Efficacy of Residual Site Radiation Therapy (ISRT) in Patients with Primary Mediastinal Lymphoma with Deauville Score 4 Following R-CHT: Results of a Retrospective Mono Institutional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Chemotherapy
2.3. Radiation Therapy
2.4. Follow-Up
2.5. Statistical Analysis
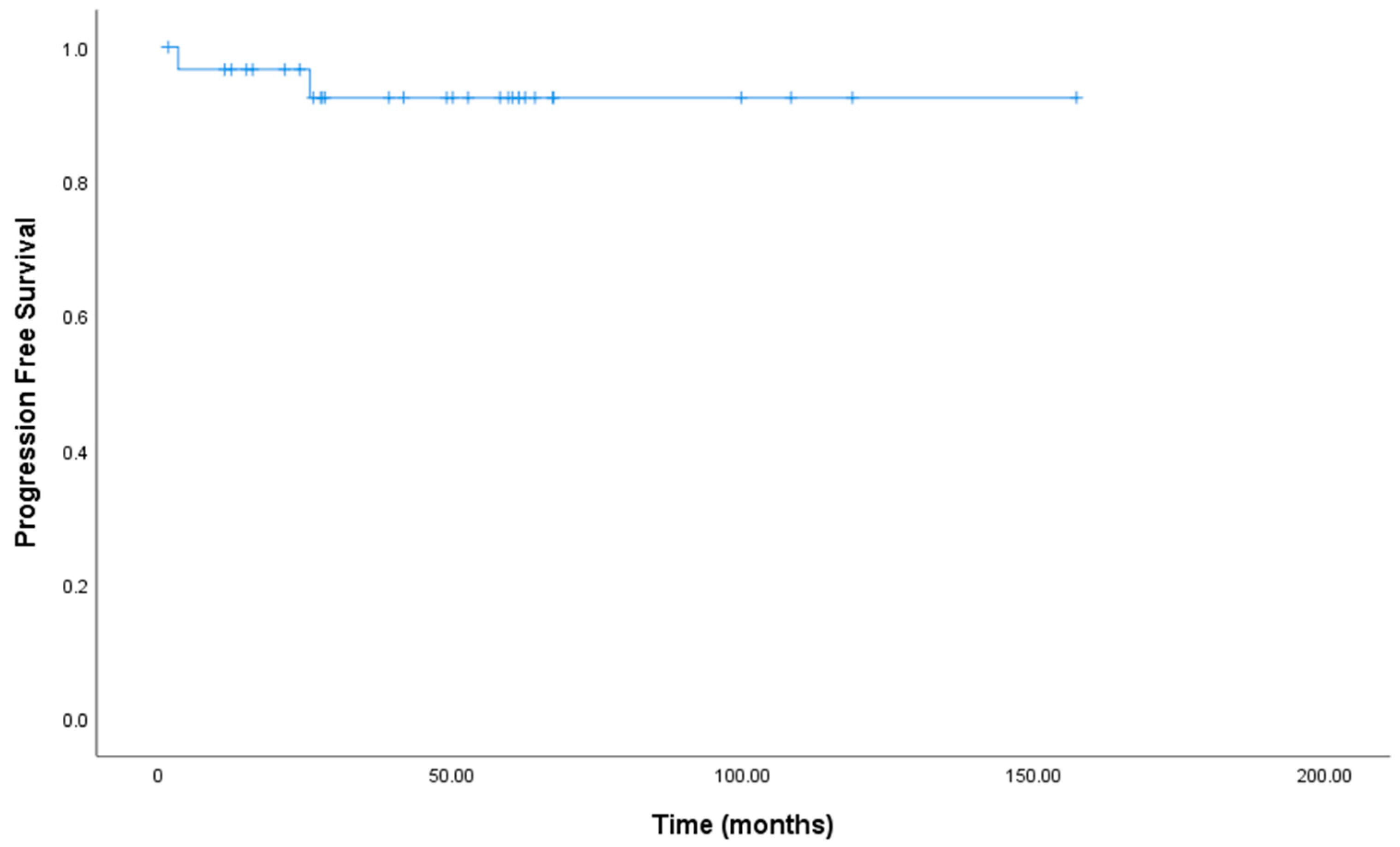
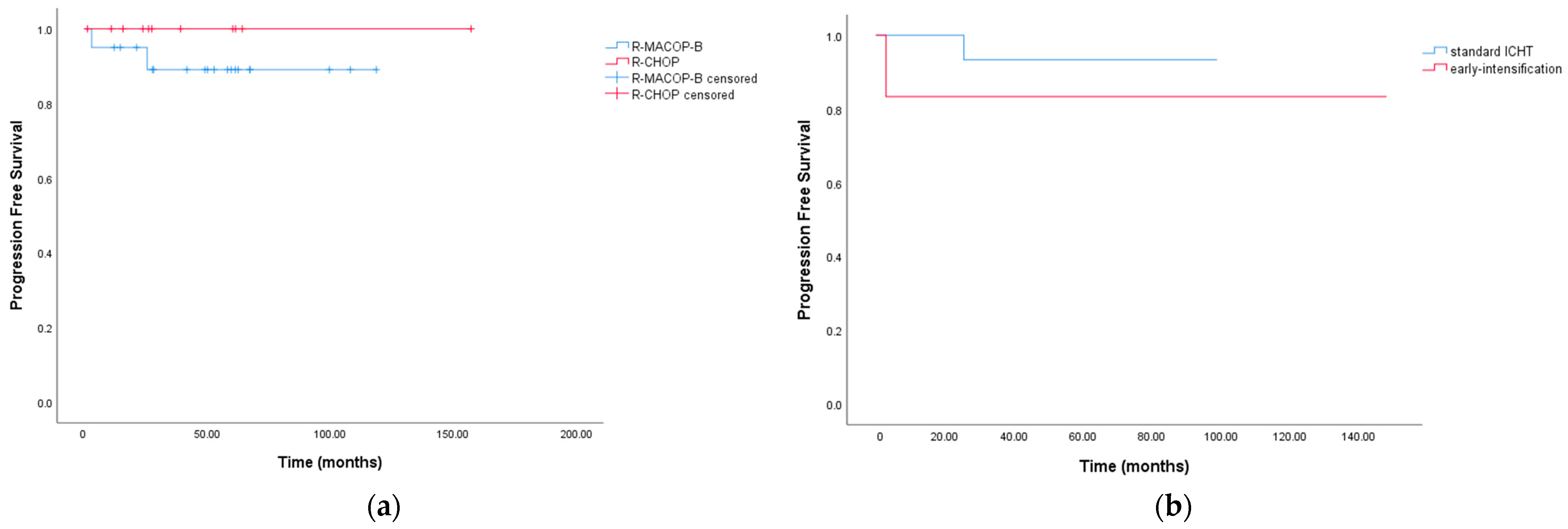
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chen, H.; Pan, T.; He, Y.; Zeng, R.; Li, Y.; Yi, L.; Zang, H.; Chen, S.; Duan, Q.; Xiao, L.; et al. Primary Mediastinal B-Cell Lymphoma: Novel Precision Therapies and Future Directions. Front. Oncol. 2021, 11, 654854. [Google Scholar] [CrossRef] [PubMed]
- De Sanctis, V.; DI Rocco, A.; Cox, M.C.; Valeriani, M.; Congedi, F.P.; Anzellini, D.; Massaro, M.; Vullo, G.; Facondo, G.; De Giacomo, F.; et al. Residual Site Radiotherapy After Immunochemotherapy in Primary Mediastinal B-Cell Lymphoma: A Monoinstitutional Retrospective Study. In Vivo 2020, 34, 1407–1413. [Google Scholar] [CrossRef] [PubMed]
- Martelli, M.; Di Rocco, A.; Russo, E.; Perrone, S.; Foà, R. Primary mediastinal lymphoma: Diagnosis and treatment options. Expert. Rev. Hematol. 2015, 8, 173–186. [Google Scholar] [CrossRef] [PubMed]
- Cwynarski, K.; Marzolini, M.A.V.; Barrington, S.F.; Follows, G.; Illidge, T.; Stern, S.; Davies, A.; British Society for Haematology Guideline. The management of primary mediastinal B-cell lymphoma: A British Society for Haematology Good Practice Paper. Br. J. Haematol. 2019, 185, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Cheson, B.D.; Fisher, R.I.; Barrington, S.F.; Cavalli, F.; Schwartz, L.H.; Zucca, E.; Lister, T.A. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: The Lugano classification. J. Clin. Oncol. 2014, 32, 3059–3068. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: B-Cell Lymphomas; National Comprehensive Cancer Network: Fort Washington, PA, USA, 2022; Available online: https://www.nccn.org/professionals/physician_gls/pdf/b-cell.pdf (accessed on 10 February 2023).
