The Treatment of Heart Failure in Patients with Chronic Kidney Disease: Doubts and New Developments from the Last ESC Guidelines
Abstract
:1. Introduction
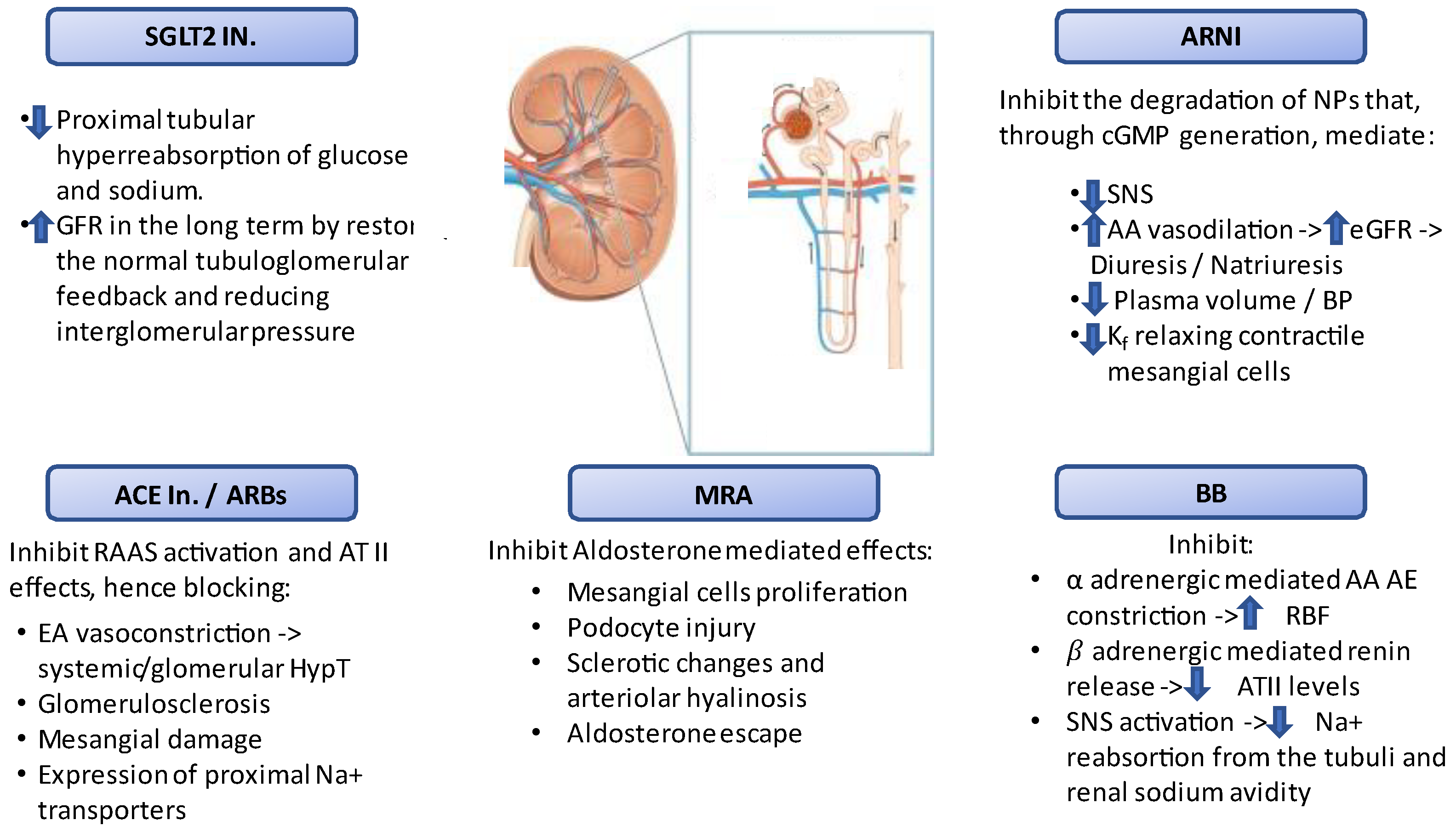
2. Clinical Characteristics of Patients with Chronic Kidney Disease and Heart Failure
3. Therapeutic Target and Limitations in Patients with Heart Failure and Chronic Kidney Disease
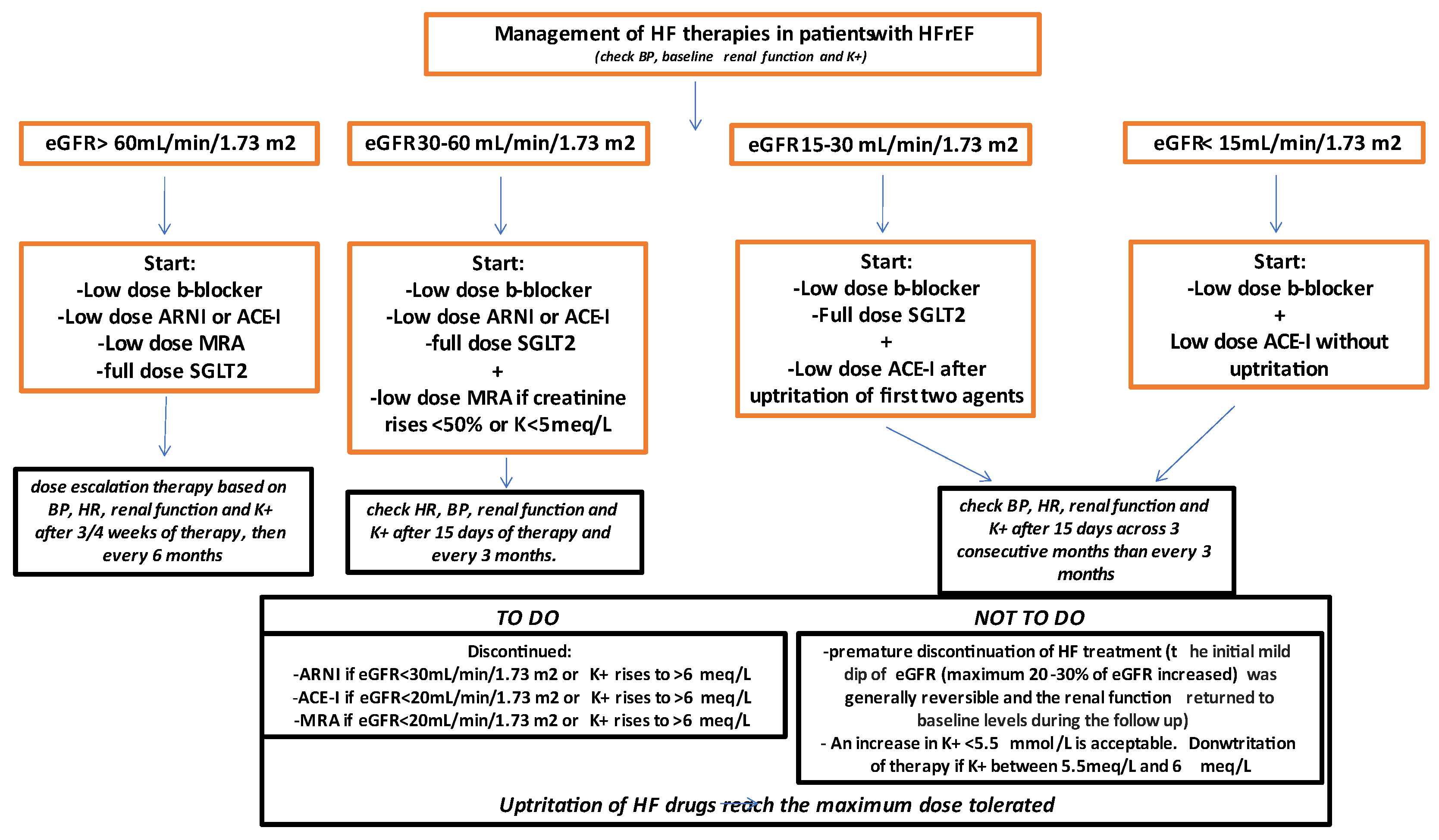
4. Renal Diagnostic Exams and Comparison between Different Criteria
5. Potential Strategy for the Correct Use of Neuro-Hormonal Inhibition Treatments According to Renal Dysfunction Severity
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Bohm, M.; Burri, H.; Butler, J.; Celutkiene, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic. Eur. Heart J. 2021, 42, 4901. [Google Scholar] [CrossRef] [PubMed]
- Onyali, C.B.; Anim-Koranteng, C.; Shah, H.E.; Bhawnani, N.; Ethirajulu, A.; Alkasabera, A.; Mostafa, J.A. Role of Selective Sodium-Glucose Co-Transporter-2 Inhibitors in Managing Cardio-Renal Complications in Type 2 Diabetes Mellitus: Beyond Glycemic Control. Cureus 2021, 13, e17452. [Google Scholar] [CrossRef] [PubMed]
- Ruocco, G.; Palazzuoli, A.; Ter Maaten, J.M. Loop diuretics in acute heart failure: Beyond the decongestive relief for the kidney. Crit. Care 2015, 19, 296. [Google Scholar]
- Palazzuoli, A.; Ruocco, G.; Pellegrini, M.; Martini, S.; Del Castillo, G.; Beltrami, M.; Franci, B.; Lucani, B.; Nuti, R. Patients with cardiorenal syndrome revealed increased neurohormonal activity, tubular and myocardial damage compared to heart failure patients with preserved renal function. Cardiorenal Med. 2014, 4, 257–268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beltrami, M.; Ruocco, G.; Ibrahim, A.; Lucani, B.; Franci, B.; Nuti, R.; Palazzuoli, A. Different trajectories and significance of B-type natriuretic peptide, congestion and acute kidney injury in patients with heart failure. Intern. Emerg. Med. 2017, 12, 593–603. [Google Scholar] [CrossRef]
- Di Lullo, L.; Bellasi, A.; Barbera, V.; Ronco, C. Cardionephrology and cardiorenal disease in Italy: State of the art. Rev. Cardiovasc. Med. 2021, 22, 563–572. [Google Scholar] [CrossRef]
- Palazzuoli, A.; Beltrami, M.; Nodari, S.; McCullough, P.A.; Ronco, C. Clinical impact of renal dysfunction in heart failure. Rev. Cardiovasc. Med. 2011, 12, 186–199. [Google Scholar] [CrossRef]
- Lofman, I.; Szummer, K.; Evans, M.; Carrero, J.J.; Lund, L.H.; Jernberg, T. Incidence of, associations with and prognostic impact of worsening renal function in heart failure with different ejection fraction categories. Am. J. Cardiol. 2019, 124, 1575–1583. [Google Scholar] [CrossRef]
- Quiroz, R.; Doros, G.; Shaw, P.; Liang, C.S.; Gauthier, D.F.; Sam, F. Comparison of characteristics and outcomes of patients with heart failure preserved ejection fraction versus reduced left ventricular ejection fraction in an urban cohort. Am. J. Cardiol. 2014, 113, 691–696. [Google Scholar] [CrossRef]
- Ather, S.; Chan, W.; Bozkurt, B.; Aguilar, D.; Ramasubbu, K.; Zachariah, A.A.; Wehrens, X.H.; Deswal, A. Impact of noncardiac comorbidities on morbidity and mortality in a predominantly male population with heart failure and preserved versus reduced ejection fraction. J. Am. Coll. Cardiol. 2012, 59, 998–1005. [Google Scholar] [CrossRef] [Green Version]
- McAlister, F.A.; Ezekowitz, J.; Tarantini, L.; Squire, I.; Komajda, M.; Bayes-Genis, A.; Gotsman, I.; Whalley, G.; Earle, N.; Poppe, K.K.; et al. Renal dysfunction in patients with heart failure with preserved versus reduced ejection fraction: Impact of the new Chronic Kidney Disease-Epidemiology Collaboration Group formula. Circ. Heart Fail. 2012, 5, 309–314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Streng, K.W.; Nauta, J.F.; Hillege, H.L.; Anker, S.D.; Cleland, J.G.; Dickstein, K.; Filippatos, G.; Lang, C.C.; Metra, M.; Ng, L.L.; et al. Non-cardiac comorbidities in heart failure with reduced, mid-range and preserved ejection fraction. Int. J. Cardiol. 2018, 271, 132–139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, G.L.; Lichtman, J.H.; Bracken, M.B.; Shlipak, M.G.; Phillips, C.O.; DiCapua, P.; Krumholz, H.M. Renal impairment and outcomes in heart failure: Systematic review and meta-analysis. J. Am. Coll. Cardiol. 2006, 47, 1987–1996. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Damman, K.; Valente, M.A.; Voors, A.A.; O’Connor, C.M.; van Veldhuisen, D.J.; Hillege, H. Renal impairment, worsening renal function, and outcome in patients with heart failure: An updated meta-analysis. Eur. Heart J. 2014, 35, 455–469. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meta-Analysis Global Group in Chronic Heart Failure. The survival of patients with heart failure with preserved or reduced left ventricular ejection fraction: An individual patient data meta-analysis. Eur. Heart J. 2012, 33, 1750–1757. [Google Scholar] [CrossRef] [Green Version]
