The Child’s Age and the Size of the Curvature Do Not Affect the Accuracy of Screw Placement with the Free-Hand Technique in Spinal Deformities in Children and Adolescents
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Patients
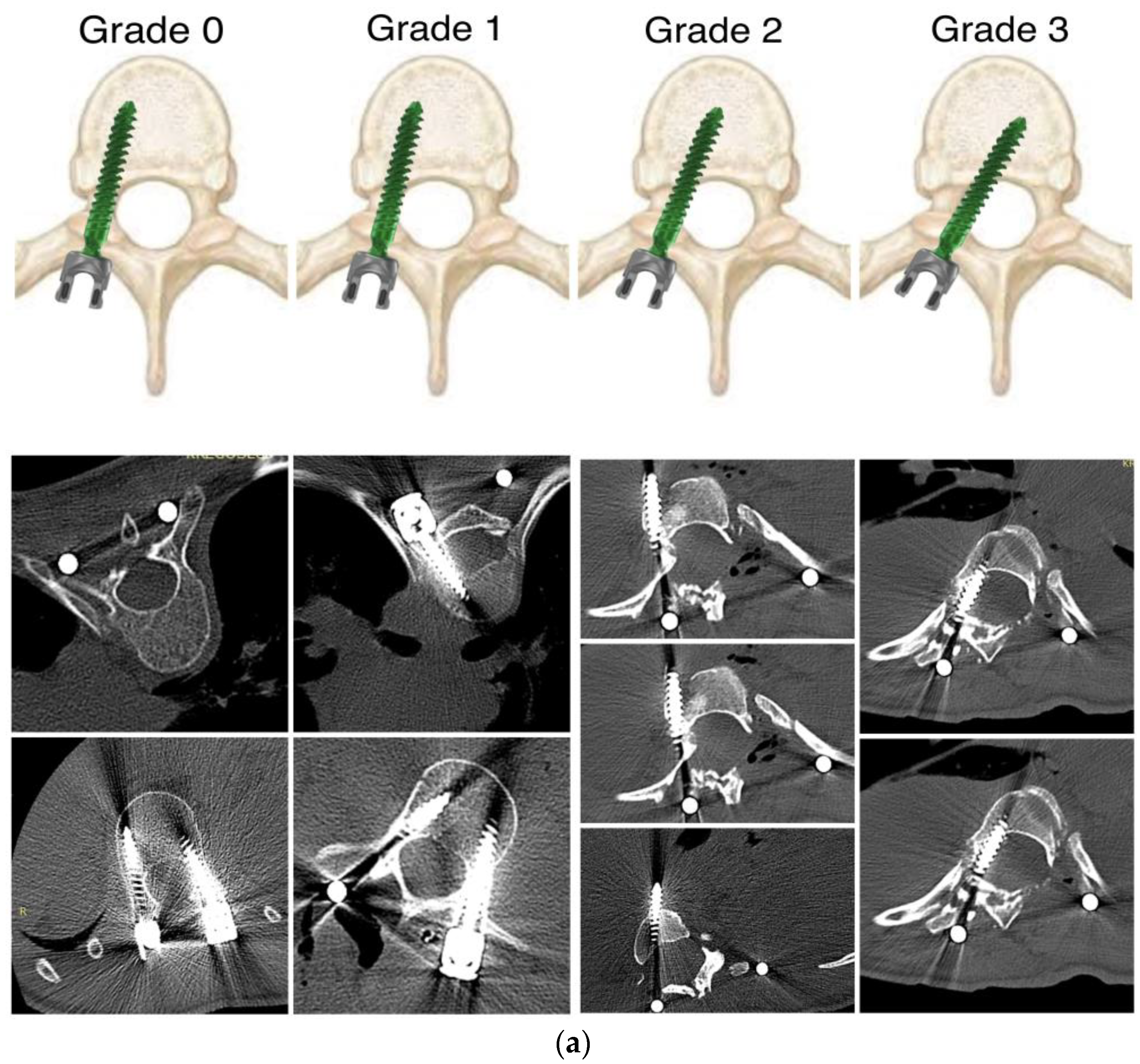
2.2. Outcome Parameters
2.3. Radiographic Parameters
2.4. Statistical Analysis
3. Results
4. Discussion
4.1. Free-Hand Screw Accuracy
4.2. Acceptable Malpositioning and Safety Zone
4.3. Power, Navigation, and Robotics-Assisted Techniques
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Suk, S.I.; Kim, W.J.; Lee, S.M.; Kim, J.H.; Chung, E.R. Thoracic pedicle screw fixation in spinal deformities: Are they really safe? Spine 2001, 26, 2049–2057. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Lenke, L.G.; Bridwell, K.H.; Cho, Y.S.; Riew, K.D. Free hand pedicle screw placement in the thoracic spine: Is it safe? Spine 2004, 29, 333–342. [Google Scholar] [CrossRef] [PubMed]
- Lenke, L.G.; Kim, Y.J. Thoracic pedicle screw placement: Free-hand technique. Neurol. India 2005, 53, 512–519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, Y.J.; Lenke, L.G.; Kim, J.; Bridwell, K.H.; Cho, S.K.; Cheh, G.; Sides, B. Comparative Analysis of Pedicle Screw Versus Hybrid Instrumentation in Posterior Spinal Fusion of Adolescent Idiopathic Scoliosis. Spine 2006, 31, 291–298. [Google Scholar] [CrossRef]
- Kim, Y.J.; Lenke, L.G.; Cheh, G.; Riew, K.D. Evaluation of Pedicle Screw Placement in the Deformed Spine Using Intraoperative Plain Radiographs: A Comparison with Computerized Tomography. Spine 2005, 30, 2084–2088. [Google Scholar] [CrossRef]
- Lenke, L.G.; Kuklo, T.R.; Ondra, S.; Polly, D.W., Jr. Rationale Behind the Current State-of-the-Art Treatment of Scoliosis (in the Pedicle Screw Era). Spine 2008, 33, 1051–1054. [Google Scholar] [CrossRef]
- Kuklo, T.R.; Lenke, L.G.; O’Brien, M.F.; Lehman, R.A., Jr.; Polly, D.W., Jr.; Schroeder, T.M. Accuracy and Efficacy of Thoracic Pedicle Screws in Curves More Than 90°. Spine 2005, 30, 222–226. [Google Scholar] [CrossRef]
- Lehman, R.A., Jr.; Lenke, L.G.; Keeler, K.A.; Kim, Y.J.; Cheh, G. Computed tomography evaluation of pedicle screw placed in the pediatric deformed spine over an 8-year period. Spine 2007, 32, 2679–2684. [Google Scholar] [CrossRef]
- Lee, C.S.; Park, S.-A.; Hwang, C.J.; Kim, D.-J.; Lee, W.-J.; Kim, Y.-T.; Lee, M.Y.; Yoon, S.J.; Lee, D.-H. A Novel Method of Screw Placement for Extremely Small Thoracic Pedicles in Scoliosis. Spine 2011, 36, E1112–E1116. [Google Scholar] [CrossRef]
- Şarlak, A.Y.; Tosun, B.; Atmaca, H.; Sarisoy, H.T.; Buluç, L. Evaluation of thoracic pedicle screw placement in adolescent idiopathic scoliosis. Eur. Spine J. 2009, 18, 1892–1897. [Google Scholar] [CrossRef] [Green Version]
