Abstract
The therapeutic alliance is a fundamental component of rehabilitation in order to achieve effective outcomes. However, what develops, maintains or hinders this relationship has not been sufficiently explored. The aim of this systematic review is to recognize the role of the therapeutic alliance in the neurological rehabilitation process. A search for articles was carried out in the databases PubMed, Web of Science, SCOPUS, CINAHL, APA PsycInfo, OTseeker and Dialnet. They were selected according to the eligibility criteria. Internal quality assessment of the articles was measured with the Consolidated Criteria for Reporting Qualitative Research (COREQ). The systematic review was registered in PROSPERO (ID 346523). The search in the databases identified 1596 articles, from which 9 different studies were finally included in the systematic review, reflecting the limitations of studies in this field. All studies are qualitative, from the point of view of the patients themselves, their relatives and healthcare professionals. The total sample of the included studies is 182 participants (96 health professionals, 76 users and 10 relatives). Semi-structured interviews, focus group discussions and written reflections were mainly used to collect the data. In conclusion, the therapeutic alliance can be an active component in the post-stroke rehabilitation process. Being recognized as a person, collaboration with the therapeutic team, empathy, empowerment, confidence, professional skills, maintenance of hope and the role of the family have been identified as aspects that can have an influence on the therapeutic alliance.
1. Introduction
Acquired brain injury is defined as any brain damage occurring after birth [1]. Causes can be traumatic, due to extrinsic injury, or non-traumatic, due to internal pathological processes, encompassing multiple diseases [1,2,3]. These include stroke, an important public health issue causing significant problems of long-term disability and considerably decreasing quality of life [4,5].
Findings indicate that rehabilitation plays an essential role in establishing functional performance and quality of life for people after stroke [6,7].
This process of neurological rehabilitation aims to achieve functionality, recovering or developing mental, physical and social capacities to their maximum potential [8]. To this end, the therapeutic alliance is considered an important aspect and a determinant of outcomes [9,10], as it has been related to functional development, productivity, self-awareness and emotional self-regulation [11], in addition to improving symptoms, increasing satisfaction, quality of life and psychological wellbeing [12]. Some people have even reported that the quality of the therapeutic relationship is more meaningful to them than the content of the therapy or its outcomes [13].
The therapeutic alliance or relationship aims to establish a consensus on goals with the patient and a personal bond between both parties [12]. It requires a person-centered approach [11], responding to the patient’s needs and improving the experience and outcomes of the individual’s recovery process [14,15].
Historically, the concept of alliance dates back to the Freudian period of psychodynamic theory [9,16]. Subsequently, this aspect has been recognized as essential in therapist–patient relationships by different psychologists from different theoretical perspectives [16,17,18].
According to Bordin, a renowned American psychology professor, the alliance is composed of three components: agreement on therapeutic goals, consensus on the tasks that are part of the therapy and the bond between patient and therapist [16]. His theoretical framework supports most of the studies that evaluate the therapeutic alliance and its effect on neurologicalrehabilitation [11].
In clinical praxis, health professionals adapt treatment through their knowledge in order to improve the quality of life and wellbeing of the individual [19,20], but it is the active participation of the individuals themselves that contributes to the relationship [19,21]. Results from physical rehabilitation in stroke show that there is a correlation between the therapeutic alliance and patient engagement, which is a facilitating factor for adherence [12]. Conversely, lack of engagement limits the increase in function and has an impact on quality of life [22].
Europe is becoming an actively aging continent to be considered, and as age increases, neurological disorders become more prevalent [4,23]. Moreover, the number of people suffering a stroke at a younger age is increasing [24], and there is evidence that health services will not be able to deal with this increase [4].
For this reason, this systematic review aims to conduct an exploration of the most recent literature to recognize the role of the therapeutic alliance in the neurological rehabilitation process. This concept plays an important role in healthcare, but research on this aspect in stroke rehabilitation is limited [11].
2. Materials and Methods
The development of this systematic review was guided by the “PRISMA 2020” statement, and its registration information is available [25].
