Rotational Thromboelastometry (ROTEM®) in Relation to Inflammatory Biomarkers and Clinical Outcome in COVID-19 Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Blood Collection and Storage
2.2. Rotational Thromboelastometry (ROTEM®)
2.3. Inflammatory Cytokines—Flow Cytometric Analysis
2.4. Statistical Analysis
3. Results
3.1. ROTEM®
3.2. Interleukins
3.3. Correlations between ROTEM Parameters and CT Severity Index
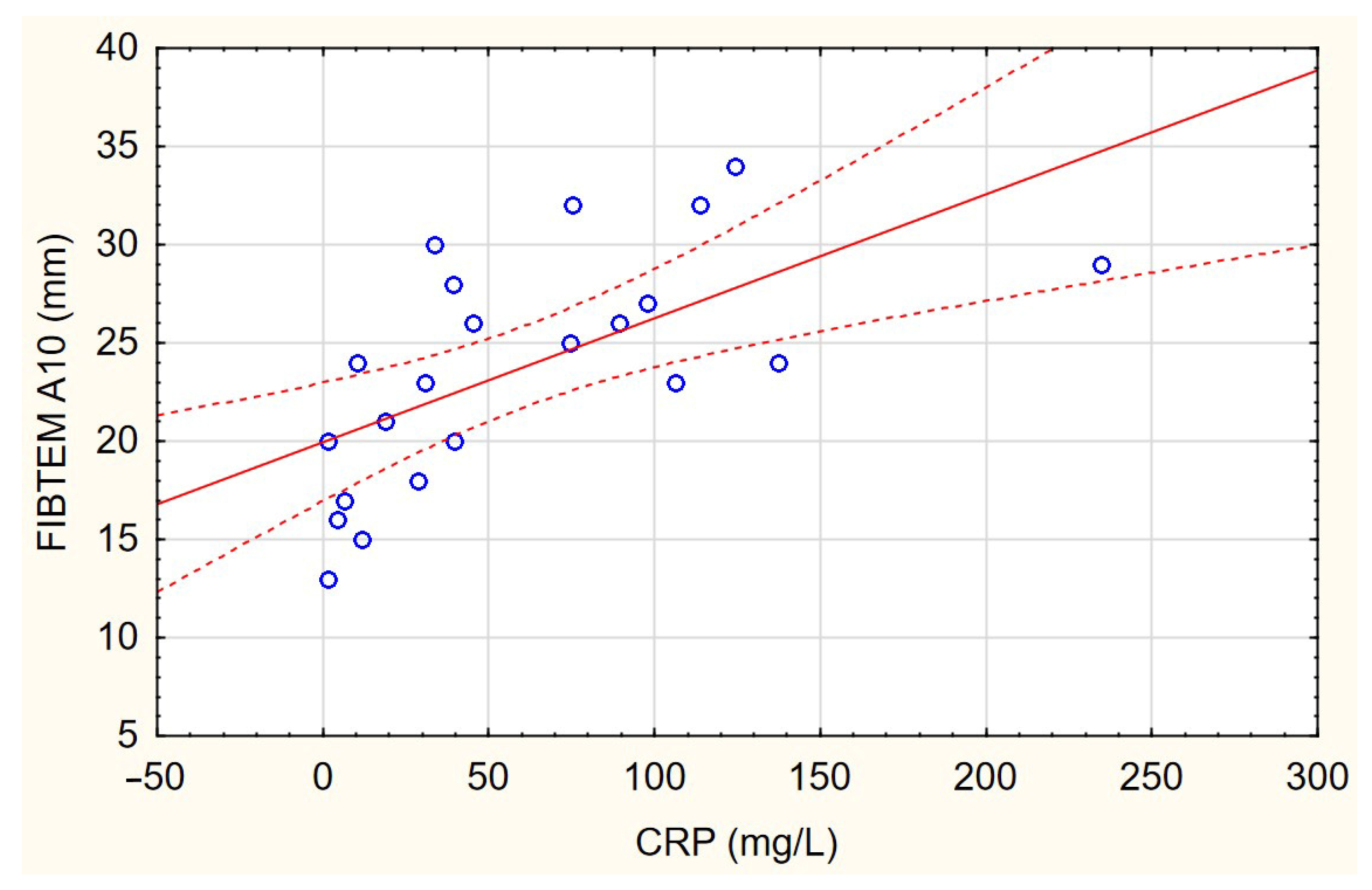
3.4. Correlations between ROTEM Parameters and Levels of Inflammatory Biomarkers
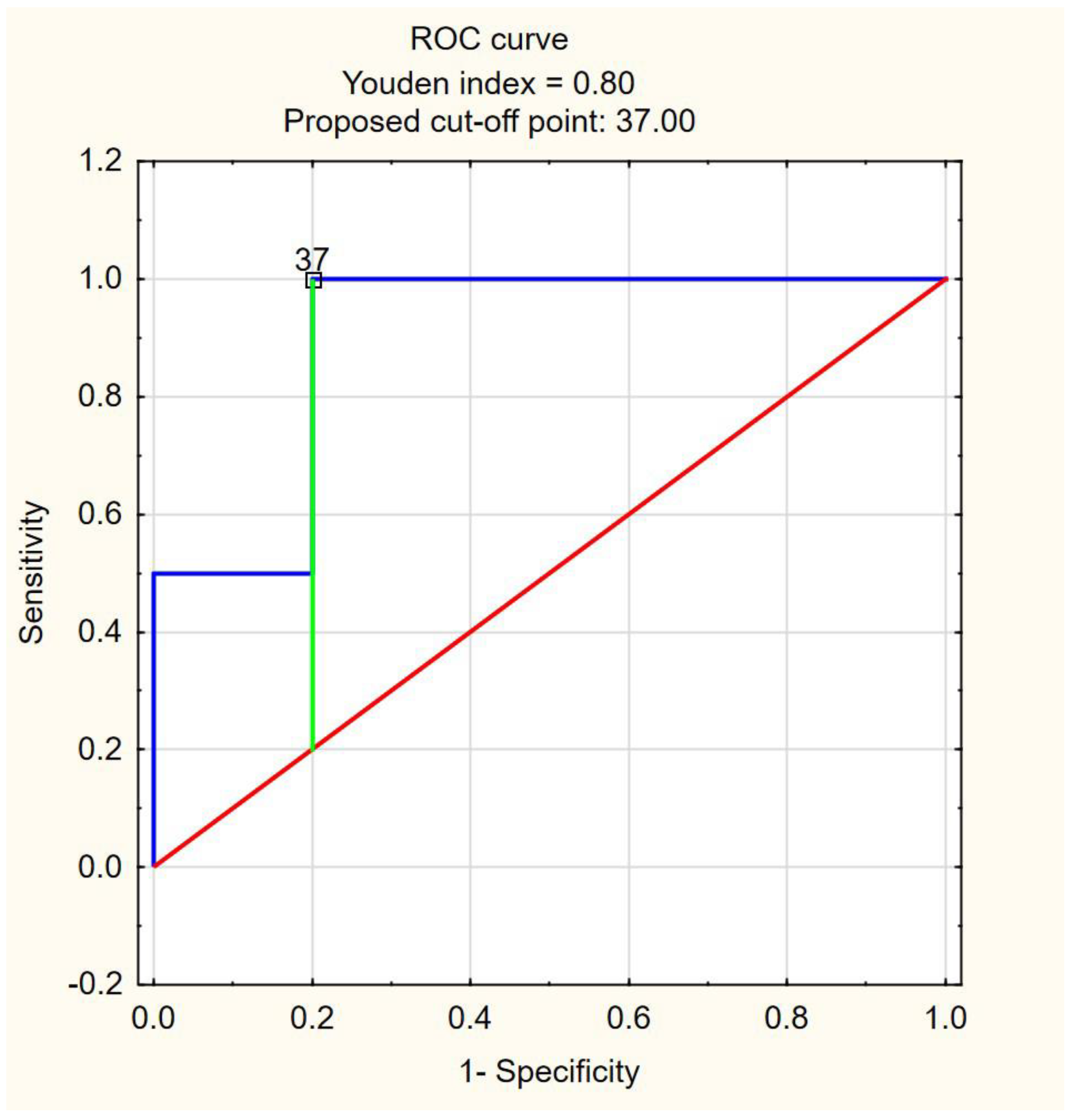
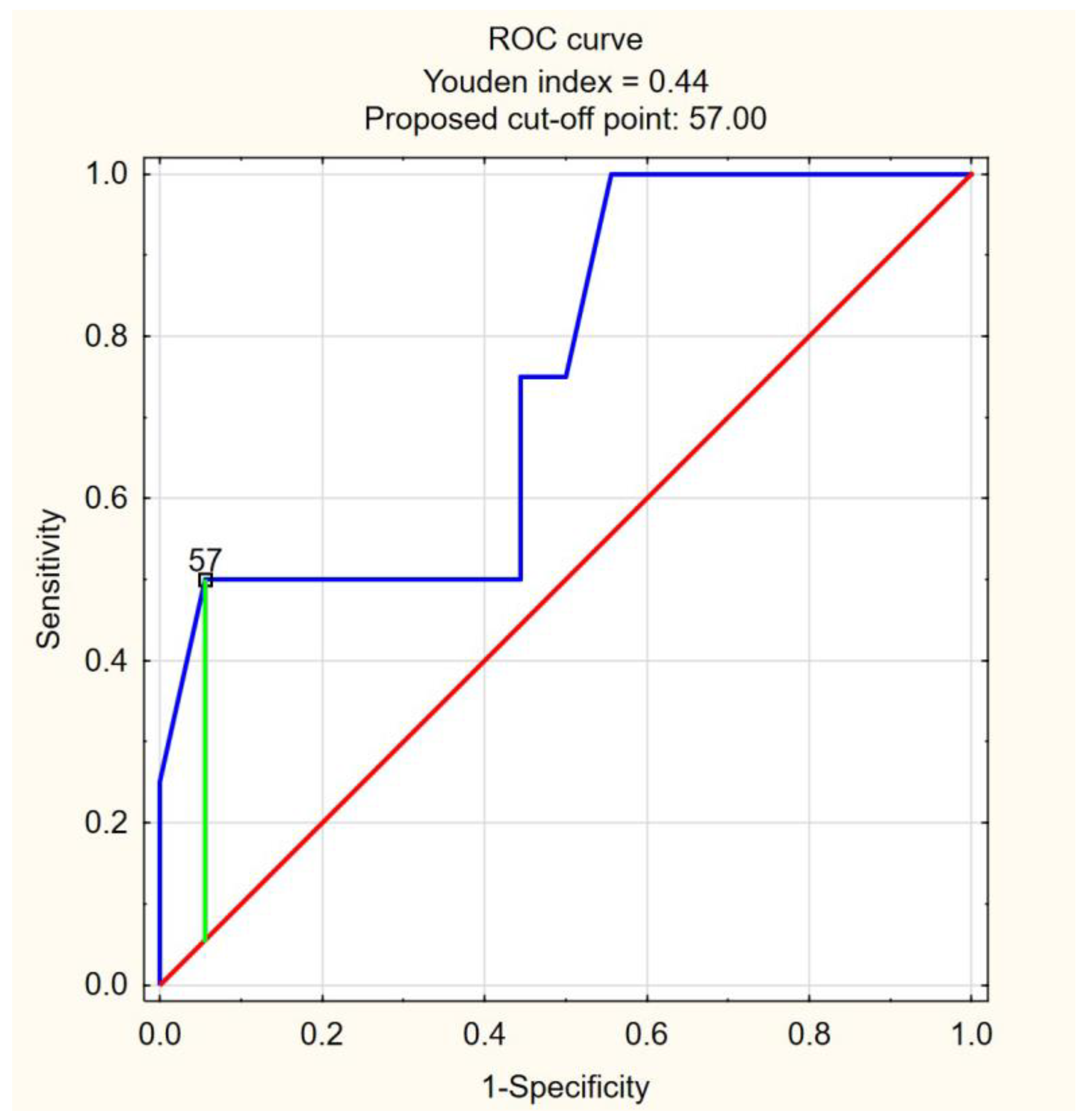
3.5. Multivariate Logistic Regression
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jiménez, D.; García-Sanchez, A.; Rali, P.; Muriel, A.; Bikdeli, B.; Ruiz-Artacho, P.; Le Mao, R.; Rodríguez, C.; Hunt, B.J.; Monreal, M. Incidence of VTE and Bleeding Among Hospitalized Patients With Coronavirus Disease 2019: A Systematic Review and Meta-analysis. Chest 2021, 159, 1182–1196. [Google Scholar] [CrossRef]
- Mansory, E.M.; Srigunapalan, S.; Lazo-Langner, A. Venous Thromboembolism in Hospitalized Critical and Noncritical COVID-19 Patients: A Systematic Review and Meta-analysis. TH Open 2021, 5, e286–e294. [Google Scholar] [CrossRef] [PubMed]
- Nopp, S.; Moik, F.; Jilma, B.; Pabinger, I.; Ay, C. Risk of venous thromboembolism in patients with COVID-19: A systematic review and meta-analysis. Res. Prac. Thromb. Haemost. 2020, 4, 1178–1191. [Google Scholar] [CrossRef] [PubMed]
- Gu, S.X.; Tyagi, T.; Jain, K.; Gu, V.W.; Lee, S.H.; Hwa, J.M.; Kwan, J.M.; Krause, D.S.; Lee, A.I.; Halene, S.; et al. Thrombocytopathy and endotheliopathy: Crucial contributors to COVID-19 thromboinflammation. Nat. Rev. Cardiol. 2021, 18, 194–209. [Google Scholar] [CrossRef] [PubMed]
