Intravenous versus Epidural Routes of Patient-Controlled Analgesia in Abdominal Surgery: Systematic Review with Meta-Analysis
Abstract
1. Introduction
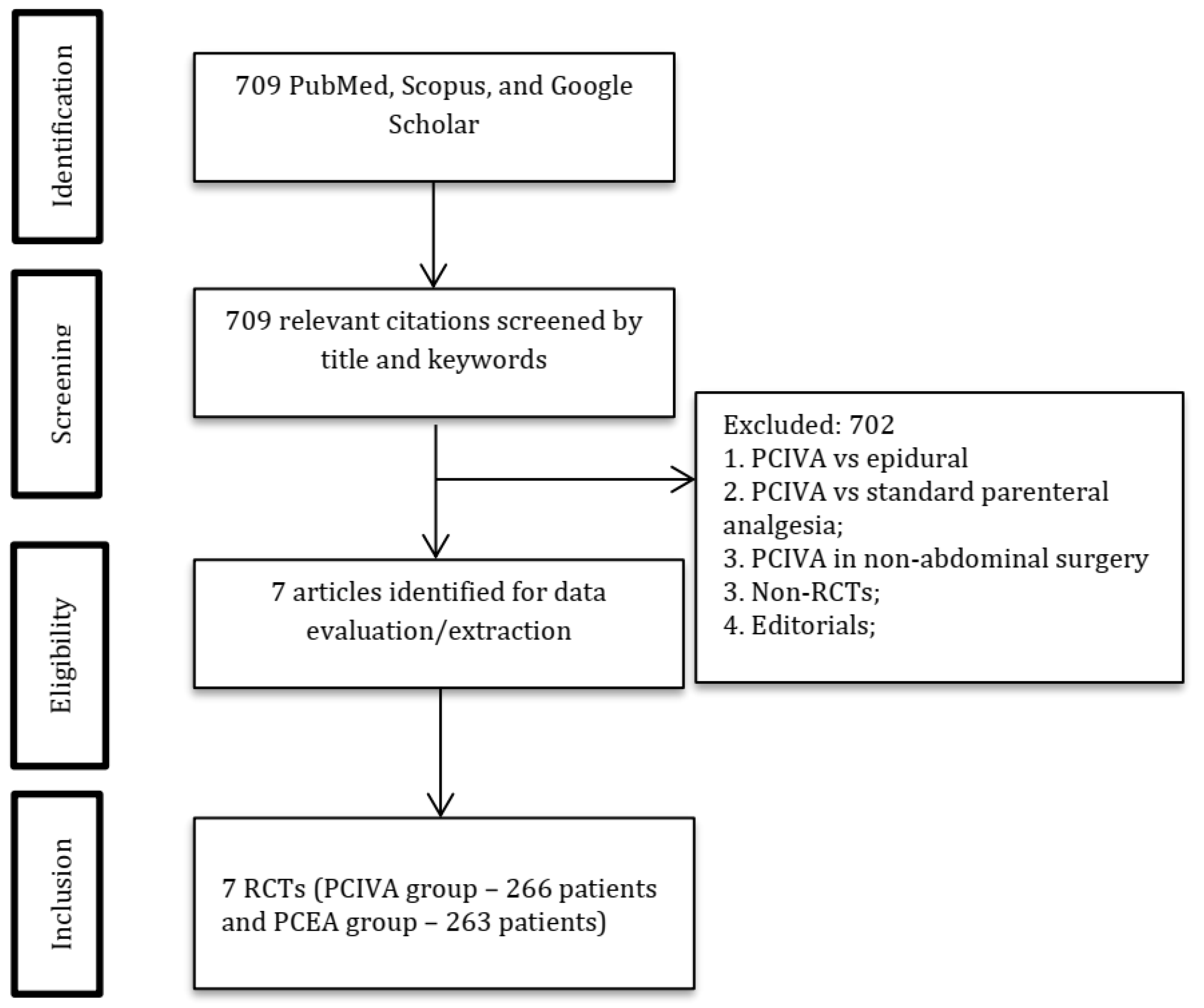
2. Materials and Methods
2.1. Criteria for Including Studies
2.2. Exclusion Criteria
2.3. Primary Outcomes
2.4. Secondary Outcomes
- Side effects
- Respiratory depression (respiratory rate <10 per minute, hypoxemia (SpO2 < 90% by pulse oximetry), administration of opioid antagonists).