- Lofman, I.; Szummer, K.; Dahlstrom, U.; Jernberg, T.; Lund, L.H. Associations with and prognostic impact of chronic kidney disease in heart failure with preserved, mid-range, and reduced ejection fraction. Eur. J. Heart Fail. 2017, 19, 1606–1614. [Google Scholar] [CrossRef] [Green Version]
- Ruocco, G.; Palazzuoli, A.; Ter Maaten, J.M. The role of the kidney in acute and chronic heart failure. Heart Fail. Rev. 2020, 25, 107–118. [Google Scholar] [CrossRef]
- Beldhuis, I.E.; Streng, K.W.; van der Meer, P.; Ter Maaten, J.M.; O’Connor, C.M.; Metra, M.; Dittrich, H.C.; Ponikowski, P.; Cotter, G.; Cleland, J.G.F.; et al. Trajectories of Changes in Renal Function in Patients with Acute Heart Failure. J. Card Fail. 2019, 25, 866–874. [Google Scholar] [CrossRef] [Green Version]
- Bowling, C.B.; Sanders, P.W.; Allman, R.M.; Rogers, W.J.; Patel, K.; Aban, I.B.; Rich, M.W.; Pitt, B.; White, M.; Bakris, G.C.; et al. Effects of enalapril in systolic heart failure patients with and without chronic kidney disease: Insights from the SOLVD Treatment trial. Int. J. Cardiol. 2013, 167, 151–156. [Google Scholar] [CrossRef] [Green Version]
- Jose, P.; Skali, H.; Anavekar, N.; Tomson, C.; Krumholz, H.M.; Rouleau, J.L.; Moye, L.; Pfeffer, M.A.; Solomon, S.D. Increase in creatinine and cardiovascular risk in patients with systolic dysfunction after myocardial infarction. J. Am. Soc. Nephrol. 2006, 17, 2886–2891. [Google Scholar] [CrossRef]
- Køber, L.; Torp-Pedersen, C.; Carlsen, J.E.; Bagger, H.; Eliasen, P.; Lyngborg, K.; Videbaek, J.; Cole, D.S.; Auclert, L.; Pauly, N.C. A clinical trial of the angiotensin-converting-enzyme inhibitor trandolapril in patients with left ventricular dysfunction after myocardial infarction. Trandolapril Cardiac Evaluation (TRACE) Study Group. N. Engl. J. Med. 1995, 333, 1670–1676. [Google Scholar] [CrossRef] [PubMed]
- Cohn, J.N.; Tognoni, G.; Valsartan Heart Failure Trial Investigators. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N. Engl. J. Med. 2001, 345, 1667–1675. [Google Scholar] [CrossRef] [PubMed]
- Young, J.B.; Dunlap, M.E.; Pfeffer, M.A.; Probstfield, J.L.; Cohen-Solal, A.; Dietz, R.; Granger, C.B.; Hradec, J.; Kuch, J.; McKelvie, R.S.; et al. Candesartan in Heart failure Assessment of Reduction in Mortality and morbidity (CHARM) Investigators and Committees. Mortality and morbidity reduction with Candesartan in patients with chronic heart failure and left ventricular systolic dysfunction: Results of the CHARM low-left ventricular ejection fraction trials. Circulation 2004, 110, 2618–2626. [Google Scholar] [PubMed] [Green Version]
- McCallum, W.; Tighiouart, H.; Ku, E.; Salem, D.; Sarnak, M.J. Acute declines in estimated glomerular filtration rate on enalapril and mortality and cardiovascular outcomes in patients with heart failure with reduced ejection fraction. Kidney Int. 2019, 96, 1185–1194. [Google Scholar] [CrossRef] [PubMed]
- Brenner, B.M.; Cooper, M.E.; de Zeeuw, D.; Keane, W.F.; Mitch, W.E.; Parving, H.H.; Remuzzi, G.; Snapinn, S.M.; Zhang, Z.; Shahinfar, S.; et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N. Engl. J. Med. 2001, 345, 861–869. [Google Scholar] [CrossRef] [Green Version]
- Badve, S.V.; Roberts, M.A.; Hawley, C.M.; Cass, A.; Garg, A.X.; Krum, H.; Tonkin, A.; Perkovic, V. Effects of beta-adrenergic antagonists in patients with chronic kidney disease: A systematic review and meta-analysis. J. Am. Coll. Cardiol. 2011, 58, 1152–1161. [Google Scholar] [CrossRef] [Green Version]
- Ghali, J.K.; Wikstrand, J.; Van Veldhuisen, D.J.; Fagerberg, B.; Goldstein, S.; Hjalmarson, A.; Johansson, P.; Kjekshus, J.; Ohlsson, L.; Samuelsson, O.; et al. The influence of renal function on clinical outcome and response to beta-blockade in systolic heart failure: Insights from Metoprolol CR/XL Randomized Intervention Trial in Chronic HF (MERIT-HF). J. Card. Fail. 2009, 15, 310–318. [Google Scholar] [CrossRef]