2.1. Information Sources and Search Strategy
To carry out this systematic review, a search was performed in the databasesPubMed, Web of Science, SCOPUS, CINAHL, APA PsycInfo, OTseeker and Dialnet, using the descriptors “Therapeutic Alliance”, “Stroke”, “Outcome” and “Recovery of function”. The final search strategy focused on stroke due to a higher amount of published studies, which allowed finding more homogeneous results.
The search strategy used was the same in the different databases, obtaining different results through the possible applicable filters (see Table 1), limiting the search chronologically (2012–2022), by language and by type of study.

Table 1.
Databases and search results.
To understand the basic procedures used in this systematic review and to analyze the screening and selection of the studies, a PRISMA flow diagram was completed (see Figure 1).
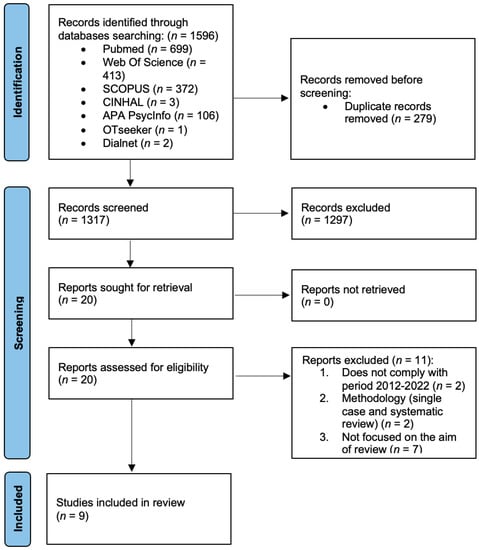
Figure 1.
PRISMA flow diagram of study selection process.
2.2. Quality Assessment of Included Studies
Internal quality assessment of the articles used in this systematic review was carried out using the Consolidated Criteria for Reporting Qualitative Research (COREQ). This instrument includes 32 items, covering the characteristics of the research team, the design and context of the study, the results of the study and the analysis and interpretation of the results [26].
2.3. Eligibility Criteria and Study Selection
Only studies published in English and in the last 10 years were selected for current data, including those published from January 2012 to January 2022. In terms of design, only qualitative studies that included exploratory, ethnographic, grounded theory, constructivist, interpretative action or interpretive description methodology were accepted. The only studies included were those that focused on acquired brain injury and the therapeutic alliance, in a physical, cognitive, language or functional rehabilitation context, with the user or their relatives.
On the other hand, studies that focused on other neurologic pathologies and one case study were excluded, as well as studies that focused on the therapeutic alliance within pharmacological therapies, because direct interaction with the therapist may be less frequent compared to physical, cognitive, language or functional rehabilitation carried out by health professionals.
3. Results
The final screen of the systematic review contains nine articles, which are presented in Table 2. In addition, the authors, year, type of study, study objective, sample, instruments used, some intervention details, main results and internal quality of the results are also briefly presented, considering the qualitative research tool mentioned above. The total sample of the included studies is 182 participants (96 health professionals, 76 users and 10 relatives).

Table 2.
Overview of included studies.
The quality of the studies included in the review has an average score of 25/32, which indicates an optimum value.
Most of the criteria that have not been fulfilled are related to the personal characteristics of the research team, such as their credentials, their occupation at the time of the study and their experience and training.
Other lacking criteria are related to the study design, in cases where we did not find information about presence of non-participants at the time of the interview and items related to data collection, such as whether interviews were repeated and whether data saturation was reached.
4. Discussion
The results of this systematic review show the characteristics associated with the therapeutic alliance in the post-stroke rehabilitation process from the point of view of healthcare professionals, patients themselves and their relatives.
Qualitative research studies explore perspectives and experiences of individuals [27], deepening the understanding of the post-stroke adaptation process of survivors and guaranteeing a person-centered practice [28].
Different aspects shared in the studies analyzed have been identified, such as the recognition of personhood, which is considered a process that builds the foundations of trust and the therapeutic alliance [11,29,30]. Differences are found between studies that support the breaking of the therapeutic gap [31] and others that value the preservation of professional limits [11,29,32].
According to some studies, patients feeling listened to and understood will increase personal connection and the perception of support [11,30,31,32,33], while for others, this relationship may create dependence [29].