- Modi, H.; Suh, S.W.; Song, H.-R.; Yang, J.-H. Accuracy of thoracic pedicle screw placement in scoliosis using the ideal pedicle entry point during the freehand technique. Int. Orthop. 2008, 33, 469–475. [Google Scholar] [CrossRef] [Green Version]
- Diab, M.; Smith, A.R.; Kuklo, T.R.; Spinal Deformity Study Group. Neural complications in the surgical treatment of adolescent idiopathic scoliosis. Spine 2007, 32, 2759–2763. [Google Scholar] [CrossRef] [Green Version]
- Marouby, S.; Jeandel, C.; M’sabah, D.L.; Delpont, M.; Cottalorda, J. Esophageal perforation caused by a thoracic pedicle screw. Eur. Spine J. 2018, 30, 2040–2045. [Google Scholar] [CrossRef]
- Lonstein, J.E.; Denis, F.; Perra, J.H.; Pinto, M.R.; Smith, M.D.; Winter, R.B. Complications Associated with Pedicle Screws. J. Bone Jt. Surg. 1999, 81, 1519–1528. [Google Scholar] [CrossRef]
- Skaggs, K.F.; Brasher, A.E.; Johnston, C.E.; Purvis, J.M.; Smith, J.T.; Myung, K.S.; Skaggs, D.L. Upper Thoracic Pedicle Screw Loss of Fixation Causing Spinal Cord Injury: A review of the literature and multicenter case series. J. Pediatr. Orthop. 2013, 33, 75–79. [Google Scholar] [CrossRef]
- Jiang, H.; Qiu, X.; Wang, W.; Zhu, Z.; Qian, B.; Guo, J.; Qiu, Y. The position of the aorta changes with altered body position in single right thoracic adolescent idiopathic scoliosis: A magnetic resonance imaging study. Spine 2012, 37, E1054–E1061. [Google Scholar] [CrossRef]
- Suk, S.-I.; Kim, J.-H.; Kim, S.-S.; Lim, D.-J. Pedicle screw instrumentation in adolescent idiopathic scoliosis (AIS). Eur. Spine J. 2011, 21, 13–22. [Google Scholar] [CrossRef] [Green Version]
- Grabala, P.; Helenius, I.J.; Buchowski, J.M.; Shah, S.A. The Efficacy of a Posterior Approach to Surgical Correction for Neglected Idiopathic Scoliosis: A Comparative Analysis According to Health-Related Quality of Life, Pulmonary Function, Back Pain and Sexual Function. Children 2023, 10, 299. [Google Scholar] [CrossRef]
- Jiang, J.; Qian, B.P.; Qiu, Y.; Wang, B.; Yu, Y.; Zhu, Z.Z. The azygous vein is at potential risk of injury from malpositioning of left thoracic pedicle screw in thoracic adolescent idiopathic scoliosis patients. Spine 2017, 42, E920–E925. [Google Scholar] [CrossRef]
- Liu, J.; Shen, J.; Zhang, J.; Li, S.; Zhao, H.; Qiu, G.; Wang, Y. The Position of the Aorta Relative to the Spine for Pedicle Screw Placement in the Correction of Idiopathic Scoliosis. J. Spinal Disord. Tech. 2012, 25, E103–E107. [Google Scholar] [CrossRef]
- Azimi, P.; Shahzadi, S.; Shahzadi, A. Accuracy and complications of pedicle screw insertion for lumbar and thoracolumbar fractures. Int. Clin. Neurosci. J. 2014, 1, 61–64. [Google Scholar] [CrossRef]
