Tentacle Mesh for Fixation-Free Spigelian Hernia Repair: Mini-Invasive Approach Granting Broad Defect Overlap
Abstract
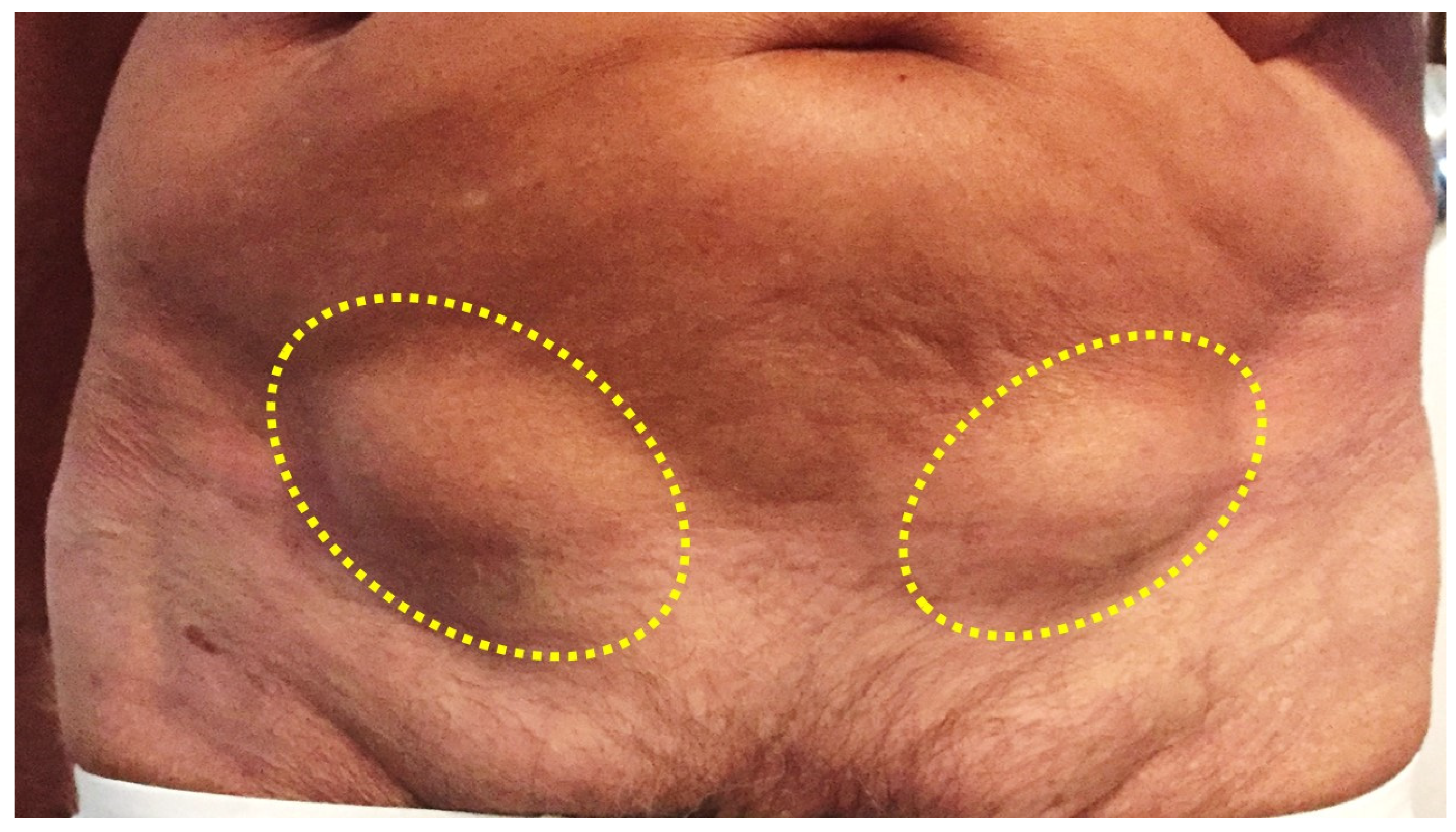
1. Introduction
2. Material and Methods
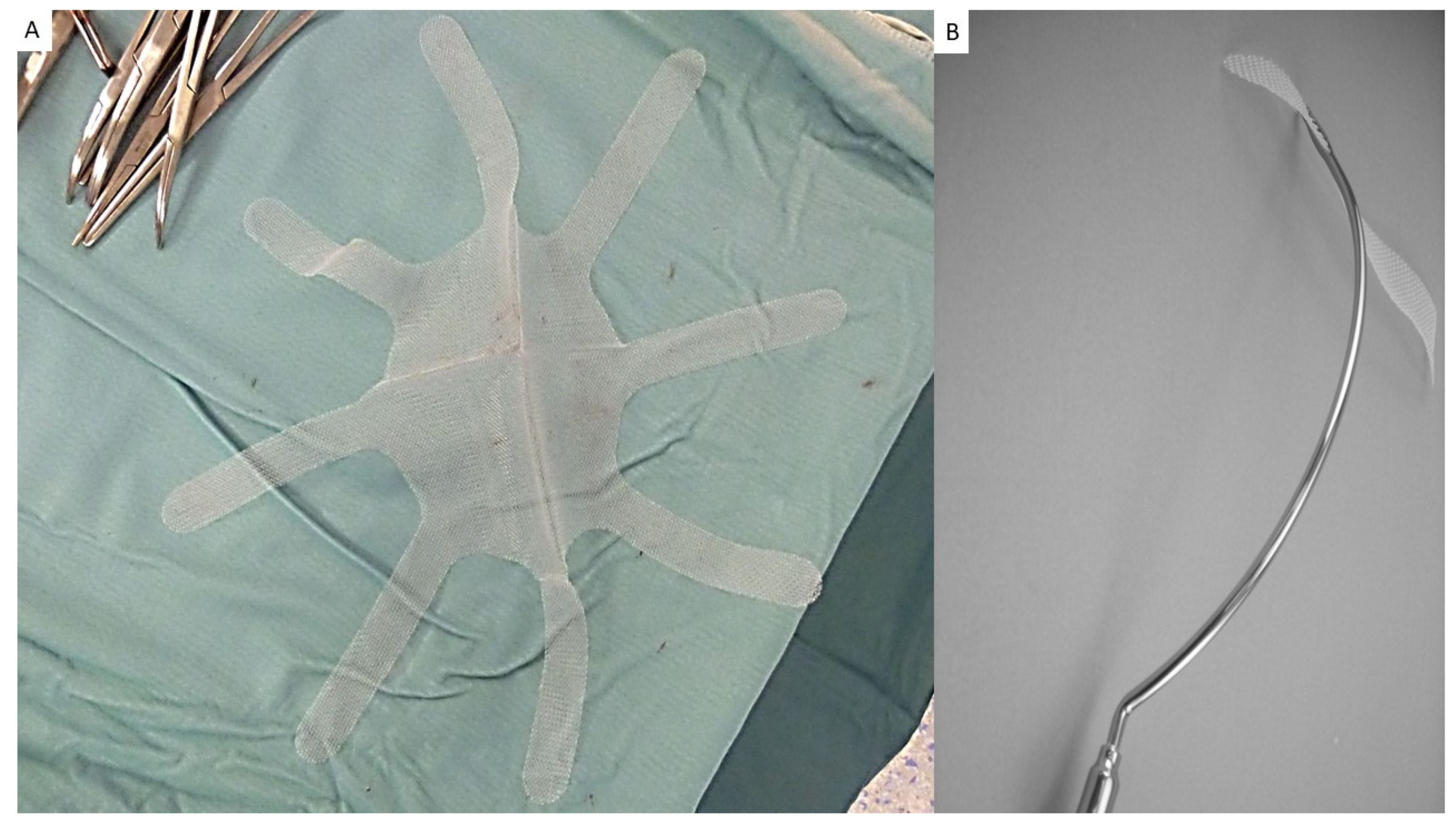
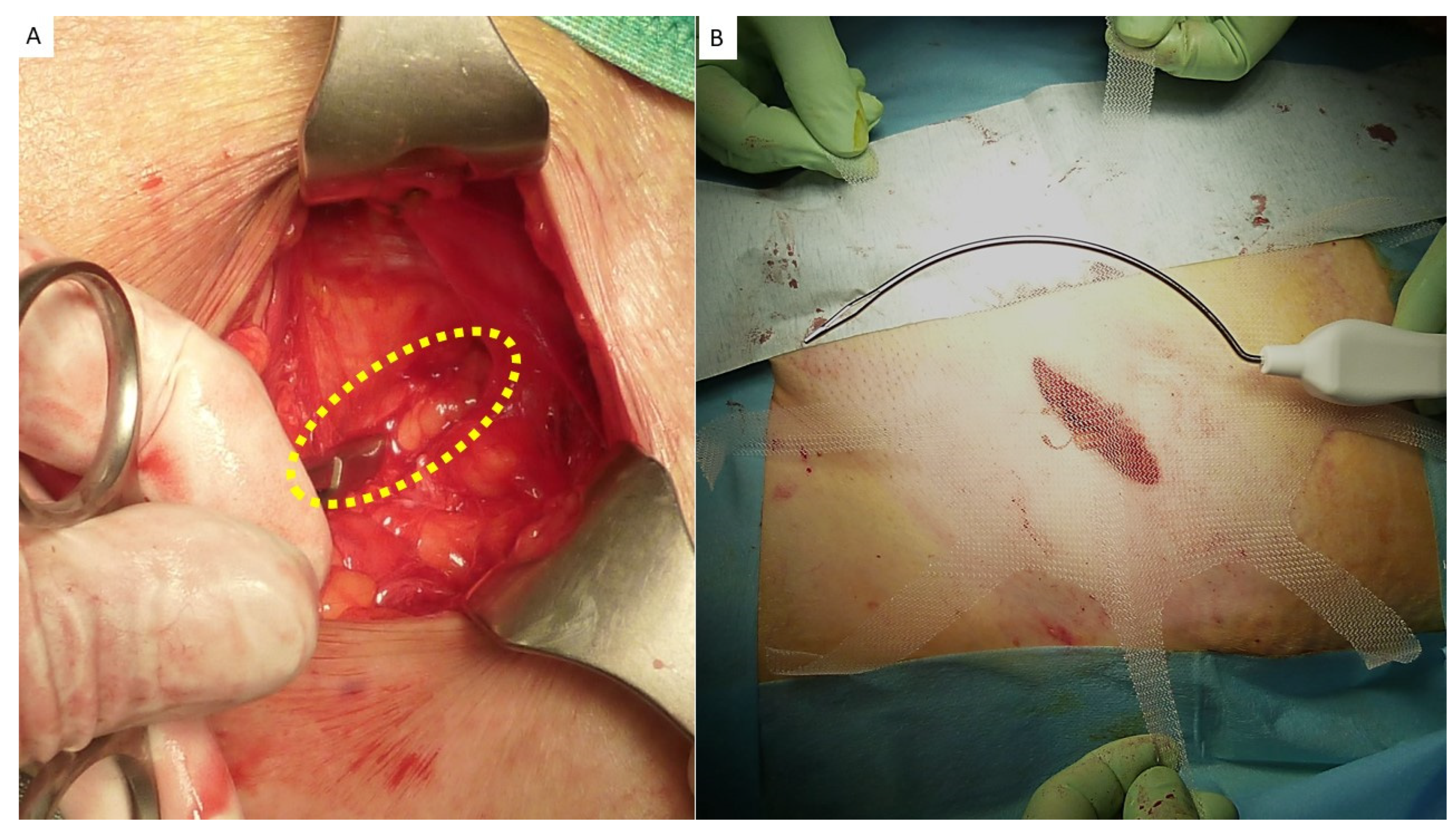
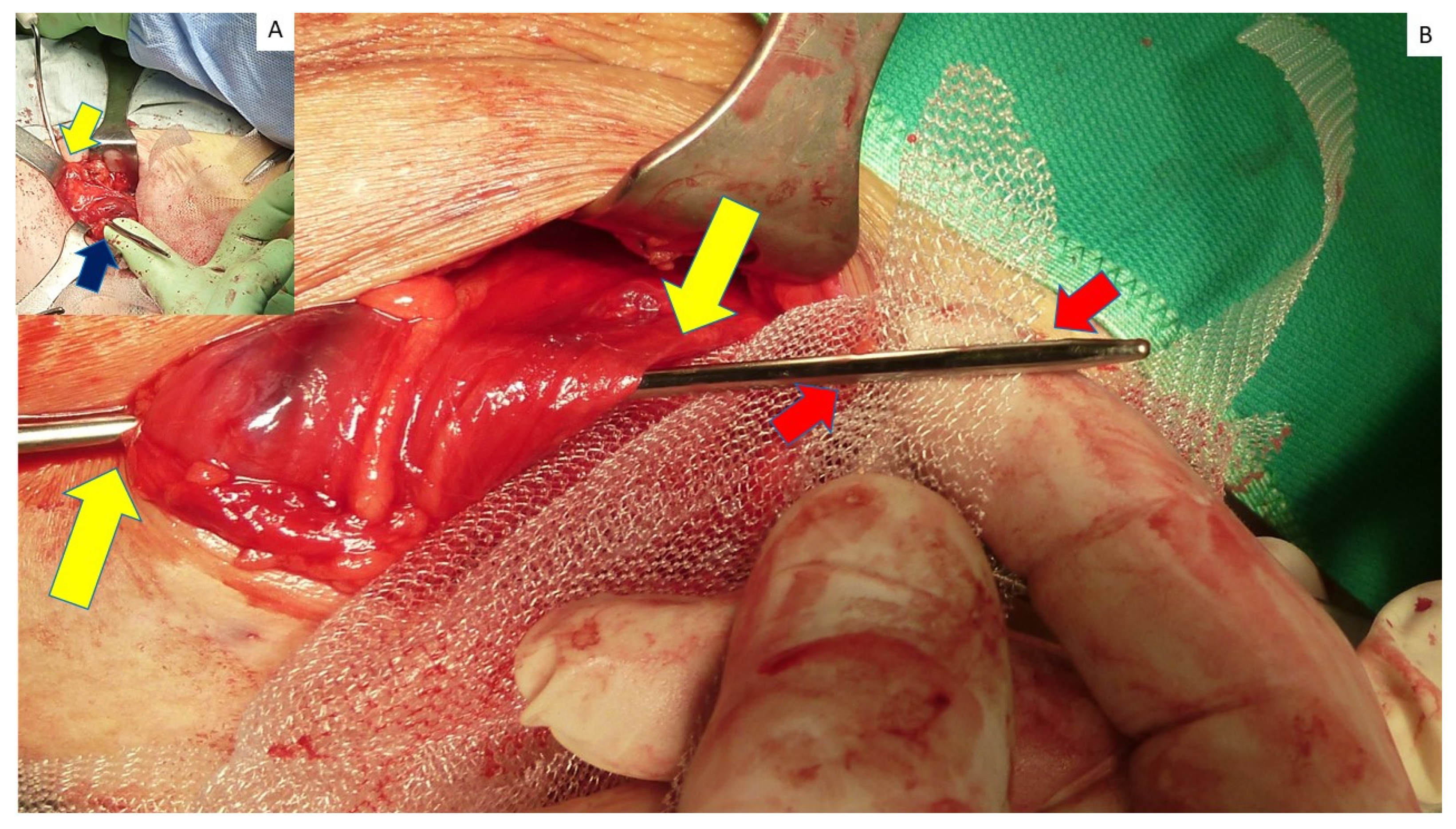
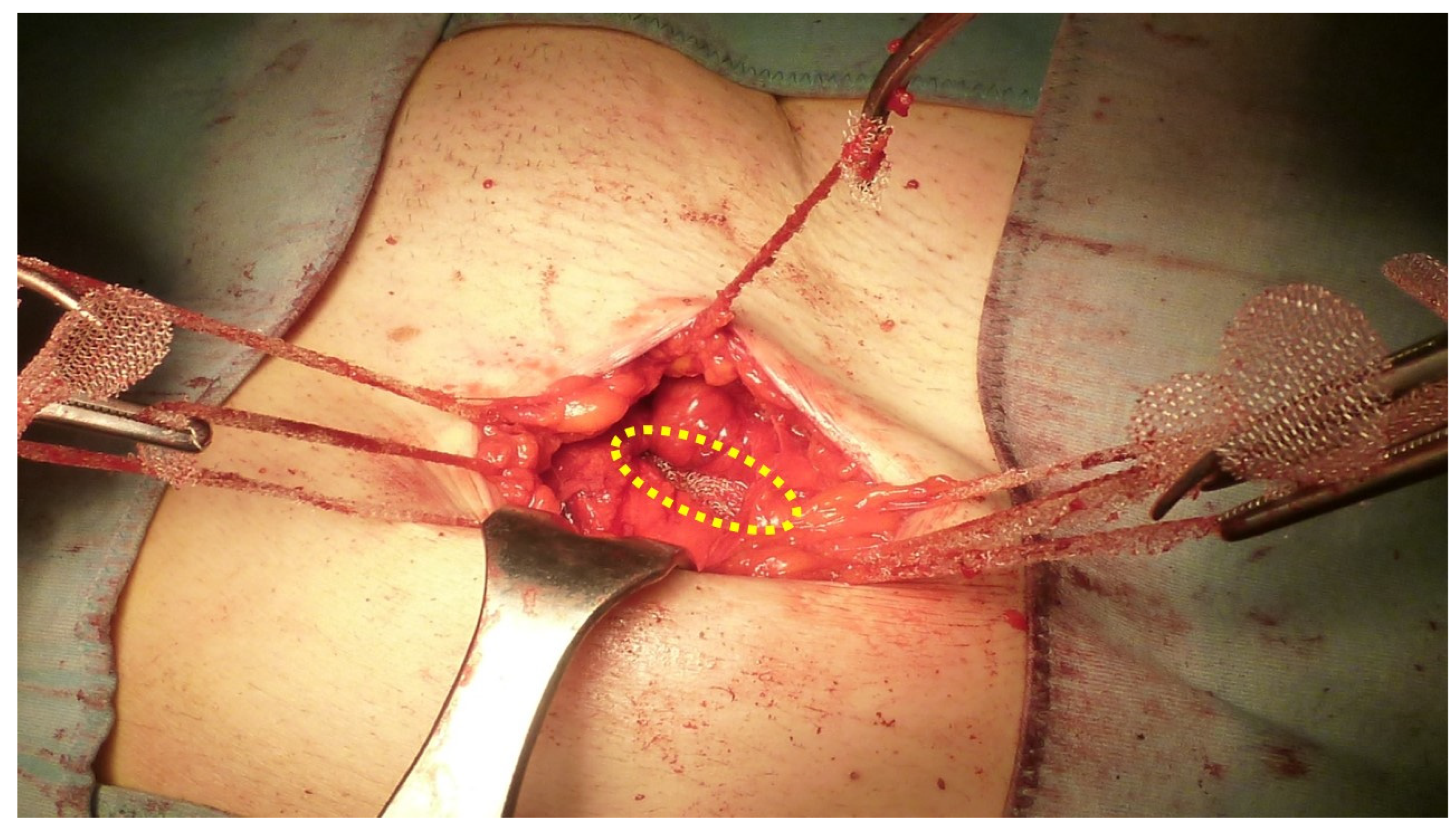
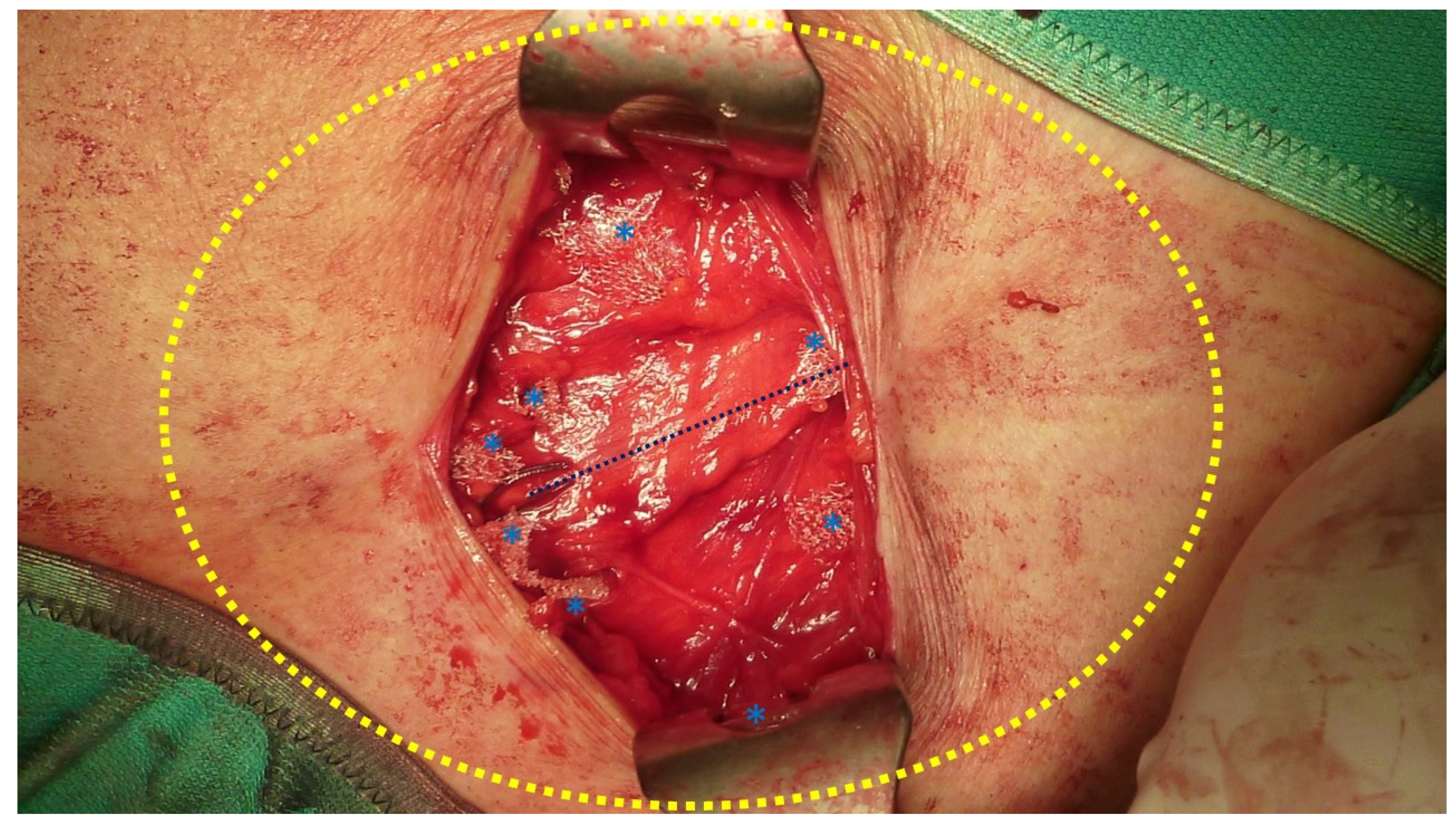
2.1. The Device
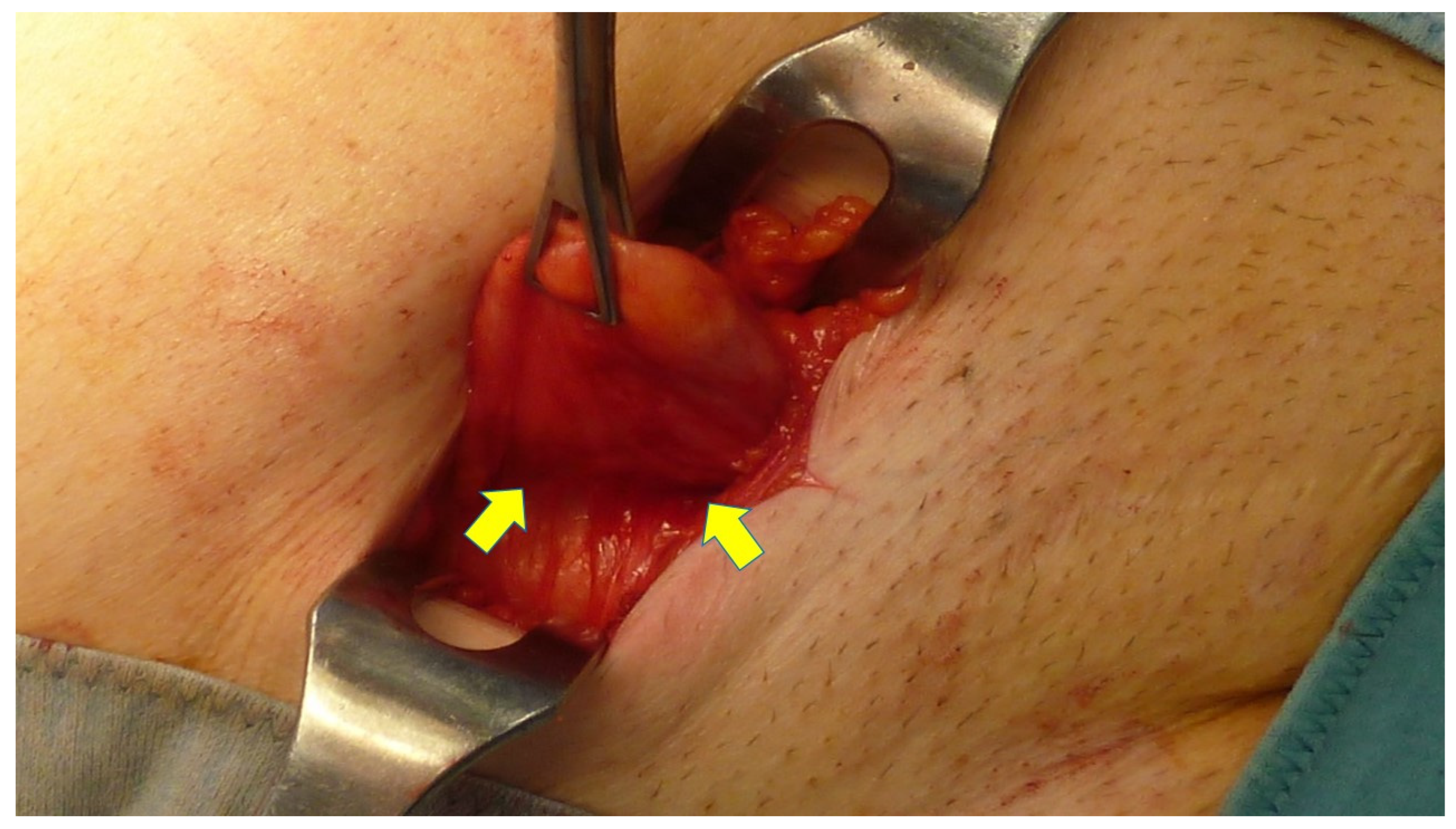
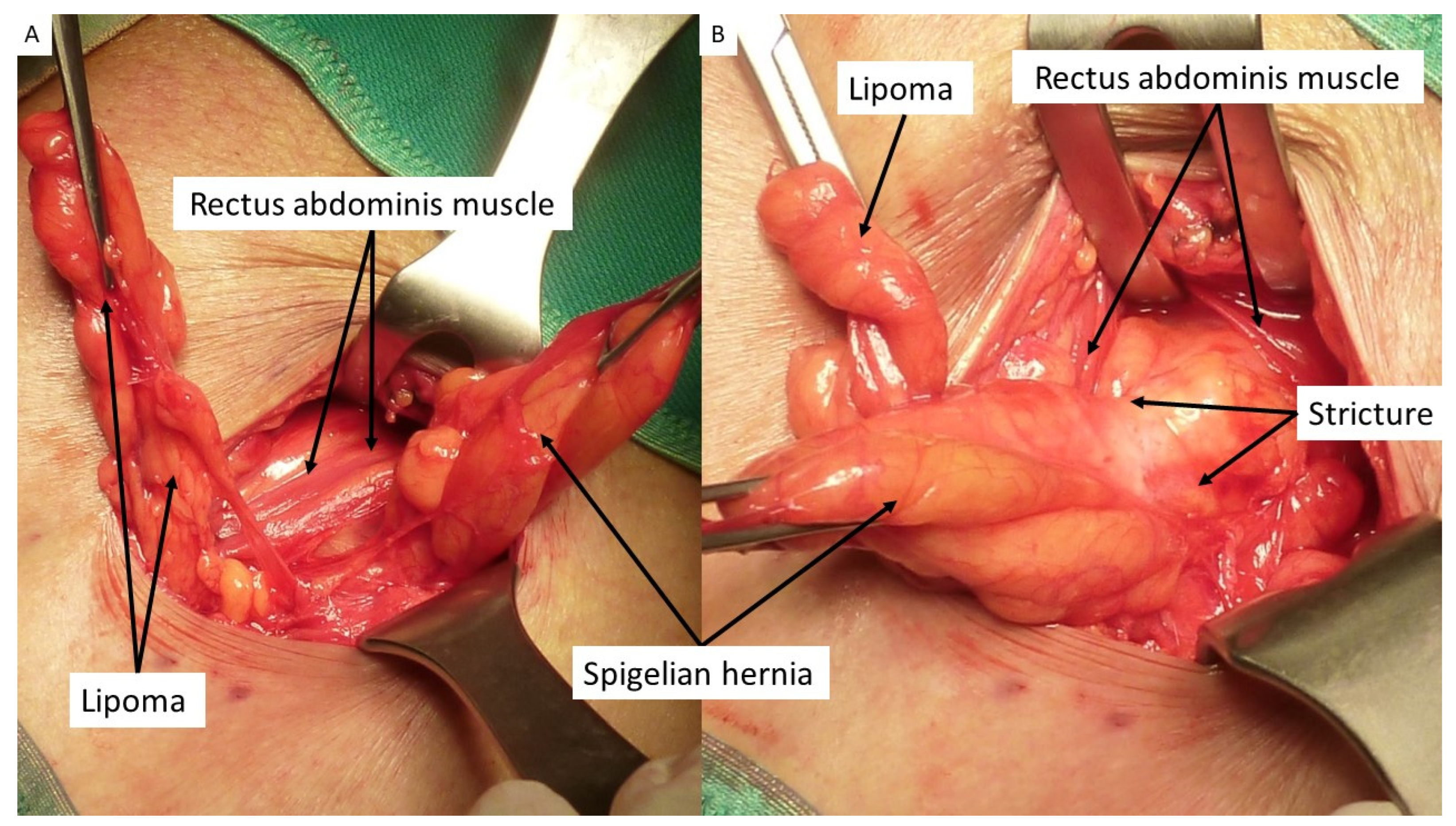
2.2. Procedural Steps
2.3. Follow-Up Protocol
3. Results
4. Discussion
5. Conclusions
- (a)
- Simplified mini-invasive procedure with a fully fixation-free implant deployment;
- (b)
- Wide overlap of the hernia defect ensuring a broad coverage of the posterior abdominal wall;
- (c)
- Short duration of the surgical procedure with the absence of intraoperative complications;
- (d)
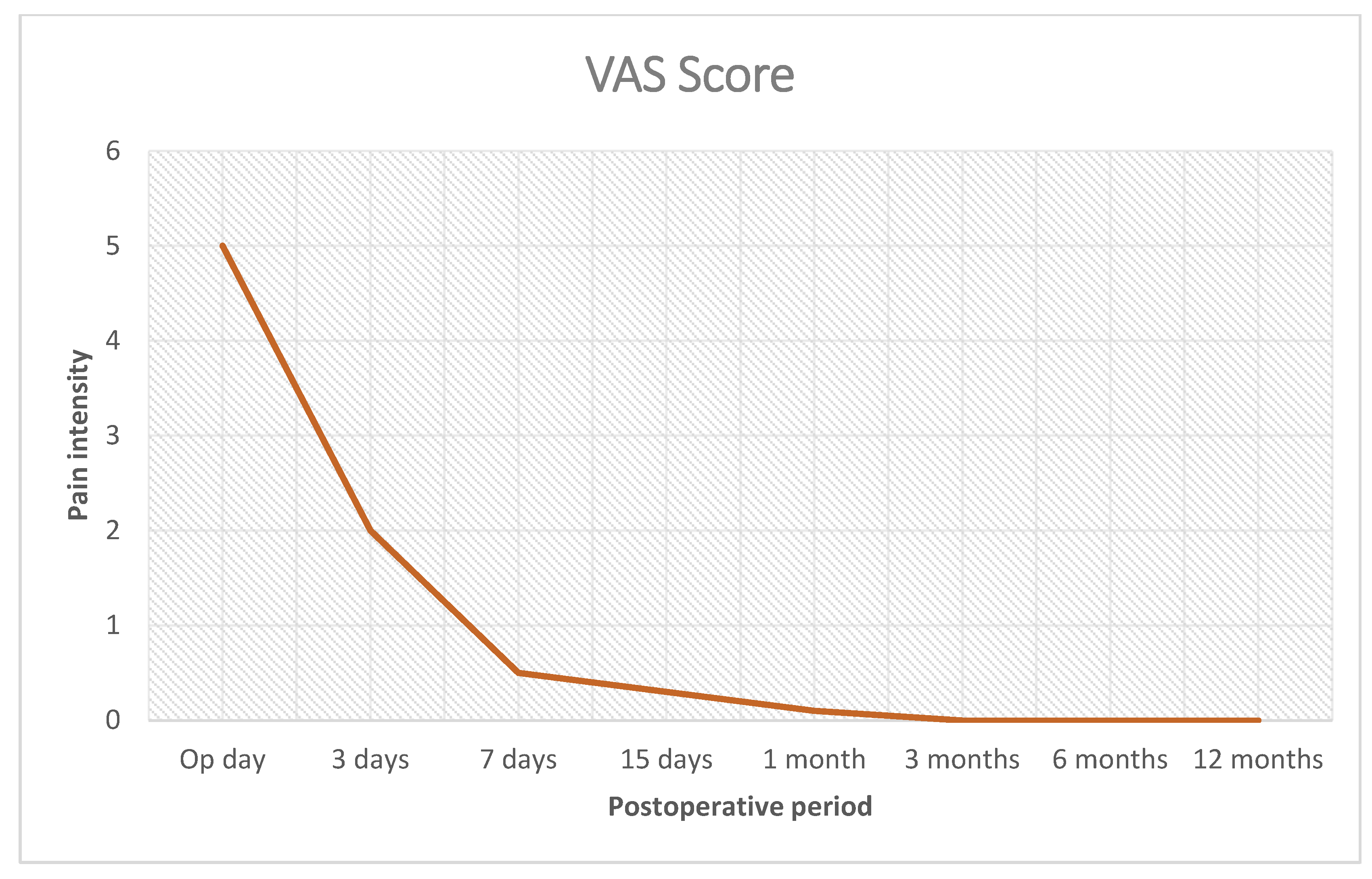
- Minimal pain allowing for an outpatient system procedure and quick return to daily activities;
- (e)
- Negligible rate of postoperative complications; no chronic pain;