- Connors, J.M.; Levy, J.H. Thromboinflammation and the hypercoagulability of COVID-19. J. Thromb. Haemost. 2020, 18, 1559–1561. [Google Scholar] [CrossRef] [PubMed]
- Smilowitz, N.R.; Kunichoff, D.; Garshick, M.; Shah, B.; Pillinger, M.; Hochman, J.S.; Berger, J.S. C-reactive protein and clinical outcomes in patients with COVID-19. Eur. Heart J. 2021, 42, 2270–2279. [Google Scholar] [CrossRef]
- Malik, P.; Patel, U.; Mehta, D.; Patel, N.; Kelkar, R.; Akrmah, M.; Gabrilove, J.L.; Sacks, H. Biomarkers and outcomes of COVID-19 hospitalisations: Systematic review and meta-analysis. BMJ Evid. Based Med. 2021, 26, 107–108. [Google Scholar] [CrossRef]
- Whiting, D.; DiNardo, J.A. TEG and ROTEM: Technology and clinical applications. Am. J. Hematol. 2014, 89, 228–232. [Google Scholar] [CrossRef]
- Rogalski, P.; Rogalska-Plonska, M.; Wroblewski, E.; Kostecka-Roslen, I.; Dabrowska, M.; Swidnicka-Siergiejko, A.; Wasielica-Berger, J.; Cydzik, M.; Hirnle, T.; Flisiak, R.; et al. Laboratory evidence for hypercoagulability in cirrhotic patients with history of variceal bleeding. Thromb. Res. 2019, 178, 41–46. [Google Scholar] [CrossRef]
- Gurbel, P.A.; Tantry, U.S.; Storey, R.F. International COVID-19 thrombosis biomarkers colloquium: COVID-19 diagnostic tests. J. Thromb. Thrombolysis 2021, 52, 992–998. [Google Scholar] [CrossRef]
- Panigada, M.; Bottino, N.; Tagliabue, P.; Grasselli, G.; Novembrino, C.; Chantarangkul, V.; Pesenti, A.; Peyvandi, F.; Tripodi, A. Hypercoagulability of COVID-19 patients in intensive care unit: A report of thromboelastography findings and other parameters of hemostasis. J. Thromb. Haemost. 2020, 18, 1738–1742. [Google Scholar] [CrossRef] [PubMed]
- Bareille, M.; Hardy, M.; Douxfils, J.; Roullet, S.; Lasne, D.; Levy, J.H.; Stépanian, A.; Susen, S.; Frère, C.; Lecompte, T.; et al. Viscoelastometric Testing to Assess Hemostasis of COVID-19: A Systematic Review. J. Clin. Med. 2021, 10, 1740. [Google Scholar] [CrossRef] [PubMed]