- Illingworth, K.D.; Claeson, A.A.; Skaggs, D.L. Surgical technique: Power pedicle preparation and screw insertion in the treatment of pediatric spinal deformity. J. Posna 2019, 1, 1. [Google Scholar] [CrossRef]
- Seehausen, D.A.; Skaggs, D.L.; Andras, L.M.; Javidan, Y. Safety and Efficacy of Power-Assisted Pedicle Tract Preparation and Screw Placement. Spine Deform. 2015, 3, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Skaggs, D.L.; Compton, E.; Vitale, M.G.; Garg, S.; Stone, J.; Fletcher, N.D.; Illingworth, K.D.; Kim, H.J.; Ball, J.; Kim, E.B.; et al. Power versus manual pedicle tract preparation: A multi-center study of early adopters. Spine Deform. 2021, 9, 1395–1402. [Google Scholar] [CrossRef] [PubMed]
- Macke, J.J.; Woo, R.; Varich, L. Accuracy of robot-assisted pedicle screw placement for adolescent idiopathic scoliosis in the pediatric population. J. Robot. Surg. 2016, 10, 145–150. [Google Scholar] [CrossRef]
- Akazawa, T.; Torii, Y.; Ueno, J.; Umehara, T.; Iinuma, M.; Yoshida, A.; Tomochika, K.; Ohtori, S.; Niki, H. Accuracy of computer-assisted pedicle screw placement for adolescent idiopathic scoliosis: A comparison between robotics and navigation. Eur. Spine J. 2022, 32, 651–658. [Google Scholar] [CrossRef]
- Li, C.; Su, J.; Wang, Z.; Li, D.; Tian, Y.; Yuan, S.; Wang, L.; Liu, X. Comparison of the Accuracy of Pedicle Screw Placement Using a Fluoroscopy-Assisted Free-Hand Technique with Robotic-Assisted Navigation Using an O-Arm or 3D C-Arm in Scoliosis Surgery. Glob. Spine J. 2022, 21925682221143076. [Google Scholar] [CrossRef]
- Chiu, C.K.; Chan, C.Y.W.; Kwan, M.K. The accuracy and safety of fluoroscopic-guided percutaneous pedicle screws in the thoracic and lumbosacral spine in the Asian population: A CT scan analysis of 1002 screws. J. Orthop. Surg. 2017, 25, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Avila, M.J.; Baaj, A.A. Freehand Thoracic Pedicle Screw Placement: Review of Existing Strategies and a Step-by-Step Guide Using Uniform Landmarks for All Levels. Cureus 2016, 8, e501. [Google Scholar] [CrossRef] [Green Version]
- Hicks, J.; Singla, A.; Arlet, V. Complications of Pedicle Screw Fixation in Scoliosis Surgery: A Systematic Review. Spine J. 2010, 35, E465–E467. [Google Scholar] [CrossRef]
- Charalampidis, A.; Jiang, F.; Wilson, J.R.F.; Badhiwala, J.H.; Brodke, D.S.; Fehlings, M.G. The Use of Intraoperative Neurophysiological Monitoring in Spine Surgery. Glob. Spine J. 2020, 10 (Suppl. S1), 104S–114S. [Google Scholar] [CrossRef]
- Lenke, L.G.; Dobbs, M.B. Management of juvenile idiopathic scoliosis. J. Bone Jt. Surg. Am. 2007, 89 (Suppl. S1), 55–63. [Google Scholar] [CrossRef] [Green Version]
