Prognostic Implications of Physical Activity on Mortality from Ischaemic Heart Disease: Longitudinal Cohort Study Data
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Sociodemographic, Lifestyle Factors, and Psychological Well-Being
2.3. Objective Measurements
2.4. Statistical Analysis
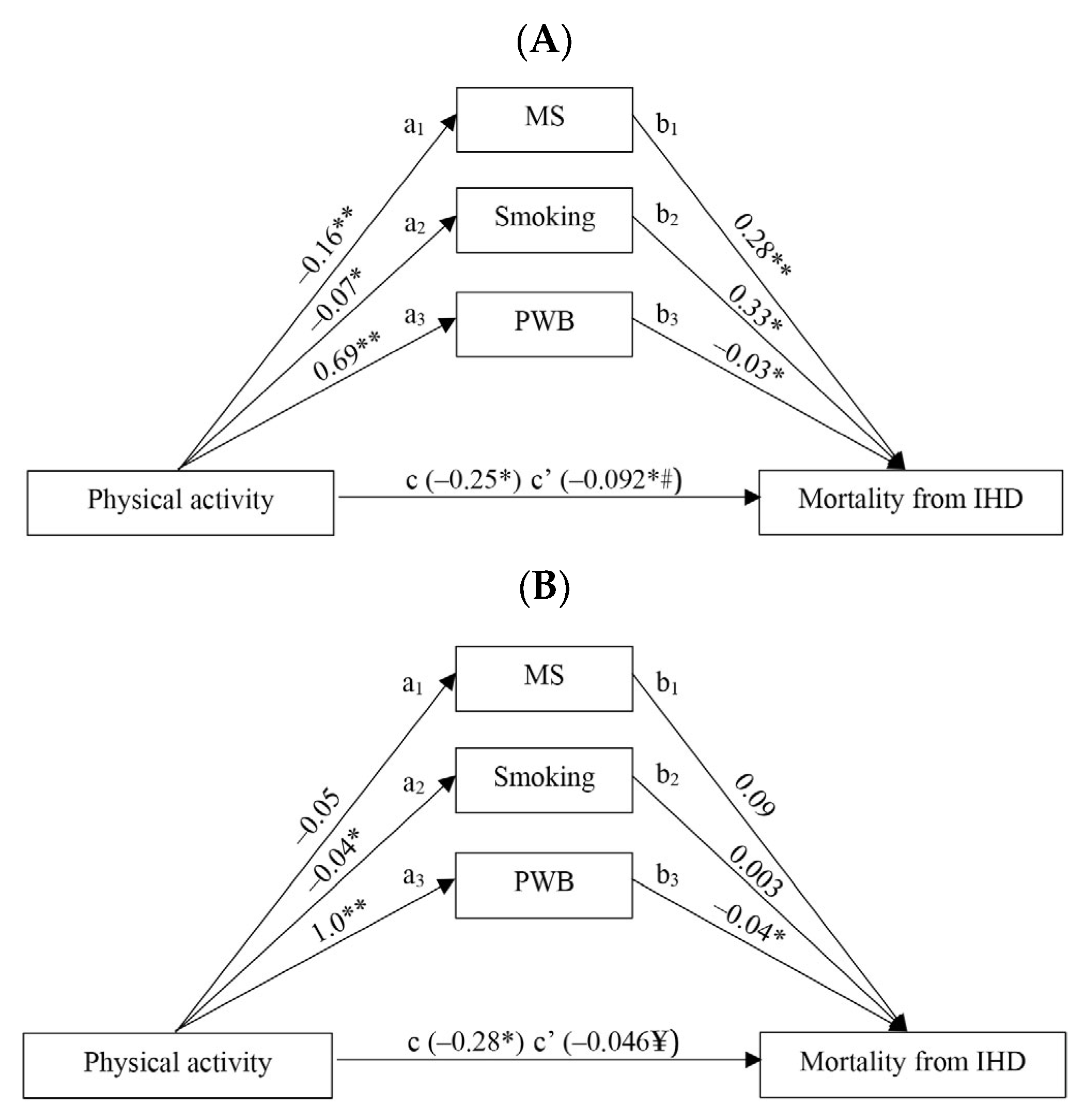
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Official Statistics Portal. The Population of Lithuania (Edition 2021). Causes of Death. Available online: https://osp.stat.gov.lt/lietuvos-gyventojai-2021/mirtingumas/gyventoju-mirties-priezastys (accessed on 10 March 2023).