- Wali, R.K.; Iyengar, M.; Beck, G.J.; Chartyan, D.M.; Chonchol, M.; Lukas, M.A.; Cooper, C.; Himmelfarb, J.; Weir, M.R.; Berl, T.; et al. Efficacy and safety of carvedilol in treatment of heart failure with chronic kidney disease: A meta-analysis of randomized trials. Circ. Heart Fail. 2011, 4, 18–26. [Google Scholar] [CrossRef] [Green Version]
- Cice, G.; Ferrara, L.; D’Andrea, A.; D’Isa, S.; Di, B.A.; Cittadini, A.; Russo, P.E.; Golino, P.; Calabro, R. Carvedilol increases two-year survivalin dialysis patients with dilated cardiomyopathy: A prospective, placebo-controlled trial. J. Am. Coll. Cardiol. 2003, 41, 1438–1444. [Google Scholar] [CrossRef] [Green Version]
- Zannad, F.; McMurray, J.J.; Krum, H.; van Veldhuisen, D.J.; Swedberg, K.; Shi, H.; Vincent, J.; Pocock, S.J.; Pitt, B.; EMPHASIS-HF Study Group. Eplerenone in patients with systolic heart failure and mild symptoms. N. Engl. J. Med. 2011, 364, 11–21. [Google Scholar] [CrossRef] [Green Version]
- Ferreira, J.P.; Abreu, P.; McMurray, J.J.V.; van Veldhuisen, D.J.; Swedberg, K.; Pocock, S.J.; Vincent, J.; Lins, K.; Rossignol, P.; Pitt, B. Renal function stratified dose comparisons of eplerenone versus placebo in the EMPHASIS-HF trial. Eur. J. Heart Fail. 2019, 21, 345–351. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bakris, G.L.; Agarwal, R.; Anker, S.D.; Pitt, B.; Ruilope, L.M.; Rossing, P.; Kolkhof, P.; Nowack, C.; Schloemer, P.; Joseph, A. Effect of Finerenone on Chronic Kidney Disease Outcomes in Type 2 Diabetes. N. Engl. J. Med. 2020, 383, 2219–2229. [Google Scholar] [CrossRef] [PubMed]
- Damman, K.; Gori, M.; Claggett, B.; Jhund, P.S.; Senni, M.; Lefkowitz, M.P.; Prescott, M.F.; Shi, V.C.; Rouleau, J.L.; Swedberg, K.; et al. Renal effects and associated outcomes during angiotensin-neprilysin inhibition in heart failure. JACC Heart Fail. 2018, 6, 489–498. [Google Scholar] [CrossRef] [PubMed]
- Packer, M.; Claggett, B.; Lefkowitz, M.P.; McMurray, J.J.V.; Rouleau, J.L.; Solomon, S.D.; Zile, M.R. Effect of neprilysin inhibition on renal function in patients with type 2 diabetes and chronic heart failure who are receiving target doses of inhibitors of the renin-angiotensin system: A secondary analysis of the PARADIGM-HF trial. Lancet Diabetes Endocrinol. 2018, 6, 547–554. [Google Scholar] [CrossRef]
- Mc Causland, F.R.; Lefkowitz, M.P.; Claggett, B.; Anavekar, N.S.; Senni, M.; Gori, M.; Jhund, P.S.; McGrath, M.M.; Packer, M.; Shi, V.; et al. Angiotensin-Neprilysin Inhibition and Renal Outcomes in Heart Failure With Preserved Ejection Fraction. Circulation 2020, 142, 1236–1245. [Google Scholar] [CrossRef] [PubMed]
- Lytvyn, Y.; Bjornstad, P.; Udell, J.A.; Lovshin, J.A.; Cherney, D.Z.I. Sodium Glucose Cotransporter-2 Inhibition in Heart Failure: Potential Mechanisms, Clinical Applications, and Summary of Clinical Trials. Circulation 2017, 136, 1643–1658. [Google Scholar] [CrossRef]
- Seferović, P.M.; Fragasso, G.; Petrie, M.; Mullens, W.; Ferrari, R.; Thum, T.; Bauersachs, J.; Anker, S.D.; Ray, R.; Çavuşoğlu, Y.; et al. Sodium-glucose co-transporter 2 inhibitors in heart failure: Beyond glycaemic control. A position paper of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2020, 22, 1495–1503. [Google Scholar] [CrossRef]
- Liu, X.; Xu, C.; Xu, L.; Li, X.; Sun, H.; Xue, M.; Li, T.; Yu, X.; Sun, B.; Chen, L. Empagliflozin improves diabetic renal tubular injury by alleviating mitochondrial fission via AMPK/SP1/PGAM5 pathway. Metabolism 2020, 111, 154334. [Google Scholar] [CrossRef]
- Hawley, S.A.; Ford, R.J.; Smith, B.K.; Gowans, G.J.; Mancini, S.J.; Pitt, R.D.; Day, E.A.; Salt, I.P.; Steinberg, G.R.; Hardie, D.G. The Na+/Glucose Cotransporter Inhibitor Canagliflozin Activates AMPK by Inhibiting Mitochondrial Function and Increasing Cellular AMP Levels. Diabetes 2016, 65, 2784–2794. [Google Scholar] [CrossRef] [Green Version]
- Zeng, Q.; Zhou, Q.; Liu, W.; Wang, Y.; Xu, X.; Xu, D. Mechanisms and Perspectives of Sodium-Glucose Co-transporter 2 Inhibitors in Heart Failure. Front. Cardiovasc. Med. 2021, 10, 636152. [Google Scholar] [CrossRef]
