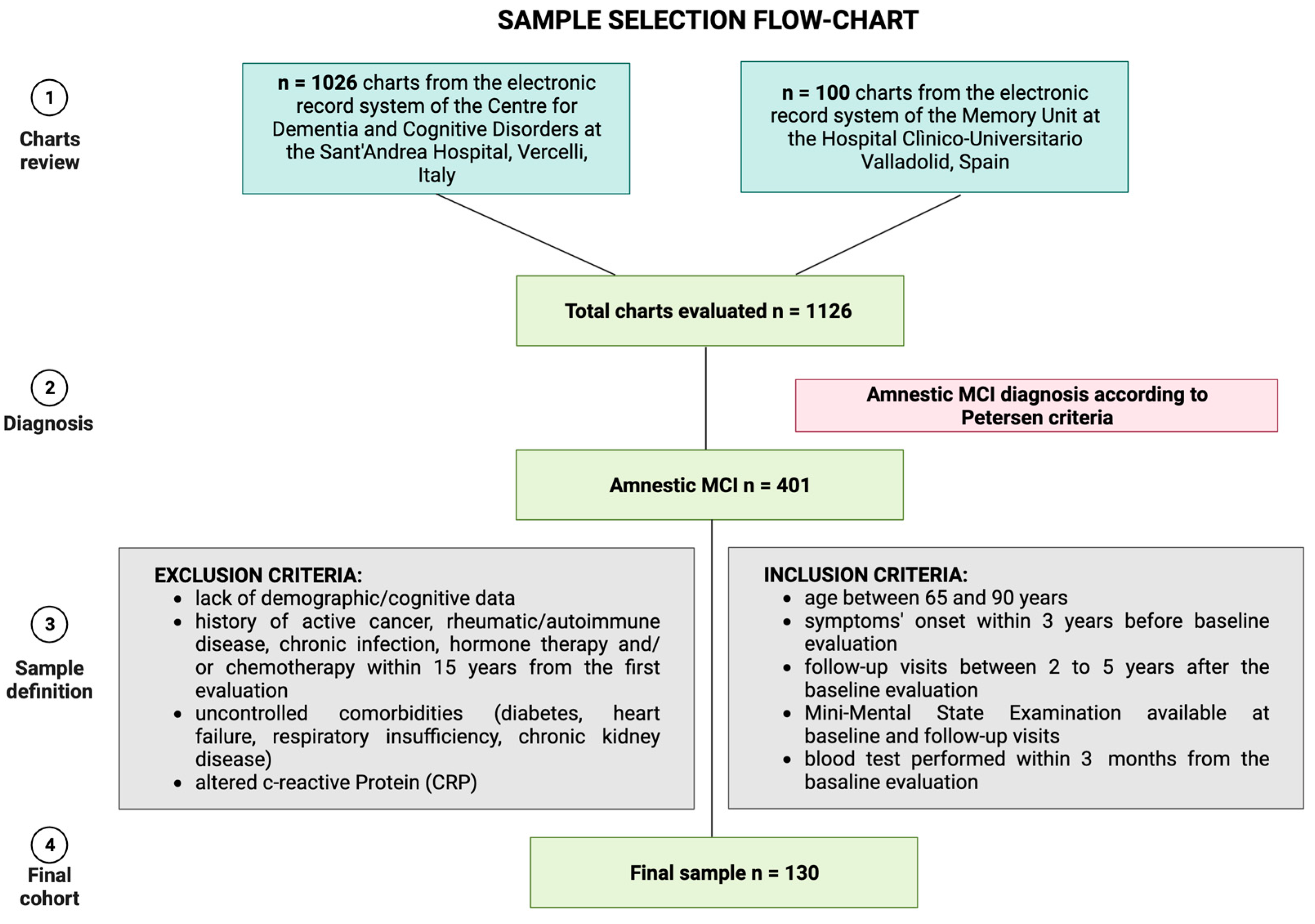
2.1. Sample Selection
- amnestic MCI diagnosis according to Petersen criteria [4],
- age between 65 and 90 years,
- symptoms’ onset within three years before the first evaluation (baseline),
- at least one available follow-up visit between two and five years after the baseline evaluation,
- Mini-mental state examination (MMSE) is available both at baseline and follow-up visits,
- a blood test performed within three months from the baseline evaluation.
- 7.
- lack of fundamental demographic data (age, educational level) or cognitive assessment at baseline or follow-up,
- 8.
- history of active cancer, rheumatic disease, autoimmune disease, chronic infection, hormone therapy, and/or chemotherapy within 15 years from the first evaluation,
- 9.