- Nausea and vomiting
- Pruritus
- Sedation
- Respiratory complications such as respiratory depression (respiratory rate less than 10 breaths per minute or requirement for an opioid antagonist), hypoxemia (defined as SpO2 < 90% by pulse oximetry).
- Hypotension leading to worsening conditions or requiring fluid or vasopressor administration.
- Length of hospital stay (LoS) and length of stay in post-anesthesia care unit or intensive care unit (if reported).
2.5. Assessment of Methodological Quality and Critical Appraisal of Individual Studies
2.6. Data Extraction and Statistical Methods
3. Results
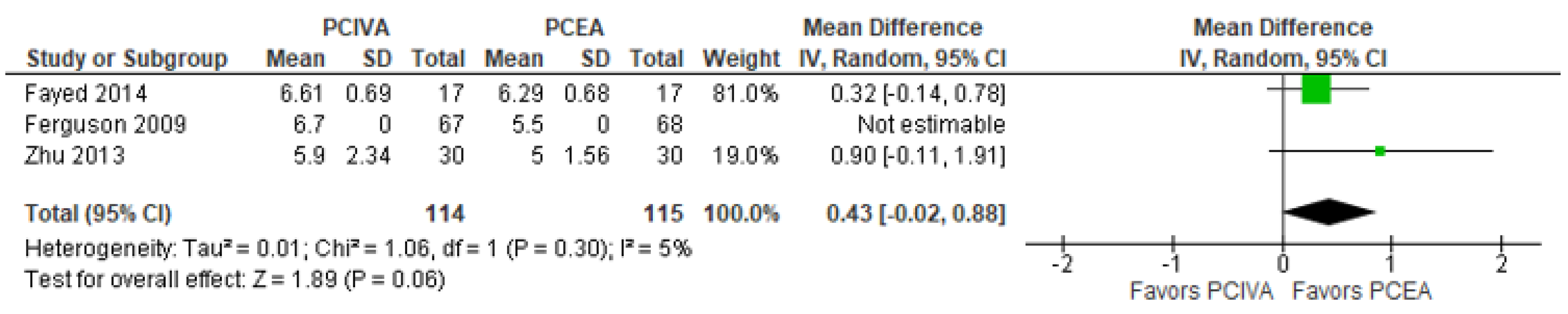
3.1. Postoperative Pain Scores at Rest (at 24 h)
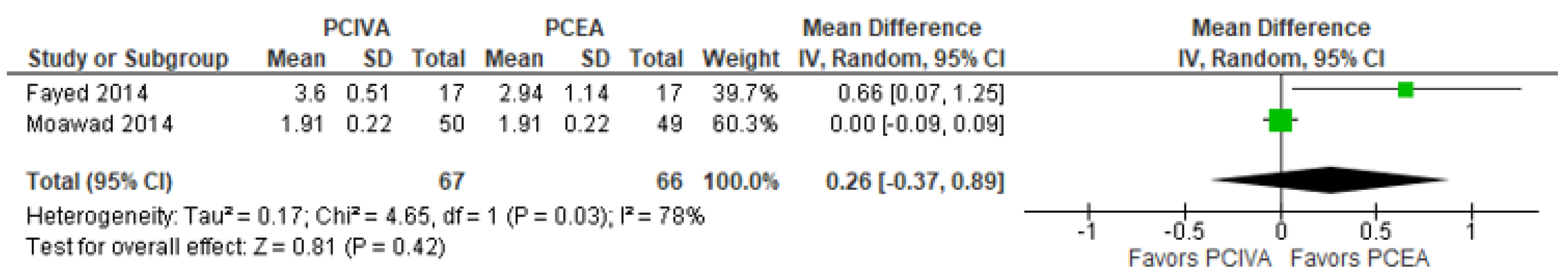
3.2. Postoperative Pain Scores on Coughing (at 24 h)
3.3. Postoperative Sedation Score (at 24 h)
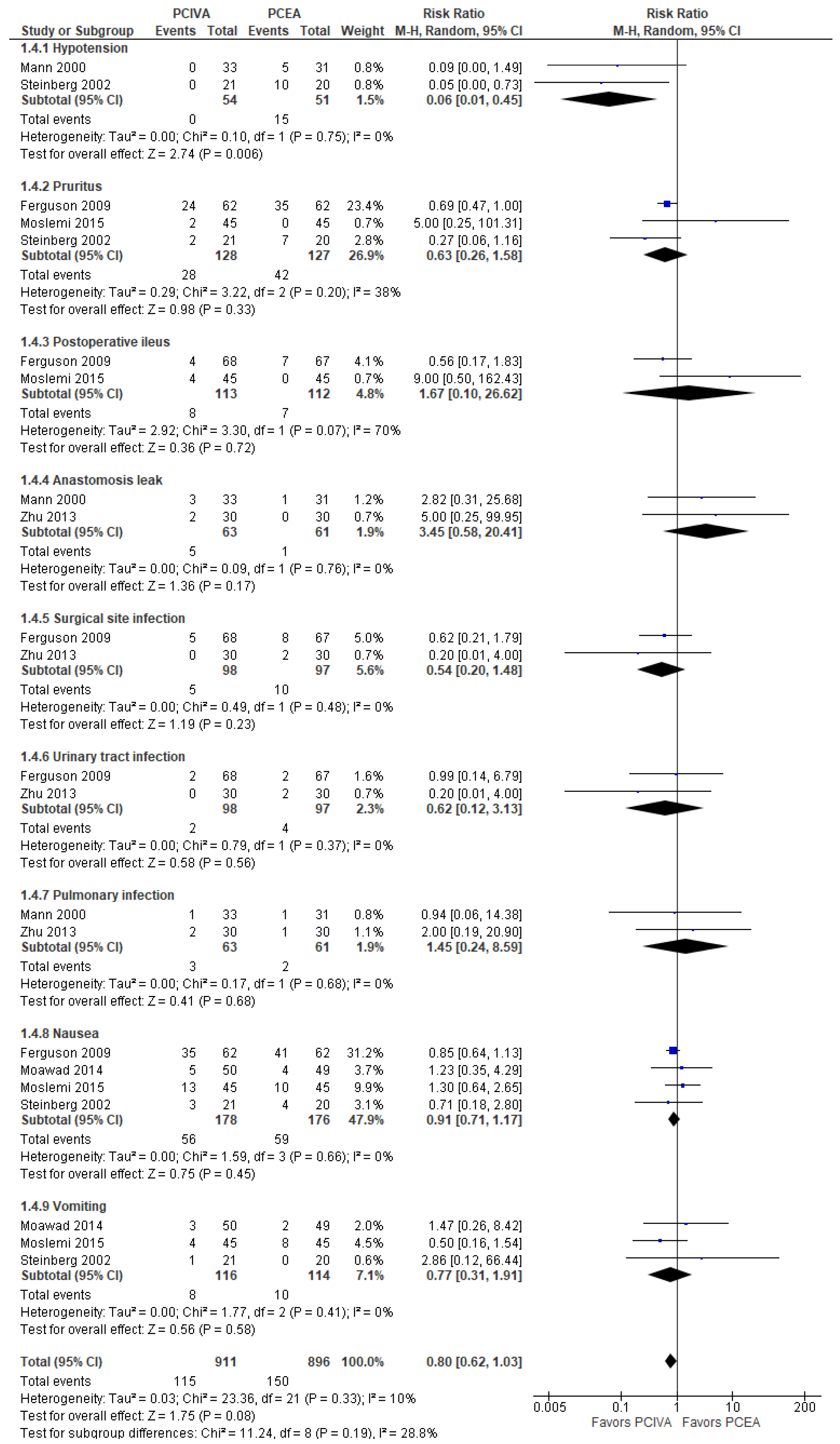
3.4. Postoperative Complications
3.5. Length of Stay (Days)
3.6. Assessment of the Methodological Quality (Jadad/Oxford Quality Scoring System)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gottschalk, A.; Durieux, M.E.; Nemergut, E.C. Intraoperative Methadone Improves Postoperative Pain Control in Patients Undergoing Complex Spine Surgery. Anesth. Analg. 2011, 112, 218–223. [Google Scholar] [CrossRef]
- Egbert, A.M.; Parks, L.H.; Short, L.M.; Burnett, M.L. Randomized Trial of Postoperative Patient-Controlled Analgesia vs. Intramuscular Narcotics in Frail Elderly Men. Arch. Intern. Med. 1990, 150, 1897–1903. [Google Scholar] [CrossRef] [PubMed]
- Hudcova, J.; McNicol, E.; Quah, C.; Lau, J.; Carr, D.B. Patient Controlled Opioid Analgesia versus Conventional Opioid Analgesia for Postoperative Pain. Cochrane Database Syst. Rev. 2006. [Google Scholar] [CrossRef]
- McNicol, E.D.; Ferguson, M.C.; Hudcova, J. Patient controlled opioid analgesia versus non-patient controlled opioid analgesia for postoperative pain. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef]
- Walder, B.; Schafer, M.; Henzi, I.; Tramèr, M.R. Efficacy and Safety of Patient-Controlled Opioid Analgesia for Acute Postoperative Pain. Acta Anaesthesiol. Scand. 2001, 45, 795–804. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.M.; Ip, W.Y.; Cheung, T.H. Patient-Controlled Analgesia versus Conventional Intramuscular Injection: A Cost Effectiveness Analysis. J. Adv. Nurs. 2004, 46, 531–541. [Google Scholar] [CrossRef]