- Gertzbein, S.D.; Robbins, S.E. Accuracy of Pedicular Screw Placement In Vivo. Spine 1990, 15, 11–14. [Google Scholar] [CrossRef]
- Choma, T.J.; Denis, F.; Lonstein, J.E.; Perra, J.H.; Schwender, J.D.; Garvey, T.A.; Mullin, W.J. Stepwise Methodology for Plain Radiographic Assessment of Pedicle Screw Placement: A Comparison with Computed Tomography. J. Spinal Disord. Tech. 2006, 19, 547–553. [Google Scholar] [CrossRef]
- Kwan, M.K.; Chiu, C.K.; Gani, S.M.A.; Wei, C.C. Accuracy and safety of pedicle screw placement in adolescent idiopathic scoliosis patients: A review of 2020 screws using computed tomography assessment. Spine 2017, 42, 326–335. [Google Scholar] [CrossRef]
- Larson, A.N.; Santos, E.R.G.; Polly, D.W., Jr.; Ledonio, C.G.T.; Sembrano, J.N.; Mielke, C.H.; Guidera, K.J. Pediatric Pedicle Screw Placement Using Intraoperative Computed Tomography and 3-Dimensional Image-Guided Navigation. Spine 2012, 37, E188–E194. [Google Scholar] [CrossRef]
- Urbanski, W.; Jurasz, W.; Wolanczyk, M.; Kulej, M.; Morasiewicz, P.; Dragan, S.L.; Zaluski, R.; Miekisiak, G. Increased Radiation but No Benefits in Pedicle Screw Accuracy with Navigation versus a Freehand Technique in Scoliosis Surgery. Clin. Orthop. Relat. Res. 2018, 476, 1020–1027. [Google Scholar] [CrossRef] [PubMed]
- Ranade, A.; Samdani, A.F.; Williams, R.; Barne, K.; McGirt, M.J.; Ramos, G.; Betz, R.R. Feasibility and Accuracy of Pedicle Screws in Children Younger Than Eight Years of Age. Spine 2009, 34, 2907–2911. [Google Scholar] [CrossRef] [PubMed]
- Belmont, P.J., Jr.; Klemme, W.R.; Robinson, M.; Polly, D.W., Jr. Accuracy of Thoracic Pedicle Screws in Patients with and Without Coronal Plane Spinal Deformities. Spine 2002, 27, 1558–1566. [Google Scholar] [CrossRef]
- Tan, L.A.; Yerneni, K.; Tuchman, A.; Li, X.J.; Cerpa, M.; Lehman, R.A., Jr.; Lenke, L.G. Utilization of the 3D-printed spine model for freehand pedicle screw placement in complex spinal deformity correction. J. Spine Surg. 2018, 4, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Swany, L.; Larson, A.N.; Garg, S.; Hedequist, D.; Newton, P.; Sponseller, P.; Harms Study Group. 0.4% incidence of return to OR due to screw malposition in a large prospective adolescent idiopathic scoliosis database. Spine Deform. 2021, 10, 361–367. [Google Scholar] [CrossRef]
- Liljenqvist, U.; Hackenberg, L. Morphometric analysis of thoracic and lumbar vertebrae in idiopathic scoliosis. Stud. Health Technol. Inform. 2002, 88, 382–386. [Google Scholar] [CrossRef]
- Puvanesarajah, V.; Liauw, J.A.; Lo, S.-F.; Lina, I.A.; Witham, T.F. Techniques and accuracy of thoracolumbar pedicle screw placement. World J. Orthop. 2014, 5, 112–123. [Google Scholar] [CrossRef]