- Bae, J.H.; Park, E.G.; Kim, S.; Kim, S.G.; Hahn, S.; Kim, N.H. Effects of sodium-glucose cotransporter 2 inhibitors on renal outcomes in patients with type 2 diabetes: A systematic review and meta-analysis of randomized controlled trials. Sci. Rep. 2019, 9, 13009. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Packer, M.; Anker, S.D.; Butler, J.; Filippatos, G.; Pocock, S.J.; Carson, P.; Januzzi, J.; Verma, S.; Tsutsui, H.; Brueckmann, M.; et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N. Engl. J. Med. 2020, 383, 1413–1424. [Google Scholar] [CrossRef] [PubMed]
- Zannad, F.; Ferreira, J.P.; Pocock, S.J.; Zeller, C.; Anker, S.D.; Butler, J.; Filippatos, G.; Hauske, S.J.; Brueckmann, M.; Pfarr, E.; et al. Cardiac and Kidney Benefits of Empagliflozin in Heart Failure Across the Spectrum of Kidney Function: Insights From EMPEROR-Reduced. Circulation 2021, 143, 310–321. [Google Scholar] [CrossRef] [PubMed]
- Heerspink, H.J.L.; Oshima, M.; Zhang, H.; Li, J.; Agarwal, R.; Capuano, G.; Charytan, D.M.; Craig, J.; de Zeeuw, D.; Di Tanna, G.L.; et al. Canagliflozin and Kidney-Related Adverse Events in Type 2 Diabetes and CKD: Findings From the Randomized CREDENCE Trial. Am. J. Kidney Dis. 2022, 79, 244–256.e1. [Google Scholar] [CrossRef]
- McMurray, J.J.V.; Solomon, S.D.; Inzucchi, S.E.; Kober, L.; Kosiborod, M.N.; Martinez, F.A.; Ponikowski, P.; Sabatine, M.S.; Anand, I.S.; Belohlavek, J.; et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N. Engl. J. Med. 2019, 381, 1995–2008. [Google Scholar] [CrossRef] [Green Version]
- Jhund, P.S.; Solomon, S.D.; Docherty, K.F.; Heerspink, H.J.L.; Anand, I.S.; Bohm, M.; Chopra, V.; de Boer, R.A.; Desai, A.S.; Ge, J.; et al. Efficacy of Dapagliflozin on Renal Function and Outcomes in Patients With Heart Failure With Reduced Ejection Fraction: Results of DAPA-HF. Circulation 2021, 143, 298–309. [Google Scholar] [CrossRef]
- Heerspink, H.J.L.; Stefánsson, B.V.; Correa-Rotter, R.; Chertow, G.M.; Greene, T.; Hou, F.-F.; Mann, J.F.E.; McMurray, J.J.V.; Lindberg, M.; Rossing, P.; et al. Dapagliflozin in patients with chronic kidney disease. N. Engl. J. Med. 2020, 383, 1436–1446. [Google Scholar] [CrossRef]
- Voors, A.A.; Mulder, H.; Reyes, E.; Cowie, M.R.; Lassus, J.; Hernandez, A.F.; Ezekowitz, J.A.; Butler, J.; O’Connor, C.M.; VICTORIA Study Group. Renal function and the effects of vericiguat in patients with worsening heart failure with reduced ejection fraction: Insights from the VICTORIA (Vericiguat Global Study in Subjects with HFrEF) trial. Eur. J. Heart Fail. 2021, 23, 1313–1321. [Google Scholar] [CrossRef]
- Lim, S.L.; Gandhi, M.; Woo, K.L.; Chua, H.R.; Lim, Y.C.; Sim, D.K.L.; Lee, S.S.G.; Teoh, Y.L.; Richards, A.M.; Lam, C.S.P. Nitrates in combination with hydralazine in cardiorenal syndrome: A randomized controlled proof-of-concept study. ESC Heart Fail. 2020, 7, 4267–4276. [Google Scholar] [CrossRef]
- Lim Shir, L.; Benson, L.; Dahlström, U.; Lam Carolyn, S.P.; Lund Lars, H. Association between use of long-acting nitrates and outcomes in heart failure with preserved ejection fraction. Circ. Heart Fail. 2017, 10, e003534. [Google Scholar]
- Zamora, E.; Lupón, J.; Vila, J.; Urrutia, A.; de Antonio, M.; Sanz, H.; Grau, M.; Ara, J.; Bayés-Genís, A. Estimated glomerular filtration rate and prognosis in heart failure: Value of the Modification of Diet in Renal Disease Study-4, chronic kidney disease epidemiology collaboration, and cockroft-gault formulas. J. Am. Coll. Cardiol. 2012, 59, 1709–1715. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valente, M.A.; Hillege, H.L.; Navis, G.; Voors, A.A.; Dunselman, P.H.; van Veldhuisen, D.J.; Damman, K. The Chronic Kidney Disease Epidemiology Collaboration equation outperforms the Modification of Diet in Renal Disease equation for estimating glomerular filtration rate in chronic systolic heart failure. Eur. J. Heart Fail. 2014, 16, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Mullens, W.; Damman, K.; Testani, J.M.; Martens, P.; Mueller, C.; Lassus, J.; Tang, W.H.W.; Skouri, H.; Verbrugge, F.H.; Orso, F.; et al. Evaluation of kidney function throughout the heart failure trajectory—a position statement from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2020, 22, 584–603. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.X.; Sun, L.; Nicholas, S.B.; Lu, Y.; Sinha, S.K.; Hua, R. Comparison of bias and accuracy using cystatin C and creatinine in CKD-EPI equations for GFR estimation. Eur. J. Intern. Med. 2020, 80, 29–34. [Google Scholar] [CrossRef]
