Application of Logistic Regression and Artificial Intelligence in the Risk Prediction of Acute Aortic Dissection Rupture
Abstract
:1. Introduction
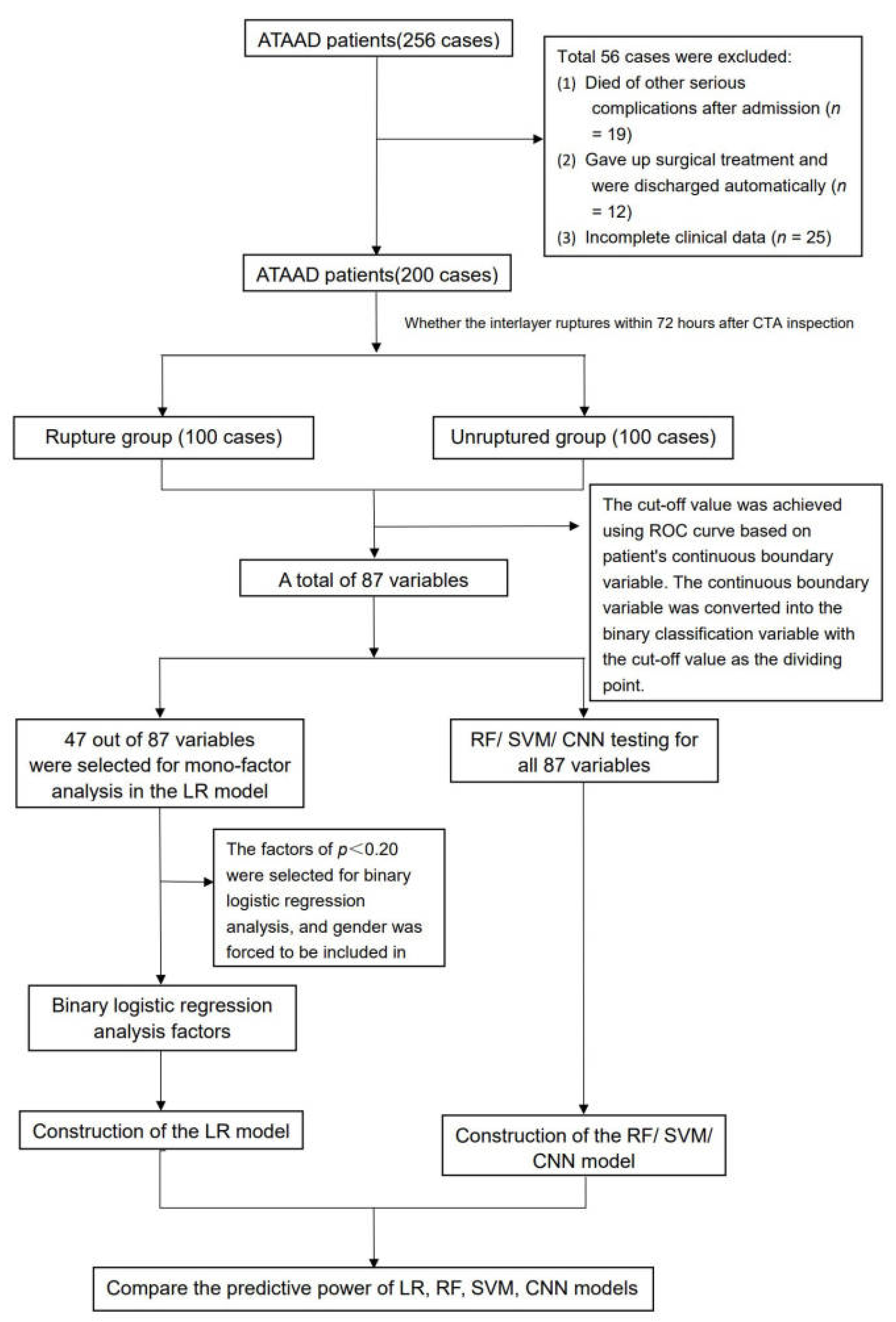
2. Materials and Methods
2.1. Study Design, Patients
2.2. Outcomes
2.3. Data Collection
2.4. Construction of the LR Model
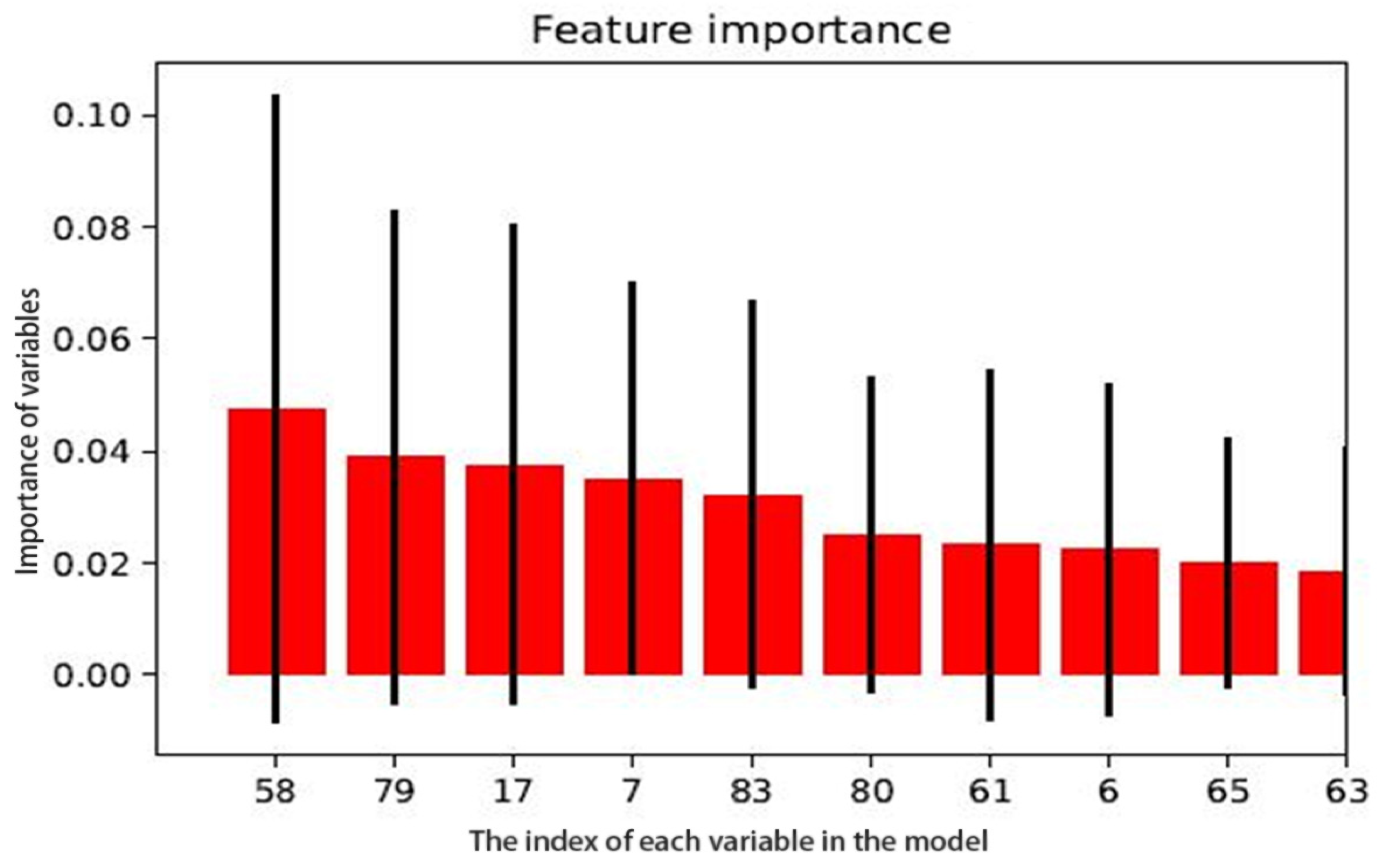
2.5. Construction of the RF Model
2.6. Construction of the SVM Model
2.7. Construction of the CNN Model
2.8. Statistical Analysis
3. Results
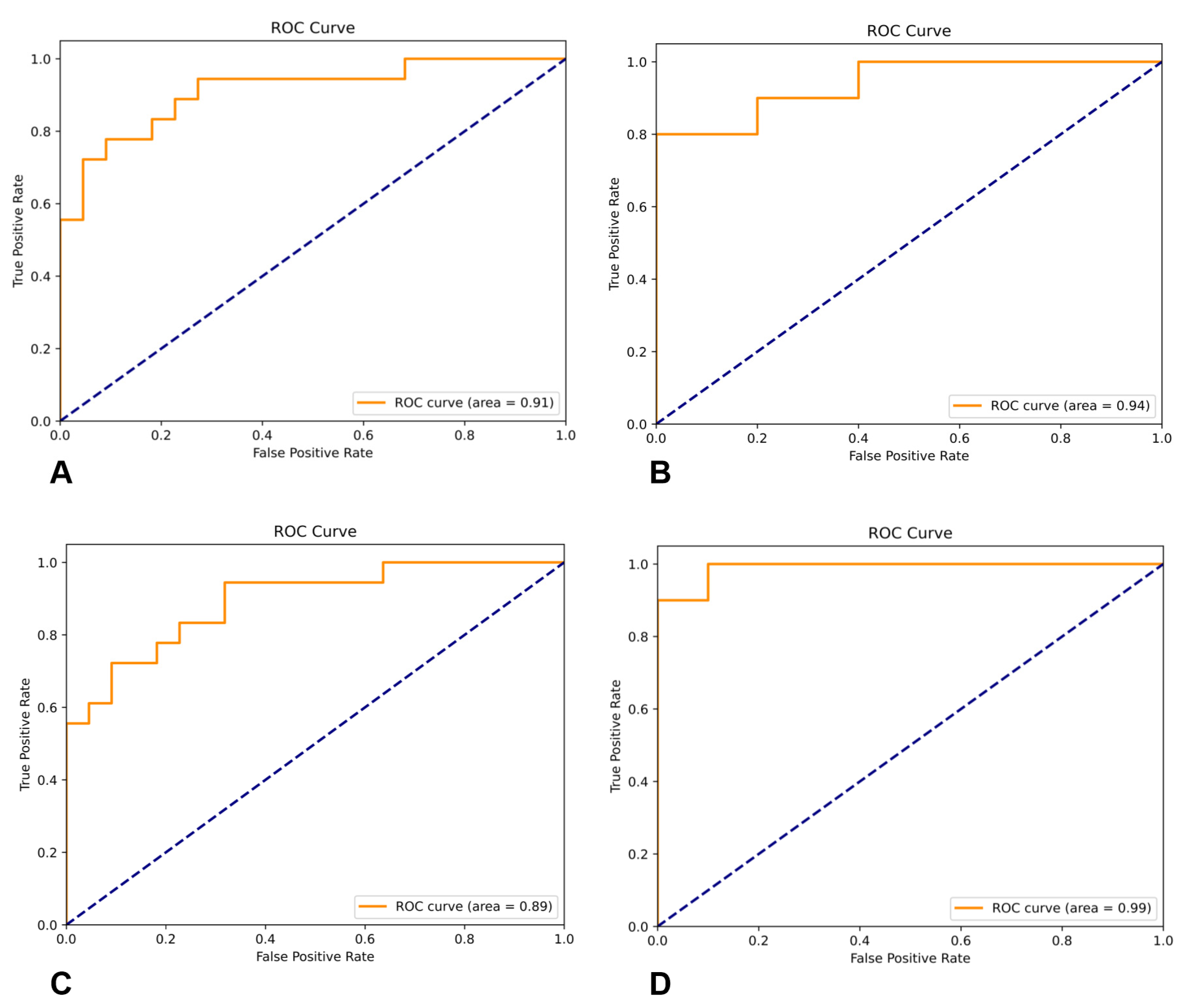
3.1. LR Model
3.2. RF Model
3.3. SVM Model
3.4. CNN Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Elsayed, R.S.; Cohen, R.G.; Fleischman, F.; Bowdish, M.E. Acute type a aortic dissection. Cardiol. Clin. 2017, 35, 331–345. [Google Scholar] [CrossRef]
- Erbel, R.; Aboyans, V.; Boileau, C.; Bossone, E.; Bartolomeo, R.D.; Eggebrecht, H.; Evangelista, A.; Falk, V.; Frank, H.; Gaemperli, O.; et al. 2014 esc guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The task force for the diagnosis and treatment of aortic diseases of the european society of cardiology (esc). Eur. Heart J. 2014, 35, 2873–2926. [Google Scholar]
- Harris, K.M.; Nienaber, C.A.; Peterson, M.D.; Woznicki, E.M.; Braverman, A.C.; Trimarchi, S.; Myrmel, T.; Pyeritz, R.; Hutchison, S.; Strauss, C. Early mortality in type a acute aortic dissection: Insights from the international registry of acute aortic dissection. JAMA Cardiol. 2022, 7, 1009–1015. [Google Scholar] [CrossRef]
- Kuang, J.; Yang, J.; Wang, Q.; Yu, C.; Li, Y.; Fan, R. A preoperative mortality risk assessment model for stanford type a acute aortic dissection. BMC Cardiovasc. Disord. 2020, 20, 508. [Google Scholar] [CrossRef]