- Schug, S.A.; Torrie, J.J. Safety Assessment of Postoperative Pain Management by an Acute Pain Service. Pain 1993, 55, 387–391. [Google Scholar] [CrossRef]
- Salicath, J.H.; Yeoh, E.C.Y.; Bennett, M.H. Epidural Analgesia versus Patient-Controlled Intravenous Analgesia for Pain Following Intra-Abdominal Surgery in Adults. Cochrane Database Syst. Rev. 2018, 2018. [Google Scholar] [CrossRef]
- Hanna, M.N.; Murphy, J.D.; Kumar, K.; Wu, C.L. Regional Techniques and Outcome: What Is the Evidence? Curr. Opin. Anaesthesiol. 2009, 22, 672–677. [Google Scholar] [CrossRef]
- Mann, C.; Pouzeratte, Y.; Boccara, G.; Peccoux, C.; Vergne, C.; Brunat, G.; Domergue, J.; Millat, B.; Colson, P. Comparison of Intravenous or Epidural Patient-Controlled Analgesia in the Elderly after Major Abdominal Surgery. Anesthesiology 2000, 92, 433. [Google Scholar] [CrossRef] [PubMed]
- Carli, F.; Trudel, J.L.; Belliveau, P. The Effect of Intraoperative Thoracic Epidural Anesthesia and Postoperative Analgesia on Bowel Function after Colorectal Surgery: A Prospective, Randomized Trial. Dis. Colon Rectum 2001, 44, 1083–1089. [Google Scholar] [CrossRef] [PubMed]
- Rigg, J.R.A.; Jamrozik, K.; Myles, P.S.; Silbert, B.S.; Peyton, P.J.; Parsons, R.W.; Collins, K.S. Epidural Anaesthesia and Analgesia and Outcome of Major Surgery: A Randomised Trial. Lancet 2002, 359, 1276–1282. [Google Scholar] [CrossRef]
- Tilleul, P.; Aissou, M.; Bocquet, F.; Thiriat, N.; le Grelle, O.; Burke, M.J.; Hutton, J.; Beaussier, M. Cost-Effectiveness Analysis Comparing Epidural, Patient-Controlled Intravenous Morphine, and Continuous Wound Infiltration for Postoperative Pain Management after Open Abdominal Surgery. Br. J. Anaesth. 2012, 108, 998–1005. [Google Scholar] [CrossRef] [PubMed]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds, D.J.M.; Gavaghan, D.J.; McQuay, H.J. Assessing the Quality of Reports of Randomized Clinical Trials: Is Blinding Necessary? Control. Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef]
- Luo, D.; Wan, X.; Liu, J.; Tong, T. Optimally Estimating the Sample Mean from the Sample Size, Median, Mid-Range, and/or Mid-Quartile Range. Stat. Methods Med. Res. 2018, 27, 1785–1805. [Google Scholar] [CrossRef] [PubMed]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the Sample Mean and Standard Deviation from the Sample Size, Median, Range and/or Interquartile Range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef] [PubMed]