- Tsantes, A.E.; Tsantes, A.G.; Kokoris, S.I.; Bonovas, S.; Frantzeskaki, F.; Tsangaris, I.; Kopterides, P. COVID-19 Infection-Related Coagulopathy and Viscoelastic Methods: A Paradigm for Their Clinical Utility in Critical Illness. Diagnostics 2020, 10, 817. [Google Scholar] [CrossRef] [PubMed]
- Gurbel, P.A.; Bliden, K.P.; Levy, J.H.; Walia, N.; Rapista, N.; Cho, A.; Jerjian, C.; Tantry, U.S. Thrombogenicity markers for early diagnosis and prognosis in COVID-19: A change from the current paradigm? Blood Coagul. Fibrinolysis 2021, 32, 544–549. [Google Scholar] [CrossRef]
- Flisiak, R.; Horban, A.; Jaroszewicz, J.; Kozielewicz, D.; Mastalerz-Migas, A.; Owczuk, R.; Parczewski, M.; Pawłowska, M.; Piekarska, A.; Simon, K.; et al. Management of SARS-CoV-2 infection: Recommendations of the Polish Association of Epidemiologists and Infectiologists as of 26 April 2021. Pol. Arch. Intern. Med. 2021, 131, 487–496. [Google Scholar] [CrossRef]
- Goligher, E.C.; Bradbury, C.A.; McVerry, B.J.; Lawler, P.R.; Berger, J.S.; Gong, M.N.; Carrier, M.; Reynolds, H.R.; Kumar, A.; Turgeon, A.F.; et al. Therapeutic Anticoagulation with Heparin in Critically Ill Patients with COVID-19. N. Engl. J. Med. 2021, 385, 777–789. [Google Scholar] [CrossRef]
- Gorog, D.A.; Storey, R.F.; Gurbel, P.A.; Tantry, U.S.; Berger, J.S.; Chan, M.Y.; Duerschmied, D.; Smyth, S.S.; Parker, W.A.E.; Ajjan, R.A.; et al. Current and novel biomarkers of thrombotic risk in COVID-19: A Consensus Statement from the International COVID-19 Thrombosis Biomarkers Colloquium. Nat. Rev. Cardiol. 2022, 19, 475–495. [Google Scholar] [CrossRef]