- Timmis, A.; Vardas, P.; Townsend, N.; Torbica, A.; Katus, H.; De Smedt, D.; Gale, C.P.; Maggioni, A.P.; Petersen, S.E.; Huculeci, R.; et al. European Society of Cardiology: Cardiovascular disease statistics 2021. Eur. Heart J. 2022, 43, 716–799. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Physical Activity. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 16 March 2023).
- Saint-Maurice, P.F.; Coughlan, D.; Kelly, S.P.; Keadle, S.K.; Cook, M.B.; Carlson, S.A.; Fulton, J.E.; Matthews, C.E. Association of Leisure-Time Physical Activity Across the Adult Life Course with All-Cause and Cause-Specific Mortality. JAMA Netw. Open 2019, 2, e190355. [Google Scholar] [CrossRef] [PubMed]
- WHO. Guidelines on Physical Activity and Sedentary Behaviour. 2020. Available online: https://www.who.int/publications/i/item/9789240015128 (accessed on 20 February 2023).
- Notthoff, N.; Reisch, R.; Gerstorf, D. Individual Characteristics and Physical Activity in Older Adults: A Systematic Review. Gerontology 2017, 63, 443–459. [Google Scholar] [CrossRef] [PubMed]
- Van Uffelen, J.G.Z.; Khan, A.; Burton, N.W. Gender differences in physical activity motivators and context preferences: A population-based study in people in their sixties. BMC Public Health 2017, 17, 624. [Google Scholar] [CrossRef] [PubMed]
- Peasey, A.; Bobak, M.; Kubinova, R.; Malyutina, S.; Pajak, A.; Tamosiunas, A.; Pikhart, H.; Nicholson, A.; Marmot, M. Determinants of cardiovascular disease and other non-communicable diseases in Central and Eastern Europe: Rationale and design of the HAPIEE study. BMC Public Health 2006, 6, 255. [Google Scholar] [CrossRef]
- Sapranaviciute-Zabazlajeva, L.; Luksiene, D.; Virviciute, D.; Bobak, M.; Tamosiunas, A. Link between healthy lifestyle and psychological well-being in Lithuanian adults aged 45–72: A cross-sectional study. BMJ Open 2017, 7, e014240. [Google Scholar] [CrossRef]
- Hyde, M.; Wiggins, R.D.; Higgs, P.; Blane, D. A measure of quality of life in early old age: The theory, development and properties of a need’s satisfaction model (CASP-19). Aging Ment. Health 2003, 7, 186–194. [Google Scholar] [CrossRef]
- Norkus, A.; Ostrauskas, R.; Sulcaite, R.; Baranauskiene, E.; Baliutaviciene, D. Classification and diagnosis of diabetes mellitus (methodology recommendations). Lith. Endocrinol. 2000, 3, 234–241. [Google Scholar]
- Grundy, S.M. Third Report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3143–3421. [Google Scholar]
- Prineas, R.J.; Crow, R.S.; Blackburn, H.W. The Minnesota Code Manual of Electrocardiographic Findings: Standards and Procedures for Measurement and Classification; J. Wright: Boston, MA, USA, 1982; p. 229. [Google Scholar]
- Rose, G.A.; Blackburn, H.; Gillum, R.F. Cardiovascular Survey Methods; (Monograph Series); World Health Organization: Geneva, Switzerland, 1982; p. 56. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Little, T.D., Ed.; Guilford Press: New York, NY, USA, 2013; p. 507. [Google Scholar]
- World Health Organization (WHO). Global Action Plan on Physical Activity 2018–2030. Available online: https://apps.who.int/iris/bitstream/handle/10665/272722/9789241514187-eng.pdf (accessed on 20 February 2023).