Finally, we also highlight factors such as hope [29,33,34] and the role of the family as contextual shapers of the development of the therapeutic alliance [11,29], as compared to studies in which the single relationship between professional and patient [11] is prioritized.
Based on the different studies consulted, we divide the present discussion into different sections on topics considered basic aspects in the therapeutic alliance that need to be addressed. The topics presented below are “Being recognised as a person”, “Empathy, emotional bonding and trust”, “Collaboration” (with the subtopics “Individualising rehabilitation”, “Control and empowerment” and “Role of health professionals”), “Maintaining hope” and “The family”.
4.1. Being Recognised as a Person
Recognition of patients’ personhood is apparently one of the first processes that promotes trust and builds the basis for the development of the therapeutic alliance [11,29,30], which originates from a connection on a human level [30]. Several people valued identity preservation by healthcare staff [32]. This quality has not always been prioritized, as some professionals consider it incongruent with patients’ expectations of their recovery process [29].
Self-revelation by professionals appears to be a feature that helps build recognition and bonding in the dyad [11,29,31,32], often being perceived as a way of breaking down barriers between both parties [11]. The therapeutic gap allows people to feel more comfortable and connected to the community [31]. However, others maintain their stance on the preservation of professional barriers [29]. In addition, there are patients who recognize the need for these limits [11], and some with fewer rehabilitation needs express satisfaction with this division approach, simply requiring therapists to focus on treatment [32], in order to “run away home” [11].
Hersh et al. [35] also highlight informal assessment as a more person-centered method of working in the early post-stroke period, the first point of contact with patients, during which professionals want to establish and facilitate interpersonal relationships.
Many professionals described the difficulty of this approach due to the hospital environment and policies, which do not allow for an in-depth relationship due to time and resource constraints [29]. However, professionals engaging in getting to know the person seems a crucial process in rehabilitation [33].
4.2. Empathy, Emotional Bonding and Trust
Close therapeutic alliances were described as open and relaxed, without any judgement from the staff [32]. In the study of Walder and Molineux [34], some people report that they perceived a lack of understanding of experience, thoughts and emotions on the part of healthcare staff.
The feeling of being listened to and understood is seen as critical to mitigating isolation and building trust [32], as well as increasing personal connection [11] and the perception of support [31]; particularly in the early stages of rehabilitation, during which people feel more vulnerable and report needing more than professionalism [30,32].
Although forming bonds is seen as a vital aspect of engagement, it has been felt that if bonds become too close, it can create dependency [29]. Therapists reported that deep connection and trust are dependent on time and frequency of contact [29]. In the study of Williams and Douglas [31], patients’ sense of comfort was related to the friendliness of professionals, and they highlighted the importance of a welcoming and positive first contact.
To empathize with patients, professionals highlighted the value of showing an understanding of the impact of stroke on a person’s life, through listening and normalizing the experience [29].
Even goal setting requires some work on an emotional level by therapists that often seems extraneous to professional value but is a crucial part of person-centered care [36].
A trusting context allows for an open and transparent space that facilitates getting to know each other and implies that patients feel safe in the interaction. In addition, trust promotes engagement in the recovery process [33].
This can be affected by the sense of unfamiliarity generated by healthcare staff, as many patients do not come to understand their diagnosis and the recovery process and are often not offered explicit information [32], creating a sense of uncertainty in the early stages [33].
4.3. Collaboration
Collaboration appears to be based on building a mutual consensus on the individual’s environment and characteristics [11]. Many report that it is dependent on the therapist’s ability to get to know the person and identify their needs [32] or meaningful goals [34] in order to acquire a shared approach [11].
Therapeutic alliance is clearly related to appropriate connection and collaboration in the recovery process [31,32].
Collaborating in the relationship seems to imply reciprocity [11] and investment [33]. Reciprocity shows the relationship between engagement and trust [33], and personhood recognition sets the foundation for its development [29]. On the other hand, investment refers to the dedication and involvement at the emotional level experienced by dyad members in the recovery process [33].
In the study of Kayes et al. [33], the professionals reported difficulty in engaging if patients are not engaged, and the individuals acknowledged their active role in the collaboration.
