Varicocele: To Treat or Not to Treat?
Abstract
:1. Introduction
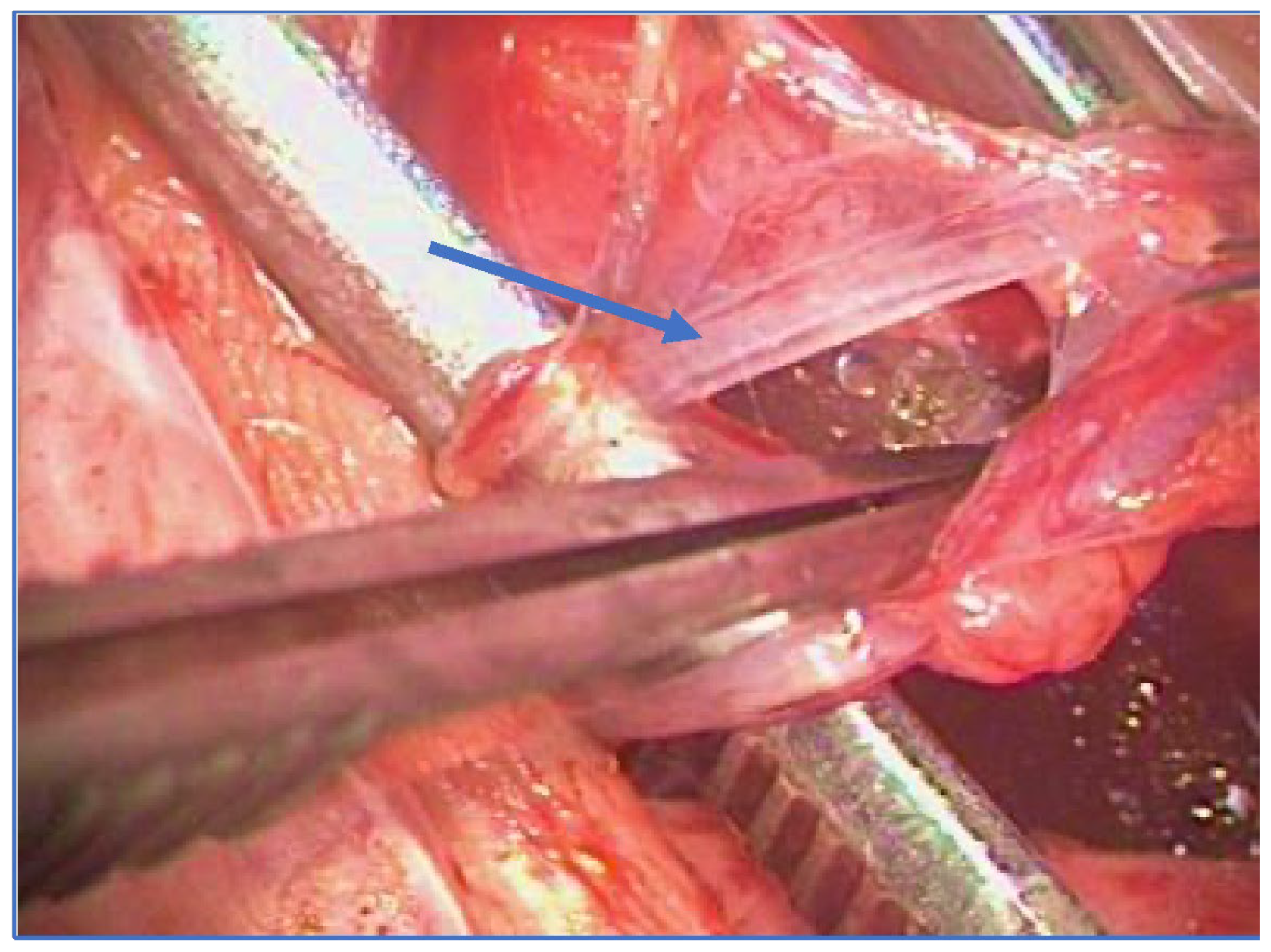
2. Surgical Treatment
- Retrograde sclero-embolization, trans-femoral or trans-brachial;
- Antegrade sclerotherapy (Tauber technique) [16].
- Retroperitoneal;
- Inguinal;
- Sub-inguinal.