- Geidl, W.; Schlesinger, S.; Mino, E.; Miranda, L.; Pfeifer, K. Dose-response relationship between physical activity and mortality in adults with noncommunicable diseases: A systematic review and meta-analysis of prospective observational studies. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 109. [Google Scholar] [CrossRef]
- Gitt, A.K.; Parhofer, K.G.; Laufs, U.; März, W.; Paar, W.D.; Bramlage, P.; Marx, N. Hypercholesterolemia diagnosis, treatment patterns and target achievement in patients with acute coronary syndromes in Germany. Clin. Res. Cardiol. 2023, 112, 299–311. [Google Scholar] [CrossRef] [PubMed]
- Imboden, M.T.; Harber, M.P.; Whaley, M.H.; Finch, W.H.; Bishop, D.L.; Kaminsky, L.A. Cardiorespiratory Fitness and Mortality in Healthy Men and Women. J. Am. Coll. Cardiol. 2018, 72, 2283–2292. [Google Scholar] [CrossRef] [PubMed]
- Kannel, W.B.; Sorlie, P. Some Health Benefits of Physical Activity: The Framingham Study. Arch. Intern. Med. 1979, 139, 857–861. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Siegrist, J. Physical activity and risk of cardiovascular disease—A meta-analysis of prospective cohort studies. Int. J. Environ. Res. Public Health 2012, 9, 391–407. [Google Scholar] [CrossRef]
- Kodama, S.; Saito, K.; Tanaka, S.; Maki, M.; Yachi, Y.; Asumi, M.; Sugawara, A.; Totsuka, K.; Shimano, H.; Ohashi, Y.; et al. Cardiorespiratory Fitness as a Quantitative Predictor of All-Cause Mortality and Cardiovascular Events in Healthy Men and Women: A Meta-analysis. JAMA 2009, 301, 2024–2035. [Google Scholar] [CrossRef]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef]
- Serrano-Sánchez, J.A.; Fernández-Rodríguez, M.J.; Sanchis-Moysi, J.; del Cristo Rodríguez-Pérez, M.; Marcelino-Rodríguez, I.; de León, A.C. Domain and intensity of physical activity are associated with metabolic syndrome: A population-based study. PLoS ONE 2019, 14, e0219798. [Google Scholar] [CrossRef]
- Gallardo-Alfaro, L.; Bibiloni, M.D.M.; Mateos, D.; Ugarriza, L.; Tur, J.A. Leisure-Time Physical Activity and Metabolic Syndrome in Older Adults. Int. J. Environ. Res. Public Health 2019, 16, 3358. [Google Scholar] [CrossRef]
- Gallardo-Alfaro, L.; Bibiloni, M.; Bouzas, C.; Mascaró, C.M.; Martínez-González, M.Á.; Salas-Salvadó, J.; Corella, D.; Schröder, H.; Alfredo Martínez, J.A.; Alonso-Gómez, A.M.; et al. Physical activity and metabolic syndrome severity among older adults at cardiovascular risk: 1-Year trends. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2870–2886. [Google Scholar] [CrossRef]
- Gallardo-Alfaro, L.; Bibiloni, M.D.M.; Mascaró, C.M.; Montemayor, S.; Ruiz-Canela, M.; Salas-Salvadó, J.; Corella, D.; Fitó, M.; Romaguera, D.; Vioque, J.; et al. Leisure-Time Physical Activity, Sedentary Behaviour and Diet Quality are Associated with Metabolic Syndrome Severity: The PREDIMED-Plus Study. Nutrients 2020, 12, 1013. [Google Scholar] [CrossRef]