- Wu, J.; Qiu, J.; Xie, E.; Jiang, W.; Zhao, R.; Qiu, J.; Zafar, M.A.; Huang, Y.; Yu, C. Predicting in-hospital rupture of type a aortic dissection using random forest. J. Thorac. Dis. 2019, 11, 4634. [Google Scholar] [CrossRef]
- Arvanitaki, A.; Ntiloudi, D.; Giannakoulas, G.; Dimopoulos, K. Prediction models and scores in adult congenital heart disease. Curr. Pharm. Des. 2021, 27, 1232–1244. [Google Scholar] [CrossRef]
- Yang, L.; Wu, H.; Jin, X.; Zheng, P.; Hu, S.; Xu, X.; Yu, W.; Yan, J. Study of cardiovascular disease prediction model based on random forest in eastern China. Sci. Rep. 2020, 10, 5245. [Google Scholar] [CrossRef] [Green Version]
- Feng, J.Z.; Wang, Y.; Peng, J.; Sun, M.W.; Zeng, J.; Jiang, H. Comparison between logistic regression and machine learning algorithms on survival prediction of traumatic brain injuries. J. Crit. Care 2019, 54, 110–116. [Google Scholar] [CrossRef]
- Albert, B.A. Deep learning from limited training data: Novel segmentation and ensemble algorithms applied to automatic melanoma diagnosis. IEEE Access 2020, 8, 31254–31269. [Google Scholar] [CrossRef]
- Asaoka, R.; Murata, H.; Hirasawa, K.; Fujino, Y.; Matsuura, M.; Miki, A.; Kanamoto, T.; Ikeda, Y.; Mori, K.; Iwase, A.; et al. Using deep learning and transfer learning to accurately diagnose early-onset glaucoma from macular optical coherence tomography images. Am. J. Ophthalmol. 2019, 198, 136–145. [Google Scholar] [CrossRef]
- Hiratzka, L.F.; Bakris, G.L.; Beckman, J.A.; Bersin, R.; Carr, V.; Casey, D.; Eagle, K.; Hermann, L.; Isselbacher, E.; Kazerooni, E. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine . Circulation 2010, 121, e266. [Google Scholar]
- Lin, K.; Xie, J.Q.; Hu, Y.H.; Kong, G.L. Application of support vector machine in predicting in-hospital mortality risk of patients with acute kidney injury in ICU. J. Peking Univ. Health Sci. 2018, 50, 239–244. (In Chinese) [Google Scholar]
