Determinants in the Underdiagnosis of COPD in Spain—CONOCEPOC Study
Abstract
:1. Introduction
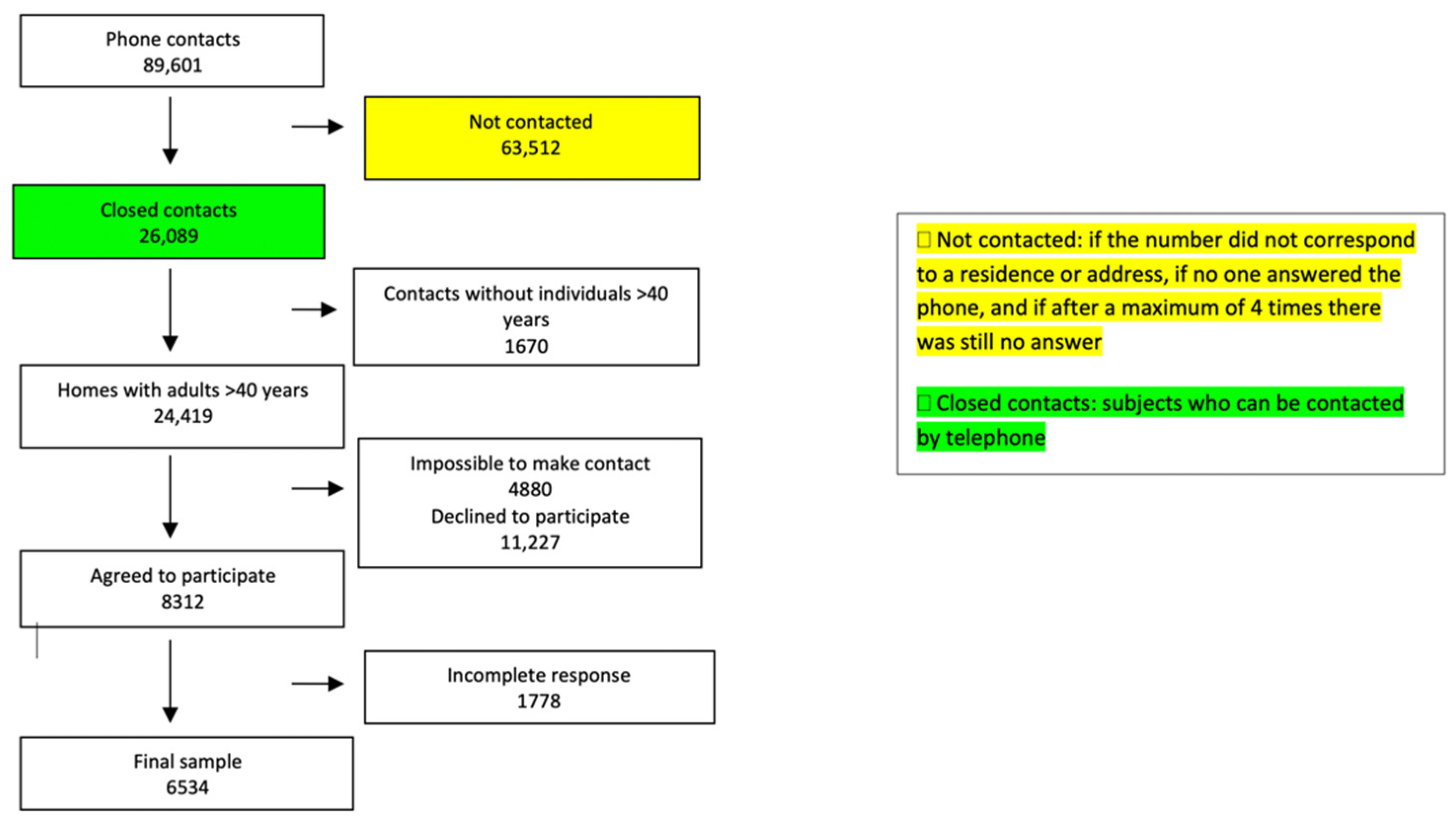
2. Materials and Methods
2.1. Data Collection
2.2. Statistical Analysis
3. Results
3.1. Chronic Respiratory Symptoms and Respiratory Disease Reported
3.2. Seeking Medical Attention for Respiratory Symptoms. Associated Factors and Situation According to the Autonomous Community
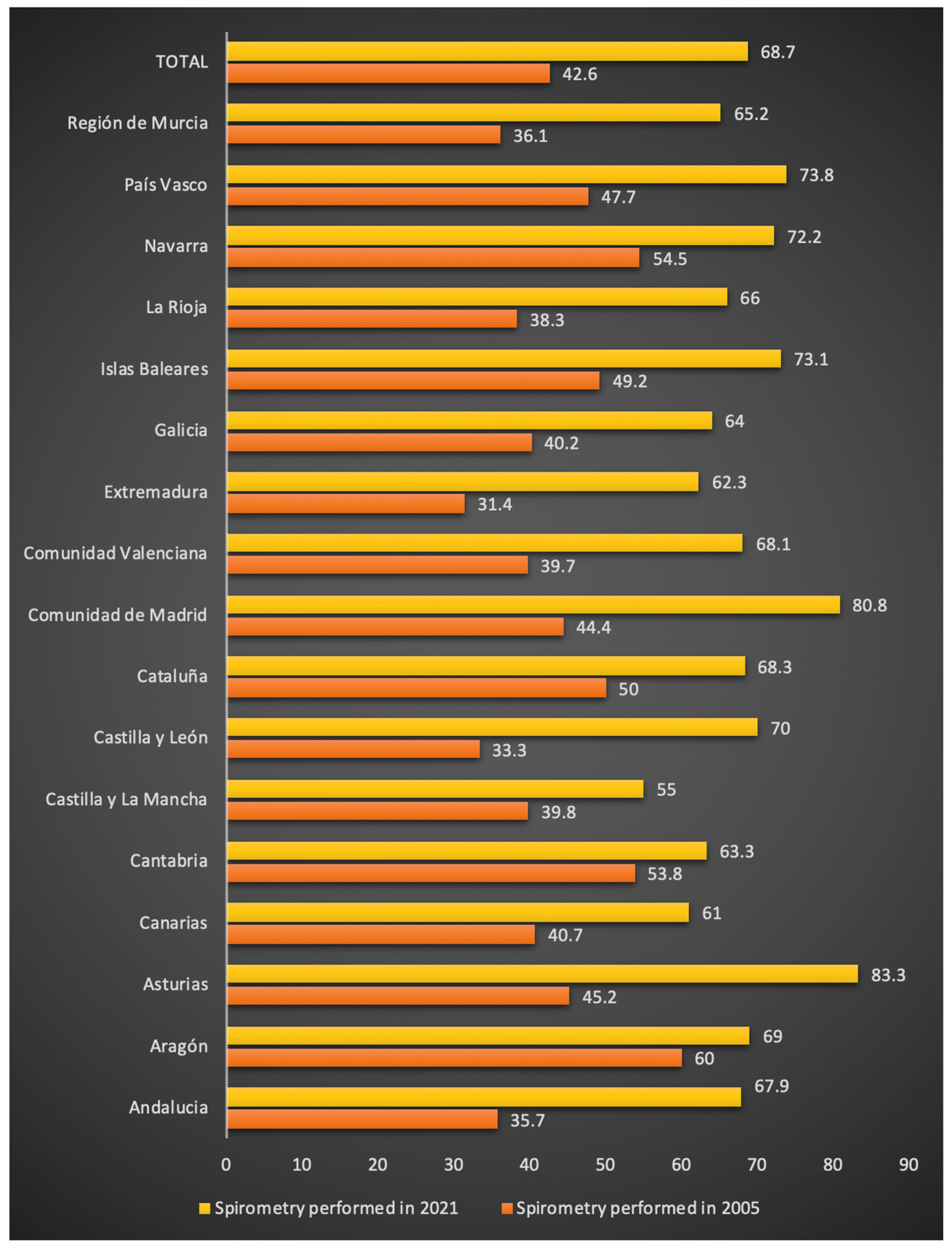
3.3. Use of Spirometry. Associated Factors, Evolution over Time, and Situation According to the Autonomous Community
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Soriano, J.B.; Abajobir, A.A.; Abate, K.H.; Abera, S.F.; Agrawal, A.; Ahmed, M.B.; Aichour, A.N.; Aichour, I.; Aichour, M.T.E.; Alam, K.; et al. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir. Med. 2017, 5, 691–706. [Google Scholar] [CrossRef] [Green Version]
- Global Burden of Disease [Database]; Institute of Health Metrics: Washington, DC, USA, 2019; Available online: https://extranet.who.int/ncdsmicrodata/index.php/catalog/270IHME (accessed on 9 March 2022).