- Pinnix, C.; Dabaja, B.; Ahmed, M.; Chuang, H.H.; Costelloe, C.; Wogan, C.F.; Reed, V.; Romaguera, J.E.; Neelapu, S.; Oki, Y.; et al. Single-institution experience in the treatment of primary mediastinal B cell lymphoma treated with immunochemotherapy in the setting of response assessment by 18fluorodeoxyglucose positron emission tomography. Int. J. Radiat. Oncol. Biol. Phys. 2015, 92, 113–121. [Google Scholar] [CrossRef]
- Giulino-Roth, L.; O’Donohue, T.; Chen, Z.; Bartlett, N.L.; LaCasce, A.; Martin-Doyle, W.; Barth, M.J.; Davies, K.; Blum, K.A.; Christian, B.; et al. Outcomes of adults and children with primary mediastinal B-cell lymphoma treated with dose-adjusted EPOCH-R. Br. J. Haematol. 2017, 179, 739–747. [Google Scholar] [CrossRef]
- Filippi, A.R.; Piva, C.; Levis, M.; Chiappella, A.; Caracciolo, D.; Bellò, M.; Bisi, G.; Vitolo, U.; Ricardi, U. Prognostic Role of Pre-Radiation Therapy (18)F-Fluorodeoxyglucose Positron Emission Tomography for Primary Mediastinal B-Cell Lymphomas Treated with R-CHOP or R-CHOP-Like Chemotherapy Plus Radiation. Int. J. Radiat. Oncol. Biol. Phys. 2016, 95, 1239–1243. [Google Scholar] [CrossRef]
- Vassilakopoulos, T.P.; Pangalis, G.A.; Chatziioannou, S.; Papageorgiou, S.; Angelopoulou, M.K.; Galani, Z.; Kourti, G.; Prassopoulos, V.; Leonidopoulou, T.; Terpos, E.; et al. PET/CT in primary mediastinal large B-cell lymphoma responding to rituximab-CHOP: An analysis of 106 patients regarding prognostic significance and implications for subsequent radiotherapy. Leukemia. 2016, 30, 238–242. [Google Scholar] [CrossRef]
- Hoppe, B.S.; Advani, R.; Milgrom, S.A.; Bakst, R.L.; Ballas, L.K.; Dabaja, B.S.; Flowers, C.R.; Ha, C.S.; Mansur, D.B.; Metzger, M.L.; et al. Primary Mediastinal B Cell Lymphoma in the Positron-Emission Tomography Era Executive Summary of the American Radium Society Appropriate Use Criteria. Int. J. Radiat. Oncol. Biol. Phys. 2021, 111, 36–44. [Google Scholar] [CrossRef]
- Cox, J.D.; Stetz, J.; Pajak, T.F. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int. J. Radiat. Oncol. Biol. Phys. 1995, 31, 1341–1346. [Google Scholar] [CrossRef] [PubMed]
- Hosein, P.J.; Lossos, I.S. The evolving role of F-FDG PET scans in patients with aggressive non-Hodgkin’s lymphoma. Eur. J. Clin. Med. Oncol. 2010, 2, 131–138. [Google Scholar]
- Barrington, S.F.; Mikhaeel, N.G.; Kostakoglu, L.; Meignan, M.; Hutchings, M.; Müeller, S.P.; Schwartz, L.H.; Zucca, E.; Fisher, R.I.; Trotman, J.; et al. Role of imaging in the staging and response assessment of lymphoma: Consensus of the International Conference on Malignant Lymphomas Imaging Working Group. J. Clin. Oncol. 2014, 32, 3048–3058, Published Correction Appears in J. Clin. Oncol. 2016, 34, 2562. [Google Scholar] [CrossRef] [PubMed]
- Haioun, C.; Itti, E.; Rahmouni, A.; Brice, P.; Rain, J.-D.; Belhadj, K.; Gaulard, P.; Garderet, L.; Lepage, E.; Reyes, F.; et al. [18F] fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) in aggressive lymphoma: An early prognostic tool for predicting patient outcome. Blood 2005, 106, 1376–1381. [Google Scholar] [CrossRef] [PubMed]
- Dupuis, J.; Gaulard, P.; Hemery, F.; Itti, E.; Gisselbrecht, C.; Rahmouni, A.; Copie-Bergman, C.; Brière, J.; El Gnaoui, T.; Gaillard, I.; et al. Respective prognostic values of germinal center phenotype and early (18)fluorodeoxyglucose-positron emission tomography scanning in previously untreated patients with diffuse large B-cell lymphoma. Haematologica 2007, 92, 778–783. [Google Scholar] [CrossRef]
