Genito Pelvic Pain/Penetration Disorder (GPPPD) in Spanish Women—Clinical Approach in Primary Health Care: Review and Meta-Analysis
Abstract
:1. Introduction
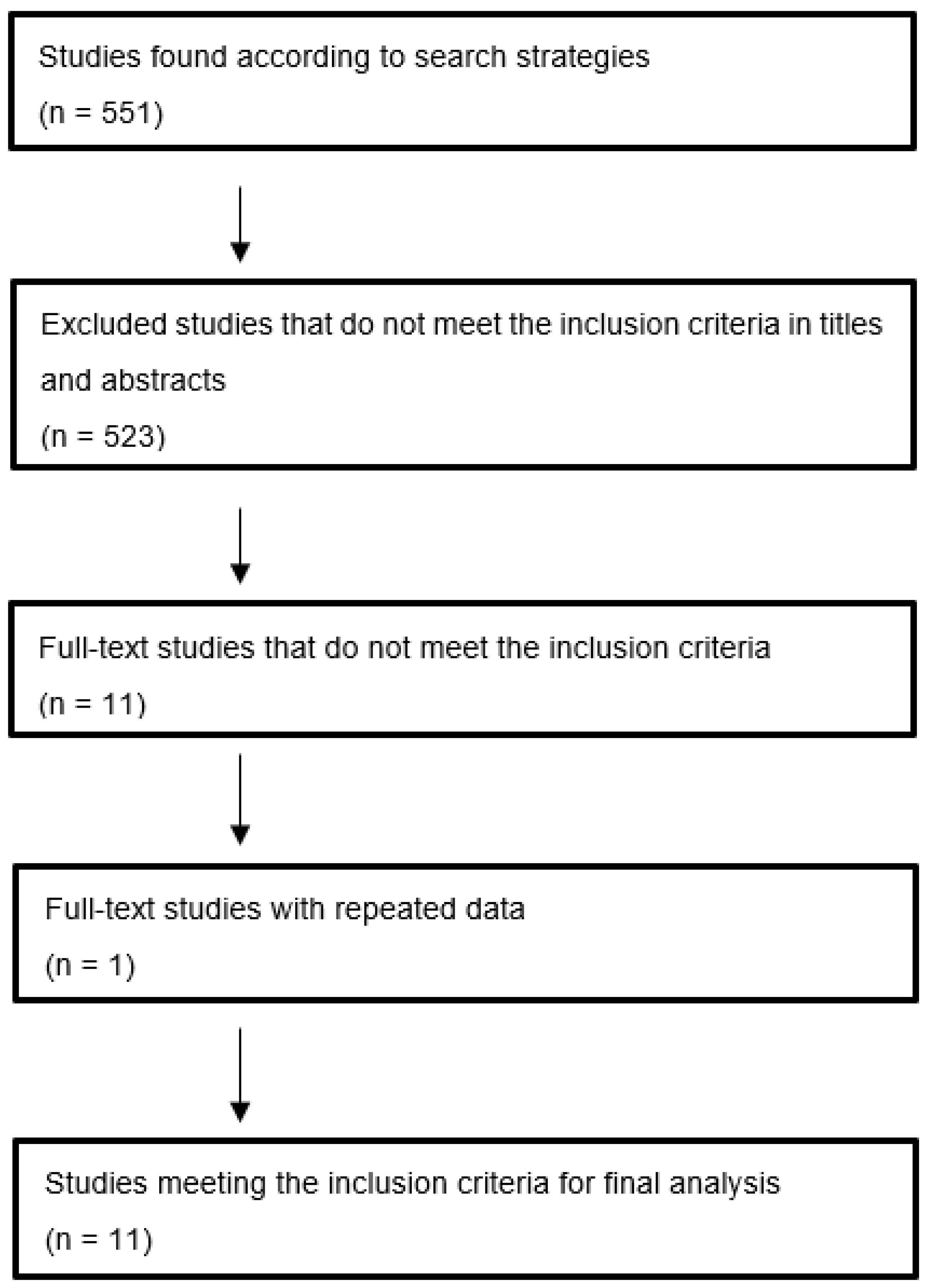
2. Materials and Methods
2.1. Design
2.2. Protocol
2.3. Selection Criteria
- Inclusion criteria: (1) All studies published in Spanish that aimed to analyze GPPPD in Spain and (2) studies including patients from primary health care centers or their support services in Spain.