- uncontrolled comorbidities (diabetes, heart failure, respiratory insufficiency, chronic kidney disease),
- 10.
- altered C-Reactive Protein (CRP).
2.2. Hematological Data
2.3. Clinical and Cognitive Baseline-to-Follow-Up Assessment
2.4. Statistical Analysis
3. Results
3.1. Study Sample and Clinical-Hematological Correlations
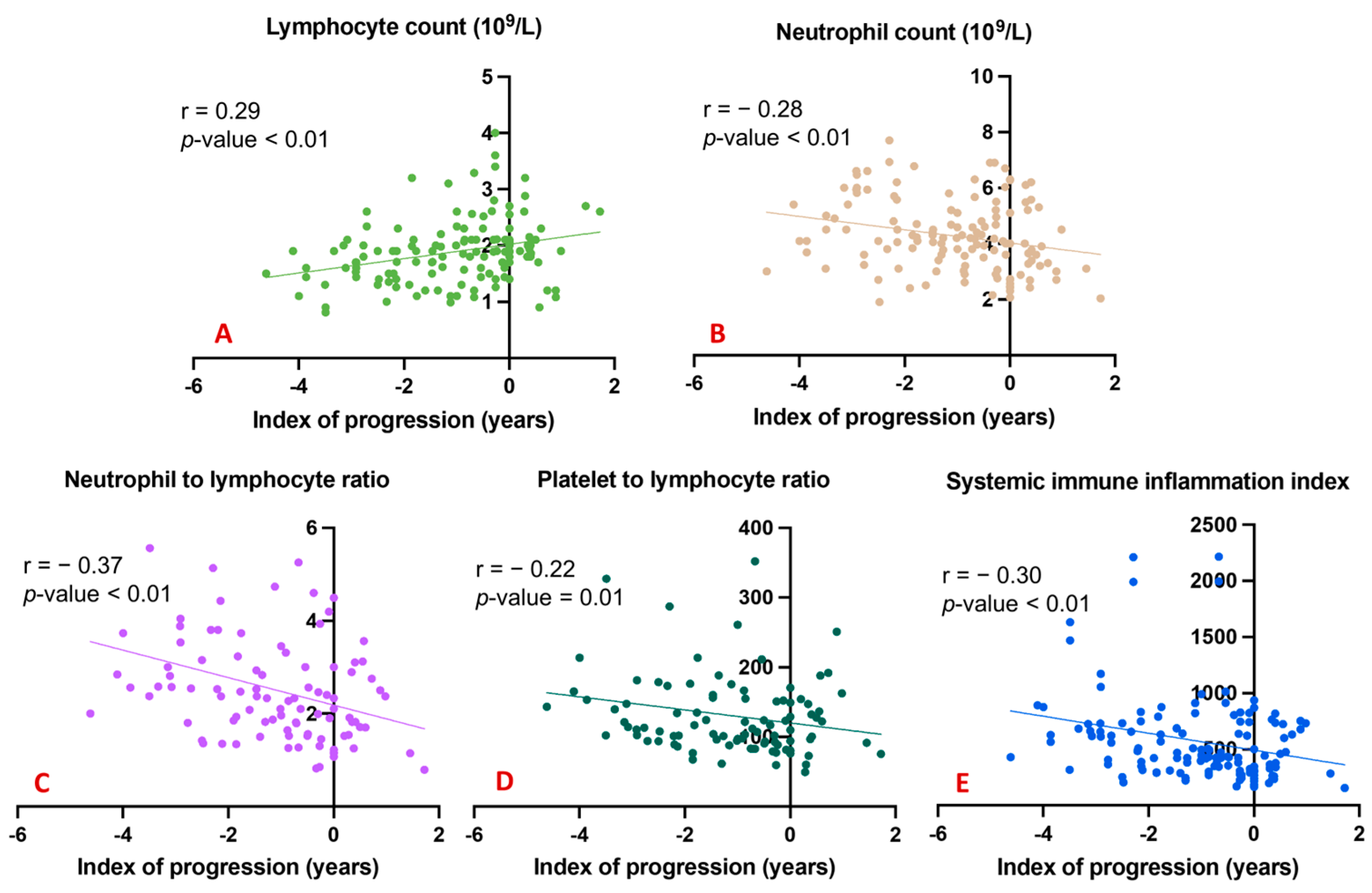
3.2. Cognitive Decline Progression: Correlation Analysis
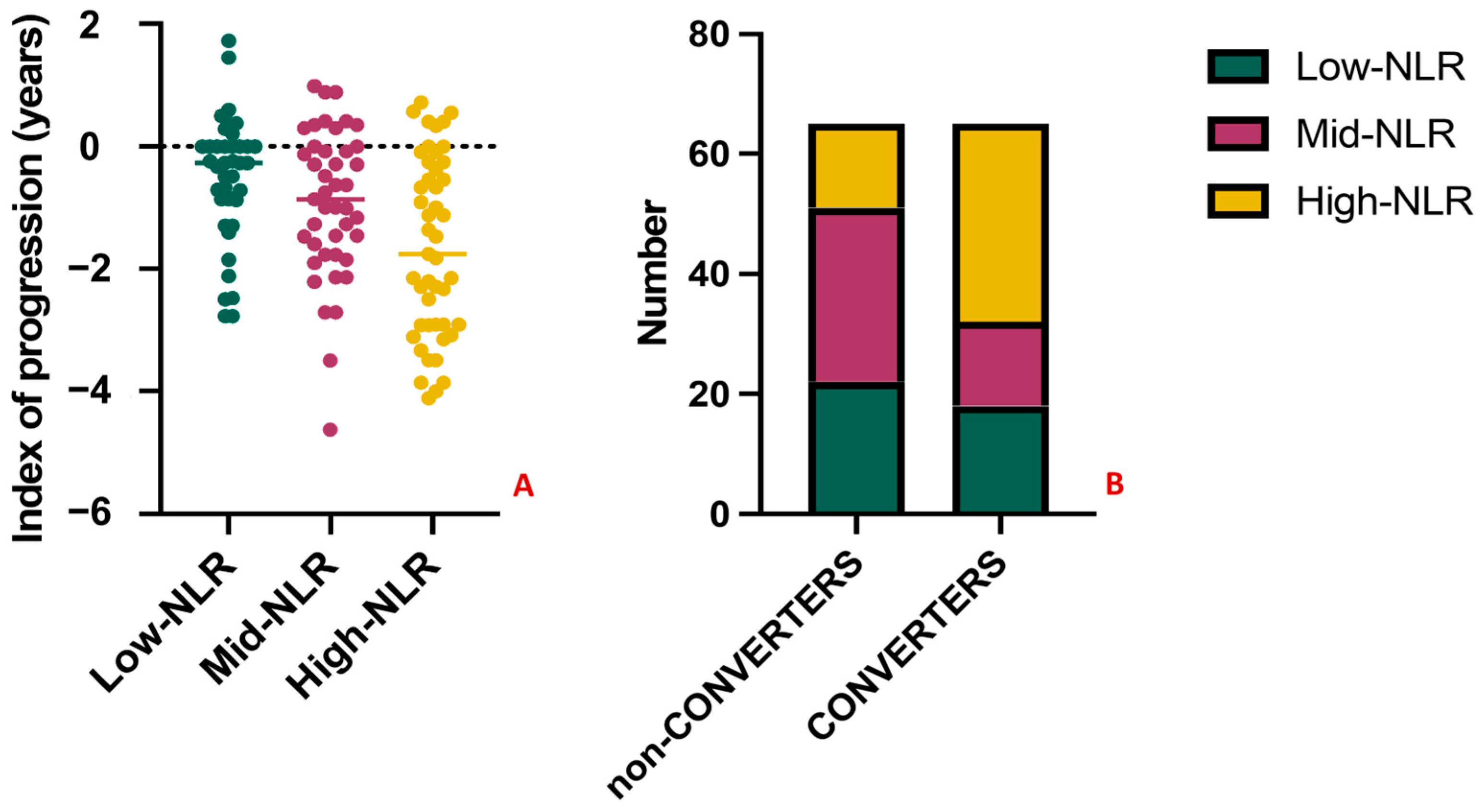
3.3. Conversion to Dementia: Comparison between Groups
3.4. Factors Predicting Conversion to Dementia
3.5. Tertiles Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nichols, E.; Steinmetz, J.D.; Vollset, S.E.; Fukutaki, K.; Chalek, J.; Abd-Allah, F.; Abdoli, A.; Abualhasan, A.; Abu-Gharbieh, E.; Akram, T.T.; et al. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: An analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2022, 7, e105–e125. [Google Scholar] [CrossRef]
- Frankish, H.; Horton, R. Prevention and management of dementia: A priority for public health. Lancet 2017, 390, 2614–2615. [Google Scholar] [CrossRef]
- Rana, J.S.; Khan, S.S.; Lloyd-Jones, D.M.; Sidney, S. Changes in mortality in top 10 causes of death from 2011 to 2018. J. Gen. Intern. Med. 2021, 36, 2517–2518. [Google Scholar] [CrossRef]
- Petersen, R.C.; Caracciolo, B.; Brayne, C.; Gauthier, S.; Jelic, V.; Fratiglioni, L. Mild cognitive impairment: A concept in evolution. J. Intern. Med. 2014, 275, 214–228. [Google Scholar] [CrossRef]
- Petersen, R.C. Mild Cognitive Impairment. Continuum 2016, 22, 404–418. [Google Scholar]
- Gjøra, L.; Strand, B.H.; Bergh, S.; Borza, T.; Brækhus, A.; Engedal, K.; Johannessen, A.; Kvello-Alme, M.; Krokstad, S.; Livingston, G.; et al. Current and Future Prevalence Estimates of Mild Cognitive Impairment, Dementia, and Its Subtypes in a Population-Based Sample of People 70 Years and Older in Norway: The HUNT Study. J. Alzheimer’s Dis. 2021, 79, 1213–1226. [Google Scholar] [CrossRef]
- Petersen, R.C.; Lopez, O.; Armstrong, M.J.; Getchius, T.S.D.; Ganguli, M.; Gloss, D.; Gronseth, G.S.; Marson, D.; Pringsheim, T.; Day, G.S.; et al. Practice guideline update summary: Mild cognitive impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology 2018, 90, 126–135. [Google Scholar] [CrossRef]
- Thomas, K.R.; Edmonds, E.C.; Eppig, J.S.; Wong, C.G.; Weigand, A.J.; Bangen, K.J.; Jak, A.J.; Delano-Wood, L.; Galasko, D.R.; Salmon, D.P.; et al. MCI-to-normal reversion using neuropsychological criteria in the Alzheimer’s Disease Neuroimaging Initiative. Alzheimer’s Dement. 2019, 15, 1322–1332. [Google Scholar] [CrossRef]