- Czupryna, P.; Moniuszko-Malinowska, A.; Rogalska, M.; Zarębska-Michaluk, D.; Lorenc, B.; Rorat, M.; Kozielewicz, D.; Tudrujek-Zdunek, M.; Sikorska, K.; Berkan-Kawińska, A.; et al. Inflammatory and thrombotic parameters associated with the COVID-19 course in Poland (SARSTer study). Adv. Med. Sci. 2022, 67, 291–297. [Google Scholar] [CrossRef]
- Georgiadou, P.; Sokou, R.; Tsantes, A.G.; Parastatidou, S.; Konstantinidi, A.; Houhoula, D.; Kokoris, S.; Iacovidou, N.; Tsantes, A.E. The Non-Activated Thromboelastometry (NATEM) Assay’s Application among Adults and Neonatal/Pediatric Population: A Systematic Review. Diagnostics 2022, 12, 658. [Google Scholar] [CrossRef]
- Hartmann, J.; Ergang, A.; Mason, D.; Dias, J.D. The Role of TEG Analysis in Patients with COVID-19-Associated Coagulopathy: A Systematic Review. Diagnostics 2021, 11, 172. [Google Scholar] [CrossRef]
- Hulshof, A.M.; Brüggemann, R.A.G.; Mulder, M.M.G.; van de Berg, T.W.; Sels, J.E.M.; Olie, R.H.; Spaetgens, B.; Streng, A.S.; Verhezen, P.; van der Horst, I.C.C.; et al. Serial EXTEM, FIBTEM, and tPA Rotational Thromboelastometry Observations in the Maastricht Intensive Care COVID Cohort-Persistence of Hypercoagulability and Hypofibrinolysis Despite Anticoagulation. Front. Cardiovasc. Med. 2021, 8, 654174. [Google Scholar] [CrossRef] [PubMed]
- Yatim, N.; Boussier, J.; Chocron, R.; Hadjadj, J.; Philippe, A.; Gendron, N.; Barnabei, L.; Charbit, B.; Szwebel, T.A.; Carlier, N.; et al. Platelet activation in critically ill COVID-19 patients. Ann. Intensive Care 2021, 11, 113. [Google Scholar] [CrossRef] [PubMed]
- Storey, R.F.; May, J.A.; Heptinstall, S. Potentiation of platelet aggregation by heparin in human whole blood is attenuated by P2Y12 and P2Y1 antagonists but not aspirin. Thromb. Res. 2005, 115, 301–307. [Google Scholar] [CrossRef]