Furthermore, when exploring individuals’ experiences, they expressed the importance of being able to be part of the team, feeling able to contribute to it [31].
Time limitations and the pressure to achieve goals within hospital policies also influenced engagement, with it being more favored in a home environment characterized by a relaxed atmosphere [29].
4.4. Individualising Rehabilitation
Many highlight as an essential factor in the therapeutic alliance the individualization of rehabilitation according to the needs of the patient [11,29,31,32,34,36].
In the study of Lawton et al. [29], they express it as being responsive and adapting behaviors to meet the person’s needs. In this process, the knowledge of the patient on the part of the healthcare staff comes into play [29,33]. Mutual understanding enables the skills of professionals to be adapted to the needs and preferences of patients [11].
On one hand, there are information needs, as expressed in the studies of Lawton et al. [29], Lawton et al. [32] and Walder and Molineux [34], as there are patients who need to understand the goal they are working on in the rehabilitation exercises. Information needs even include information about the diagnosis, the prognosis and their process, as expressed by Lawton et al. [32].Transition points such as discharge or assessment for admission to rehabilitation were key points where participants noted a lack of information [34], and adapting this to their understanding was valued by patients [31].
On the other hand, there was also the need for adaptation, highlighted in the study of Kayes et al. [33].Practitioners need to know where the pressure limit is, balancing a challenge without creating a sense of frustration due to functionality problems.
Underpinning this is the ability of therapists to respond and adjust tasks accordingly [32].
A non-adaptive outcome could lead to disengagement of the patient in their process [11,34] and affect their engagement [32].
4.5. Control and Empowerment
These aspects are seen as an integral part of the development of the therapeutic relationship, as professionals take on an accompanying role in the rehabilitation process [29] and patients want to be empowered [36], a dimension included in the dynamic conceptualization of the alliance [37].
Taking ownership of the recovery process is relevant for patients [31,32,34]. Participants in the study of Walder and Molineux [34] reported not feeling in control of important decisions and feeling excluded from preferences about their care, with no consideration of their emotions or needs.
On the other hand, some prioritized therapists taking on this responsibility [11,32] and others reported being unprepared due to cognitive, emotional or psychosocial factors [36], particularly in the early stages of stroke [29].
The fact that professionals place trust in patients’ ability to be active agents in the process, taking risks and knowing their abilities, seems to be an important aspect for them [33]. In addition, professionals described feeling more relaxed with people who were in control and actively involved in the relationship [29].
The findings of dissatisfied needs suggest that the level of collaboration and empowerment of the individual may not always be optimal [38]. Alliances distinguished by imposition accentuate the professional–patient division and have the potential to damage self-esteem [32].
4.6. Role of Health Professionals
Professionals’ skills also interact to dictate the success of the alliance [11,29]. Patients described that feeling heard and understood and understanding information derived from their recovery process depended on the therapist’s communication skills [31,32]. In addition, other studies add knowledge as a basis for adapting rehabilitation according to the characteristics of the individual [29,32,33].
Personal engagement and advanced communication skills can add significant value to therapeutic connections, but many professionals are not prepared for this [36]. Some therapists report feeling poorly equipped, lacking the necessary skills to promote behavior change and intervene in patients’ engagement and motivation [29].
On the other hand, it is important for individuals to know the rehabilitation team, their background, their experience and their qualifications, as it seemed to establish trust within the dyad [33].
4.7. Maintaining Hope
There is a discomfort for professionals with setting ‘unrealistic’ goals for patients, creating an acknowledged emotional tension due to conflict between the biomedical model and the person-centered perspective [36]. In the study of Lawton et al. [29], several speech therapists reported that there is a possibility of disengagement and the creation of conflict with the patient if conflicting expectations are not managed. At the same time, such a realistic approach can damage hope, and so‘walking the line’ is recommended, which involves balancing what are perceived as realistic expectations with hope.
False hope is correlated with a lack of skills or explicit knowledge on the part of health professionals, who do not believe in influencing this concept [29]. However, health professionals can intervene in it in a meaningful way, and it is considered an important aspect for patients in their recovery process, as they identify it as an emotional motivator related to quality of life and influencing their engagement [33,34].