- Tondo, G.; Carli, G.; Santangelo, R.; Mattoli, M.V.; Presotto, L.; Filippi, M.; Magnani, G.; Iannaccone, S.; Cerami, C.; Perani, D.; et al. Biomarker-based stability in limbic-predominant amnestic mild cognitive impairment. Eur. J. Neurol. 2021, 28, 1123–1133. [Google Scholar] [CrossRef]
- Chitnis, T.; Weiner, H.L. CNS inflammation and neurodegeneration. J. Clin. Investig. 2017, 127, 3577–3587. [Google Scholar] [CrossRef]
- González-Hernández, S.; Mukouyama, Y.-S. Lymphatic vasculature in the central nervous system. Front. Cell Dev. Biol. 2023, 11, 1150775. [Google Scholar] [CrossRef]
- Comi, C.; Tondo, G. Insights into the protective role of immunity in neurodegenerative disease. Neural Regen Res. 2017, 12, 64. [Google Scholar] [CrossRef] [PubMed]
- Tondo, G.; Iaccarino, L.; Caminiti, S.P.; Presotto, L.; Santangelo, R.; Iannaccone, S.; Magnani, G.; Perani, D. The combined effects of microglia activation and brain glucose hypometabolism in early-onset Alzheimer’s disease. Alzheimer’s Res. Ther. 2020, 12, 50. [Google Scholar] [CrossRef] [PubMed]
- Kreisl, W.C.; Henter, I.D.; Innis, R.B. Imaging Translocator Protein as a Biomarker of Neuroinflammation in Dementia. Adv. Pharmacol. 2018, 82, 163–185. [Google Scholar]
- Bradburn, S.; Murgatroyd, C.; Ray, N. Neuroinflammation in mild cognitive impairment and Alzheimer’s disease: A meta-analysis. Ageing Res Rev. 2019, 50, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Tondo, G.; Boccalini, C.; Caminiti, S.P.; Presotto, L.; Filippi, M.; Magnani, G.; Frisoni, G.B.; Iannaccone, S.; Perani, D. Brain metabolism and microglia activation in mild cognitive impairment: A combined [18F] FDG and [11C]-(R)-PK11195 PET study. J. Alzheimer’s Dis. 2021, 80, 433–445. [Google Scholar] [CrossRef]
- Sayed, A.; Bahbah, E.I.; Kamel, S.; Barreto, G.E.; Ashraf, G.M.; Elfil, M. The neutrophil-to-lymphocyte ratio in Alzheimer’s disease: Current understanding and potential applications. J. Neuroimmunol. 2020, 349, 577398. [Google Scholar] [CrossRef] [PubMed]
- Kara, S.P.; Altunan, B.; Unal, A. Investigation of the peripheral inflammation (neutrophil-lymphocyte ratio) in two neurodegenerative diseases of the central nervous system. Neurol. Sci. 2022, 43, 1799–1807. [Google Scholar] [CrossRef]
- Zhang, L.; Cao, B.; Hou, Y.; Wei, Q.; Ou, R.; Zhao, B.; Shang, H. High neutrophil-to-lymphocyte ratio predicts short survival in multiple system atrophy. NPJ Park Dis. 2022, 8, 11. [Google Scholar] [CrossRef]
- Choi, S.-J.; Hong, Y.-H.; Kim, S.-M.; Shin, J.-Y.; Suh, Y.J.; Sung, J.-J. High neutrophil-to-lymphocyte ratio predicts short survival duration in amyotrophic lateral sclerosis. Sci. Rep. 2020, 10, 428. [Google Scholar] [CrossRef]