- Exclusion criteria: (1) Editorials, letters to the editor, or clinical cases and (2) studies not undertaken in Spanish primary health care centers or their support services.
2.4. Information Sources and Search
2.5. Study Selection
2.6. Data Extraction
2.7. Methodological Evaluation of the Studies
2.8. Statistical Analysis
2.9. Risk of Bias
3. Results
4. Discussion
5. Clinical Approach
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Manohar, J.S.; Rao, S.S.; Tandon, A.; Rao, T.S.S. Healthy Sexuality. In Quality of Life—Biopsychosocial Perspectives; Irtelli, F., Durbano, F., Taukeni, S.G., Eds.; IntechOpen: London, UK, 2020; Available online: https://www.intechopen.com/chapters/72056 (accessed on 10 March 2022). [CrossRef]
- Brajkovic, L.; Hernandez, R.; Navarro-Cremades, F.; Azim, S.A.; Pacheco Palha, A. Sexual Disorders. In Person Centered Psychiatry; Mezzich, J., Botbol, M., Christodoulou, G., Cloninger, C.R., Salloum, I., Eds.; Springer: Cham, Switzerland, 2016; pp. 393–412. [Google Scholar] [CrossRef]
- Navarro-Cremades, F.; Simonelli, C.; Montejo, A.L. Sexual disorders beyond DSM-5: The unfinished affaire. Curr. Opin. Psychiatry 2017, 30, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Bitzer, J.; Kirana, P.S. Female Sexual Dysfunctions. In Psychiatry and Sexual Medicine; Lew-Starowicz, M., Giraldi, A., Krüger, T., Eds.; Springer: Cham, Switzerland, 2021; pp. 109–134. [Google Scholar]
- Montejo, A.L.; Montejo, L.; Navarro-Cremades, F. Sexual side-effects of antidepressant and antipsychotic drugs. Curr. Opin. Psychiatry 2015, 28, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Montejo, A.L.; Montejo, L.; Baldwin, D.S. The impact of severe mental disorders and psychotropic medications on sexual health and its implications for clinical management. World Psychiatry 2018, 17, 3–11. [Google Scholar] [CrossRef] [Green Version]
- Montejo, A.L.; Prieto, N.; de Alarcón, R.; Casado-Espada, N.; de la Iglesia, J.; Montejo, L. Management Strategies for Antidepressant-Related Sexual Dysfunction: A Clinical Approach. J. Clin. Med. 2019, 7, 1640. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Montejo, A.L.; de Alarcón, R.; Prieto, N.; Acosta, J.M.; Buch, B.; Montejo, L. Management Strategies for Antipsychotic-Related Sexual Dysfunction: A Clinical Approach. J. Clin. Med. 2021, 10, 308. [Google Scholar] [CrossRef]
- Reed, G.M.; Drescher, J.; Krueger, R.B.; Atalla, E.; Cochran, S.D.; First, M.B.; Cohen-Kettenis, P.T.; Arango-de Montis, I.; Parish, S.J.; Cottler, S.; et al. Disorders related to sexuality and gender identity in the ICD-11: Revising the ICD-10 classification based on current scientific evidence, best clinical practices, and human rights considerations. World Psychiatry 2016, 15, 205–221, Erratum in: World Psychiatry 2017, 16, 220. [Google Scholar] [CrossRef] [Green Version]
- American Psychiatric Association. DSM-5. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM IV-TR; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM IV; American Psychiatric Association: Washington, DC, USA, 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM III-TR; American Psychiatric Association: Washington, DC, USA, 1987. [Google Scholar]
- ICD-10. Available online: https://icd.who.int/browse10/2010/en?msclkid=3a473fbbbcf411eca51eae9f16243848#/V (accessed on 20 December 2021).