Findings from previous studies already identify the importance of aligning expectations and maintaining hope during alliance building [39,40,41,42]. In the study of Walder and Molineux [34], patients described that, to protect this maintenance of hope, it is necessary to know when not to press to safeguard the person’s psychological state and preserve optimism in the dyad.
4.8. The Family
Recently, the dynamic concept of the alliance has also been extended to include the family dimension [37], in which rehabilitation recognizes individuals and their relatives as team members involved in decisionmaking [43].
As some studies show, the therapeutic alliance is not limited to the professional–patient dyad, and the family connection becomes vitally important [11,29]. It was recognized as a context shaperthat facilitates or impedes the development of the alliance [11,29]. However, others prioritize the exclusive therapeutic relationship between healthcare professionals and patients [11].
Several studies have shown that a good alliance with the family influences outcomes, making it another crucial component in rehabilitation [43].
We have been able to explore the characteristics of the therapeutic alliance during the post-stroke recovery process, but more research is needed on the role of the therapeutic alliance in rehabilitation. For example, it would be valuable to increase the sample size of studies in order to build on the current knowledge base. It would also be useful to explore the relationship of the therapeutic alliance with adherence, engagement and rehabilitation outcomes.
This study has potential limitations. When carrying out searches in the different databases, a seemingly large number of results were found, which has then been significantly reduced by the exclusion criteria of this review. This is justified, as there is a considerable amount of research on the therapeutic alliance, but most of it is associated with pharmacological therapies, without focusing on the process of functional rehabilitation after stroke. Furthermore, following the difficulties experienced in the early stages of the research process, studies with less scientific evidence have been used, justified by the absence ofquantitative results.
5. Conclusions
The therapeutic alliance concept has been explored in recent qualitative studies, in which patients, their relatives and health professionals have recognized that it can be an active component in the rehabilitation process after stroke.
The research involved shows us the characteristics that can influence the therapeutic alliance, such as being recognized as a person; collaboration with the health professional, including qualities such as empathy, trust, empowerment and professional skills; maintenance of hope; and the role of the family.
Despite all the findings, the progress in the literature and the knowledge we have that the therapeutic alliance is of significant value in healthcare, research on this aspect of stroke rehabilitation is limited [11]. Further understanding of the role this concept plays in the process of recovery and adaptation after stroke may be helpful in working with individuals to optimize rehabilitation outcomes. Therefore, we suggest continuing with research and carrying out studies on a larger scale, in order torecognize the therapeutic alliance as a determinant in the recovery process and to be able to achieve better outcomes and increase quality of life.
Furthermore, the relationship of the therapeutic alliance to adherence and the development of assessment tools to measure this concept could be of interest. The first accessible and theoretically robust measure of therapeutic alliance has recently been developed, called “Aphasia and stroke therapeutic alliance measure (A-STAM)”. The sample size and the exclusion of people with more severe language abilities and family members are some of its limitations [44]. Therefore, modifying them may become of significant importance for research in order to further study and understand therapeutic alliance.
Author Contributions
Conceptualization, A.H.-C. and M.C.R.-M.; methodology, A.H.-C., M.C.R.-M. and P.G.-P.; writing—original draft preparation, A.H.-C., P.G.-P. and M.C.R.-M.; writing—review and editing, A.H.-C., M.C.R.-M., P.G.-P., J.A.A.-P. and M.Á.I.-R.; supervision, M.C.R.-M., P.G.-P., J.A.A.-P. and M.Á.I.-R.; funding acquisition, M.C.R.-M., J.A.A.-P. and M.Á.I.-R. All authors have read and agreed to the published version of the manuscript.
Funding
The APC was funded by University of Málaga.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
For additional information, please contact with María Carmen Rodríguez-Martínez (marrodmar@uma.es).
Conflicts of Interest
The authors have no relevant financial or non-financial interests to disclose. The systematic review was registered in PROSPERO (ID 346523). The principles of the Declaration of Helsinki were followed.