- Pottel, H.; Bjork, J.; Courbebaisse, M.; Couzi, L.; Ebert, N.; Eriksen, B.O.; Dalton, R.N.; Dubourg, L.; Gaillard, F.; Garrouste, C.; et al. Development and validation of a modified full age spectrum creatinine-based equation to estimate glomerular filtration rate: A cross-sectional analysis of pooled data. Ann. Intern. Med. 2020, 174, 183–191. [Google Scholar] [CrossRef]
- Ando, T.; Okuhara, Y.; Orihara, Y.; Nishimura, K.; Yamamoto, K.; Masuyama, T.; Hirotani, S. Urinary composition predicts diuretic efficiency of hypertonic saline solution with furosemide therapy and heart failure prognosis. Heart Vessels 2018, 33, 1029–1036. [Google Scholar] [CrossRef]
- Palazzuoli, A.; Tecson, K.M.; Ronco, C.; McCullough, P.A. Nomenclature for Kidney Function from KDIGO: Shortcomings of Terminology Oversimplification. Cardiorenal Med. 2021, 11, 119–122. [Google Scholar] [CrossRef]
- Poniatowski, B.; Malyszko, J.; Bachorzewska-Gajewska, H.; Malyszko, J.S.; Dobrzycki, S. Serum neutrophil gelatinase-associated lipocalin as a marker of renal function in patients with chronic heart failure and coronary artery disease. Kidney Blood Press Res. 2009, 32, 77–80. [Google Scholar] [CrossRef]
- Ter Maaten, J.M.; Beldhuis, I.E.; van der Meer, P.; Krikken, J.A.; Coster, J.E.; Nieuwland, W.; van Veldhuisen, D.J.; Voors, A.A.; Damman, K. Natriuresis guided therapy in acute heart failure: Rationale and design of the Pragmatic Urinary Sodium-based Treatment algoritHm in Acute Heart Failure (PUSH-AHF) trial. Eur. J. Heart Fail. 2021, 24, 385–392. [Google Scholar] [CrossRef]
- Martens, P.; Dupont, M.; Verbrugge, F.H.; Damman, K.; Degryse, N.; Nijst, P.; Reynders, C.; Penders, J.; Tang, W.H.W.; Testani, J.; et al. Urinary sodium profiling in chronic heart failure to detect development of acute decompensated heart failure. JACC Heart Fail. 2019, 7, 404–414. [Google Scholar] [CrossRef]
- Cuthbert, J.J.; Bhandari, S.; Clark, A.L. Hypochloraemia in Patients with Heart Failure: Causes and Consequences. Cardiol. Ther. 2020, 9, 333–347. [Google Scholar] [CrossRef] [PubMed]
- Eichhorn, E.J.; Domanski, M.J.; Krause-Steinrauf, H.; Bristow, M.R.; Lavori, P.W. Beta-Blocker Evaluation of Survival Trial Investigators. A trial of the beta-blocker bucindolol in patients with advanced chronic heart failure. N. Engl. J. Med. 2001, 344, 1659–1667. [Google Scholar] [PubMed]
- Silva-Cardoso, J.; Brito, D.; Frazão, J.M.; Ferreira, A.; Bettencourt, P.; Branco, P.; Fonseca, C. Management of RAASi-associated hyperkalemia in patients with cardiovascular disease. Heart Fail Rev. 2021, 26, 891–896. [Google Scholar] [CrossRef] [PubMed]
| Clinical Scenarios | ||
|---|---|---|
| (1) “Pseudo” WRF | Good renal function at baseline and occurrence of WRF during hospitalization for acute HF, usually secondary to the decongestion therapy. | |
| (2) “True” WRF | WRF due to congestion and hypoperfusion, in which renal deterioration persisted also in the post-discharge period with a higher burden of HF re-hospitalization. | |
| (3) WRF in CKD | WRF could occur in the presence of CKD. This subtype was common in older patients with several comorbidities, where WRF reflected the real deterioration of the renal function, with worse prognostic value. | |
| Laboratory/urine Output Criteria | ||
| eGFR Criteria | Urine output criteria | |
| RIFLE (an acute rise in SCr over 7d) | ||
| Risk | Increased SCr ≥ ×1.5 or eGFR decrease > 25% | UO < 0.5 mL/kg/h × 6 h |
| Injury | Increase in SCr ≥ ×2 or eGFR decrease > 50% | UO < 0.5 mL/kg/h × 12 h |
| Failure | Increase in SCr ≥ ×3 or eGFR decrease > 75% or SCr ≥ 4.0 mg/dL | UO < 0.5 mL/kg/h × 24 h or anuria × 12 h |
| Loss | Persistent ARF = Complete loss of kidney function > 4 wk | |
| ESKD | End stage renal disease (>3 months) | |
| AKIN (an acute rise in SCr within 48 h) | ||
| Stage 1 | Same as RIFLE Risk or increase in SCr ≥ 0.3 mg/dL (≥26.4 μmol/L) | Same as RIFLE Risk |
| Stage 2 | Same as RIFLE Injury | Same as RIFLE Injury |
| Stage 3 | Increase in SCr ≥ ×3 or serum creatinine of ≥4.0 mg/dL with an acute increase of at least 0.5 mg/dL or RRT | Same as RIFLE Failure |
| Trial; Author; Year | Pts (n) | Design | Main Eligibility Criteria | Primary Outcome | Mean Follow up (years) | Renal Function Exclusion | CKD Groups (eGFR, mL/min/ 1.73 m2) | Main Findings |
|---|---|---|---|---|---|---|---|---|
| Angiotensin Converting Enzyme inhibitors | ||||||||