- ICD-11. Available online: https://icd.who.int/browse11/l-m/en (accessed on 3 January 2022).
- Binik, Y.M.; Reissing, E.; Pukall, C.; Flory, N.; Payne, K.A.; Khalifé, S. The female sexual pain disorders: Genital pain or sexual dysfunction? Arch. Sex. Behav. 2002, 31, 425–429. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; Version 6.3 (Updated February 2022); Cochrane: London, UK, 2022; Available online: www.training.cochrane.org/handbook (accessed on 10 March 2022).
- PRISMA Statement. Available online: http://www.prisma-statement.org/ (accessed on 3 November 2021).
- PICO. Available online: https://guides.nyu.edu/c.php?g=276561&p=1847897 (accessed on 3 November 2021).
- Lee, J.-H.; Ahn, J.; Park, W.S.; Choe, E.K.; Kim, E.; Shin, R.; Heo, S.C.; Jung, S.; Kim, K.; Chai, Y.J.; et al. Colorectal Cancer Prognosis Is Not Associated with BRAF and KRAS Mutations-A STROBE Compliant Study. J. Clin. Med. 2019, 8, 111. [Google Scholar] [CrossRef] [Green Version]
- Joanna Briggs Institute. Checklist for Systematic Reviews and Research Syntheses. 2017. Available online: https://jbi.global/critical-appraisal-tools (accessed on 1 February 2022).
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Qureshi, R.; Mattis, P.; Lisy, K.; et al. Chapter 7: Systematic reviews of etiology and risk. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, South Australia, 2020; Available online: https://synthesismanual.jbi.global (accessed on 10 March 2022).
- Bown, M.J.; Sutton, A.J. Quality Control in Systematic Reviews and Meta-analyses. Eur. J. Vasc. Endovasc. Surg. 2010, 40, 669–677. [Google Scholar] [CrossRef] [Green Version]
- StatsDirect Medical Statistics Software. Available online: www.statsdirect.com (accessed on 7 November 2021).
- Alonso, P.; Urrutia, G.; Solà, I.; Rigaua, D. Metaanálisis: ¿efectos fijos o aleatorios? Med. Contin. Aten. Prim. 2009, 16, 305–306. [Google Scholar] [CrossRef]
- Barili, F.; Parolari, A.; Kappetein, P.A.; Freemantle, N. Statistical Primer: Heterogeneity, random- or fixed-effects model analyses? Interact. Cardiovasc. Thorac. Surg. 2018, 27, 317–321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- West, S.L.; Gartlehner, G.; Mansfield, A.J.; Poole, C.; Tant, E.; Lenfestey, N.; Lux, L.J.; Amoozegar, J.; Morton, S.C.; Carey, T.C.; et al. Comparative Effectiveness Review Methods: Clinical Heterogeneity; Methods Research Paper. AHRQ Publication No. 10-EHC070-EF; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2010. Available online: https://www.ncbi.nlm.nih.gov/books/NBK53310/ (accessed on 22 November 2021).
- Huedo-Medina, T.B.; Sánchez-Meca, J.; Marín-Martínez, F.; Botella, J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol. Methods 2006, 11, 193–206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cochrane. Available online: https://uk.cochrane.org/news/how-read-forest-plot (accessed on 2 February 2021).