References
- Fleminger, S.; Ponsford, J. Long Term Outcome after Traumatic Brain Injury. BMJ 2005, 331, 1419–1420. [Google Scholar] [CrossRef]
- Bruns, J.; Hauser, W.A. The Epidemiology of Traumatic Brain Injury: A Review. Epilepsia 2003, 44, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Goldman, L.; Siddiqui, E.M.; Khan, A.; Jahan, S.; Rehman, M.U.; Mehan, S.; Sharma, R.; Budkin, S.; Kumar, S.N.; Sahu, A.; et al. Understanding Acquired Brain Injury: A Review. Biomedicines 2022, 10, 2167. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Neurological Disorders: Public Health Challenges; World Health Organization: Geneva, Switzerland, 2006; Volume 218. [Google Scholar]
- Perin, C.; Bolis, M.; Limonta, M.; Meroni, R.; Ostasiewicz, K.; Cornaggia, C.M.; Alouche, S.R.; da Silva Matuti, G.; Cerri, C.G.; Piscitelli, D. Differences in Rehabilitation Needs after Stroke: A Similarity Analysis on the ICF Core Set for Stroke. Int. J. Environ. Res. Public Health 2020, 17, 4291. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, R.B.C.; Galvão, S.C.B.; Frederico, L.M.P.; Amaral, N.S.L.; Carneiro, M.I.S.; de Moura Filho, A.G.; Piscitelli, D.; Monte-Silva, K. Cortical and Spinal Excitability Changes after Repetitive Transcranial Magnetic Stimulation Combined to Physiotherapy in Stroke Spastic Patients. Neurol. Sci. 2019, 40, 1199–1207. [Google Scholar] [CrossRef]
- Monte-Silva, K.; Piscitelli, D.; Norouzi-Gheidari, N.; Batalla, M.A.P.; Archambault, P.; Levin, M.F. Electromyogram-Related Neuromuscular Electrical Stimulation for Restoring Wrist and Hand Movement in Poststroke Hemiplegia: A Systematic Review and Meta-Analysis. Neurorehabil. Neural Repair 2019, 33, 96–111. [Google Scholar] [CrossRef]
- World Health Organization (Ed.) International Classification of Functioning, Disability and Health: ICF; World Health Organization: Geneva, Switzerland, 2001; ISBN 978-92-4-154542-6. [Google Scholar]
- Ardito, R.; Rabellino, D. Therapeutic Alliance and Outcome of Psychotherapy: Historical Excursus, Measurements, and Prospects for Research. Front. Psychol. 2011, 2, 270. [Google Scholar] [CrossRef]
- Graves, T.A.; Tabri, N.; Thompson-Brenner, H.; Franko, D.L.; Eddy, K.T.; Bourion-Bedes, S.; Brown, A.; Constantino, M.J.; Flückiger, C.; Forsberg, S.; et al. A Meta-Analysis of the Relation between Therapeutic Alliance and Treatment Outcome in Eating Disorders. Int. J. Eat. Disord. 2017, 50, 323–340. [Google Scholar] [CrossRef] [PubMed]
- Bishop, M.; Kayes, N.; McPherson, K. Understanding the Therapeutic Alliance in Stroke Rehabilitation. Disabil. Rehabil. 2021, 43, 1074–1083. [Google Scholar] [CrossRef]
- Babatunde, F.; MacDermid, J.; MacIntyre, N. Characteristics of Therapeutic Alliance in Musculoskeletal Physiotherapy and Occupational Therapy Practice: A Scoping Review of the Literature. BMC Health Serv. Res. 2017, 17, 375. [Google Scholar] [CrossRef]
- Peiris, C.L.; Taylor, N.F.; Shields, N. Patients Value Patient-Therapist Interactions More than the Amount or Content of Therapy during Inpatient Rehabilitation: A Qualitative Study. J. Physiother. 2012, 58, 261–268. [Google Scholar] [CrossRef]
- McCormack, B.; Karlsson, B.; Dewing, J.; Lerdal, A. Exploring Person-Centredness: A Qualitative Meta-Synthesis of Four Studies. Scand. J. Caring Sci. 2010, 24, 620–634. [Google Scholar] [CrossRef]