- El Sayed Moawad, H.; Mokbel, E.M. Postoperative Analgesia after Major Abdominal Surgery: Fentanyl-Bupivacaine Patient Controlled Epidural Analgesia versus Fentanyl Patient Controlled Intravenous Analgesia. Egypt. J. Anaesth. 2014, 30, 393–397. [Google Scholar] [CrossRef][Green Version]
- Moslemi, F.; Rasooli, S.; Baybordi, A.; Golzari, S.E.J. A Comparison of Patient Controlled Epidural Analgesia with Intravenous Patient Controlled Analgesia for Postoperative Pain Management after Major Gynecologic Oncologic Surgeries: A Randomized Controlled Clinical Trial. Anesthesiol. Pain Med. 2015, 5, e29540. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.; Wang, C.; Xu, C.; Cai, Q. Influence of Patient-Controlled Epidural Analgesia versus Patient-Controlled Intravenous Analgesia on Postoperative Pain Control and Recovery after Gastrectomy for Gastric Cancer: A Prospective Randomized Trial. Gastric Cancer 2013, 16, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Fayed, N.A.; Abo El-Wafa, H.B.; Gab-Alla, N.M.; Yassen, K.A.; Lotfy, M.E. Comparison between Intravenous Patient Controlled Analgesia and Patient Controlled Epidural Analgesia in Cirrhotic Patients after Hepatic Resection. Middle East J. Anesthesiol. 2014, 22, 467–476. [Google Scholar]
- Ferguson, S.E.; Malhotra, T.; Seshan, V.E.; Levine, D.A.; Sonoda, Y.; Chi, D.S.; Barakat, R.R.; Abu-Rustum, N.R. A Prospective Randomized Trial Comparing Patient-Controlled Epidural Analgesia to Patient-Controlled Intravenous Analgesia on Postoperative Pain Control and Recovery after Major Open Gynecologic Cancer Surgery. Gynecol. Oncol. 2009, 114, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, R.B.; Liu, S.S.; Wu, C.L.; Mackey, D.C.; Grass, J.A.; Ahlén, K.; Jeppsson, L. Comparison of Ropivacaine-Fentanyl Patient-Controlled Epidural Analgesia with Morphine Intravenous Patient-Controlled Analgesia for Perioperative Analgesia and Recovery after Open Colon Surgery. J. Clin. Anesth. 2002, 14, 571–577. [Google Scholar] [CrossRef]
- Beattie, W.S.; Badner, N.H.; Choi, P. Epidural Analgesia Reduces Postoperative Myocardial Infarction: A Meta-Analysis. Anesth. Analg. 2001, 93, 853–858. [Google Scholar] [CrossRef] [PubMed]