- Ministerio de Sanidad y Política Social. Estrategia en EPOC del Sistema Nacional de Salud. 2009. Available online: https://www.mscbs.gob.es/organizacion/sns/planCalidadSNS/docs/EstrategiaEPOCSNS.pdf (accessed on 30 December 2021).
- Miravitlles, M.; Calle, M.; Molina, J.; Almagro, P.; Gómez, J.-T.; Trigueros, J.A.; Cosío, B.G.; Casanova, C.; López-Campos, J.L.; Riesco, J.A.; et al. Spanish COPD Guidelines (GesEPOC) 2021: Updated Pharmacological treatment of stable COPD. Arch. Bronconeumol. 2022, 58, 69–81. [Google Scholar] [CrossRef] [PubMed]
- Miravitlles, M.; Soriano, J.B.; Garcia-Rio, F.; Munoz, L.; Duran-Tauleria, E.; Sanchez, G.; Sobradillo, V.; Ancochea, J. Prevalence of COPD in Spain: Impact of undiagnosed COPD on quality of life and daily life activities. Thorax 2009, 64, 863–868. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soriano, J.B.; Alfageme, I.; Miravitlles, M.; de Lucas, P.; Soler-Cataluña, J.J.; García-Río, F.; Casanova, C.; Rodríguez González-Moro, J.M.; Cosío, B.G.; Sánchez, G.; et al. Prevalence and determinants of COPD in Spain: EPISCAN II. Arch. Bronconeumol. 2021, 57, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Miravitlles, M.; De La Roza, C.; Naberan, K.; Lamban, M.; Gobartt, E.; Martín, A.; Chapman, K. Attitudes Toward the Diagnosis of Chronic Obstructive Pulmonary Disease in Primary Care. Arch. Bronconeumol. 2006, 42, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Soriano, J.B.; Calle, M.; Montemayor, T.; Álvarez-Sala, J.L.; Ruiz-Manzano, J.; Miravitlles, M. Conocimientos de la población general sobre la enfermedad pulmonar obstructiva crónica y sus determinantes: Situación actual y cambios recientes. Arch. Bronconeumol. 2012, 48, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Potthoff, R.F. Telephone Sampling in Epidemiologic Research: To Reap the Benefits, Avoid the Pitfalls. Am. J. Epidemiol. 1994, 139, 967–978. [Google Scholar] [CrossRef]
- Minette, A. Questionnaire of the European Community for Coal and Steel (ECSC) on respiratory symptoms. 1987–updating of the 1962 and 1967 questionnaires for studying chronic bronchitis and emphysema. Eur. Respir. J. 1989, 2, 165–177. [Google Scholar]
- Maio, S.; Baldacci, S.; Carrozzi, L.; Pistelli, F.; Angino, A.; Simoni, M.; Sarno, G.; Cerrai, S.; Martini, F.; Fresta, M.; et al. Respiratory symptoms/diseases prevalence is still increasing: A 25-yr population study. Respir. Med. 2016, 110, 58–65. [Google Scholar] [CrossRef] [Green Version]
- Brøgger, J.C.; Bakke, P.; Eide, G.E.; Johansen, B.; Andersen, A.R.; Gulsvik, A. Trends in symptoms of obstructive lung disease in Norway. Int. J. Tuberc. Lung Dis. 2004, 8, 1416–1422. [Google Scholar] [PubMed]
- Backman, H.; Hedman, L.; Jansson, S.-A.; Lindberg, A.; Lundbäck, B.; Rönmark, E. Prevalence trends in respiratory symptoms and asthma in relation to smoking-two cross-sectional studies ten years apart among adults in northern Sweden. World Allergy Organ. J. 2014, 7, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Encuesta Europea de Salud en España (EESE) 2020, Realizada Por el Instituto Nacional de Estadística (INE). 2020. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/EncuestaEuropea/EncuestaEuropea2020/EESE2020_inf_evol_princip_result.pdf (accessed on 9 March 2022).