- Søgaard, M.B.; Andresen, K.; Kristiansen, M. Systematic Review of Patient-Engagement Interventions: Potentials for Enhancing Person-Centred Care for Older Patients with Multimorbidity. BMJ Open 2021, 11, e048558. [Google Scholar] [CrossRef] [PubMed]
- Bordin, E.S. The Generalizability of the Psychoanalytic Concept of the Working Alliance. Psychother. Theory Res. Pract. 1979, 16, 252–260. [Google Scholar] [CrossRef]
- Muran, J.C.; Barber, J.P. (Eds.) The Therapeutic Alliance: An Evidence-Based Guide to Practice; Guilford Press: New York, NY, USA, 2011; Volume 41. [Google Scholar] [CrossRef]
- Rønnestad, M.H.; Willutzki, U.; Tarragona, M.; David, E. Orlinsky: Developing Psychotherapy Research, Researching Psychotherapist Development. In Bringing Psychotherapy Research to Life: Understanding Change through the Work of Leading Clinical Researchers; American Psychological Association: Washington, DC, USA, 2010; pp. 233–243. ISBN 978-1-4338-0774-9. [Google Scholar]
- Flückiger, C.; Del Re, A.C.; Wampold, B.E.; Znoj, H.; Caspar, F.; Jörg, U. Valuing Clients’ Perspective and the Effects on the Therapeutic Alliance: A Randomized Controlled Study of an Adjunctive Instruction. J. Couns. Psychol. 2012, 59, 18–26. [Google Scholar] [CrossRef]
- Mohr, W.; Rädke, A.; Afi, A.; Edvardsson, D.; Mühlichen, F.; Platen, M.; Roes, M.; Michalowsky, B.; Hoffmann, W. Key Intervention Categories to Provide Person-Centered Dementia Care: A Systematic Review of Person-Centered Interventions. J. Alzheimer’s Dis. 2021, 84, 343–366. [Google Scholar] [CrossRef] [PubMed]
- Flückiger, C.; Del Re, A.C.; Wampold, B.E.; Horvath, A.O. The Alliance in Adult Psychotherapy: A Meta-Analytic Synthesis. Psychotherapy 2018, 55, 316–340. [Google Scholar] [CrossRef] [PubMed]
- Danzl, M.M.; Etter, N.M.; Andreatta, R.D.; Kitzman, P.H. Facilitating Neurorehabilitation through Principles of Engagement. J. Allied Health 2012, 41, 35–41. [Google Scholar]
- Deuschl, G.; Beghi, E.; Fazekas, F.; Varga, T.; Christoforidi, K.A.; Sipido, E.; Bassetti, C.L.; Vos, T.; Feigin, V.L. The Burden of Neurological Diseases in Europe: An Analysis for the Global Burden of Disease Study 2017. Lancet Public Health 2020, 5, E551–E567. [Google Scholar] [CrossRef]
- Béjot, Y.; Daubail, B.; Jacquin, A.; Durier, J.; Osseby, G.-V.; Rouaud, O.; Giroud, M. Trends in the Incidence of Ischaemic Stroke in Young Adults between 1985 and 2011: The Dijon Stroke Registry. J. Neurol. Neurosurg. Psychiatry 2014, 85, 509–513. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-Item Checklist for Interviews and Focus Groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Mudge, S.; Stretton, C.; Kayes, N. Are Physiotherapists Comfortable with Person-Centred Practice? An Autoethnographic Insight. Disabil. Rehabil. 2014, 36, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Lawton, M.; Sage, K.; Haddock, G.; Conroy, P.; Serrant, L. Speech and Language Therapists’ Perspectives of Therapeutic Alliance Construction and Maintenance in Aphasia Rehabilitation Post-Stroke. Int. J. Lang. Commun. Disord. 2018, 53, 550–563. [Google Scholar] [CrossRef]
- Hersh, D.; Wood, P.; Armstrong, E. Informal Aphasia Assessment, Interaction and the Development of the Therapeutic Relationship in the Early Period after Stroke. Aphasiology 2018, 32, 876–901. [Google Scholar] [CrossRef]