- Woodall, G.M. Graphical Depictions of Toxicological Data. In Encyclopedia of Toxicology, 3rd ed.; Wexler, P., Ed.; Elsevier Science & Technology: Amsterdam, The Netherlands, 2014; pp. 786–795. [Google Scholar]
- Van Enst, W.A.; Ochodo, E.; Scholten, R.J.P.M.; Hooft, L.; Leeflang, M.M. Investigation of publication bias in meta-analyses of diagnostic test accuracy: A meta-epidemiological study. BMC Med. Res. Methodol. 2014, 14, 70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, L.; Chu, H. Quantifying Publication Bias in Meta-Analysis. Biometrics 2018, 74, 785–794. [Google Scholar] [CrossRef] [PubMed]
- Begg, C.B.; Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef] [PubMed]
- Harbord, R.M.; Egger, M.; Sterne, J.A.C. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat. Med. 2006, 25, 3443–3457. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [Green Version]
- Delgado, M.; Palma, S. Consideraciones prácticas acerca de la detección del sesgo de publicación. Gac. Sanit. 2006, 20, 10–16. [Google Scholar]
- Ballester, R.; Gil, M.D. Estudio epidemiológico sobre la prevalencia de disfunciones sexuales en la comunidad valenciana. Psicothema 1995, 7, 95–104. [Google Scholar]
- Marqués, M.J.; Caballero, J. Análisis de la población femenina atendida por dificultades sexuales en centros de orientación familiar. Cuad. Med. Psicosom. Psiquiatr. Enlace 1999, 49, 19–30. [Google Scholar]
- Ávila, J.J.; Pérez, A.; Olazábal, J.C.; López, J. Disfunciones sexuales en el alcoholismo. Adicciones 2004, 18, 1–6. [Google Scholar]
- Hurtado, F.; Ciscar, C.; Rubio, M. Conflicto de pareja y violencia de género. Rev. Psicopatol. Y Psicol. 2004, 9, 49–64. [Google Scholar]
- Tomás, R.; Tárraga, P.J.; Álvarez, M.C.; Cerdán, M.; Celada, A.; Solera, J. Disfunciones sexuales en Atención Primaria. MGF 2007, 92, 13–23. [Google Scholar]
- García-Giralda, L.; Guirao, L.; Delgadillo, J.; Torres, F. Assessment of sexual health in primary care centres in Spain. The impact of hysterectomy on female sexual dysfunctions. In Proceedings of the 12th World Congress on Menopause, Madrid, Spain, 19–23 May 2008; Volume 11. PS-99. [Google Scholar] [CrossRef]
- García, L.; Guirao, L.; Alfaro, J.V.; Casas, I.; Torralba, Y.; Izquierdo, M.T. Disfunciones sexuales en el sistema sanitario: ¿y nosotras qué? Rev. Int. Androl. Internet 2008, 6, 23–26. [Google Scholar]
- López, J. Trastorno del deseo sexual hipoactivo: Comparación de 2 cuestionarios (Breve Perfil de la Función Sexual Femenina, y Salud y Disfunción Sexual Femenina en Atención primaria) en 2 grupos de mujeres (ovariectomizadas e histerectomizadas, y normales). Clin. Investig. Ginecol. Obs. 2010, 37, 14–26. [Google Scholar]
- Olivares, J.; Sánchez, M.; De Miguel, M. Disfunción sexual femenina en atención primaria: Estudio de prevalencia. Med. Gen. 2012, 1, 71–78. [Google Scholar]
- Hurtado, F.; Donat, F.; Alcaraz, M.; Pellicer, R.; Royo, A.; Cantero, J. Características de la demanda asistencial de la población inmigrante en salud sexual con perspectiva de género. Rev. Esp. Sexol. 2012, 2, 9–32. [Google Scholar]
- López, J. Diferencias en disfunciones sexuales y depresión entre mujeres premenopáusicas (de 40-50 años) y mujeres posmenopáusicas (de 50–60 años). Estudio prospectivo de un año. Clin. Investig. Ginecol. Obs. 2016, 43, 50–57. [Google Scholar]