- Kong, Y.; Qu, L.; Li, Y.; Liu, D.; Lv, X.; Han, J. Predictive Significance of a New Prognostic Score for Patients with Diffuse Large B-Cell Lymphoma in the Interim-Positron Emission Tomography Findings. Medicine 2016, 95, e2808. [Google Scholar] [CrossRef]
- Pepper, N.B.; Oertel, M.; Rehn, S.; Kobe, C.; Eich, H.T. Modern PET-Guided Radiotherapy Planning and Treatment for Malignant Lymphoma. Semin. Nucl. Med. 2023, 53, 389–399. [Google Scholar] [CrossRef]
- Campbell, B.A.; Bakst, R.L.; Milgrom, S.A.; Seymour, J.F. Balancing the Therapeutic Ratio in DLBCL Requires Appropriate, Individualized Patient Selection Rather Than Broad Elimination of Radiation Therapy. Int. J. Radiat. Oncol. Biol. Phys. 2022, 113, 479–488. [Google Scholar] [CrossRef]
- Oertel, M.; Berdel, C.; Held, G.; Herfarth, K.; Schmidberger, H.; Ernst, M.; Lenz, G.; Borchmann, P.; Eich, H.T. The new German evidence-based guideline on diffuse large B-cell lymphoma-key aspects for radiation oncologists. Strahlenther. Onkol. 2023, 199, 115–120. [Google Scholar] [CrossRef]
- Lee, J.W.; Oh, D.; Eom, K.-Y.; Kim, J.H.; Kim, W.C.; Chung, M.J.; Lee, J.H. The prognostic value of PET/CT evaluation with Deauville score on the recurrence and survival in diffuse large B-cell lymphoma: A multi-institutional study of KROG 17-02. Clin. Exp. Metastasis 2020, 37, 125–131. [Google Scholar] [CrossRef]
- Martelli, M.; Ceriani, L.; Zucca, E.; Zinzani, P.L.; Ferreri, A.J.; Vitolo, U.; Stelitano, C.; Brusamolino, E.; Cabras, M.G.; Rigacci, L.; et al. [18F]fluorodeoxyglucose positron emission tomography predicts survival after chemoimmunotherapy for primary mediastinal large B-cell lymphoma: Results of the International Extranodal Lymphoma Study Group IELSG-26 Study. J. Clin. Oncol. 2014, 32, 1769–1775. [Google Scholar] [CrossRef]
- Filippi, A.R.; Piva, C.; Giunta, F.; Bellò, M.; Chiappella, A.; Caracciolo, D.; Zotta, M.; Douroukas, A.; Ragona, R.; Vitolo, U.; et al. Radiation therapy in primary mediastinal B-cell lymphoma with positron emission tomography positivity after rituximab chemotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2013, 87, 311–316. [Google Scholar] [CrossRef]
- Ceriani, L.; Martelli, M.; Gospodarowicz, M.K.; Ricardi, U.; Ferreri, A.J.; Chiappella, A.; Stelitano, C.; Balzarotti, M.; Cabrera, M.E.; Cunningham, D.; et al. Positron Emission Tomography/Computed Tomography Assessment After Immunochemotherapy and Irradiation Using the Lugano Classification Criteria in the IELSG-26 Study of Primary Mediastinal B-Cell Lymphoma. Int. J. Radiat. Oncol. Biol. Phys. 2017, 97, 42–49. [Google Scholar] [CrossRef]
- Martelli, M. The IELSG-37 study: A randomized trial assessing the role of mediastinal radiotherapy after front-line rituximab and anthracycline containing regimens in patients with primary mediastinal B cell lymphoma (PMBCL). In Proceedings of the 13th International Conference on Malignant Lymphoma 2015, Lugano, Switzerland, 17–20 June 2015. [Google Scholar]
- De Sanctis, V.; Finolezzi, E.; Osti, M.F.; Grapulin, L.; Alfò, M.; Pescarmona, E.; Berardi, F.; Natalino, F.; Moleti, M.L.; Di Rocco, A.; et al. MACOP-B and involved-field radiotherapy is an effective and safe therapy for primary mediastinal large B cell lymphoma. Int. J. Radiat. Oncol. Biol. Phys. 2008, 72, 1154–1160. [Google Scholar] [CrossRef]