- Hou, D.; Wang, C.; Luo, Y.; Ye, X.; Han, X.; Feng, Y.; Zhong, P.; Wu, D. Systemic immune-inflammation index (SII) but not platelet-albumin-bilirubin (PALBI) grade is associated with severity of acute ischemic stroke (AIS). Int. J. Neurosci. 2021, 131, 1203–1208. [Google Scholar] [CrossRef] [PubMed]
- Nam, K.-W.; Kwon, H.-M.; Jeong, H.-Y.; Park, J.-H.; Kwon, H. Systemic immune-inflammation index is associated with white matter hyperintensity volume. Sci. Rep. 2022, 12, 7379. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Nao, J.; Shi, J.; Zheng, D. Predictive Value of Routine Peripheral Blood Biomarkers in Alzheimer’s Disease. Front. Aging Neurosci. 2019, 11, 332. [Google Scholar] [CrossRef]
- Shad, K.F.; Aghazadeh, Y.; Ahmad, S.; Kress, B. Peripheral markers of Alzheimer’s disease: Surveillance of white blood cells. Synapse 2013, 67, 541–543. [Google Scholar] [CrossRef] [PubMed]
- Kuyumcu, M.E.; Yesil, Y.; Oztürk, Z.A.; Kizilarslanoglu, C.; Etgül, S.; Halil, M.; Ulger, Z.; Cankurtaran, M.; Ariogul, S. The evaluation of neutrophil-lymphocyte ratio in Alzheimer’s disease. Dement. Geriatr. Cogn. Disord. 2012, 34, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Rembach, A.; Watt, A.D.; Wilson, W.J.; Rainey-Smith, S.; Ellis, K.A.; Rowe, C.C.; Villemagne, V.L.; Macaulay, S.L.; Bush, A.I.; Martins, R.N.; et al. An increased neutrophil-lymphocyte ratio in Alzheimer’s disease is a function of age and is weakly correlated with neocortical amyloid accumulation. J. Neuroimmunol. 2014, 273, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Kalelioglu, T.; Yuruyen, M.; Gultekin, G.; Yavuzer, H.; Özturk, Y.; Kurt, M.; Topcu, Y.; Doventas, A.; Emul, M. Neutrophil and platelet to lymphocyte ratios in people with subjective, mild cognitive impairment and early Alzheimer’s disease. Psychogeriatrics 2017, 17, 506–508. [Google Scholar] [CrossRef]
- Fani, L.; Ahmad, S.; Ikram, M.K.; Ghanbari, M.; Ikram, M.A. Immunity and amyloid beta, total tau and neurofilament light chain: Findings from a community-based cohort study. Alzheime’rs Dement. 2021, 17, 446–456. [Google Scholar] [CrossRef]
- Stephan, B.C.M.; Brayne, C.; Savva, G.M.; Matthews, F.E. Occurrence of medical co-morbidity in mild cognitive impairment: Implications for generalisation of MCI research. Age Ageing 2011, 40, 501–507. [Google Scholar] [CrossRef]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef]