- Pavoni, V.; Gianesello, L.; Pazzi, M.; Stera, C.; Meconi, T.; Frigieri, F.C. Evaluation of coagulation function by rotation thromboelastometry in critically ill patients with severe COVID-19 pneumonia. J. Thromb. Thrombolysis 2020, 50, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Zuo, Y.; Warnock, M.; Harbaugh, A.; Yalavarthi, S.; Gockman, K.; Zuo, M.; Madison, J.A.; Knight, J.S.; Kanthi, Y.; Lawrence, D.A. Plasma tissue plasminogen activator and plasminogen activator inhibitor-1 in hospitalized COVID-19 patients. Sci. Rep. 2021, 11, 1580. [Google Scholar] [CrossRef]
- Kwaan, H.C.; Lindholm, P.F. The Central Role of Fibrinolytic Response in COVID-19-A Hematologist’s Perspective. Int. J. Mol. Sci. 2021, 22, 1283. [Google Scholar] [CrossRef]
- Magomedov, A.; Zickler, D.; Karaivanov, S.; Kurreck, A.; Münch, F.H.; Kamhieh-Milz, J.; Ferse, C.; Kahl, A.; Piper, S.K.; Eckardt, K.U.; et al. Viscoelastic testing reveals normalization of the coagulation profile 12 weeks after severe COVID-19. Sci. Rep. 2021, 11, 13325. [Google Scholar] [CrossRef]
- Hulshof, A.M.; Braeken, D.C.W.; Ghossein-Doha, C.; van Santen, S.; Sels, J.E.M.; Kuiper, G.J.A.J.; van der Horst, I.C.C.; Ten Cate, H.; van Bussel, B.C.T.; Olie, R.H.; et al. Hemostasis and fibrinolysis in COVID-19 survivors 6 months after intensive care unit discharge. Res. Prac. Thromb. Haemost. 2021, 5, e12579. [Google Scholar] [CrossRef]

| COVID-19 Patients (n = 29) | |
|---|---|
| Clinical category on admission to the hospital | |
| Asymptomatic | - |
| Hb saturation > 95% | 6 (20.69%) |
| Hb saturation 91–95% | 11 (37.93%) |
| Hb saturation < 90% | 12 (41.38%) |
| BMI | 29.95 ± 5.0 |
| WBC (×103/μL) | 6.235 (5.1; 8.05) |
| Monocytes (×103/μL) | 0.59 ± 0.17 |
| Lymphocytes (×103/μL) | 2.03 (1.53; 2.3) |
| PLT (×103/μL) | 232.91 ± 52.18 |
| MPV (μm3) | 10.4 (10; 11.4) |
| PDW | 11.8 (10.9; 13.8) |
| CRP (mg/L) | 39.75 (11.64; 113.85) |
| ALT (IU/L) | 25 (18; 40) |
| Creatinine (mg/L) | 0.92 (0.83; 1.33) |
| PT (s) | 12.3 (12; 13.1) |