- Zinzani, P.L.; Stefoni, V.; Finolezzi, E.; Brusamolino, E.; Cabras, M.G.; Chiappella, A.; Salvi, F.; Rossi, A.; Broccoli, A.; Martelli, M. Rituximab combined with MACOP-B or VACOP-B and radiation therapy in primary mediastinal large B-cell lymphoma: A retrospective study. Clin. Lymphoma Myeloma Leuk. 2009, 9, 381–385. [Google Scholar] [CrossRef]
- Rieger, M.; Österborg, A.; Pettengell, R.; White, D.; Gill, D.; Walewski, J.; Kuhnt, E.; Loeffler, M.; Pfreundschuh, M.; Ho, A. Primary mediastinal B-cell lymphoma treated with CHOP-like chemotherapy with or without rituximab: Results of the Mabthera International Trial Group study. Ann. Oncol. 2011, 22, 664–670. [Google Scholar] [CrossRef]

| Characteristic N: 31 Patients | n (%) Median (IQR) |
|---|---|
| Age (year) | 34 (28–44) |
| Sex | |
| Male | 18 (58) |
| Female | 13 (41.9) |
| Stage | |
| I | 4 (12.9) |
| II | 25 (80.6) |
| IV | 2 (6.4) |
| Chemotherapy | |
| R-CHOP | 11 (35.4) |
| R-MACOP-B | 20 (64.5) |
| Duration CHT (week) | 12 (10.5–13.8) |
| T CHT-RT (week) | 9 (8.2–14.7) |
| Total dose (Gy) | 30 |
| Fractions (n) | 15 |
| Dose per fraction (Gy) | 2 |
| Planning technique | |
| 3D-CRT | 3 (9.6) |
| IMRT | 28 (90.3) |
| CTV, (cc) | 110.3 (77.5–208.1) |
| PTV, (cc) | 266.1 (219.1–421) |
| Toxicities 31 Patients | N (%) |
|---|---|
| Acute toxicities | 5 (16.1) |
| Nausea G1 | 2 |
| Asthenia G1 | 2 |
| Neutropenia G2 | 1 |
| Late toxicities | 5 (16.1) |
| Neutropenia G1 | 2 |
| Neutropenia G3 | 1 |
| Pulmonary infection G2 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Facondo, G.; Serio, M.; Vullo, G.; Bianchi, M.P.; Pelliccia, S.; Di Rocco, A.; Lanzolla, T.; Valeriani, M.; Di Napoli, A.; Tafuri, A.; et al. Efficacy of Residual Site Radiation Therapy (ISRT) in Patients with Primary Mediastinal Lymphoma with Deauville Score 4 Following R-CHT: Results of a Retrospective Mono Institutional Study. J. Clin. Med. 2023, 12, 3777. https://doi.org/10.3390/jcm12113777
Facondo G, Serio M, Vullo G, Bianchi MP, Pelliccia S, Di Rocco A, Lanzolla T, Valeriani M, Di Napoli A, Tafuri A, et al. Efficacy of Residual Site Radiation Therapy (ISRT) in Patients with Primary Mediastinal Lymphoma with Deauville Score 4 Following R-CHT: Results of a Retrospective Mono Institutional Study. Journal of Clinical Medicine. 2023; 12(11):3777. https://doi.org/10.3390/jcm12113777
Chicago/Turabian StyleFacondo, Giuseppe, Mattia Serio, Gianluca Vullo, Maria Paola Bianchi, Sabrina Pelliccia, Alice Di Rocco, Tiziana Lanzolla, Maurizio Valeriani, Arianna Di Napoli, Agostino Tafuri, and et al. 2023. "Efficacy of Residual Site Radiation Therapy (ISRT) in Patients with Primary Mediastinal Lymphoma with Deauville Score 4 Following R-CHT: Results of a Retrospective Mono Institutional Study" Journal of Clinical Medicine 12, no. 11: 3777. https://doi.org/10.3390/jcm12113777
APA StyleFacondo, G., Serio, M., Vullo, G., Bianchi, M. P., Pelliccia, S., Di Rocco, A., Lanzolla, T., Valeriani, M., Di Napoli, A., Tafuri, A., Martelli, M., Osti, M. F., & De Sanctis, V. (2023). Efficacy of Residual Site Radiation Therapy (ISRT) in Patients with Primary Mediastinal Lymphoma with Deauville Score 4 Following R-CHT: Results of a Retrospective Mono Institutional Study. Journal of Clinical Medicine, 12(11), 3777. https://doi.org/10.3390/jcm12113777