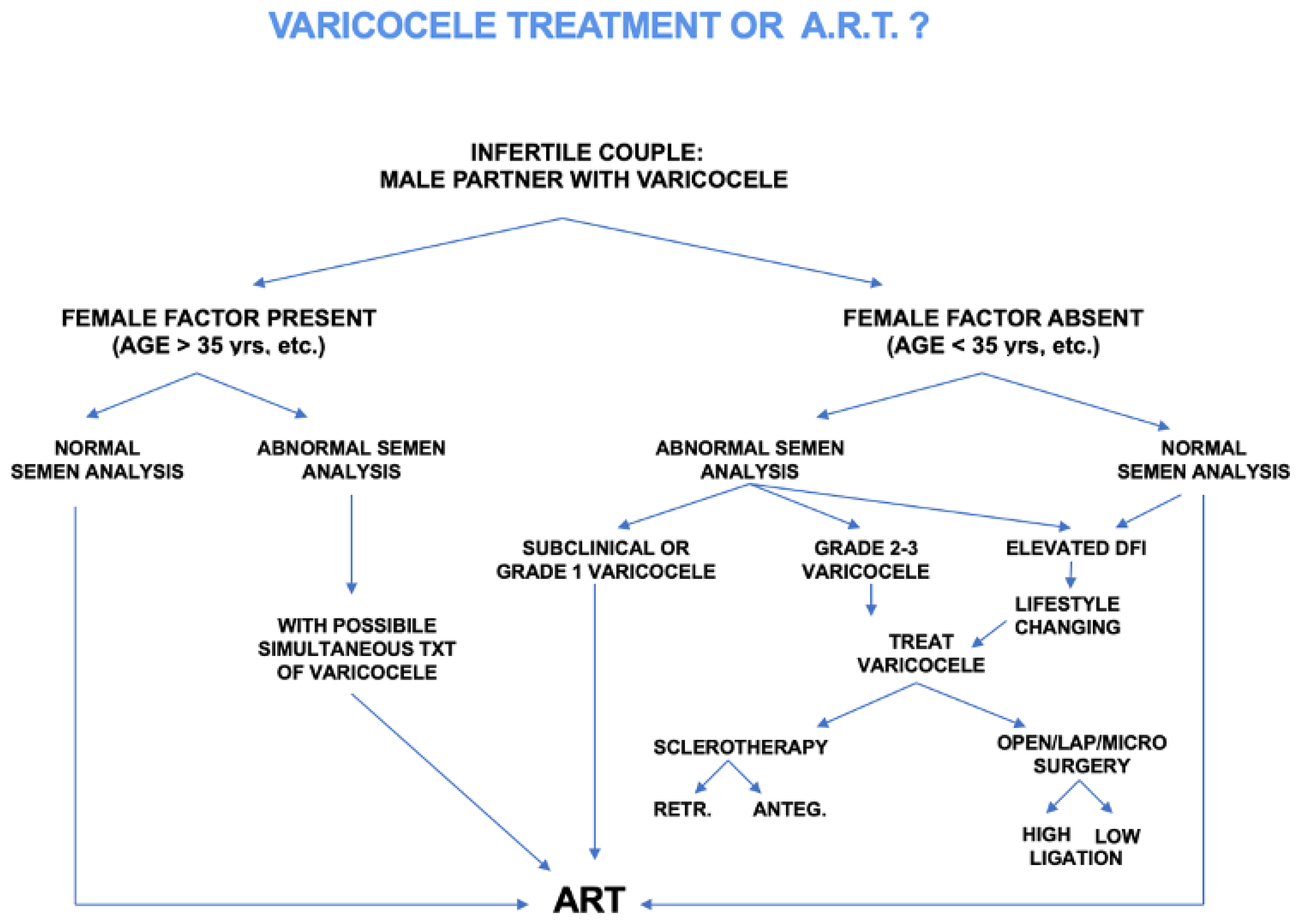
3. Varicocelectomy Indications
- VR in children and adolescents;
- VR in infertile couples, oligoasthenoteratozoospermia and sperm DNA fragmentation;
- VR in azoospermia;
- VR prior to assisted reproductive techniques (ART);
- VR in subclinical varicocele;
- VR in bilateral varicocele.