- (f)
- Easy postoperative US detection of the implant elements in light of recurrence prediction.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Larson, D.W.; Farley, D.R. Spigelian Hernias: Repair and Outcome for 81 Patients. World J. Surg. 2002, 26, 1277–1281. [Google Scholar] [CrossRef] [PubMed]
- Skandalakis, P.N.; Zoras, O.; Skandalakis, J.E.; Mirilas, P. Spigelian hernia: Surgical anatomy, embryology, and technique of repair. Am. Surg. 2006, 72, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Pichi Graziani, M.; Pacifico, G.; Landi, L.; Corsi, A.; Rizzo, D.M.; Senesi, S.; Freschi, G. Spigelian hernia: Anatomo-clinical considerations. Minerva Chir. 1999, 54, 425–431. [Google Scholar] [PubMed]
- Polistina, F.A.; Garbo, G.; Trevisan, P.; Frego, M. Twelve years of experience treating Spigelian hernia. Surgery 2015, 157, 547–550. [Google Scholar] [CrossRef]
- Morenilla, L.M.; Durántez, F.D.; Robles, J.M.; Frutos, R.D.Q. Spigelian hernia in Spain: An analysis of 162 cases. Rev. Esp. Enferm. Dig. 2005, 97, 338–347. [Google Scholar] [CrossRef]