| Author, Citation | Country | Study Design | Study Goals | Age | N of Patients: Total (Intervention/Control) | Group | Diagnosis | Surgery | General Anesthesia | ASA | Dose of Opioids and Local Anesthetics | Postoperative Analgesia | Conclusions |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ferguson, 2009 [21] | USA | RCT | Primary—pain at rest and cough (VAS, 0–10). Secondary—GI and GU function, time to discharge | PCEA: 57 C: 55 | 135 (67/68) | PCEA C: IV PCA | Gynecologic cancer | Open GYN cancer surgery | Yes | - | PCEA: morphine 100 μg/mL, 0.05% bupivacaine, 4 mL/h. Rescue: 4 mL every 0.5 h | All: 15–30 mg IV ketorolac every 8 h, 2 post-op days PCEA: morphine 100 μg/mL, 0.05% bupivacaine, 4 mL/h, continuous Rescue: 4 mL every 0.5 h C: morphine, 1 mg/h, continuous Rescue PCA: 1 mg every 10 min | PCEA provides better analgesia after open GYN cancer resections |
| Zhu, 2013 [19] | China | RCT | Pain (VAS, 0–10), blood sugar, time to flatus, safety, duration of hospital stay | 20-75 PCEA: 61.1 (12.6) PCIA: 59.6 (13.0) | 60 (30/30) | PCEA: T8-T9 PCIA | Gastric cancer | Gastrectomy | Yes | - | PCEA: 0.05% bupivacaine, 100 μg/mL morphine, 4 mL/h, 2 days. Rescue: 4 mL, 0.5 h lockout | All: pethidine. PCEA: 0.05 % bupivacaine, 100 μg/mL morphine, 4 mL/h continuous, 2 days. Rescue: 4 mL, 0.5 h lockout PCIA: morphine, 1 mg/h, continuous. Rescue: 1 mg every 10 min | After gastrectomy, PCEA provided safer and better pain control and faster recovery of GI function. |
| Moawad, 2014 [17] | Egypt | RCT | Pain (NPRS, 0–10), rescue analgesia use, sedation, and patient satisfaction. Complications (PONV, shivering, pruritus, or pulmonary problems) | 20-60 PCEA: 44.45 (10.56)PCIA: 45.20 (10.61) | 99 (49/50) | PCEA: T10-12 PCIA: IV | - | Abdominal surgery | Yes | I, II | PCEA: bupivacaine 0.125%, fentanyl | All: Rescue 0.5 μg/kg IV fentanyl PCEA: fentanyl 5 μg/mL, bupivacaine 0.125% (1.25 mg/mL), bolus PCIA: fentanyl 20 μg/mL, bolus | PCEA demonstrated superior analgesia, less sedation, and higher patient satisfaction. |