3.1. Role of Varicocelectomy in Children and Adolescents
3.2. Role of Varicocelectomy in Infertile Couples, OAT and DNA Fragmentation
3.3. Role of Varicocelectomy in Azoospermia
3.4. Role of Varicocelectomy Prior to ART
3.5. Role of Varicocelectomy in Subclinical Varicocele
3.6. Role of Varicocelectomy in Bilateral Varicocele
| Technique | Pros | Cons |
|---|---|---|
| Open retroperitoneal high ligation (Palomo) [23,33,48,83] | Complete ligation | General anesthesia, Higher hydrocele risk |
| Microsurgical lymphatic sparing Palomo [13,17,18,19,20] | Complete ligation Lower hydrocele risk | General anesthesia Access to operating microscope |
| Microsurgical subinguinal or inguinal surgery [23,28,33] | Less invasive (local anesthesia) Lower recurrence rate Lower hydrocele risk | Access to operating microscope Longer surgical time |
| Laparoscopic surgery [23,32,33] | Bilateral varicocele Higher magnification Lower recurrence rate | High costs More invasive (intraperitoneal) General anesthesia |
| Sclero-embolization [15,16,23,24,25,26,48] | Minimally invasive Short time Outpatient | Limited applicability Higher recurrence rate Radiation exposure |
4. Summary
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Franco, G.; Iori, F.; De Dominicis, C.; Dal Forno, S.; Mander, A.; Laurenti, C. Challenging the Role of Cremasteric Reflux in the Pathogenesis of Varicocele Using a New Venographic Approach. J. Urol. 1999, 161, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Alsaikhan, B.; Alrabeeah, K.; Delouya, G.; Zini, A. Epidemiology of Varicocele. Asian J. Androl. 2016, 18, 179. [Google Scholar] [PubMed]
- Dubin, L.; Amelar, R.D. Varicocele Size and Results of Varicocelectomy in Selected Subfertile Men with Varicocele. Fertil. Steril. 1970, 21, 606–609. [Google Scholar] [CrossRef]
- Freeman, S.; Bertolotto, M.; Richenberg, J.; Belfield, J.; Dogra, V.; Huang, D.Y.; Lotti, F.; Markiet, K.; Nikolic, O.; Ramanathan, S.; et al. Ultrasound Evaluation of Varicoceles: Guidelines and Recommendations of the European Society of Urogenital Radiology Scrotal and Penile Imaging Working Group (ESUR-SPIWG) for Detection, Classification, and Grading. Eur. Radiol. 2020, 30, 11–25. [Google Scholar] [CrossRef]
- WHO Manual for the Standardized Investigation and Diagnosis of the Infertile Male. Available online: https://www.who.int/publications/i/item/9780521774741 (accessed on 15 May 2023).
- Sarteschi, L.; Paoli, R.; Bianchini, M.; Menchini Fabris, G. Lo Studio Del Varicocele Con Eco-Color-Doppler. G Ital. Ultrasonol. 1993, 4, 43–49. [Google Scholar]
- Cavallini, G.; Scroppo, F.I.; Colpi, G.M. The Clinical Usefulness of a Novel Grading System for Varicocoeles Using Duplex Doppler Ultrasound Examination Based on Postsurgical Modifications of Seminal Parameters. Andrology 2019, 7, 62–68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schlegel, P.N.; Sigman, M.; Collura, B.; De Jonge, C.J.; Eisenberg, M.L.; Lamb, D.J.; Mulhall, J.P.; Niederberger, C.; Sandlow, J.I.; Sokol, R.Z.; et al. Diagnosis and Treatment of Infertility in Men: AUA/ASRM Guideline Part I. Fertil. Steril. 2021, 115, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Minhas, S.; Bettocchi, C.; Boeri, L.; Capogrosso, P.; Carvalho, J.; Cilesiz, N.C.; Cocci, A.; Corona, G.; Dimitropoulos, K.; Gül, M.; et al. European Association of Urology Guidelines on Male Sexual and Reproductive Health: 2021 Update on Male Infertility. Eur. Urol. 2021, 80, 603–620. [Google Scholar] [CrossRef]
- Su, J.S.; Farber, N.J.; Vij, S.C. Pathophysiology and Treatment Options of Varicocele: An Overview. Andrologia 2021, 53, e13576. [Google Scholar] [CrossRef]