- Wu, X.; Zuo, W.; Lin, L.; Jia, W.; Zhang, D. F-svm: Combination of feature transformation and svm learning via convex relaxation. IEEE Trans. Neural. Netw. Learn Syst. 2018, 29, 5185–5199. [Google Scholar] [CrossRef]
- LeCun, Y.; Bengio, Y.; Hinton, G. Deep learning. Nature 2015, 521, 436–444. [Google Scholar] [CrossRef]
- Liu, X.; Guo, S.; Yang, B.; Ma, S.; Zhang, H.; Li, J.; Sun, C.; Jin, L.; Li, X.; Yang, Q.; et al. Automatic organ segmentation for ct scans based on super-pixel and convolutional neural networks. J. Digit. Imaging 2018, 31, 748–760. [Google Scholar] [CrossRef]
- von Kodolitsch, Y.; Schwartz, A.G.; Nienaber, C.A. Clinical prediction of acute aortic dissection. Arch. Intern. Med. 2000, 160, 2977–2982. [Google Scholar] [CrossRef] [Green Version]
- Casanova, R.; Saldana, S.; Simpson, S.L.; Lacy, M.E.; Subauste, A.R.; Blackshear, C.; Wagenknecht, L.; Bertoni, A.G. Prediction of incident diabetes in the jackson heart study using high-dimensional machine learning. PLoS ONE 2016, 11, e0163942. [Google Scholar] [CrossRef] [Green Version]
- Howard, D.P.; Banerjee, A.; Fairhead, J.F.; Perkins, J.; Silver, L.E.; Rothwell, P.M. Population-based study of incidence and outcome of acute aortic dissection and premorbid risk factor control: 10-year results from the oxford vascular study. Circulation 2013, 127, 2031–2037. [Google Scholar] [CrossRef] [Green Version]
- Peng, W.; Peng, Z.; Chai, X.; Zhu, Q.; Yang, G.; Zhao, Q.; Zhou, S. Potential biomarkers for early diagnosis of acute aortic dissection. Heart Lung 2015, 44, 205–208. [Google Scholar] [CrossRef]
- Du, R.; Li, D.; Yu, J.; Ma, Y.; Zhang, Q.; Zeng, Z.; Zeng, R. Association of platelet to lymphocyte ratio and risk of in-hospital mortality in patients with type b acute aortic dissection. Am. J. Emerg. Med. 2017, 35, 368–370. [Google Scholar] [CrossRef]