- Martínez Lomakin, F.; Madrid Aris, E. Revisiones sistemáticas de la literatura: Una introducción para el clínico ocupado. Systematic reviews of biomedical literature: An introduction for busy clinicians. Medwave 2014, 14, e5955. [Google Scholar] [CrossRef]
- Sutton, A.J.; Higgins, J.P. Recent developments in meta-analysis. Stat. Med. 2008, 27, 625–650. [Google Scholar] [CrossRef]
- Laumann, E.O.; Nicolosi, A.; Glasser, D.B.; Paik, A.; Gingell, C.; Moreira, E.; Wang, T. Sexual problems among women and men aged 40-80 years: Prevalence and correlates identified in the Global Study of Sexual Attitudes and Behaviors. Int. J. Impot. Res. 2005, 17, 39–57. [Google Scholar] [CrossRef] [Green Version]
- Alizadeh, A.; Farnam, F.; Raisi, F.; Parsaeian, M. Prevalence of and Risk Factors for Genito-Pelvic Pain/Penetration Disorder: A Population-Based Study of Iranian Women. J. Sex. Med. 2019, 16, 1068–1077. [Google Scholar] [CrossRef]
- Mitchell, K.R.; Geary, R.; Graham, C.A.; Datta, J.; Wellings, K.; Sonnenberg, P.; Field, N.; Nunns, D.; Bancroft, J.; Jones, K.G.; et al. Painful sex (dyspareunia) in women: Prevalence and associated factors in a British population probability survey. BJOG 2017, 124, 1689–1697. [Google Scholar] [CrossRef] [Green Version]
- Briken, P.; Matthiesen, S.; Pietras, L.; Wiessner, C.; Klein, V.; Reed, G.M.; Dekker, A. Estimating the Prevalence of Sexual Dysfunction Using the New ICD-11 Guidelines. Dtsch. Arztebl. Int. 2020, 117, 653–658. [Google Scholar] [CrossRef]
- Kliesch, S. The connection between general and sexual health. The publication of the GeSiD study. Dtsch. Arztebl. Int. 2020, 117, 643–644. [Google Scholar] [CrossRef]
- Ricoy-Cano, A.J.; Obrero-Gaitán, E.; Caravaca-Sánchez, F.; Fuente-Robles, Y.M.D.L. Factors Conditioning Sexual Behavior in Older Adults: A Systematic Review of Qualitative Studies. J. Clin. Med. 2020, 9, 1716. [Google Scholar] [CrossRef]
- Balon, R.; Woodard, T.L. Diagnosis of Female Sexual Dysfunction. In Management of Sexual Dysfunction in Men and Women; Lipshultz, L., Pastuszak, A., Goldstein, A., Giraldi, A., Perelman, M., Eds.; Springer: New York, NY, USA, 2016; pp. 213–222. [Google Scholar]
- Derogatis, L.R.; Balon, R. Clinical evaluation of sexual dysfunctions. In Clinical Manual of Sexual Disorders; Balon, R., Segraves, R.T., Eds.; American Psychiatric Publishing: Arlington, VA, USA, 2009; pp. 23–57. [Google Scholar]
- Bortun, A.-M.C.; Ivan, V.; Navolan, D.-B.; Dehelean, L.; Borlea, A.; Stoian, D. Thyroid Autoimmune Disease—Impact on Sexual Function in Young Women. J. Clin. Med. 2021, 10, 369. [Google Scholar] [CrossRef]
- Barra, F.; Scala, C.; Leone Roberti Maggiore, U.; Ferrero, S. Long-Term Administration of Dienogest for the Treatment of Pain and Intestinal Symptoms in Patients with Rectosigmoid Endometriosis. J. Clin. Med. 2020, 9, 154. [Google Scholar] [CrossRef] [Green Version]
- Comptour, A.; Lambert, C.; Chauvet, P.; Figuier, C.; Gremeau, A.-S.; Canis, M.; Pereira, B.; Bourdel, N. Long-Term Evolution of Quality of Life and Symptoms Following Surgical Treatment for Endometriosis: Different Trajectories for Which Patients? J. Clin. Med. 2020, 9, 2461. [Google Scholar] [CrossRef]
- Donnez, J.; Dolmans, M.-M. Endometriosis and Medical Therapy: From Progestogens to Progesterone Resistance to GnRH Antagonists: A Review. J. Clin. Med. 2021, 10, 1085. [Google Scholar] [CrossRef]