- Rocha, V.; Soares, S.; Stringhini, S.; Fraga, S. Socioeconomic circumstances and respiratory function from childhood to early adulthood: A systematic review and meta-analysis. BMJ Open 2019, 9, e027528. [Google Scholar] [CrossRef] [PubMed]
- Hosseinpoor, A.R.; Parker, L.A.; D’Espaignet, E.T.; Chatterji, S. Socioeconomic Inequality in Smoking in Low-Income and Middle-Income Countries: Results from the World Health Survey. PLoS ONE 2012, 7, e42843. [Google Scholar] [CrossRef] [PubMed]
- Informe Anual del Sistema Nacional de Salud. 2019. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/sisInfSanSNS/tablasEstadisticas/InfAnualSNS2019/Informe_SNS_2019.pdf (accessed on 9 March 2022).
- Rubio, M.C.; Hermosa, J.L.R.; Miravitlles, M.; López-Campos, J.L. Knowledge of Chronic Obstructive Pulmonary Disease, Presence of Chronic Respiratory Symptoms and Use of Spirometry Among the Spanish Population: CONOCEPOC 2019 study. Arch. Bronconeumol. 2020. [Google Scholar] [CrossRef]
- Penña, V.S.; Miravitlles, M.; Gabriel, R.; Jiménez-Ruiz, C.A.; Villasante, C.; Masa, J.F.; Viejo, J.L.; Fernández-Fau, L. Geographic variations in prevalence and underdiagnosis of COPD: Results of the IBERPOC multicentre epidemiological study. Chest 2000, 118, 981–989. [Google Scholar] [CrossRef] [PubMed]
- Lamprecht, B.; Soriano, J.B.; Studnicka, M.; Kaiser, B.; Vanfleteren, L.E.; Gnatiuc, L.; Burney, P.; Miravitlles, M.; Garcia-Rio, F.; Akbari, K.; et al. Determinants of Underdiagnosis of COPD in National and International Surveys. Chest 2015, 148, 971–985. [Google Scholar] [CrossRef] [PubMed]
- Dharmage, S.; Perret, J.L.; Custovic, A. Epidemiology of Asthma in Children and Adults. Front. Pediatr. 2019, 7, 246. [Google Scholar] [CrossRef]
- Izquierdo, J.L.; Morena, D.; Gonzalez-Moro, J.M.R.; Paredero, J.M.; Pérez, B.; Graziani, D.; Gutiérrez, M.; Rodríguez, J.M. Clinical Management of COPD in a Real-World Setting. A Big Data Analysis. Arch. Bronconeumol. 2021, 57, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Nakken, N.; Janssen, D.J.A.; Bogaart, E.V.D.; Muris, J.W.M.; Vercoulen, J.H.; Custers, F.L.; Bootsma, G.P.; Gronenschild, M.H.M.; Wouters, E.F.M.; Spruit, M.A. Knowledge gaps in patients with COPD and their proxies. BMC Pulm. Med. 2017, 17, 136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- López-Campos, J.L.; Soriano, J.B.; Calle, M. A comprehensive, national survey of spirometry in Spain: Current bottlenecks and future directions in primary and sec-ondary care. Chest 2013, 144, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de Estadística. Datos Sobre Equipamiento y Uso de Tecnologías de Información y Comunicación en los Hogares de España. Available online: https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176741&menu=ultiDatos&idp=1254735976608 (accessed on 30 December 2021).