- Watanabe, K.; Lenke, L.G.; Matsumoto, M.; Harimaya, K.; Kim, Y.J.; Hensley, M.R.; Stobbs, G.R.; Toyama, Y.; Chiba, K. A Novel Pedicle Channel Classification Describing Osseous Anatomy: How many thoracic scoliotic pedicles have cancellous channels? Spine 2010, 35, 1836–1842. [Google Scholar] [CrossRef]
- Dvorak, M.M.; MacDonald, S.; Gurr, K.R.M.; Bailey, S.I.M.; Haddad, R.G.F. An Anatomic, Radiographic, and Biomechanical Assessment of Extrapedicular Screw Fixation in the Thoracic Spine. Spine 1993, 18, 1689–1694. [Google Scholar] [CrossRef]
- Polly, D.W., Jr.; Potter, B.K.; Kuklo, T.; Young, S.; Johnson, C.; Klemme, W.R. Volumetric spinal canal intrusion: A comparison between thoracic pedicle screws and thoracic hooks. Spine 2004, 29, 63–69. [Google Scholar] [CrossRef]
- Baghdadi, Y.M.; Larson, A.N.; McIntosh, A.L.; Shaughnessy, W.J.; Dekutoski, M.B.; Stans, A.A. Complications of pedicle screws in children 10 years or younger: A case control study. Spine 2013, 38, E386–E393. [Google Scholar] [CrossRef]
- Ledonio, C.G.; Polly, D.W., Jr.; Vitale, M.G.; Wang, Q. Pediatric pedicle screws: Comparative effectiveness and safety: A systematic literature review from the Scoliosis Research Society and the Pediatric Orthopaedic Society of North America task force. J. Bone Jt. Surg. Am. 2011, 93, 1227–1234. [Google Scholar] [CrossRef]
- Abul-Kasim, K.; Ohlin, A.; Strombeck, A.; Maly, P.; Sundgren, P.C. Radiological and clinical outcome of screw placement in adolescent idiopathic scoliosis: Evaluation with low-dose computed tomography. Eur. Spine J. 2010, 19, 96–104. [Google Scholar] [CrossRef] [Green Version]
- Ughwanogho, E.; Patel, N.M.; Baldwin, K.D.; Sampson, N.R.; Flynn, J.M. Computed tomography-guided navigation of thoracic pedicle screws for adoles- cent idiopathic scoliosis results in more accurate placement and less screw removal. Spine 2012, 37, E473–E478. [Google Scholar] [CrossRef]
- Faldini, C.; Barile, F.; Viroli, G.; Manzetti, M.; Ialuna, M.; Traversari, M.; Paolucci, A.; Rinaldi, A.; D’antonio, G.; Ruffilli, A. Freehand power-assisted pedicle screw placement in scoliotic patients: Results on 5522 consecutive pedicle screws. Musculoskelet. Surg. 2022. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Du, S.-Y.; Dai, J.; Zhou, Z.-T.; Shan, B.-C.; Jiang, F.-X.; Yang, J.-Y.; Cao, L.; Zhou, X.-Z. Size selection and placement of pedicle screws using robot-assisted versus fluoroscopy-guided techniques for thoracolumbar fractures: Possible implications for the screw loosening rate. BMC Surg. 2022, 22, 365. [Google Scholar] [CrossRef] [PubMed]