| Moslemi, 2015 [18] | Iran | RCT | Primary—pain (VAS, 1–10). Secondary—rescue analgesia use, side effects (nausea, vomiting, ileus, pruritis, sedation, pulmonary problems) | 40-60 IVPCA: 53.8 (11.4) PCEA: 49.9 (8.8) | 90 (45/45) | PCEA: L2-L3 IVPCA | Ovarian, endometrial, cervical cancer | GYN cancer surgeries | Yes | I, II | PCEA: 0.5% bupivacaine 120 mg (24 mL) (bupivacaine hydrochloride 50 mg/20 mL), fentanyl 150 µg (3 mL) in saline. 6–8 mL/h, 2 mL every 15 min on demand. | All: rescue—pethidine (0.5 mg/kg IV) PCEA: 0.5% bupivacaine 120 mg (24 mL) (bupivacaine hydrochloride 50 mg/20 mL), fentanyl 150 µg (3 mL) in saline. 6–8 mL/h, 2 mL bolus every 15 min on demand IVPCA: 300 µg (6 mL) fentanyl, 200 mg (4 mL) pethidine, 8 mg (2 mL) ondansetron in 0.9% saline, total 100 mL. 6–8 mL/h, 2 mL bolus every 15 min, on demand. | Epidural analgesia provided lower sedation and less respiratory depression |
| Fayed, 2014 [20] | Egypt | RCT | Primary—pain. Secondary—side effects (sedation, PONV, urinary retention, pulmonary and neurological complications), recovery of GI function, duration of ICU and hospital stay. | P: 50.1 (9.7)E: 50.8 (11.5) | 34 (17/17) | E: epidural T11-T12 P: IV PCA | Liver cirrhosis | Hepatic resection | Yes | I, II | E: bupivacaine 0.125%, 2 µg/mL fentanyl | All: IV pethidine, paracetamol E: bupivacaine 0.125%, 2 µg/mL fentanyl. 6 mL/h, continuous, 3 mL bolus every 15 min. P: IV fentanyl 15 μg, 10 min lockout, 90 μg/h maximum. | IV PCA and epidural analgesia are similarly efficient. Higher risk of coagulopathy in cirrhotic patients favors IVPCA. |
| Steinberg, 2002 [22] | USA | RCT | Primary—duration of hospital stay. Secondary—recovery, safety | 18-80 PCEA: 62 (10) IV PCA: 61 (15) | 41 (20/21) | PCEA IV PCA | - | Open colon surgery | Yes | I-III | PCEA: ropivacaine 0.2%, fentanyl (2 g/mL), 8 mL/h intraoperatively | All: ketorolac 15 mg. After 3 days, ibuprofen 400 mg PO 4/day until discharge or post-op day 6 PCEA: ropivacaine 0.2%, fentanyl (2 g/mL), 4 mL/h 2 mL ropivacaine/fentanyl bolus, 15 min lockout. Rescue—5 mL ropivacaine 2 mg/mL, fentanyl 2 g/mL, in 15 min. If needed, another bolus in 0.5 h. If inadequate analgesia—4–6 mL ropivacaine 7.5 mg/mL. IV PCA: morphine 0.1 mg/kg intraoperatively | PCEA offers better pain management, lowers opioid use, and enables faster recovery. |