| Total | With Respiratory Symptoms | Without Respiratory Symptoms | p-Value | |
|---|---|---|---|---|
| N | 6529 | 1618 (24.8) | 4911 (75.2) | |
| Age (years), (average ± SD) | 61.5 (13.1) | 63.8 (13.4) | 60.8 (12.9) | <0.001 |
| Sex (male), n (%) | 3238 (49.5) | 796 (49.2) | 2440 (49.7) | 0.734 |
| Setting < 10,000 inhabitants | 2758 (42.2) | 695 (45.6) | 2063 (44.1) | 0.302 |
| Smoking history | ||||
| Accumulated consumption (pack-years), (average ± SD) | 19.3 (18.7) | 23.4 (19.4) | 16.5 (17.7) | <0.001 |
| Attempted to quit smoking, (average ± SD) | 609 (63.6) | 268 (70) | 34.1 (59.3) | 0.001 |
| Attempts to quit, median (P25–P75) | 2 (1–3) | 2 (1–4) | 2 (1–3) | 0.94 |
| Never smoked, n (%) | 3554 (54.4) | 736 (45.5) | 2817 (57.4) | <0.001 |
| Former smoker, n (%) | 2018 (30.9) | 499 (30.8) | 1519 (30.9) | 0.83 |
| Current smoker, n (%) | 958 (14.7) | 383 (23.7) | 575 (11.7) | <0.001 |
| Have tried alternatives to tobacco, (%) | 4.5 | 9.6 | 3.4 | <0.001 |
| Respiratory symptoms, (%) | ||||
| Chronic cough | 17.5 | 450 (27.9) | - | |
| Chronic expectoration | 9.5 | 325 (20.1) | - | |
| Chest wheezing or noises | 12.9 | 269 (16.6) | - | |
| Shortness of breath or trouble breathing | 55.6 | 1283 (79.3) | - | |
| COPD risk, n (%) | 627 (38.8) | |||
| Suffer from a respiratory disease, n (%) | 1174 (17.9) | 410 (25.3) | 764 (15.5) | <0.001 |
| Asthma | 95 (1.5) | 57 (3.5) | 38 (0.7) | <0.001 |
| Bronchitis or emphysema or COPD | 199 (3.1) | 125 (7.7) | 74 (1.5) | <0.001 |
| Perceived level of health *, (average ± SD) | 7.4 (1.7) | 6.7 (1.9) | 7.6 (1.6) | <0.001 |
| Self-reported health status, n (%) | <0.001 | |||
| Poor (<5) | 334 (5.1) | 162 (10) | 172 (3.5) | |
| Average (5–7) | 2536 (38.9) | 847 (52.3) | 1690 (34.4) | |
| Good (>7) | 3659 (56) | 609 (37.5) | 3049 (62.1) | |
| Patient with Chronic Respiratory Symptoms | Sought Medical Attention | Didn’t Seek Medical Attention | p-Value | |
|---|---|---|---|---|
| N | 1618 | 836 (51.7) | 782 (48.3) | |
| Sex (male), n (%) | 796 (49.2) | 416 (49.8) | 380 (48.6) | 0.639 |
| Age (years), (average ± SD) | 63.8 (13.4) | 65.2 (13.3) | 62.2 (13.3) | <0.001 |
| Setting < 10,000 inhabitants | 695 (42.9) | 334 (39.9) | 361 (46.2) | 0.027 |
| Smoking history | <0.001 | |||
| Current smoker, n (%) | 736 (45.5) | 162 (19.4) | 221 (28.3) | |
| Former smoker, n (%) | 499 (30.8) | 269 (32.2) | 230 (29.4) | |
| Never smoked, n (%) | 383 (23.7) | 405 (48.4) | 331 (42.3) | |
| Chronic cough, (%) | 27.9 | 27.1 | 29.7 | 0.501 |
| Chronic expectoration, (%) | 20.1 | 21.3 | 20.1 | 0.207 |
| Chest wheezing or noises, (%) | 16.6 | 16.4 | 16.4 | 0.976 |
| Shortness of breath or trouble breathing, (%) | 79.3 | 82.2 | 76.9 | 0.130 |
| COPD risk, n (%) | 627 (38.8) | 333 (39.8) | 294 (37.6) | 0.356 |
| Presence of respiratory disease reported, n (%) | 410 (25.3) | 227 (27.2) | 183 (23.4) | 0.009 |
| Have gone to the emergency room for worsening of respiratory symptoms, n (%) | 209 (12.9) | 174 (20.8) | 35 (4.5) | <0.001 |