- Dieamant, F.; Petersen, C.G.; Mauri, A.L.; Conmar, V.; Mattila, M.; Vagnini, L.D.; Renzi, A.; Costa, B.P.; Zamara, C.; Oliveira, J.B.A.; et al. Semen Parameters in Men with Varicocele: DNA Fragmentation, Chromatin Packaging, Mitochondrial Membrane Potential, and Apoptosis. JBRA Assist. Reprod. 2017, 21, 295–301. [Google Scholar] [CrossRef] [Green Version]
- Franco, G.; Misuraca, L.; Ciletti, M.; Leonardo, C.; De Nunzio, C.; Palminteri, E.; De Dominicis, C. Surgery of Male Infertility: An Update. Urologia 2014, 81, 154–164. [Google Scholar] [CrossRef]
- Agarwal, A.; Cannarella, R.; Saleh, R.; Boitrelle, F.; Gül, M.; Toprak, T.; Salvio, G.; Arafa, M.; Russo, G.I.; Harraz, A.M.; et al. Impact of Varicocele Repair on Semen Parameters in Infertile Men: A Systematic Review and Meta-Analysis. World J. Men’s Health 2023, 41, 220142. [Google Scholar] [CrossRef]
- Crestani, A.; Giannarini, G.; Calandriello, M.; Rossanese, M.; Mancini, M.; Novara, G.; Ficarra, V. Antegrade Scrotal Sclerotherapy of Internal Spermatic Veins for Varicocele Treatment: Technique, Complications, and Results. Asian J. Androl. 2016, 18, 292–295. [Google Scholar] [CrossRef]
- Matsuda, T.; Horii, Y.; Yoshida, O. Should the Testicular Artery Be Preserved at Varicocelectomy? J. Urol. 1993, 149, 1357–1360. [Google Scholar] [CrossRef]
- Ferro, F.; Gentile, V. Il Varicocele in Età Pediatrica Ed Adolescenziale. In Varicocele e Infertilità Maschile; Flati, G., Gentile, V., Lenzi, A., Eds.; SEU: Rome, Italy, 2006. [Google Scholar]
- Riccabona, M.; Oswald, J.; Koen, M.; Lusuardi, L.; Radmayr, C.; Bartsch, G. Optimizing the Operative Treatment of Boys with Varicocele: Sequential Comparison of 4 Techniques. J. Urol. 2003, 169, 666–668. [Google Scholar] [CrossRef] [PubMed]
- Silveri, M.; Bassani, F.; Adorisio, O. Changing Concepts in Microsurgical Pediatric Varicocelectomy: Is Retroperitoneal Approach Better than Subinguinal One? Urol. J. 2015, 12, 2032–2035. [Google Scholar] [PubMed]
- Zhang, H.; Li, H.; Hou, Y.; Jin, J.; Gu, X.; Zhang, M.; Huo, W.; Li, H. Microscopic Retroperitoneal Varicocelectomy with Artery and Lymphatic Sparing: An Alternative Treatment for Varicocele in Infertile Men. Urology 2015, 86, 511–515. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.F.; Bagley, F.H. An Abdominal Extraperitoneal Approach for the Difficult Orchidopexy. Br. J. Surg. 1979, 66, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Kroese, A.C.; de Lange, N.M.; Collins, J.; Evers, J.L. Surgery or Embolization for Varicoceles in Subfertile Men. Cochrane Database Syst. Rev. 2012, 10, 67. [Google Scholar] [CrossRef] [Green Version]
- Çayan, S.; Shavakhabov, S.; Kadioǧlu, A. Treatment of Palpable Varicocele in Infertile Men: A Meta-Analysis to Define the Best Technique. J. Androl. 2009, 30, 33–40. [Google Scholar] [CrossRef]
- Makris, G.C.; Efthymiou, E.; Little, M.; Boardman, P.; Anthony, S.; Uberoi, R.; Tapping, C. Safety and Effectiveness of the Different Types of Embolic Materials for the Treatment of Testicular Varicoceles: A Systematic Review. Br. J. Radiol. 2018, 91, 20170445. [Google Scholar] [CrossRef]
- Halpern, J.; Mittal, S.; Pereira, K.; Bhatia, S.; Ramasamy, R. Percutaneous Embolization of Varicocele: Technique, Indications, Relative Contraindications, and Complications. Asian J. Androl. 2016, 18, 234–238. [Google Scholar] [CrossRef]
- Bebi, C.; Bilato, M.; Minoli, D.G.; De Marco, E.A.; Gnech, M.; Paraboschi, I.; Boeri, L.; Fulgheri, I.; Brambilla, R.; Campoleoni, M.; et al. Radiation Exposure and Surgical Outcomes after Antegrade Sclerotherapy for the Treatment of Varicocele in the Paediatric Population: A Single Centre Experience. J. Clin. Med. 2023, 12, 755. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, M.; Gilbert, B.R.; Dicker, A.P.; Dwosh, J.; Gnecco, C. Microsurgical Inguinal Varicocelectomy with Delivery of the Testis: An Artery and Lymphatic Sparing Technique. J. Urol. 1992, 148, 1808–1811. [Google Scholar] [CrossRef]