- Tai, F.-W.; Chang, C.Y.-Y.; Chiang, J.-H.; Lin, W.-C.; Wan, L. Association of Pelvic Inflammatory Disease with Risk of Endometriosis: A Nationwide Cohort Study Involving 141,460 Individuals. J. Clin. Med. 2018, 7, 379. [Google Scholar] [CrossRef] [Green Version]
- Balzarro, M.; Rubilotta, E.; Antonelli, A. Cystocele Repair by a Modified Surgical Technique of Bilateral Pubococcygeus Plication: Long-Term Surgical and Functional Results. J. Clin. Med. 2020, 9, 3318. [Google Scholar] [CrossRef]
- Elessawy, M.; Schneekloth, S.; Günther, V.; Maass, N.; Mettler, L.; Alkatout, I. Postoperative Telephone-Based Questionnaire on Quality of Life after Robotic-Assisted Laparoscopic Hysterectomy versus Conventional Total Laparoscopic Hysterectomy. J. Clin. Med. 2020, 9, 2849. [Google Scholar] [CrossRef]
- Cuenca-Barrales, C.; Ruiz-Villaverde, R.; Molina-Leyva, A. Sexual Distress in Patients with Hidradenitis Suppurativa: A Cross-Sectional Study. J. Clin. Med. 2019, 8, 532. [Google Scholar] [CrossRef] [Green Version]
- Lev-Sagie, A.; Wertman, O.; Lavee, Y.; Granot, M. Vestibular Anatomic Localization of Pain Sensitivity in Women with Insertional Dyspareunia: A Different Approach to Address the Variability of Painful Intercourse. J. Clin. Med. 2020, 9, 2023. [Google Scholar] [CrossRef]
- Tempest, N.; Efstathiou, E.; Petros, Z.; Hapangama, D.K. Laparoscopic Outcomes after Normal Clinical and Ultrasound Findings in Young Women with Chronic Pelvic Pain: A Cross-Sectional Study. J. Clin. Med. 2020, 9, 2593. [Google Scholar] [CrossRef]
- Parish, S.J.; Cottler-Casanova, S.; Clayton, A.H.; McCabe, M.C.; Coleman, E.; Reed, G.M. The Evolution of the Female Sexual Disorder/Dysfunction Definitions, Nomenclature, and Classifications: A Review of DSM, ICSM, ISSWSH, and ICD. Sex. Med. 2021, 9, 36–56. [Google Scholar] [CrossRef]


| Author/Year | No. of Women Evaluated | Study Location |
|---|---|---|
| Ballester Arnal R, 1995 [37] | 644 | Population, Valencia-Castellón |
| Marques Matéu MJ, 1999 [38] | 128 | SRHM *, Villareal |
| Ávila Escribano JJ, 2004 [39] | 33 | Alcoholism Unit, Salamanca |
| Hurtado Murillo F, 2004 [40] | 39 | SRHM *, Valencia |
| Tomás R, 2007 [41] | 47 | Health center, Albacete |
| García-Giralda L, 2008 [42] | 2599 | Health centers in Spain |
| García L, 2008 [43] | 403 | Health center, Murcia |
| López Olmos J, 2010 [44] | 98 | Specialty center, Valencia |
| Olivares Ortiz J, 2012 [45] | 226 | Health center, Madrid |
| Hurtado Murillo F, 2012 [46] | 625 | SRHM *, Valencia |
| López Olmos J, 2016 [47] | 453 | Specialty center, Valencia |
| Begg-Mazumdar: Kendall’s tau = 0.236364 p = 0.3587 |
| Egger: bias = 4.057145 (95% CI = 1.060592 to 9.174882) p = 0.1065 |
| Harbord: bias = 3.144143 (92.5% CI = 4.248425 to 10.536711) p = 0.4142 |
| Authors | Type of Study/Design | Intervention | Results |
|---|---|---|---|
| Ballester Arnal R, 1995 | Analytical cross-sectional study | BES questionnaire not validated. 20 items. Two main variables: experience of suffering from sexual dysfunctions (DSM III-R) and item about the size of the penis. DSM-III-TR | Dyspareunia 29% Vaginismus 5% |
| Marques Matéu MJ, 1999 | Case control study | Reference to DSM-IV. | Dyspareunia19.5% Vaginismus 5% |