- Kanaly, C.W.; Backes, D.M.; Toossi, N.; Bucklen, B. A Retrospective Analysis of Pedicle Screw Placement Accuracy Using the ExcelsiusGPS Robotic Guidance System: Case Series. Oper. Neurosurg. 2023, 24, 242–247. [Google Scholar] [CrossRef] [PubMed]





| Variable | Group 1 (n = 94) | Group 2 (n = 116) | Group 3 (n = 108) |
|---|---|---|---|
| Age (range, years) | 2–10 | 11–13 | 14–18 |
| Sex (M, F) | M-6, F-41 | M-9, F-107 | M-11, F-97 |
| Follow-up range (months) | 12–70 | 12–68 | 12–63 |
| Etiology: | |||
| Congenital (n) | 12 | 4 | 3 |
| Neuromuscular (n) | 12 | 16 | 12 |
| Syndromic (n) | 12 | 7 | 3 |
| Idiopathic (n) | 58 | 89 | 90 |
| Main curve magnitude (degrees, range) preoperative | 65–122 | 52–141 | 55–145 |
| Main curve magnitude (degrees, range) postoperative | 18–77 | 16–68 | 12–71 |
| Main thoracic kyphosis (degrees, range) preoperative | 12–105 | 16–120 | 19–128 |
| Main thoracic kyphosis (degrees, range) postoperative | 11–62 | 12–58 | 14–52 |
| Main lumbar lordosis (degrees, range) preoperative | 42–76 | 44–79 | 42–76 |
| Main lumbar lordosis (degrees, range) postoperative | 12–55 | 11–49 | 9–52 |
| Variable | Group 1 | Group 2 | Group 1 vs. 2 | Group 3 | Group 1 vs. 3 |
|---|---|---|---|---|---|
| Number of screw placements (n), percent of total screws (%) | 1201 18.9% | 2704 42.53% | N.S. | 2453 38.58% | N.S. |
| Number of screw placements in thoracic spine (n), percent of total screws (%) | 924 14.53% | 1922 30.23% | p = 0.122 | 1817 28.58% | p = 0.229 |
| Number of screw placements in lumbar spine (n), percent of total screws (%) | 277 4.36% | 781 12.28% | p = 0.551 | 637 10.02% | p = 0.682 |
| Total breaches | 60 (4.99%) | 155 (5.73%) | p = 0.228 | 162 (6.60%) | p = 0.131 |
| Medial breaches | 36 (2.99%) | 95 (3.51%) | p = 0.091 | 90 (3.66%) | p = 0.101 |
| Lateral breaches | 51 (1.88%) | 51 (1.88%) | p = 0.88 | 62 (2.52%) | p = 0.628 |
| Anterior breaches | 2 (0.16%) | 4 (0.14%) | p = 0.92 | 4 (0.16%) | p = 0.88 |
| Inferior breaches | 2 (0.16%) | 2 (0.07%) | p = 0.96 | (0.08%) | p = 0.91 |
| Superior breaches | 2 (0.16%) | 3 (0.11%) | p = 0.96 | (0.16%) | p = 0.93 |
| Thoracic breaches | 48 (3.99%) | 117 (4.32%) | p = 0.61 | 126 (5.13%) | p = 0.21 |
| Lumbar and sacral breaches | 12 (0.99%) | 38 (1.40%) | p = 0.89 | 36 (1.47%) | p = 0.79 |
| Thoracic vs. lumbar and sacral breaches | p = 0.03 | p = 0.02 | NA | p = 0.01 | NA |
| Variable | A | B | C | D |
|---|---|---|---|---|
| Group 1 | 679 | 406 | 41 | 75 |
| (n = 1201) | (56.6%) | (33.8%) | (3.4%) | (6.2%) |
| Group 2 | 1630 | 857 | 76 | 141 |
| (n = 2704) | (60.3%) | (31.7%) | (2.8%) | (5.2%) |
| Group 1 vs. Group 2 | p = 0.871 | p = 0.682 | p = 0.771 | p = 0.921 |
| Group 3 | 1236 | 971 | 101 | 145 |