- Sagawa, N.; Rockette-Wagner, B.; Azuma, K.; Ueshima, H.; Hisamatsu, T.; Takamiya, T.; El-Saed, A.; Miura, K.; Kriska, A.; Sekikawa, A. Physical activity levels in American and Japanese men from the ERA-JUMP Study and associations with metabolic syndrome. J. Sport Heal. Sci. 2020, 9, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Uemura, H.; Katsuura-Kamano, S.; Iwasaki, Y.; Arisawa, K.; Hishida, A.; Okada, R.; Tamura, T.; Kubo, Y.; Ito, H.; Oze, I.; et al. Independent relationships of daily life activity and leisure-time exercise with metabolic syndrome and its traits in the general Japanese population. Endocrine 2019, 64, 552–563. [Google Scholar] [CrossRef]
- Morseth, B.; Jacobsen, B.K.; Emaus, N.; Wilsgaard, T.; Jørgensen, L. Secular trends and correlates of physical activity: The Tromsø Study 1979–2008. BMC Public Health 2016, 16, 1215. [Google Scholar] [CrossRef] [PubMed]
- Lounassalo, I.; Hirvensalo, M.; Palomäki, S.; Salin, K.; Tolvanen, A.; Pahkala, K.; Rovio, S.; Fogelholm, M.; Yang, X.; Hutri-Kähönen, N.; et al. Life-course leisure-time physical activity trajectories in relation to health-related behaviors in adulthood: The Cardiovascular Risk in Young Finns study. BMC Public Health 2021, 21, 533. [Google Scholar] [CrossRef] [PubMed]
- Salin, K.; Kankaanpää, A.; Hirvensalo, M.; Lounassalo, I.; Yang, X.; Magnussen, C.G.; Hutri-Kähönen, N.; Rovio, S.; Viikari, J.; Raitakari, O.T.; et al. Smoking and physical activity trajectories from childhood to midlife. Int. J. Environ. Res. Public Health 2019, 16, 974. [Google Scholar] [CrossRef] [PubMed]
- Min, S.; Masanovic, B.; Bu, T.; Matic, R.M.; Vasiljevic, I.; Vukotic, M.; Li, J.; Vukovic, J.; Fu, T.; Jabucanin, B.; et al. The Association Between Regular Physical Exercise, Sleep Patterns, Fasting, and Autophagy for Healthy Longevity and Well-Being: A Narrative Review. Front. Psychol. Sec. Health Psychol. 2021, 12, 803421. [Google Scholar] [CrossRef]
| Physical Activity Levels/Tertiles | Min–Max * | Mean (SD) |
|---|---|---|
| MEN | ||
| Physically inactive (1st tertile) | 0.0–10.0 | 5.8 (3.1) |
| Moderately physically active (2nd tertile) | 10.5–19.5 | 14.7 (2.6) |
| Higher physically active (3rd tertile) | 20.0–42.0 | 26.8 (5.9) |
| WOMEN | ||
| Physically inactive (1st tertile) | 0.0–13.5 | 8.6 (3.4) |
| Moderately physically active (2nd tertile) | 14.0–22.0 | 17.5 (2.6) |
| Higher physically active (3rd tertile) | 22.5–42.0 | 29.2 (5.1) |
| ALL | ||
| Physically inactive (1st tertile) | 0.0–12.0 | 7.2 (3.4) |
| Moderately physically active (2nd tertile) | 12.5–20.5 | 16.2 (2.4) |
| Higher physically active (3rd tertile) | 21.0–42.0 | 28.1 (5.7) |
| 22.5–42.0 | 29.2 (5.1) |
| Variables | MEN n = 3065 | WOMEN n = 3705 | p |
|---|---|---|---|
| Age, years, mean ± SD Education, % Secondary and lower | 57.3 ± 7.87 | 57.1 ± 7.84 | 0.217 |
| <0.001 | |||
| 46.8 | 37.5 | ||
| College and higher Metabolic syndrome, % | 53.2 | 62.5 | |
| 27.5 | 33.8 | <0.001 | |
| Elevated arterial blood pressure (≥130/85 mm/Hg), % Increased waist circumference, % Men ≥ 102 cm, women ≥ 88 cm HDL cholesterol, | 83.4 | 69.7 | <0.001 |