- Hsieh, W.C.; Henry, B.M.; Hsieh, C.C.; Maruna, P.; Omara, M.; Lindner, J. Prognostic role of admission c-reactive protein level as a predictor of in-hospital mortality in type-a acute aortic dissection: A meta-analysis. Vasc. Endovasc. Surg. 2019, 53, 547–557. [Google Scholar] [CrossRef] [PubMed]
- Sampaio, P.S.; Castanho, A.; Almeida, A.S.; Oliveira, J.; Brites, C. Identification of rice flour types with near-infrared spectroscopy associated with pls-da and svm methods. Eur. Food Res. Technol. 2020, 246, 527–537. [Google Scholar] [CrossRef]
- Gharbi, M.; Chen, J.; Barron, J.T.; Hasinoff, S.W.; Durand, F. Deep bilateral learning for real-time image enhancement. ACM Trans. Graph. 2017, 36, 1–12. [Google Scholar] [CrossRef]
- Liang, M.; Zhou, T.; Zhang, F.; Yang, J.; Xia, Y. Research on convolutional neural network and its application on medical image. J. Biomed. Eng. 2018, 35, 977–985. (In Chinese) [Google Scholar]
| Risk Factors | |||
|---|---|---|---|
| Age | Ischemic manifestation of superior mesenteric artery | Presence of severe aortic regurgitation | Creatine kinase isoenzyme value |
| Women | Aortic sinus diameter | Presence of a large amount of pericardial effusion presence | Age > 63 years b |
| EF | Sinus canal junction diameter | High blood pressure presence | Aortic sinus diameter > 41 mm |
| PH | Widest diameter d | Diabetes | Sinus canal junction diameter > 38 mm |
| Lac | Arc length of false cavity d | Smoking history | Arc length of false cavity > 119 mm d |
| PaO2 | Radian of false cavity d | Marfan syndrome | Radian of false cavity > 4.42 rad d |
| PaCO2 | False cavity area d | Heart rate | Length of aortic dissection > 534 mm |
| FiO2 | Ratio of false lumen area to true lumen area d | Respiratory rate | False cavity area > 11.85 cm2 d |