| INR | 1.08 ± 0.08 |
| APTT (s) | 32.08 ± 3.23 |
| D-dimer | 696 (547; 1494) |
| Fibrinogen (mg/dL) | 549.41 ± 185.84 |
| Controls | COVID-19 | p | |
|---|---|---|---|
| NATEM® | |||
| CT (s) | 677 (618; 775) | 584 (513.5; 652.5) | 0.009 |
| CFT (s) | 202 (167; 237) | 146 (127; 188.5) | 0.0016 |
| MCF (mm) | 52 (50; 55) | 59 (54.5; 62.5) | <0.0001 |
| alpha (degrees) | 54.85 ± 7.87 | 60.96 ± 9.75 | 0.0136 |
| ML (%) | 9.93 ± 5.20 | 11.14 ± 4.82 | 0.3721 |
| CFR (degrees) | 62 (57; 67) | 68.5 (64.5; 73.5) | 0.0141 |
| MCE (dynes/cm2) | 108 (98; 125) | 142 (120.5; 167) | <0.0001 |
| EXTEM® | |||
| CT (s) | 68.5 (64; 75) | 72 (66; 82) | 0.0587 |
| CFT (s) | 80.5 (71; 94) | 73 (65; 83) | 0.1101 |
| MCF (mm) | 63.23 ± 3.38 | 64.93 ± 5.5 | 0.1613 |
| alpha (degrees) | 74 (71; 75) | 77 (76; 79) | 0.0002 |
| ML (%) | 10 (9; 14) | 10 (8; 13) | 0.6140 |
| CFR (degrees) | 76 (74; 78) | 78 (77; 80) | 0.0113 |
| MCE (dynes/cm2) | 173.97 ± 25.48 | 191.79 ± 48.05 | 0.0837 |
| FIBTEM® | |||
| MCF (mm) | 16 (14; 19) | 26.5 (22; 31) | <0.0001 |
| MCE (mm) | 18 (16; 23) | 36.5 (28; 45) | <0.0001 |
| A10 (mm) | 15.33 ± 3.25 | 23.77 ± 5.84 | <0.0001 |
| A20 (mm) | 16.47 ± 3.40 | 25.64 ± 6.95 | <0.0001 |
| Controls | COVID-19 | p | |
|---|---|---|---|
| TNF (pg/mL) | 1.32 (0.7; 3.21) | 6 (2.8; 17.87) | <0.0001 |
| IL-6 (pg/mL) | 1.32 (0.76; 2.25) | 45.65 (19.95; 199.76) | <0.0001 |
| IL-1B (pg/mL) | 0.06 (0.02; 0.08) | 1.43 (0.76; 4.23) | <0.0001 |
| IL-8 (pg/mL) | 0.54 (0.07; 1.2) | 16.68 (5.32; 44.67) | <0.0001 |
| IL-10 (pg/mL) | 0.25 (0.07; 0.65) | 10.56 (3.23; 32.2) | <0.0001 |
| IL-12p70 (pg/mL) | 0.12 (0.043; 0.43) | 2.76 (1.43; 7.98) | <0.0001 |
| Correlated Parameters | R | p | |
|---|---|---|---|
| CT severity index | FIBTEM MCF (mm) | 0.520923 | 0.012924 |
| FIBTEM MCE (mm) | 0.512226 | 0.014801 | |