- Moreta, M.P.-G.; Burgos-Alonso, N.; Torrecilla, M.; Marco-Contelles, J.; Bruzos-Cidón, C. Efficacy of Acetylcholinesterase Inhibitors on Cognitive Function in Alzheimer’s Disease. Review of Reviews. Biomedicines 2021, 9, 1689. [Google Scholar] [CrossRef] [PubMed]
- Borda, M.G.; Jaramillo-Jimenez, A.; Oesterhus, R.; Santacruz, J.M.; Tovar-Rios, D.A.; Soennesyn, H.; Cano-Gutierrez, C.A.; Vik-Mo, A.O.; Aarsland, D. Benzodiazepines and antidepressants: Effects on cognitive and functional decline in Alzheimer’s disease and Lewy body dementia. Int. J. Geriatr. Psychiatry 2021, 36, 917–925. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, C.; Garcez, H.; Balaban, S.; Barbosa, F.; Pereira, M.R.; Silveira, C.; Marques-Teixeira, J.; Gonçalves, A.R. Effects of Concomitant Benzodiazepines and Antidepressants Long-Term Use on Social Decision-Making: Results from the Ultimatum Game. Front Psychol. 2022, 13, 915265. [Google Scholar] [CrossRef] [PubMed]
- McKhann, G.M.; Knopman, D.S.; Chertkow, H.; Hyman, B.T.; Jack, C.R.J.; Kawas, C.H.; Klunk, W.E.; Koroshetz, W.J.; Manly, J.J.; Mayeux, R.; et al. The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dement. 2011, 7, 263–269. [Google Scholar] [CrossRef]
- McKeith, I.G.; Boeve, B.F.; Dickson, D.W.; Halliday, G.; Taylor, J.-P.; Weintraub, D.; Aarsland, D.; Galvin, J.; Attems, J.; Ballard, C.G.; et al. Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium. Neurology 2017, 89, 88–100. [Google Scholar] [CrossRef] [PubMed]
- Rascovsky, K.; Hodges, J.R.; Knopman, D.; Mendez, M.F.; Kramer, J.H.; Neuhaus, J.; Van Swieten, J.C.; Seelaar, H.; Dopper, E.G.; Onyike, C.U.; et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain 2011, 134, 2456–2477. [Google Scholar] [CrossRef] [PubMed]
- Román, G.C.; Tatemichi, T.K.; Erkinjuntti, T.; Cummings, J.L.; Masdeu, J.C.; Garcia, J.H.; Amaducci, L.; Orgogozo, J.M.; Brun, A.; Hofman, A.; et al. Vascular dementia: Diagnostic criteria for research studies. Report of the NINDS-AIREN International Workshop. Neurology 1993, 43, 250–260. [Google Scholar] [CrossRef]
- Caroli, A.; Prestia, A.; Galluzzi, S.; Ferrari, C.; van der Flier, W.M.; Ossenkoppele, R.; Van Berckel, B.; Barkhof, F.; Teunissen, C.; Wall, A.E.; et al. Mild cognitive impairment with suspected nonamyloid pathology (SNAP): Prediction of progression. Neurology 2015, 84, 508–515. [Google Scholar] [CrossRef]
- Wu, C.-Y.; Bawa, K.K.; Ouk, M.; Leung, N.; Yu, D.; Lanctôt, K.L.; Herrmann, N.; Pakosh, M.; Swardfager, W. Neutrophil activation in Alzheimer’s disease and mild cognitive impairment: A systematic review and meta-analysis of protein markers in blood and cerebrospinal fluid. Ageing Res Rev. 2020, 62, 101130. [Google Scholar] [CrossRef]