| CONSENSUS; 1987; The CONSENSUS Trial Study Group | 253 | Enalapril vs. Pl. | Congested HF, NYHA IV, cardiomegaly on chest X-ray | ACM | 0.5 | Serum creatinine concentration > 3.4 mg/dL | NA | Enalapril significantly reduced ACM in patients with sCr > 1.39 mg/dL compared to pl. (30% vs. 55%) but did not have a significant effect in those with sCr < 1.39 mg/dL. |
| SOLVD treatment; 1991; The SOLVD Investigators [19] | 2569 | Enalapril vs. Pl. | LVEF ≤ 35%, NYHA I–IV (90% NYHA II, III) | ACM | 3.4 | Creatinine > 2 mg/dL | ≥60 (n = 1466) (59, 7%) <60 (n = 1036) (40, 3%) | Enalapril reduced mortality and hospitalization in SHF patients without significant heterogeneity between those with and without CKD. |
| SOLVD prevention; 1992; The SOLVD Investigators | 4228 | Enalapril vs. Pl. | Receiving digitalis, diuretics, or vasodilators (remainder same as SOLVD treatment trial) | ACM | 3.08 | Creatinine > 2 mg/dL | <45 (n = 450) 10.6% ≥45 <60 (n = 669) 15.8% ≥60 <75 (n = 640) 15.1% >75 (n = 863) 20.4 | No significant interaction between CKD and treatment |
| SAVE; 1992; Tokmakova et al. [20] | 2331 | Captopril vs. Pl. | Acute myocardial infarction (age 21–80 years) LVEF < 40% | ACM | 3.5 | Creatinine > 2.5 mg/dL | ≥60 (n = 1562) 67% <60 (n = 769) 33% | Captopril reduced CV events irrespective of baseline kidney function. CKD was associated with a heightened risk for all major CV events after MI, particularly among subjects with an eGFR < 45 mL/min/1.73 m2. |
| AIRE; 1997; Hall et al. | 2006 | Ramipril vs. Pl. | Acute myocardial infarction (ECG and enzymes) and transient or persistent congestive heart failure after index infarct. Clinical CHF by physical examination or radiography. | ACM | 1.25 | NA | NA | ACM significantly lower for Ramipril (17%) than pl. (23%). |
| TRACE; 1995; Køber et al. [21] | 1749 | Trandolapril vs. Pl. | Able to tolerate a test dose of 0.5 mg trandolapril adults with acute myocardial infarction 2–6 days prior to trial entry. Echocardiographic ejection fraction < 35% | ACM | 3 | Creatinine > 2.5 mg/dL | NA | Trandalopril reduced relative risk of death. Trandolapril also reduces the risk of death from CV causes. |
| NETWORK; 1998; The NETWORK investigators | 1532 | Enalapril 2.5 vs. 5 vs. 10 mg BID | Age 18 to 85 years, NYHA II–IV, abnormality of the heart and current treatment for heart failure | ACM, HFH, WHF | 0.5 | Creatinine > 2.3 mg/dL | No relationship between dose of enalapril and clinical outcome in patients with HF. | |
| ATLAS; 1999; Packer et al. | 3174 | Lisinopril high vs. low dose | LVEF ≤ 30 NYHA II–IV | ACM | 3.8 | Creatinine > 2.5 mg/dL | Creatinine > 1.5 mg/dL 2176 (68.5%) Creatinine < 1.5 mg/dL 998 (31.5%) | ACM was non-significantly reduced both in patients with and without CKD. |
| Angiotensin Receptor Blockers | ||||||||
| Val-HeFT; 2003; Carson et al. [22] | 5010 | Valsartan vs. Pl. | LVEF < 40%; clinically stable CHF NYHA II–IV; treatment with ACE inhibitors; LVDD > 2.9 cm/bsa | ACM | 1.9 | Creatinine > 2.5 mg/dL | <60 2114 (47%) ≥60 2196 (53%) | Patients with WRF demonstrated the same benefits with valsartan treatment compared with pl. in the overall population. |
| CHARM added, 2001; McMurray et al. [23] | 2548 | Candesartan vs. Pl. | LVEF ≤ 40%; NYHA II–IV; treatment with ACE inhibitor | CV death or HFH | 3.4 | Creatinine >3 mg/dL | ≥60 67% <60 33% | The risk for CV death or hospitalization for worsening CHF as well as the risk for ACM increased significantly below an eGFR of 60 mL/min per 1.73 m2. |
| CHARM alternative, 2003; Granger et al. | 2028 | Candesartan vs. Pl. | CHF NYHA II–IV, LVEF ≤ 40%, ACE inhibitors intolerance | CV death or HFH | 2.8 | Creatinine > 3 mg/dL | ≥60 57.4% <60 42.6% | See above |
| HEEAL; 2009; Konstam et al. | 3846 | High dose vs. Low dose Losartan | LVEF ≤ 40%; NYHA II–IV; ACE inhibitors intolerance | ACM or HFH | 4.7 | Creatinine > 2.5 mg/dL | NA | Losartan 150 mg vs. 50 mg maintained its net clinical benefit and was associated with reduced risk of death or HFH, despite higher rates of WRF and greater rates of eGFR decline. |
| Mineralcorticoid Receptor Antagonist | ||||||||
| RALES; 1999; Kulbertus et al. | 1663 | Spironolactone vs. Pl. | LVEF < 35%; NYHA III–IV; creatinine ≤ 2.5 mmol/L | ACM | 2 | creatinine ≥ 2.5 mg/dL | <60 (n = 792) 47.62% ≥60 (n = 866) 52.07% | Individuals with reduced baseline eGFR exhibited similar relative risk reductions in all-cause death and the combined. Endpoint of death or hospital stayed for HF as those with normal renal function and greater absolute risk reduction compared with those with a higher baseline eGFR. |