| FIBTEM A10 (mm) | 0.483663 | 0.022573 | |
| FIBTEM A20 (mm) | 0.532274 | 0.010772 | |
| Characteristic | Coefficient | SE | p-Value | OR | 95% CI for OR |
|---|---|---|---|---|---|
| Death | |||||
| FIBTEM MCE | 2.81 | 0.05 | 0.094 | 1.09 | 0.99–1.20 |
| Constant | 5.24 | 2.67 | 0.022 | 0.01 | 0.01–0.42 |
| ICU/need for mechanical | |||||
| FIBTEM MCE | 2.88 | 0.05 | 0.0897 | 1.08 | 0.99–1.19 |
| Constant | 5.11 | 2.17 | 0.0248 | 0.01 | 0.01–0.52 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rogalski, P.; Rogalska, M.; Martonik, D.; Rusak, M.; Pawlus, J.; Chociej-Stypulkowska, J.; Dabrowska, M.; Flisiak, R. Rotational Thromboelastometry (ROTEM®) in Relation to Inflammatory Biomarkers and Clinical Outcome in COVID-19 Patients. J. Clin. Med. 2023, 12, 3919. https://doi.org/10.3390/jcm12123919
Rogalski P, Rogalska M, Martonik D, Rusak M, Pawlus J, Chociej-Stypulkowska J, Dabrowska M, Flisiak R. Rotational Thromboelastometry (ROTEM®) in Relation to Inflammatory Biomarkers and Clinical Outcome in COVID-19 Patients. Journal of Clinical Medicine. 2023; 12(12):3919. https://doi.org/10.3390/jcm12123919
Chicago/Turabian StyleRogalski, Pawel, Magdalena Rogalska, Diana Martonik, Malgorzata Rusak, Joanna Pawlus, Joanna Chociej-Stypulkowska, Milena Dabrowska, and Robert Flisiak. 2023. "Rotational Thromboelastometry (ROTEM®) in Relation to Inflammatory Biomarkers and Clinical Outcome in COVID-19 Patients" Journal of Clinical Medicine 12, no. 12: 3919. https://doi.org/10.3390/jcm12123919
APA StyleRogalski, P., Rogalska, M., Martonik, D., Rusak, M., Pawlus, J., Chociej-Stypulkowska, J., Dabrowska, M., & Flisiak, R. (2023). Rotational Thromboelastometry (ROTEM®) in Relation to Inflammatory Biomarkers and Clinical Outcome in COVID-19 Patients. Journal of Clinical Medicine, 12(12), 3919. https://doi.org/10.3390/jcm12123919