| Mann, 2000 [10] | France | RCT | Primary—pain and side effects. Secondary—mental status and complications (GI, pulmonary, and hemodynamic) | PCA: 76.8 (4.7) PCEA: 76.1 (5.6) | 70 (35/35) | IVPCA PCEA: T7-T9 or T9-T11 | - | Colectomy, gastrectomy, cephalic panreatectomy | Yes | I, II | PCEA: intraoperative 0.25% bupivacaine, 1 pg/mL sufentanil, postoperative 0.125% bupivacaine, 0.5-pg/mL sufentanil, 2–3 mL, 12 min lockout, 3–5 mL/h | IV PCA: 1.5 mg morphine bolus, 8 min lockout. PCEA: 2–3 mL, 12 min lockout, 3–5 mL/h, continuous. | Epidural analgesia provides superior pain control and better mental and GI activity but did not improve postoperative delirium or complications rate. |
| Study or Subgroup | Was This Study Described as Randomized? | Was the Method Used to Generate the Sequence of Randomization Appropriate and Described? | Was the Study Described as Double-Blind? | Was the Method of Double-Blind Appropriate and Described? | Was There a Description of Withdraw and Dropouts? | Total Score |
|---|---|---|---|---|---|---|
| Fayed, 2014 [20] | 1 | 0 | 0 | 0 | 0 | 1 |
| Ferguson, 2009 [21] | 1 | 0 | 0 | 0 | 1 | 2 |
| Mann, 2000 [10] | 1 | 1 | 0 | 0 | 1 | 3 |
| Moawad, 2014 [17] | 1 | 1 | 0 | 0 | 1 | 3 |
| Moslemi, 2015 [18] | 1 | 1 | 0 | 0 | 1 | 3 |
| Steinberg, 2002 [22] | 1 | 0 | 0 | 0 | 1 | 2 |
| Zhu, 2013 [19] | 1 | 0 | 0 | 0 | 1 | 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Viderman, D.; Tapinova, K.; Nabidollayeva, F.; Tankacheev, R.; Abdildin, Y.G. Intravenous versus Epidural Routes of Patient-Controlled Analgesia in Abdominal Surgery: Systematic Review with Meta-Analysis. J. Clin. Med. 2022, 11, 2579. https://doi.org/10.3390/jcm11092579
Viderman D, Tapinova K, Nabidollayeva F, Tankacheev R, Abdildin YG. Intravenous versus Epidural Routes of Patient-Controlled Analgesia in Abdominal Surgery: Systematic Review with Meta-Analysis. Journal of Clinical Medicine. 2022; 11(9):2579. https://doi.org/10.3390/jcm11092579
Chicago/Turabian StyleViderman, Dmitriy, Karina Tapinova, Fatima Nabidollayeva, Ramil Tankacheev, and Yerkin G. Abdildin. 2022. "Intravenous versus Epidural Routes of Patient-Controlled Analgesia in Abdominal Surgery: Systematic Review with Meta-Analysis" Journal of Clinical Medicine 11, no. 9: 2579. https://doi.org/10.3390/jcm11092579
APA StyleViderman, D., Tapinova, K., Nabidollayeva, F., Tankacheev, R., & Abdildin, Y. G. (2022). Intravenous versus Epidural Routes of Patient-Controlled Analgesia in Abdominal Surgery: Systematic Review with Meta-Analysis. Journal of Clinical Medicine, 11(9), 2579. https://doi.org/10.3390/jcm11092579