| EMPHASIS-HF, 2001; Zannad et al. [30] | 2737 | Eplerenone vs. Pl. | LVEF ≤ 35%; NYHA II; eGFR ≥ 30 mL/min/1.73 m | CV death or HFH | 1.75 | eGFR < 30 mL/min/1.73 m | <60 (n = 912) 33.32% ≥60 (n = 1821) 66.53% | Eplerenone, as compared with placebo, reduced both the risk of death and the risk of hospitalization in HFrEF patients with CKD. |
| TOPCAT; 2021; Khumbanj, et al. | 3445 | Spironolactone vs. placebo (n = 3445) | LVEF ≥ 45%; HF hospitalization or elevated NP level; eGFR ≥ 30 mL/min/1.73 m2 or creatinine ≤ 2.5 | CV death or aborted cardiac arrest or hospitalization for HF | 3.3 | eGFR < 30 mL/min/1.73 m or serum creatinine >2.5 mg/dL | <45 (n = 411) 11.9% 45–60 (n = 533) 15.47% ≥60 (n = 823) 23.88% | The primary endpoint was similar between the spironolactone and placebo arms. The risk of adverse events was amplified in the lower eGFR categories. These data supported use of spironolactone to treat HFpEF patients with advanced CKD only when close laboratory surveillance was possible. |
| Trial; Author; Year | Pts (n) | Design | Main Eligibility Criteria | Primary outcome | Mean Follow up (years) | Renal Function Exclusion | CKD Groups (eGFR, mL/min/ 1.73 m2) | Main Findings |
|---|---|---|---|---|---|---|---|---|
| Beta-Blockers | ||||||||
| MDC; 1993; Waagstein et al. | 383 | Metoprolol vs. Pl. | LVEF ≤ 40%; NYHA II, III | ACM | 0.9 | NA | NA | Treatment with Metoprolol improved symptoms, LVEF, exercise time. It reduced PCWP and clinical deterioration. |
| CIBIS; 1994; CIBIS Investigators and Committees | 641 | Bisoprolol vs. Pl. | LVEF ≤ 40% NYHA III–IV Age 18–75 Treatment with diuretic and vasodilator | ACM | 1.9 | Creatinine > 3.4 mg/dL | Renal insufficiency being a non-inclusion criterion | No significant difference in mortality or sudden death. Improvements in functional status in the bisoprolol arm. |
| US-Carvedilol; 1996; Packer et al. | 1094 | Carvedilol vs. Pl. | LVEF ≤ 35%; NYHA II, III despite at least two months of treatment with diuretics and an ACE inhibitor | ACM | 0.5 | Clinical important renal disease | NA | Carvedilol reduced overall mortality rate, CV risk, hospitalization for CV reasons. |
| MERIT HF; 1999; MERIT-HF Study Group [27] | 3991 | Metoprolol vs. Pl. | LVEF ≤ 40%; NYHA II–IV | ACM | 1.0 | NA | <45 (n = 493) ≥ 45 ≤ 60 (n = 976) >60 (n = 2496) | Metoprolol CR/XL was effective in reducing death and hospitalizations for worsening HF in patients with eGFR < 45 as in those with eGFR > 60. eGFR was a powerful predictor of death and hospitalizations from HF. |
| CIBIS-II; 1999; CIBIS-II Investigators and Committees | 2289 | Bisoprolol vs. Pl. | LVEF ≤ 35%; NYHA III, IV | ACM | 1.3 | Creatinine > 3.4 mg/dL | <60 mL/min (n = 849) 37.1% ≥60 mL/min (n = 1198) 52.3% | Patients with eGFR <60 mL/min had a markedly higher mortality rate than patients with less compromised renal function; however, they benefited to the same extent from bisoprolol treatment. |
| COPERNICUS; 2001; Eric J Eichhorn et al. | 2289 | Carvedilol vs. Pl. | LVEF ≤ 25%; NYHA IV | ACM | 0.9 | Creatinine > 2.8 mg/dL | ≤60 (n = 2566) 61% >60 (n = 1651) 39% Data to be referred to both the COPERNICUS and CAPRICORN studies considered together | Among the CKD group, treatment with carvedilol was associated with decreased risks of ACM, CV mortality, HF mortality, first HFH. Treatment with carvedilol did not have a statistically significant impact on sudden cardiac death in HF patients with CKD. |
| CAPRICORN; 2005; McMurray et al. | 1959 | Carvedilol vs. Pl. | CHF LVEF ≤ 35% | ACM | 1.3 | Renal Impairment | ≤60 (n = 2566) 61% >60 (n = 1651) 39% Data to be referred to both the COPERNICUS and CAPRICORN studies Considered together. | See Copernicus results above. |
| COMET; 2003; Pool Wilson et al. | 3029 | Carvedilol vs. Metoprolol | LVEF ≤ 35%; NYHA II to IV; ACE inhibitor therapy for at least 4 weeks; Diuretic therapy for at least 2 weeks. Prior hospitalization for CV reasons at least once in the year preceding inclusion. | ACM | 4.8 | NA | NA | Carvedilol improved vascular outcomes better than metoprolol. |