- Moreno-Egea, A.; Flores, B.; Girela, E.; Martín, J.G.; Aguayo, J.L.; Canteras, M. Spigelian hernia: Bibliographical study and presentation of a series of 28 patients. Hernia 2002, 6, 167–170. [Google Scholar] [CrossRef]
- Artioukh, D.Y.; Walker, S.J. Spigelian herniae: Presentation, diagnosis and treatment. J. R. Coll. Surg. Edinb. 1996, 41, 241–243. [Google Scholar]
- Sanchez-Montes, I.; Deysine, M. Spigelian Hernias: A new repair technique using preshaped polypropylene umbrella plugs. Arch. Surg. 1998, 133, 670–672. [Google Scholar] [CrossRef]
- Slakey, D.R.; Teplitsky, S.; Cheng, S.S. Incarcerated Spigelian hernia following laparoscopic living-donor nephrectomy. JSLS J. Soc. Laparoendosc. Surg. 2002, 6, 217–219. [Google Scholar]
- Spangen, L. Spigelian hernia. World J. Surg. 1989, 13, 573–580. [Google Scholar] [CrossRef]
- Bilici, S.; Güneş, M.; Göksu, M.; Melek, M.; Pirinçci, N. Undescended testis accompanying congenital Spigelian hernia: Is it a reason, a result, or a new syndrome? Eur. J. Pediatr. Surg. Off. J. Austrian Assoc. Pediatr. Surg. = Zeitschrift fur Kinderchirurgie 2012, 22, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Inan, M.; Basaran, U.N.; Aksu, B.; Dortdogan, Z.; Dereli, M. Congenital Spigelian hernia associated with undescended testis. World J. Pediatr. 2011, 8, 185–187. [Google Scholar] [CrossRef]
- Kelly, M.E.; Courtney, D.; McDermott, F.D.; Heeney, A.; Maguire, D.; Geoghegan, J.G.; Winter, D.C. Laparoscopic Spigelian Hernia Repair: A Series of 40 Patients. Surg. Laparosc. Endosc. Percutaneous Tech. 2015, 25, e86–e89. [Google Scholar] [CrossRef] [PubMed]
- Subramanya, M.S.; Chakraborty, J.; Memon, B.; Memon, M.A. Emergency Intraperitoneal Onlay Mesh Repair of Incarcerated Spigelian Hernia. JSLS J. Soc. Laparosc. Robot. Surg. 2010, 14, 275–278. [Google Scholar] [CrossRef] [PubMed]
- Lavin, A.; Gupta, A.; Lopez-Viego, M.; Buicko, J.L. Incarcerated Spigelian Hernias: A Rare Cause of a High-grade Small Bowel Obstruction. Cureus 2020, 12, e7397. [Google Scholar] [CrossRef]
- Skouras, C.; Purkayastha, S.; Jiao, L.; Tekkis, P.; Darzi, A.; Zacharakis, E. Laparoscopic Management of Spigelian Hernias. Surg. Laparosc. Endosc. Percutaneous Tech. 2011, 21, 76–81. [Google Scholar] [CrossRef]