- Hou, J.-H.; Ou, Y.-N.; Xu, W.; Zhang, P.-F.; Tan, L.; Yu, J.-T. Association of peripheral immunity with cognition, neuroimaging, and Alzheimer’s pathology. Alzheimer’s Res. Ther. 2022, 14, 29. [Google Scholar] [CrossRef]
- Li, W.; Hou, M.; Ding, Z.; Liu, X.; Shao, Y.; Li, X. Prognostic Value of Neutrophil-to-Lymphocyte Ratio in Stroke: A Systematic Review and Meta-Analysis. Front. Neurol. 2021, 12, 686983. [Google Scholar] [CrossRef] [PubMed]
- Tondo, G.; De Marchi, F. From Biomarkers to Precision Medicine in Neurodegenerative Diseases: Where Are We? J. Clin. Med. 2022, 11, 4515. [Google Scholar] [CrossRef]
- Hou, L.; Zhang, S.; Qi, D.; Jia, T.; Wang, H.; Zhang, W.; Wei, S.; Xue, C.; Wang, P. Correlation between neutrophil/lymphocyte ratio and cognitive impairment in cerebral small vessel disease patients: A retrospective study. Front. Neurol. 2022, 13, 925218. [Google Scholar] [CrossRef]
- Arevalo-Rodriguez, I.; Smailagic, N.; Roqué-Figuls, M.; Ciapponi, A.; Sanchez-Perez, E.; Giannakou, A.; Pedraza, O.L.; Cosp, X.B.; Cullum, S. Mini-Mental State Examination (MMSE) for the early detection of dementia in people with mild cognitive impairment (MCI). Cochrane Database Syst. Rev. 2021, 7, CD010783. [Google Scholar] [PubMed]
- An, P.; Zhou, X.; Du, Y.; Zhao, J.; Song, A.; Liu, H.; Ma, F.; Huang, G. Association of Neutrophil-Lymphocyte Ratio with Mild Cognitive Impairment in Elderly Chinese Adults: A Case-control Study. Curr. Alzheimer Res. 2019, 16, 1309–1315. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Cejudo, J.; Johnson, A.D.; Beiser, A.; Seshadri, S.; Salinas, J.; Berger, J.S.; Fillmore, N.R.; Do, N.; Zheng, C.; Kovbasyuk, Z.; et al. The Neutrophil to Lymphocyte Ratio Is Associated with the Risk of Subsequent Dementia in the Framingham Heart Study. Front. Aging Neurosci. 2021, 13, 773984. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Chen, Q.; Luo, X.; Hong, J.; Pan, K.; Lin, X.; Liu, X.; Zhou, L.; Wang, H.; Xu, Y.; et al. Neutrophil-to-Lymphocyte Ratio Positively Correlates to Age in Healthy Population. J. Clin. Lab. Anal. 2015, 29, 437–443. [Google Scholar] [CrossRef]
- Thaipisuttikul, P.; Jaikla, K.; Satthong, S.; Wisajun, P. Rate of conversion from mild cognitive impairment to dementia in a Thai hospital-based population: A retrospective cohort. Alzheimer’s Dement. 2022, 8, e12272. [Google Scholar] [CrossRef]
- Espinosa, A.; Alegret, M.; Valero, S.; Vinyes-Junqué, G.; Hernández, I.; Mauleón, A.; Rosende-Roca, M.; Ruiz, A.; López, O.; Tárraga, L.; et al. A longitudinal follow-up of 550 mild cognitive impairment patients: Evidence for large conversion to dementia rates and detection of major risk factors involved. J. Alzheimer’s Dis. 2013, 34, 769–780. [Google Scholar] [CrossRef]