| WBC | Maximum breaking diameter | Shock | Ratio of false lumen area to true lumen area > 2.12 d |
| NEUT | Length of aortic dissection | Ventilator assisted ventilation | Initial break diameter > 15.5 mm |
| PLT | Full-length aorta | Chest pain | Number of branch vessels involved > 3 |
| cTnT | Ratio of aortic dissection length to aortic length | Syncope | Maximum diameter > 48 mmd |
| NT-proBNP | No thrombus in the false cavity | Mental symptoms presence | Time of onset to the hospital > 20 h |
| Cr | No distortion of the inner membrane a | Limb ischemia | Lac > 1.9 mmol/L |
| FIB | Number of breaks | Ischemic manifestation in abdominal vasculature | WBC > 14.2 × 109/L |
| D-Dimer | Number of branch vessels involved | Limb blood pressure e | AST > 80 U/L c |
| AST | Difference in blood pressure of extremities > 20 mmHg | Aortic branch vessels involved f | Type A interlayer classification |
| True cavity area d | Creatine kinase value | ||
| Risk Factor | Regression Coefficient (β) | Waldx2 | p | OR Value | 95% CI |
| Age > 63 years | 1.687 | 8.487 | 0.004 | 5.403 | 1.737–16.810 |
| Women | 1.769 | 10.131 | 0.001 | 5.865 | 1.973–17.432 |
| Ventilator-assisted ventilation | 3.052 | 14.203 | 0.010 | 21.156 | 4.326–4.326 |
| AST value > 80 U/L | 1.594 | 5.156 | 0.023 | 4.926 | 1.244–19.506 |
| No distortion of the inner membrane | 1.571 | 9.685 | 0.002 | 4.811 | 1.789–12.940 |
| Aortic sinus diameter > 41 mm | 0.927 | 3.790 | 0.052 | 2.527 | 0.994–6.426 |
| Widest diameter > 48 mm | 1.320 | 8.751 | 0.003 | 3.745 | 1.561–8.982 |
| Ratio of false lumen area to true lumen area > 2.12 | 1.935 | 13.336 | 0.010 | 6.927 | 2.451–19.574 |
| Lac value > 1.9 mmol/L | 2.281 | 20.955 | 0.010 | 9.782 | 3.684–25.973 |