- Marmar, J.L.; DeBenedictis, T.J.; Praiss, D. The Management of Varicoceles by Microdissection of the Spermatic Cord at the External Inguinal Ring. Fertil. Steril. 1985, 43, 583–588. [Google Scholar] [CrossRef]
- Colpi, G.M.; Carmignani, L.; Nerva, F.; Piediferro, G.; Castiglioni, F.; Grugnetti, C.; Galasso, G. Surgical Treatment of Varicocele by a Subinguinal Approach Combined with Antegrade Intraoperative Sclerotherapy of Venous Vessels. BJU Int. 2006, 97, 142–145. [Google Scholar] [CrossRef] [Green Version]
- Practice Committee of the American Society for Reproductive Medicine. Report on Varicocele and Infertility. Fertil. Steril. 2008, 90, S247–S249. [Google Scholar] [CrossRef] [PubMed]
- Mehta, A.; Goldstein, M. Microsurgical Varicocelectomy: A Review. Asian J. Androl. 2013, 15, 56–60. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.; Ji, Z.G. Microsurgery Versus Laparoscopic Surgery for Varicocele: A Meta-Analysis and Systematic Review of Randomized Controlled Trials. J. Investig. Surg. 2020, 33, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Al-Kandari, A.M.; Shabaan, H.; Ibrahim, H.M.; Elshebiny, Y.H.; Shokeir, A.A. Comparison of Outcomes of Different Varicocelectomy Techniques: Open Inguinal, Laparoscopic, and Subinguinal Microscopic Varicocelectomy: A Randomized Clinical Trial. Urology 2007, 69, 417–420. [Google Scholar] [CrossRef]
- Evers, J.L.H.; Collins, J.; Clarke, J. Surgery or Embolisation for Varicoceles in Subfertile Men. Cochrane Database Syst. Rev. 2009, 10, CD000479, Update in: Cochrane Database Syst. Rev. 2012, 10, CD000479. [Google Scholar] [CrossRef] [Green Version]
- Evers, J.L.H.; Collins, J.A. Assessment of Efficacy of Varicocele Repair for Male Subfertility: A Systematic Review. Lancet 2003, 361, 1849–1852. [Google Scholar] [CrossRef]
- Abdel-Meguid, T.A.; Al-Sayyad, A.; Tayib, A.; Farsi, H.M. Does Varicocele Repair Improve Male Infertility? An Evidence-Based Perspective from a Randomized, Controlled Trial. Eur. Urol. 2011, 59, 455–461. [Google Scholar] [CrossRef]
- Shah, R.; Agarwal, A.; Kavoussi, P.; Rambhatla, A.; Saleh, R.; Cannarella, R.; Harraz, A.M.; Boitrelle, F.; Kuroda, S.; Hamoda, T.A.A.A.M.; et al. Consensus and Diversity in the Management of Varicocele for Male Infertility: Results of a Global Practice Survey and Comparison with Guidelines and Recommendations. World J. Men’s Health 2023, 41, 164. [Google Scholar] [CrossRef] [PubMed]
- Takihara, H.; Sakatoku, J.; Cockett, A.T.K. The Pathophysiology of Varicocele in Male Infertility. Fertil. Steril. 1991, 55, 861–868. [Google Scholar] [CrossRef] [PubMed]
- Çayan, S.; Woodhouse, C.R.J. The Treatment of Adolescents Presenting with a Varicocele. BJU Int. 2007, 100, 744–747. [Google Scholar] [CrossRef] [PubMed]
- Çayan, S.; Şahin, S.; Akbay, E. Paternity Rates and Time to Conception in Adolescents with Varicocele Undergoing Microsurgical Varicocele Repair vs Observation Only: A Single Institution Experience with 408 Patients. J. Urol. 2017, 198, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Silay, M.S.; Hoen, L.; Quadackaers, J.; Undre, S.; Bogaert, G.; Dogan, H.S.; Kocvara, R.; Nijman, R.J.M.; Radmayr, C.; Tekgul, S.; et al. Treatment of Varicocele in Children and Adolescents: A Systematic Review and Meta-Analysis from the European Association of Urology/European Society for Paediatric Urology Guidelines Panel. Eur. Urol. 2019, 75, 448–461. [Google Scholar] [CrossRef] [PubMed]
- Elder, J. Does the Evidence Support Adolescent Varicocelectomy? Eur. Urol. 2019, 75, 462–463. [Google Scholar] [CrossRef]