- Tondo, G.; De Marchi, F.; Terazzi, E.; Prandi, P.; Sacchetti, M.; Comi, C.; Cantello, R. Chronic obstructive pulmonary disease may complicate Alzheimer’s disease: A comorbidity problem. Neurol. Sci. 2018, 39, 1585–1589. [Google Scholar] [CrossRef]
- Goldstein, F.C.; Ashley, A.V.; Endeshaw, Y.W.; Hanfelt, J.; Lah, J.J.; Levey, A.I. Effects of hypertension and hypercholesterolemia on cognitive functioning in patients with alzheimer disease. Alzheimer Dis. Assoc. Disord. 2008, 22, 336–342. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Seo, H.I.; Cha, H.Y.; Yang, Y.J.; Kwon, S.H.; Yang, S.J. Diabetes and Alzheimer’s Disease: Mechanisms and Nutritional Aspects. Clin. Nutr. Res. 2018, 7, 229–240. [Google Scholar] [CrossRef] [PubMed]



| Sample Characteristics | Amnestic MCI (n = 130) |
|---|---|
| Age at the first evaluation (median ± IQR) | 76.50 (72.00–79.00) years |
| Female sex, n (%) | 72 (55%) |
| Educational level (mean ± SD) | 7.25 ± 3.28 years |
| Symptom’s onset (median ± IQR) | 1.20 (0.60–2.40) years |
| Follow-up duration (median ± IQR) | 2.67 (2.33–3.50) years |
| Baseline MMSE corrected score (mean ± SD) | 26.02 ± 2.28 points |
| Follow-up MMSE corrected score (mean ± SD) | 23.10 ± 4.32 |
| Index of progression | −1.06 ± 1.33 points per year |
| Conversion at the last follow-up, n (%) | 65 (50%) |
| Demographics and Clinical Data | Non-Converters n = 65 | Converters n = 65 | p-Value |
|---|---|---|---|
| Age at the first evaluation (mean ± SD) | 75.42 ± 5.08 years | 76.83 ± 5.07 years | 0.169 |
| Female sex, n (%) | 31 (48%) | 41 (63%) | 0.077 |
| Educational level (mean ± SD) | 7.02 ± 3.07 years | 7.49 ± 3.47 years | 0.342 |
| Symptom’s onset (mean ± SD) | 1.15 ± 0.83 years | 1.10 ± 0.76 years | 0.783 |
| Follow-up duration (mean ± SD) | 2.84 ± 0.87 years | 3.01 ± 0.73 years | 0.119 |
| Subjects with no or one comorbidity, n (%) | 21 (32%) | 21 (32%) | - |
| Subjects with two or more comorbidities, n (%) | 44 (68%) | 44 (68%) | - |
| Cognitive data | p-value | ||
| Baseline MMSE corrected score (mean ± SD) | 26.69 ± 2.37 points | 25.36 ± 1.97 points | 0.004 |
| Follow-up MMSE corrected score (mean ± SD) | 26.18 ± 2.80 points | 20.01 ± 3.24 points | <0.001 |
| Index of progression | −0.19 ± 0.73 points per year | −1.93 ± 1.23 points per year | <0.001 |
| Hematological and biochemistry data | p-value | ||
| WBCs (109/L) | 6.69 ± 1.60 | 6.78 ± 1.42 | 0.495 |
| Neutrophils (109/L) | 4.17 ± 1.26 | 4.89 ± 1.35 | 0.328 |