| WBC value > 14.2 × 109/L | 1.225 | 7.672 | 0.006 | 3.404 | 1.431–8.101 |
| Model Name | AUC | Accuracy | Precision | F1-Score | Specificity | Recall |
|---|---|---|---|---|---|---|
| LR | 0.91 (0.90–0.94) | 0.85 (0.84–0.85) | 0.90 (0.86–0.93) | 0.88 (0.87–0.91) | 0.86 (0.85–0.88) | 0.90 (0.89–0.91) |
| RF | 0.94 (0.90–0.97) | 0.90 (0.85–0.93) | 0.92 (0.90–0.97) | 0.89 (0.86–0.90) | 0.91 (0.90–0.93) | 0.95 (0.90–0.98) |
| SVM | 0.89 (0.86–0.94) | 0.83 (0.82–0.85) | 0.78 (0.76–0.79) | 0.77 (0.73–0.78) | 0.85 (0.81–0.85) | 0.88 (0.83–0.91) |
| CNN | 0.99 (0.95–0.99) | 0.90 (0.88–0.91) | 0.90 (0.89–0.92) | 0.90 (0.89–0.93) | 0.90 (0.87–0.93) | 0.90 (0.88–0.92) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, Y.; Hu, J.; Xu, R.; Wu, S.; Ma, F.; Liu, H.; Xie, Y.; Li, X. Application of Logistic Regression and Artificial Intelligence in the Risk Prediction of Acute Aortic Dissection Rupture. J. Clin. Med. 2023, 12, 179. https://doi.org/10.3390/jcm12010179
Lin Y, Hu J, Xu R, Wu S, Ma F, Liu H, Xie Y, Li X. Application of Logistic Regression and Artificial Intelligence in the Risk Prediction of Acute Aortic Dissection Rupture. Journal of Clinical Medicine. 2023; 12(1):179. https://doi.org/10.3390/jcm12010179
Chicago/Turabian StyleLin, Yanya, Jianxiong Hu, Rongbin Xu, Shaocong Wu, Fei Ma, Hui Liu, Ying Xie, and Xin Li. 2023. "Application of Logistic Regression and Artificial Intelligence in the Risk Prediction of Acute Aortic Dissection Rupture" Journal of Clinical Medicine 12, no. 1: 179. https://doi.org/10.3390/jcm12010179
APA StyleLin, Y., Hu, J., Xu, R., Wu, S., Ma, F., Liu, H., Xie, Y., & Li, X. (2023). Application of Logistic Regression and Artificial Intelligence in the Risk Prediction of Acute Aortic Dissection Rupture. Journal of Clinical Medicine, 12(1), 179. https://doi.org/10.3390/jcm12010179