- Bisgaard, T.; Kehlet, H.; Bay-Nielsen, M.; Iversen, M.G.; Rosenberg, J.; Jørgensen, L.N. A nationwide study on readmission, morbidity, and mortality after umbilical and epigastric hernia repair. Hernia 2011, 15, 541–546. [Google Scholar] [CrossRef]
- Amato, G.; Romano, G.; Agrusa, A.; Cassata, G.; Salamone, G.; Gulotta, G. Prosthetic strap system for simplified ventral hernia repair: Results of a porcine experimental model. Hernia 2010, 14, 389–395. [Google Scholar] [CrossRef]
- Amato, G.; Romano, G.; Goetze, T.; Salamone, G.; Agrusa, A.; Gulotta, G.; Paolucci, V. New mesh shape and improved implantation procedure to simplify and standardize open ventral hernia repair: A preliminary report. Hernia 2011, 15, 659–665. [Google Scholar] [CrossRef]
- Romano, G.; Calò, P.G.; Erdas, E.; Medas, F.; Gordini, L.; Podda, F.; Amato, G. Fixation-free incisional hernia repair in the elderly: Our experience with a tentacle-shaped implant. Aging Clin. Exp. Res. 2016, 29, 173–177. [Google Scholar] [CrossRef]
- Amato, G.; Romano, G.; Goetze, T.; Gordini, L.; Erdas, E.; Medas, F.; Calò, P. Long-Term Results of Fixation-Free Incisional Hernia Repair Using a Tentacle-Shaped Implant. Surg. Technol. Online 2017, 30, 175–181. [Google Scholar]
- Amato, G.; Romano, G.; Agrusa, A.; Canu, G.L.; Gulotta, E.; Erdas, E.; Calò, P.G. Tentacle-shaped mesh for fixation-free repair of umbilical hernias. Hernia 2019, 23, 801–807. [Google Scholar] [CrossRef]
- Welty, G.; Klinge, U.; Klosterhalfen, B.; Kasperk, R.; Schumpelick, V. Functional impairment and complaints following incisional hernia repair with different polypropylene meshes. Hernia 2001, 5, 142–147. [Google Scholar] [PubMed]
- Awad, Z.T.; Puri, V.; LeBlanc, K.; Stoppa, R.; Fitzgibbons, R.J., Jr.; Iqbal, A.; Filipi, C.J. Mechanisms of ventral vernia recurrence after mesh repair and a new proposed classification. J. Am. Coll. Surg. 2005, 201, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Fatton, B.; Amblard, J.; Debodinance, P.; Cosson, M.; Jacquetin, B. Transvaginal repair of genital prolapse: Preliminary results of a new tension-free vaginal mesh (Prolift™ technique)—A case series multicentric study. Int. Urogynecol. J. 2006, 18, 743–752. [Google Scholar] [CrossRef]
- Altman, D.; Väyrynen, T.; Engh, M.E.; Axelsen, S.; Falconer, C. For the Nordic Transvaginal Mesh Group Short-term outcome after transvaginal mesh repair of pelvic organ prolapse. Int. Urogynecol. J. 2007, 19, 787–793. [Google Scholar] [CrossRef]
- Abdel-Fattah, M.; Ramsay, I. West of Scotland Study Group Retrospective multicentre study of the new minimally invasive mesh repair devices for pelvic organ prolapse. BJOG Int. J. Obstet. Gynaecol. 2007, 115, 22–30. [Google Scholar] [CrossRef]
- Malik, B.; Lambaudie, E.; Collinet, P.; Dubois, P.; Cosson, M. Mechanical resistance of syntetic meshes for incontinence or polapse surgery. Int. Urogynecol. J. 2007, 18, 183–187. [Google Scholar]
- Alcalay, M.; Livne, M.; Shidlovsky, D.; Hod, E. Pullout force of polypropylene mesh deployed by endofast reliant fastener—A comparative study in a sheep model. ICS Congress Abstract 543. Thursday 1st October 2009. Available online: https://www.ics.org/Abstracts/Publish/47/ScientificProgramme.pdf (accessed on 2 June 2023).