| Ávila Escribano JJ, 2004 | Analytical cross-sectional study | Self-administered and anonymous survey containing sociodemographic questions and the LoPiccolo Sexual History Questionnaire | Dyspareunia 5% Vaginismus 10% |
| Hurtado Murillo F, 2004 | Analytical cross-sectional study | Self-Applied Marital Adjustment Scale; Beck-depression inventory BDI, State Trait Anxiety questionnaire, Personality Questionnaire EPI, Seef- esteem survey EAE | Dyspareunia 5.13% Vaginismus 0% |
| Tomás R, 2007 | Analytical cross-sectional study | Psychological well-being (IBP questionnaire) and quality and satisfaction (LISAT-8). A questionnaire was developed following DSM-IV criteria | Penetration Pain 12.8% |
| García-Giralda L, 2008 | Analytical Cross-sectional, multicenter study | Validated questionnaire on female sexual health and dysfunction (SyDSF). DSM-IV-TR. | Penetration Pain 6.93% |
| García L, 2008 | Analytical cross sectional multicenter study | Validated questionnaire on female sexual health and dysfunction (SyDSF). DSM-IV-TR. | Penetration Pain 11% |
| López Olmos J, 2010 | Case-control study | Female health and sexual dysfunction questionnaire in primary care (SyDSF-Ap) | Dyspareunia 26.92% |
| Olivares Ortiz J, 2012 | Analytical cross-sectional study | FMS questionnaire for female sexual disfunction | Penetration Pain 2.6% |
| Hurtado Murillo F, 2012 | Analytical cross-sectional study, clinical sample; SD | Review of medical records | Dyspareunia 5.3% |
| López Olmos J, 2016 | Analytical cross-sectional study | Brief Profile of Female Sexual Function (BPFSF) questionnaire. | Dyspareunia 24.28% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berenguer-Soler, M.; Navarro-Sánchez, A.; Compañ-Rosique, A.; Luri-Prieto, P.; Navarro-Ortiz, R.; Gómez-Pérez, L.; Pérez-Tomás, C.; Font-Juliá, E.; Gil-Guillén, V.F.; Cortés-Castell, E.; et al. Genito Pelvic Pain/Penetration Disorder (GPPPD) in Spanish Women—Clinical Approach in Primary Health Care: Review and Meta-Analysis. J. Clin. Med. 2022, 11, 2340. https://doi.org/10.3390/jcm11092340
Berenguer-Soler M, Navarro-Sánchez A, Compañ-Rosique A, Luri-Prieto P, Navarro-Ortiz R, Gómez-Pérez L, Pérez-Tomás C, Font-Juliá E, Gil-Guillén VF, Cortés-Castell E, et al. Genito Pelvic Pain/Penetration Disorder (GPPPD) in Spanish Women—Clinical Approach in Primary Health Care: Review and Meta-Analysis. Journal of Clinical Medicine. 2022; 11(9):2340. https://doi.org/10.3390/jcm11092340
Chicago/Turabian StyleBerenguer-Soler, María, Antonio Navarro-Sánchez, Antonio Compañ-Rosique, Paloma Luri-Prieto, Ramón Navarro-Ortiz, Luis Gómez-Pérez, Carla Pérez-Tomás, Elsa Font-Juliá, Vicente F. Gil-Guillén, Ernesto Cortés-Castell, and et al. 2022. "Genito Pelvic Pain/Penetration Disorder (GPPPD) in Spanish Women—Clinical Approach in Primary Health Care: Review and Meta-Analysis" Journal of Clinical Medicine 11, no. 9: 2340. https://doi.org/10.3390/jcm11092340
APA StyleBerenguer-Soler, M., Navarro-Sánchez, A., Compañ-Rosique, A., Luri-Prieto, P., Navarro-Ortiz, R., Gómez-Pérez, L., Pérez-Tomás, C., Font-Juliá, E., Gil-Guillén, V. F., Cortés-Castell, E., Navarro-Cremades, F., Montejo, A. L., Arroyo-Sebastián, M. d. Á., & Pérez-Jover, V. (2022). Genito Pelvic Pain/Penetration Disorder (GPPPD) in Spanish Women—Clinical Approach in Primary Health Care: Review and Meta-Analysis. Journal of Clinical Medicine, 11(9), 2340. https://doi.org/10.3390/jcm11092340