| Perceived level of health, (average ± SD) | 6.7 (1.9) | 6.3 (2.0) | 7.0 (1.7) | <0.001 |
| Doctor seen, n (%) | ||||
| Family medicine specialist | 468 (56) | |||
| Pulmonologist | 368 (44) | |||
| OR (95% CI) | p-Value | |
|---|---|---|
| Area of residence | ||
| Area ≥ 10,000 inhabitants (ref.) | ||
| Area < 10,000 inhabitants | 0.797 (0.651–0.975) | 0.027 |
| Smoking status | ||
| Never (ref.) | ||
| Former smoker | 0.956 (0.761–1.201) | 0.698 |
| Active smoker | 0.599 (0.467–0.769) | <0.001 |
| Presence of respiratory disease | ||
| No (ref.) | ||
| Yes | 1.409 (1.090–1.822) | 0.009 |
| Have gone to emergency room for respiratory problem | ||
| No (ref.) | ||
| Yes | 5.610 (3.845–8.186) | <0.001 |
| OR (95% CI) | p-Value | Adjusted Autonomous Community OR (95% CI) | p-Value | |
|---|---|---|---|---|
| Sex, female (ref.) | ||||
| Male | 1.508 (2.024–1.123) | 0.006 | 1.535 (2.074–1.136) | 0.005 |
| Area ≥ 10,000 inhab. (ref.) | ||||
| Area < 10,000 inhab. | 0.655 (0.890–0.483) | 0.007 | 0.691 (0.957–0.498) | 0.026 |
| Age 40–50 years old (ref.) | ||||
| 51–60 years old | 1.868 (3.112–1.121) | 0.017 | 1.865 (3.136–1.109) | 0.019 |
| 61–70 years old | 1.068 (1.661–0.687) | 0.769 | 1.135 (1.780–0.723) | 0.582 |
| >71 years old | 0.910 (1.381–0.600) | 0.659 | 0.902 (1.380–0.589) | 0.633 |
| Smoking status | ||||
| Never (ref.) | ||||
| Former smoker | 1.684 (2.370–1.197) | 0.003 | 1.696 (2.407–1.195) | 0.003 |
| Current smoker | 1.394 (2.070–0.939) | 0.099 | 1.393 (2.084–0.931) | 0.107 |
| COPD, No (ref.) | ||||
| Yes COPD | 3.134 (13.746–0.715) | 0.13 | 2.524 (11.564–0.551) | 0.233 |
| COPD risk | 1.472 (1.998–1.085) | 0.013 | 1.488 (2.035–1.088) | 0.013 |
| Doctor seen, | ||||
| Family (ref.) | ||||
| Pulmonologist | 5.438 (7.728–3.826) | <0.001 | 6.151 (8.869–4.265) | <0.001 |
| Emergency room for respiratory problem | ||||
| Yes (ref.) | ||||
| No | 0.334 (0.518–0.215) | <0.001 | 0.335 (0.523–0.214) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calle Rubio, M.; Rodríguez Hermosa, J.L.; Miravitlles, M.; López-Campos, J.L. Determinants in the Underdiagnosis of COPD in Spain—CONOCEPOC Study. J. Clin. Med. 2022, 11, 2670. https://doi.org/10.3390/jcm11092670
Calle Rubio M, Rodríguez Hermosa JL, Miravitlles M, López-Campos JL. Determinants in the Underdiagnosis of COPD in Spain—CONOCEPOC Study. Journal of Clinical Medicine. 2022; 11(9):2670. https://doi.org/10.3390/jcm11092670
Chicago/Turabian StyleCalle Rubio, Myriam, Juan Luis Rodríguez Hermosa, Marc Miravitlles, and José Luis López-Campos. 2022. "Determinants in the Underdiagnosis of COPD in Spain—CONOCEPOC Study" Journal of Clinical Medicine 11, no. 9: 2670. https://doi.org/10.3390/jcm11092670
APA StyleCalle Rubio, M., Rodríguez Hermosa, J. L., Miravitlles, M., & López-Campos, J. L. (2022). Determinants in the Underdiagnosis of COPD in Spain—CONOCEPOC Study. Journal of Clinical Medicine, 11(9), 2670. https://doi.org/10.3390/jcm11092670