| 27.3 | 48.6 | <0.001 | |
| Men < 1.0 mmol/L, women < 1.3 mmol/L, % | 12.1 | 23.2 | <0.001 |
| Triglycerides ≥ 1.7 mmol/L, % | 28.3 | 25.0 | 0.001 |
| Fasting glucose ≥ 6.1 mmol/L, % | 30.8 | 30.9 | 0.475 |
| Psychological well-being groups | 0.004 | ||
| Higher | 52.8 | 56.3 | |
| Lower | 47.2 | 43.7 | |
| Regular smoking, % | 37.7 | 13.6 | <0.001 |
| Nutrition habits, % | |||
| More frequent consumption of fresh fruit and vegetables | 51.1 | 59.4 | <0.001 |
| More frequent consumption of sweets | 51.4 | 48.9 | 0.020 |
| More frequent consumption of cereals, and infrequent consumption of meat | 32.7 | 58.0 | <0.001 |
| More frequent consumption of meat, potatoes, and eggs | 61.4 | 42.6 | <0.001 |
| More frequent consumption of chicken and fish | 55.4 | 49.3 | <0.001 |
| Physical activity (hours/week), mean ± SD | 15.3 ± 9.39 | 18.2 ± 8.96 | 0.024 |
| Prevalence of IHD at baseline survey, % | 21.0 | 22.3 | 0.197 |
| IHD Status | ||||
|---|---|---|---|---|
| Without IHD HR (95 % CI) | p | With IHD HR (95 % CI) | p | |
| MEN | n = 2422 | n = 643 | ||
| Physically inactive | 1 | 1 | ||
| Moderately physically active | 0.54 (0.33–0.89) | 0.016 | 0.69 (0.43–1.10) | 0.121 |
| Higher physically active | 0.60 (0.37–0.95) | 0.031 | 0.54 (0.32–0.91) | 0.021 |
| WOMEN | n = 2877 | n = 828 | ||
| Physically inactive | 1 | 1 | ||
| Moderately physically active | 0.75 (0.40–1.39) | 0.354 | 0.41 (0.19–0.89) | 0.025 |
| Higher physically active | 0.73 (0.38–1.38) | 0.331 | 0.54 (0.25–1.18) | 0.123 |
| ALL | n = 5299 | n = 1471 | ||
| Physically inactive | 1 | 1 | ||
| Moderately physically active | 0.63 (0.43–0.92) | 0.017 | 0.54 (0.37–0.81) | 0.003 |
| Higher physically active | 0.56 (0.39–0.82) | 0.003 | 0.48 (0.31–0.74) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luksiene, D.; Jasiukaitiene, V.; Radisauskas, R.; Tamosiunas, A.; Bobak, M. Prognostic Implications of Physical Activity on Mortality from Ischaemic Heart Disease: Longitudinal Cohort Study Data. J. Clin. Med. 2023, 12, 4218. https://doi.org/10.3390/jcm12134218
Luksiene D, Jasiukaitiene V, Radisauskas R, Tamosiunas A, Bobak M. Prognostic Implications of Physical Activity on Mortality from Ischaemic Heart Disease: Longitudinal Cohort Study Data. Journal of Clinical Medicine. 2023; 12(13):4218. https://doi.org/10.3390/jcm12134218
Chicago/Turabian StyleLuksiene, Dalia, Vilma Jasiukaitiene, Ricardas Radisauskas, Abdonas Tamosiunas, and Martin Bobak. 2023. "Prognostic Implications of Physical Activity on Mortality from Ischaemic Heart Disease: Longitudinal Cohort Study Data" Journal of Clinical Medicine 12, no. 13: 4218. https://doi.org/10.3390/jcm12134218
APA StyleLuksiene, D., Jasiukaitiene, V., Radisauskas, R., Tamosiunas, A., & Bobak, M. (2023). Prognostic Implications of Physical Activity on Mortality from Ischaemic Heart Disease: Longitudinal Cohort Study Data. Journal of Clinical Medicine, 12(13), 4218. https://doi.org/10.3390/jcm12134218