| (n = 2453) | (50.4%) | (39.6%) | (4.1%) | (5.9%) |
| Group 1 vs. Group 3 | p = 0.322 | p = 0.214 | p = 0.691 | p = 0.682 |
| Total Screws | (55.75%) | (35.14%) | (3.43%) | (5.68%) |
| (n = 6358) | 3545 | 2234 | 218 | 361 |
| Parameter n = 6358 | No Breaches n = 5562 | Lateral n = 131 | Medial n = 221 | Other and Juxtapedicular n = 444 (6.98%) | Replacement n = 17 (0.26%) |
|---|---|---|---|---|---|
| Tapping canal n = 3205 | 2916 (91%) | 47 (1.47%) | 100 (3.12%) | 275 (8.5%) | 6 (0.18%) |
| No tapping canal n = 3153 | 2646 (84%) | 84 (2.66%) | 121 (3.84%) | 169 (5.36%) | 11 (0.35%) |
| p = 0.037 | p = 0.329 | p = 0.431 | p = 0.1121 | p = 0.0212 | |
| Curve more than 90 degrees n = 2861 | 2489 (87%) | 85 (2.97%) | 121 (4.23%) | 232 (8.1%) | 12 (0.41%) |
| Curve less than 90 degrees n = 3497 | 3073 (88%) | 46 (1.31%) | 100 (2.85%) | 212 (6.06%) | 5 (0.14%) |
| p = 0.881 | p = 0.671 | p = 0.127 | p = 0.562 | p = 0.324 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grabala, P.; Helenius, I.J.; Kowalski, P.; Grabala, M.; Zacha, S.; Deszczynski, J.M.; Albrewczynski, T.; Galgano, M.A.; Buchowski, J.M.; Chamberlin, K.; et al. The Child’s Age and the Size of the Curvature Do Not Affect the Accuracy of Screw Placement with the Free-Hand Technique in Spinal Deformities in Children and Adolescents. J. Clin. Med. 2023, 12, 3954. https://doi.org/10.3390/jcm12123954
Grabala P, Helenius IJ, Kowalski P, Grabala M, Zacha S, Deszczynski JM, Albrewczynski T, Galgano MA, Buchowski JM, Chamberlin K, et al. The Child’s Age and the Size of the Curvature Do Not Affect the Accuracy of Screw Placement with the Free-Hand Technique in Spinal Deformities in Children and Adolescents. Journal of Clinical Medicine. 2023; 12(12):3954. https://doi.org/10.3390/jcm12123954
Chicago/Turabian StyleGrabala, Pawel, Ilkka J. Helenius, Piotr Kowalski, Michal Grabala, Slawomir Zacha, Jaroslaw M. Deszczynski, Tomasz Albrewczynski, Michael A. Galgano, Jacob M. Buchowski, Kelly Chamberlin, and et al. 2023. "The Child’s Age and the Size of the Curvature Do Not Affect the Accuracy of Screw Placement with the Free-Hand Technique in Spinal Deformities in Children and Adolescents" Journal of Clinical Medicine 12, no. 12: 3954. https://doi.org/10.3390/jcm12123954
APA StyleGrabala, P., Helenius, I. J., Kowalski, P., Grabala, M., Zacha, S., Deszczynski, J. M., Albrewczynski, T., Galgano, M. A., Buchowski, J. M., Chamberlin, K., & Shah, S. A. (2023). The Child’s Age and the Size of the Curvature Do Not Affect the Accuracy of Screw Placement with the Free-Hand Technique in Spinal Deformities in Children and Adolescents. Journal of Clinical Medicine, 12(12), 3954. https://doi.org/10.3390/jcm12123954