- Lacerda, J.I.; Del Giudice, P.T.; Da Silva, B.F.; Nichi, M.; Fariello, R.M.; Fraietta, R.; Restelli, A.E.; Blumer, C.G.; Bertolla, R.P.; Cedenho, A.P. Adolescent Varicocele: Improved Sperm Function after Varicocelectomy. Fertil. Steril. 2011, 95, 994–999. [Google Scholar] [CrossRef]
- Cannarella, R.; Calogero, A.E.; Condorelli, R.A.; Giacone, F.; Aversa, A.; La Vignera, S. Management and Treatment of Varicocele in Children and Adolescents: An Endocrinologic Perspective. J. Clin. Med. 2019, 8, 1410. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baazeem, A.; Belzile, E.; Ciampi, A.; Dohle, G.; Jarvi, K.; Salonia, A.; Weidner, W.; Zini, A. Varicocele and Male Factor Infertility Treatment: A New Meta-Analysis and Review of the Role of Varicocele Repair. Eur. Urol. 2011, 60, 796–808. [Google Scholar] [CrossRef] [PubMed]
- Kroese, A.C.J.; Lange, N.M.D.; Collins, J.A.; Evers, J.L.H. Varicocele Surgery, New Evidence. Hum. Reprod. Update 2013, 19, 317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marmar, J.L.; Agarwal, A.; Prabakaran, S.; Agarwal, R.; Short, R.A.; Benoff, S.; Thomas, A.J. Reassessing the Value of Varicocelectomy as a Treatment for Male Subfertility with a New Meta-Analysis. Fertil. Steril. 2007, 88, 639–648. [Google Scholar] [CrossRef]
- Persad, E.; O’Loughlin, C.A.A.; Kaur, S.; Wagner, G.; Matyas, N.; Hassler-Di Fratta, M.R.; Nussbaumer-Streit, B. Surgical or Radiological Treatment for Varicoceles in Subfertile Men. Cochrane Database Syst. Rev. 2021, 4, CD000479. [Google Scholar] [CrossRef] [PubMed]
- Lara-Cerrillo, S.; Gual-Frau, J.; Benet, J.; Abad, C.; Prats, J.; Amengual, M.J.; Ribas-Maynou, J.; García-Peiró, A. Microsurgical Varicocelectomy Effect on Sperm Telomere Length, DNA Fragmentation and Seminal Parameters. Hum. Fertil. 2022, 25, 135–141. [Google Scholar] [CrossRef]
- Lira Neto, F.T.; Roque, M.; Esteves, S.C. Effect of Varicocelectomy on Sperm Deoxyribonucleic Acid Fragmentation Rates in Infertile Men with Clinical Varicocele: A Systematic Review and Meta-Analysis. Fertil. Steril. 2021, 116, 696–712. [Google Scholar] [CrossRef]
- Ribas-Maynou, J.; Yeste, M.; Becerra-Tomás, N.; Aston, K.I.; James, E.R.; Salas-Huetos, A. Clinical Implications of Sperm DNA Damage in IVF and ICSI: Updated Systematic Review and Meta-Analysis. Biol. Rev. Camb. Philos. Soc. 2021, 96, 1284–1300. [Google Scholar] [CrossRef]
- Qiu, D.; Shi, Q.; Pan, L. Efficacy of Varicocelectomy for Sperm DNA Integrity Improvement: A Meta-Analysis. Andrologia 2021, 53, e13885. [Google Scholar] [CrossRef]
- Yan, S.; Shabbir, M.; Yap, T.; Homa, S.; Ramsay, J.; McEleny, K.; Minhas, S. Should the Current Guidelines for the Treatment of Varicoceles in Infertile Men Be Re-Evaluated? Hum. Fertil. 2021, 24, 78–92. [Google Scholar] [CrossRef]
- Jayasena, C.N.; Radia, U.K.; Figueiredo, M.; Revill, L.F.; Dimakopoulou, A.; Osagie, M.; Vessey, W.; Regan, L.; Rai, R.; Dhillo, W.S. Reduced Testicular Steroidogenesis and Increased Semen Oxidative Stress in Male Partners as Novel Markers of Recurrent Miscarriage. Clin. Chem. 2019, 65, 161–169. [Google Scholar] [CrossRef] [Green Version]
- Negri, L.; Levi-Setti, P.E. Pregnancy Rate after Varicocele Repair: How Many Miscarriages? J. Androl. 2011, 32, 1. [Google Scholar] [CrossRef]
- Ghanaie, M.M.; Asgari, S.A.; Dadrass, N.; Allahkhah, A.; Iran-Pour, E.; Safarinejad, M.R. Effects of Varicocele Repair on Spontaneous First Trimester Miscarriage: A Randomized Clinical Trial. Urol. J. 2012, 9, 505–513. [Google Scholar]
- Farkouh, A.; Agarwal, A.; Hamoda, T.A.-A.A.-M.; Kavoussi, P.; Saleh, R.; Zini, A.; Arafa, M.; Harraz, A.M.; Gul, M.; Karthikeyan, V.S.; et al. Controversy and Consensus on the Management of Elevated Sperm DNA Fragmentation in Male Infertility: A Global Survey, Current Guidelines, and Expert Recommendations. World J. Men’s Health 2023, 41, e48. [Google Scholar] [CrossRef] [PubMed]