| Lymphocytes (109/L) | 2.94 ± 0.62 | 1.73 ± 0.49 | 0.001 |
| Monocyte (109/L) | 0.45 ± 0.12 | 0.40 ± 0.12 | 0.054 |
| Eosinophilia (109/L) | 0.18 ± 0.11 | 0.17 ± 0.10 | 0.406 |
| Basophilia (109/L) | 0.04 ± 0.04 | 0.03 ± 0.04 | 0.533 |
| RBCs (1012/L) | 4.34 ± 0.50 | 4.30 ± 0.48 | 0.192 |
| Hemoglobin (g/dL) | 13.64 ± 1.33 | 13.55 ± 1.47 | 0.849 |
| Hematocrit (%) | 42% | 41% | 0.732 |
| Platelet (109/L) | 213.52 ± 50.81 | 231.64 ± 64.92 | 0.167 |
| Mean platelet volume (femtoliters) | 8.76 ± 1.70 | 8.57 ± 1.63 | 0.418 |
| NLR | 2.23 ± 0.99 | 2.77 ± 1.21 | 0.005 |
| LMR | 4.81 ± 1.73 | 4.82 ± 2.84 | 0.416 |
| MLR | 0.23 ± 0.08 | 0.24 ± 0.008 | 0.416 |
| PLR | 113.43 ± 42.83 | 146.47 ± 69.53 | 0.002 |
| SII | 471.56 ± 218.04 | 673.37 ± 468.88 | 0.015 |
| Fasting glucose (mg/dL) | 100.45 ± 25.98 | 99.18 ± 31.15 | 0.614 |
| Creatinine (mg/dL) | 0.88 ± 0.15 | 0.85 ± 0.21 | 0.721 |
| Total Cholesterol (mg/dL) | 172.30 ± 56.79 | 180.49 ± 53.25 | 0.393 |
| Triglycerides (mg/dL) | 120.97 ± 60.81 | 115.37 ± 47.65 | 0.899 |
| Vitamin B12 (pg/mL) | 380.95 ± 258.10 | 345.73 ± 251.20 | 0.335 |
| Folate (ng/mL) | 6.58 ± 4.53 | 6.28 ± 4.54 | 0.829 |
| Thyroid-stimulating hormone (mIU/L) | 1.84 ± 1.76 | 1.31 ± 0.99 | 0.109 |
| C-Reactive Protein (mg/dL) | 0.34 ± 0.10 | 0.32 ± 0.12 | 0.784 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tondo, G.; Aprile, D.; De Marchi, F.; Sarasso, B.; Serra, P.; Borasio, G.; Rojo, E.; Arenillas, J.F.; Comi, C. Investigating the Prognostic Role of Peripheral Inflammatory Markers in Mild Cognitive Impairment. J. Clin. Med. 2023, 12, 4298. https://doi.org/10.3390/jcm12134298
Tondo G, Aprile D, De Marchi F, Sarasso B, Serra P, Borasio G, Rojo E, Arenillas JF, Comi C. Investigating the Prognostic Role of Peripheral Inflammatory Markers in Mild Cognitive Impairment. Journal of Clinical Medicine. 2023; 12(13):4298. https://doi.org/10.3390/jcm12134298
Chicago/Turabian StyleTondo, Giacomo, Davide Aprile, Fabiola De Marchi, Barbara Sarasso, Paola Serra, Giordana Borasio, Esther Rojo, Juan Francisco Arenillas, and Cristoforo Comi. 2023. "Investigating the Prognostic Role of Peripheral Inflammatory Markers in Mild Cognitive Impairment" Journal of Clinical Medicine 12, no. 13: 4298. https://doi.org/10.3390/jcm12134298
APA StyleTondo, G., Aprile, D., De Marchi, F., Sarasso, B., Serra, P., Borasio, G., Rojo, E., Arenillas, J. F., & Comi, C. (2023). Investigating the Prognostic Role of Peripheral Inflammatory Markers in Mild Cognitive Impairment. Journal of Clinical Medicine, 12(13), 4298. https://doi.org/10.3390/jcm12134298