- Katkhouda, N.; Mavor, E.; Friedlander, M.H.; Mason, R.J.; Kiyabu, M.; Grant, S.W.; Achanta, K.; Kirkman, E.L.; Narayanan, K.; Essani, R. Use of Fibrin Sealant for Prosthetic Mesh Fixation in Laparoscopic Extraperitoneal Inguinal Hernia Repair. Ann. Surg. 2001, 233, 18–25. [Google Scholar] [CrossRef]
- Pascual, G.; Sotomayor, S.; Rodriguez, M.; Pérez-Köhler, B.; Kühnhardt, A.; Fernández-Gutiérrez, M.; San Román, J.; Bellón, J.M. Cytotoxicity of cyanoacrylate-based tissue adhesives and short term preclinical in vivo biocompatibility in abdominal hernia repair. PLoS ONE 2016, 11, e0157920. [Google Scholar] [CrossRef]
- Schmedt, C.G.; Sauerland, S.; Bittner, R. Comparison of endoscopic procedure vs Lichtenstein and other open mesh techniques for inguinal hernia repair: A meta-analysis of randomized controlled trials. Surg. Endosc. 2005, 19, 188–189. [Google Scholar] [CrossRef] [PubMed]
- Peach, G.; Tan, L.C. Small bowel obstruction and perforation due to a displaced spiral tacker: A rare complication of laparoscopic inguinal hernia repair. Hernia 2007, 12, 303–305. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, H.L.; Orenstein, S.B.; Novitsky, Y.W. Small Bowel Obstruction Owing to Displaced Spiral Tack After Laparoscopic TAPP Inguinal Hernia Repair. Surg. Laparosc. Endosc. Percutaneous Tech. 2010, 20, e132–e135. [Google Scholar] [CrossRef]
- Haltmeier, T.; Groebli, Y. Small bowel lesion due to spiral tacks after laparoscopic intraperitoneal onlay mesh repair for incisional hernia. Int. J. Surg. Case Rep. 2013, 4, 283–285. [Google Scholar] [CrossRef] [PubMed]
| Patient Characteristics | Hernia Types |
|---|---|
| Number of patients: 54 (24 male–30 female) | Primary Spigelian hernia: 48 (7 incarcerated) |
| Mean BMI: 27.40 (24–31) | Recurrent Spigelian hernia: 6 (2 multi-recurrent–1 incarcerated) |
| Mean age: 64 years (53–76) | Mean hernia defect size: 2.5 cm (1.5–3 cm) |
| Procedure Details | |
|---|---|
| Anesthesia | Local: 45 General: 9 |
| Mean mesh overlap | 6 cm (5–7 cm) |
| Time needed for mesh placement and strap positioning | Mean: 6 min (range 4–8 min) |
| Hospital stay | |
| Uncomplicated patients: 46 | 1 day |
| Patients with incarcerated hernias: 8 | 2 days |
| Postoperative Complications Mean Follow-Up Length: 64 Months (6–84 Months) | |
|---|---|
| Wound infection | 0 (0%) |
| Seroma | 4 |
| Recurrence | 0 (0%) |
| Total complication rate | 7.41% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amato, G.; Agrusa, A.; Buscemi, S.; Di Buono, G.; Calò, P.G.; Vella, R.; Romano, G.; Barletta, G.; Cassata, G.; Cicero, L.; et al. Tentacle Mesh for Fixation-Free Spigelian Hernia Repair: Mini-Invasive Approach Granting Broad Defect Overlap. J. Clin. Med. 2023, 12, 3866. https://doi.org/10.3390/jcm12123866
Amato G, Agrusa A, Buscemi S, Di Buono G, Calò PG, Vella R, Romano G, Barletta G, Cassata G, Cicero L, et al. Tentacle Mesh for Fixation-Free Spigelian Hernia Repair: Mini-Invasive Approach Granting Broad Defect Overlap. Journal of Clinical Medicine. 2023; 12(12):3866. https://doi.org/10.3390/jcm12123866
Chicago/Turabian StyleAmato, Giuseppe, Antonino Agrusa, Salvatore Buscemi, Giuseppe Di Buono, Pietro Giorgio Calò, Roberta Vella, Giorgio Romano, Gabriele Barletta, Giovanni Cassata, Luca Cicero, and et al. 2023. "Tentacle Mesh for Fixation-Free Spigelian Hernia Repair: Mini-Invasive Approach Granting Broad Defect Overlap" Journal of Clinical Medicine 12, no. 12: 3866. https://doi.org/10.3390/jcm12123866
APA StyleAmato, G., Agrusa, A., Buscemi, S., Di Buono, G., Calò, P. G., Vella, R., Romano, G., Barletta, G., Cassata, G., Cicero, L., & Romano, G. (2023). Tentacle Mesh for Fixation-Free Spigelian Hernia Repair: Mini-Invasive Approach Granting Broad Defect Overlap. Journal of Clinical Medicine, 12(12), 3866. https://doi.org/10.3390/jcm12123866