- Lipshultz, L.I.; Corriere, J.N. Progressive Testicular Atrophy in the Varicocele Patient. J. Urol. 1977, 117, 175–176. [Google Scholar] [CrossRef]
- Fırat, F.; Erdemir, F. The Effect of Age on Semen Quality and Spontaneous Pregnancy Rates in Patients Who Treated with Microsurgical Inguinal Varicocelectomy. Cureus 2020, 12, e7744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsiao, W.; Rosoff, J.S.; Pale, J.R.; Greenwood, E.A.; Goldstein, M. Older Age Is Associated with Similar Improvements in Semen Parameters and Testosterone after Subinguinal Microsurgical Varicocelectomy. J. Urol. 2011, 185, 620–625. [Google Scholar] [CrossRef] [PubMed]
- Esteves, S.C.; Miyaoka, R.; Roque, M.; Agarwal, A. Outcome of Varicocele Repair in Men with Nonobstructive Azoospermia: Systematic Review and Meta-Analysis. Asian J. Androl. 2016, 18, 246–253. [Google Scholar] [CrossRef]
- Berookhim, B.M.; Schlegel, P.N. Azoospermia Due to Spermatogenic Failure. Urol. Clin. N. Am. 2014, 41, 97–113. [Google Scholar] [CrossRef]
- Abdel-Meguid, T.A. Predictors of Sperm Recovery and Azoospermia Relapse in Men with Nonobstructive Azoospermia after Varicocele Repair. J. Urol. 2012, 187, 222–226. [Google Scholar] [CrossRef]
- Lee, J.S.; Park, H.J.; Seo, J.T. What Is the Indication of Varicocelectomy in Men with Nonobstructive Azoospermia? Urology 2007, 69, 352–355. [Google Scholar] [CrossRef] [PubMed]
- Elzanaty, S. Varicocele Repair in Non-Obstructive Azoospermic Men: Diagnostic Value of Testicular Biopsy—A Meta-Analysis. Scand. J. Urol. 2014, 48, 494–498. [Google Scholar] [CrossRef]
- Agarwal, A.; Deepinder, F.; Cocuzza, M.; Agarwal, R.; Short, R.A.; Sabanegh, E.; Marmar, J.L. Efficacy of Varicocelectomy in Improving Semen Parameters: New Meta-Analytical Approach. Urology 2007, 70, 532–538. [Google Scholar] [CrossRef]
- Esteves, S.C.; Roque, M.; Agarwal, A. Outcome of Assisted Reproductive Technology in Men with Treated and Untreated Varicocele: Systematic Review and Meta-Analysis. Asian J. Androl. 2016, 18, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Kirby, E.W.; Wiener, L.E.; Rajanahally, S.; Crowell, K.; Coward, R.M. Undergoing Varicocele Repair before Assisted Reproduction Improves Pregnancy Rate and Live Birth Rate in Azoospermic and Oligospermic Men with a Varicocele: A Systematic Review and Meta-Analysis. Fertil. Steril. 2016, 106, 1338–1343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghayda, R.A.; El-Doueihi, R.Z.; Lee, J.Y.; Bulbul, M.; Heidar, N.A.; Bulbul, J.; Asmar, S.; Hong, S.H.; Yang, J.W.; Kronbichler, A.; et al. Anthropometric Variables as Predictors of Semen Parameters and Fertility Outcomes after Varicocelectomy. J. Clin. Med. 2020, 9, 1160. [Google Scholar] [CrossRef] [Green Version]
- Sousa, A.P.; Santos-Pereira, J.; Freire, M.J.; Parada, B.; Almeida-Santos, T.; Bernardino, J.; Ramalho-Santos, J. Using Data Mining to Assist in Predicting Reproductive Outcomes Following Varicocele Embolization. J. Clin. Med. 2021, 10, 3503. [Google Scholar] [CrossRef]
- Chiles, K.A.; Schlegel, P.N. Cost-Effectiveness of Varicocele Surgery in the Era of Assisted Reproductive Technology. Asian J. Androl. 2016, 18, 259–261. [Google Scholar] [CrossRef]
- Dubin, J.M.; Greer, A.B.; Kohn, T.P.; Masterson, T.A.; Ji, L.; Ramasamy, R. Men with Severe Oligospermia Appear to Benefit From Varicocele Repair: A Cost-Effectiveness Analysis of Assisted Reproductive Technology. Urology 2018, 111, 99–103. [Google Scholar] [CrossRef]
- Seo, J.T.; Kim, K.T.; Moon, M.H.; Kim, W.T. The Significance of Microsurgical Varicocelectomy in the Treatment of Subclinical Varicocele. Fertil. Steril. 2010, 93, 1907–1910. [Google Scholar] [CrossRef]