- Lawton, M.; Haddock, G.; Conroy, P. People with Aphasia’s Perception of the Therapeutic Alliance in Aphasia Rehabilitation Post Stroke: A Thematic Analysis. Aphasiology 2018, 32, 1397–1417. [Google Scholar] [CrossRef]
- Walder, K.; Molineux, M. Listening to the Client Voice—A Constructivist Grounded Theory Study of the Experiences of Client-Centred Practice after Stroke. Aust. Occup. Ther. J. 2020, 67, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Kayes, N.M.; Cummins, C.; McPherson, K.M.; Worrall, L.; Bright, F.A.S. Developing Connections for Engagement in Stroke Rehabilitation. Brain Impair. 2021, 23, 42–59. [Google Scholar] [CrossRef]
- Williams, L.M.; Douglas, J.M. It Takes Two to Tango: The Therapeutic Alliance in Community Brain Injury Rehabilitation. Brain Impair. 2021, 23, 24–41. [Google Scholar] [CrossRef]
- Gordon, C.; Ellis-Hill, C.; Dewar, B.; Watkins, C. Knowing-in-Action That Centres Humanising Relationships on Stroke Units: An Appreciative Action Research Study. Brain Impair. 2022, 23, 60–75. [Google Scholar] [CrossRef]
- Grohn, B.; Worrall, L.; Simmons-Mackie, N.; Hudson, K. Living Successfully with Aphasia during the First Year Post-Stroke: A Longitudinal Qualitative Study. Aphasiology 2014, 28, 1405–1425. [Google Scholar] [CrossRef]
- Pallesen, H. Body, Coping and Self-Identity. A Qualitative 5-Year Follow-up Study of Stroke. Disabil. Rehabil. 2014, 36, 232–241. [Google Scholar] [CrossRef] [PubMed]
- Kayes, N.M.; McPherson, K.M. Human Technologies in Rehabilitation: “Who” and “How” We Are with Our Clients. Disabil. Rehabil. 2012, 34, 1907–1911. [Google Scholar] [CrossRef]
- Andrew, N.E.; Kilkenny, M.; Naylor, R.; Purvis, T.; Lalor, E.; Moloczij, N.; Cadilhac, D.A. National Stroke Foundation Understanding Long-Term Unmet Needs in Australian Survivors of Stroke. Int. J. Stroke 2014, 9 (Suppl. A100), 106–112. [Google Scholar] [CrossRef] [PubMed]
- Besley, J.; Kayes, N.M.; McPherson, K.M. Assessing Therapeutic Relationships in Physiotherapy: Literature Review. New Zealand J. Physiother. 2011, 39, 81–91. [Google Scholar]
- Bright, F.A.S.; Kayes, N.M.; McCann, C.M.; McPherson, K.M. Understanding Hope after Stroke: A Systematic Review of the Literature Using Concept Analysis. Top. Stroke Rehabil. 2011, 18, 490–508. [Google Scholar] [CrossRef] [PubMed]
- Soundy, A.; Sayers, J.; Stubbs, B.; Roskell, C. Don’t Take My Hope Away: Understanding the Patient’s Hope Inneurological Rehabilitation. Int. J. Ther. Rehabil. 2014, 21, 257–258. [Google Scholar] [CrossRef]
- Lawton, M.; Haddock, G.; Conroy, P.; Sage, K. Therapeutic Alliances in Stroke Rehabilitation: A Meta-Ethnography. Arch. Phys. Med. Rehabil. 2016, 97, 1979–1993. [Google Scholar] [CrossRef] [PubMed]
- Foster, A.M.; Armstrong, J.; Buckley, A.; Sherry, J.; Young, T.; Foliaki, S.; James-Hohaia, T.M.; Theadom, A.; McPherson, K.M. Encouraging Family Engagement in the Rehabilitation Process: A Rehabilitation Provider’s Development of Support Strategies for Family Members of People with Traumatic Brain Injury. Disabil. Rehabil. 2012, 34, 1855–1862. [Google Scholar] [CrossRef]
- Lawton, M.; Conroy, P.; Sage, K.; Haddock, G. Aphasia and stroke therapeutic alliance measure (A-STAM): Development and preliminary psychometric evaluation. Int. J. Speech-Lang. Pathol. 2019, 21, 459–469. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).