- Cantoro, U.; Polito, M.; Muzzonigro, G. Reassessing the Role of Subclinical Varicocele in Infertile Men with Impaired Semen Quality: A Prospective Study. Urology 2015, 85, 826–830. [Google Scholar] [CrossRef]
- Yamamoto, M.; Hibi, H.; Hirata, Y.; Miyake, K.; Ishigaki, T. Effect of Varicocelectomy on Sperm Parameters and Pregnancy Rate in Patients with Subclinical Varicocele: A Randomized Prospective Controlled Study. J. Urol. 1996, 155, 1636–1638. [Google Scholar] [CrossRef] [PubMed]
- Grasso, M.; Lania, C.; Castelli, M.; Galli, L.; Franzoso, F.; Rigatti, P. Low-Grade Left Varicocele in Patients over 30 Years Old:The Effect of Spermatic Vein Ligation on Fertility. BJU Int. 2000, 85, 305–307. [Google Scholar] [CrossRef]
- Pallwein, L.; Pinggera, G.; Schuster, A.H.; Klauser, A.; Weirich, H.G.; Recheis, W.; Herwig, R.; Halpern, E.J.; Bartsch, G.; Zur Nedden, D.; et al. The Influence of Left Renal Vein Entrapment on Outcome after Surgical Varicocele Repair: A Color Doppler Sonographic Demonstration. J. Ultrasound Med. 2004, 23, 595–601. [Google Scholar] [CrossRef] [PubMed]
- Jensen, C.F.S.; Østergren, P.; Dupree, J.M.; Ohl, D.A.; Sønksen, J.; Fode, M. Varicocele and Male Infertility. Nat. Rev. Urol. 2017, 14, 523–533. [Google Scholar] [CrossRef]
- Pinggera, G.M.; Herwig, R.; Pallwein, L.; Frauscher, F.; Judmaier, W.; Mitterberger, M.; Bartsch, G.; Mallouhi, A. Isolated Right-Sided Varicocele as a Salvage Pathway for Portal Hypertension. Int. J. Clin. Pract. 2005, 59, 740–742. [Google Scholar] [CrossRef] [PubMed]
- Elbendary, M.A.; Elbadry, A.M. Right Subclinical Varicocele: How to Manage in Infertile Patients with Clinical Left Varicocele? Fertil. Steril. 2009, 92, 2050–2053. [Google Scholar] [CrossRef] [PubMed]
- Scherr, D.; Goldstein, M. Comparison of Bilateral versus Unilateral Varicocelectomy in Men with Palpable Bilateral Varicoceles. J. Urol. 1999, 162, 85–88. [Google Scholar] [CrossRef]
- Niu, Y.; Wang, D.; Chen, Y.; Pokhrel, G.; Xu, H.; Wang, T.; Wang, S.; Liu, J. Comparison of Clinical Outcome of Bilateral and Unilateral Varicocelectomy in Infertile Males with Left Clinical and Right Subclinical Varicocele: A Meta-Analysis of Randomised Controlled Trials. Andrologia 2018, 50, e13078. [Google Scholar] [CrossRef]
- Sun, X.; Wang, J.; Peng, Y.; Gao, Q.; Song, T.; Yu, W.; Xu, Z.; Chen, Y.; Dai, Y. Bilateral Is Superior to Unilateral Varicocelectomy in Infertile Males with Left Clinical and Right Subclinical Varicocele: A Prospective Randomized Controlled Study. Int. Urol. Nephrol. 2018, 50, 205–210. [Google Scholar] [CrossRef]
- Palomo, A. Radical Cure of Varicocele by a New Technique; Preliminary Report. J. Urol. 1949, 61, 604–607. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Franco, A.; Proietti, F.; Palombi, V.; Savarese, G.; Guidotti, M.; Leonardo, C.; Ferro, F.; Manna, C.; Franco, G. Varicocele: To Treat or Not to Treat? J. Clin. Med. 2023, 12, 4062. https://doi.org/10.3390/jcm12124062
Franco A, Proietti F, Palombi V, Savarese G, Guidotti M, Leonardo C, Ferro F, Manna C, Franco G. Varicocele: To Treat or Not to Treat? Journal of Clinical Medicine. 2023; 12(12):4062. https://doi.org/10.3390/jcm12124062
Chicago/Turabian StyleFranco, Antonio, Flavia Proietti, Veronica Palombi, Gabriele Savarese, Michele Guidotti, Costantino Leonardo, Fabio Ferro, Claudio Manna, and Giorgio Franco. 2023. "Varicocele: To Treat or Not to Treat?" Journal of Clinical Medicine 12, no. 12: 4062. https://doi.org/10.3390/jcm12124062
APA StyleFranco, A., Proietti, F., Palombi, V., Savarese, G., Guidotti, M., Leonardo, C., Ferro, F., Manna, C., & Franco, G. (2023). Varicocele: To Treat or Not to Treat? Journal of Clinical Medicine, 12(12), 4062. https://doi.org/10.3390/jcm12124062