| SENIORS; 2005; Flather et al. | 2128 | Nebivolol vs. Placebo | Age ≥ 70 y, HF confirmed as HF hospitalization in recent 12 months and/or LVEF ≤ 35% in recent 6 months | ACM or CV hospitalization | 1.8 | Significant renal disease | <55.5 (n = 704) 33% 55.5–72.8 (n = 704) 33% >72.8 (n = 704) 33% | SENIORS was not powered to detect reductions in the primary outcome for the renal sub-groups and hence none of the eGFR tertiles reached statistical significance. Nebivolol was safe for use in those with renal dysfunction, albeit with a marginal increase in bradycardia-related treatment discontinuation. |
| Trial; Author; Year | Pts (n) | Design | Main Eligibility Criteria | Primary Outcome | Mean Follow up (years) | Renal Function Exclusion | CKD Groups (eGFR, mL/min/ 1.73 m2) | Main Findings |
|---|---|---|---|---|---|---|---|---|
| Sodium Glucose Linked Transporter 2 Inhibitors | ||||||||
| DAPA-HF; 2019; Mc Murray et al. [45] | 4744 | Dapaglifozin vs. Pl. | LVEF ≤ 40%; NYHA III–V; eGFR ≥ 30 mL/min/1.73 m2 | WHF or CV death | 1.5 | eGFR < 30 mL/min/1.73 m² | <60 (n = 1926) 41% ≥60 (n = 2816) 59, 35% | The effect of dapagliflozin on the primary and secondary outcomes did not differ by eGFR category or examining eGFR as a continuous variable. |
| EMPEROR reduced; 2020; Packer et al.; | 3730 | Empaglifozin vs. Pl. | LVEF ≤ 40%; NYHA IIIV; eGFR ≥ 20 mL/min/1.73 m2 | WHF or CV death | 1.3 | eGFR < 20 mL/min/1.73 m² | <60 (n = 1978) 53, 2% ≥60 (n = 1746) 46.8% | Empagliflozin reduced the primary outcome and total HF hospitalizations in patients with and without CKD. |
| SOLOIST-WHF; 2021; Bhatt et al. | 1222 | Sotaglifozin vs. Pl. | 18–85 years old; symptoms or sign of HF; type II diabetes; recent hospitalization for WHF. | Total WHF and CV death | 0.75 | eGFR < 30 mL/min/1.73 m² | <60 (n = 854) 69.9% ≥60 (n = 368) 30.1% | Sotaglifozin therapy resulted in lower total number of deaths from CV causes and hospitalizations or urgent visits for HF than placebo even in patients with CKD across the full range of proteinuria. |
| Angiotensin Receptor Neprylisin Inhibitors | ||||||||
| PARADIGM-HF; 2014; Solomon et al. | 8442 | Enalapril vs. Sac/Val | LVEF ≤ 40%; NYHA III–V; eGFR ≥ 30 mL/min/1.73 m2 | CV death or HFH | 2.25 | eGFR ≤ 30 mL/min/1.73 m² | <60 (n = 3061) 36.2% ≥60 (n = 5338) 63.2% | Compared with enalapril, sacubitril and valsartan led to a slower rate of decrease in the eGFR and improved CV outcomes, even in patients with CKD. |
| PARAGON-HF; 2019; Solomon et al. | 4822 | Sac/Val vs. Valsartan | LVEF ≥ 45%; NYHA III–V; eGFR ≥ 30 mL/min/1.73 m2 | CV death or HFH | 2.92 | eGFR ≤ 30 mL/min/1.73 m² | <60 (n = 2341) 48.5% ≥60 (n = 2454) 50.9% | Sacubitril–valsartan did not result in a significantly lower rate of total HFH and death from CV causes both in patients with CKD and without CKD. |
| Agents Considered in Selected HFrEF Patients | ||||||||
| SHIFT; 2012; Bohrer et al. | 6558 | Ivabradine vs. Pl. | LVEF < 35%; synus rhythm; Heart rate > 70 bpm | CV Death or HFH | 1.9 | Sever renal disease | <60 (n = 1579) 24.07% ≥60 (n = 4581) 69.85% | Ivabradine significantly reduced the combined primary end point of CV mortality or HFH compared with pl. The incidence of the primary end point was similar in both patients with (CKD stages 3–5) and without CKD. |
| VICTORIA; 2020; Armstrong et al. | 5050 | Vericiguat vs. Pl. | LVEF < 45%; NYHA III–V; recent hospitalization; eGFR 15 ≥ mL/min/1.73 m2 (no more than 15% of subjects with an eGFR in the 15 L/min/1.73 m2 to 30 mL/min/1.73 m2 range). | CV Death or HFH | 0.8 | eGFR < 15 mL/min/1.73 m² | ≤30 (n = 506) 10% >30 ≤60 (n = 2118) 41.94% >60 (n = 2335) 46.23% | Vericiguat reduced the primary composite endpoint of CV death or HFH across all eGFR spectrum. the beneficial effects of vericiguat were similar in patients with and without WRF. |
| GALACTIC-HF; 2021; Teerlink et al. | 8256 | Omecamtiv /Mecarbil vs. Pl. | LVEF ≤ 35%; symptomatic chronic HF | CV Death or HFH/WHF | 1.8 | eGFR < 15 mL/min/1.73 m² | NA | Lower incidence of HF event or death from CV causes in the omecamtiv mecarbil arm compared with placebo. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beltrami, M.; Milli, M.; Dei, L.L.; Palazzuoli, A. The Treatment of Heart Failure in Patients with Chronic Kidney Disease: Doubts and New Developments from the Last ESC Guidelines. J. Clin. Med. 2022, 11, 2243. https://doi.org/10.3390/jcm11082243
Beltrami M, Milli M, Dei LL, Palazzuoli A. The Treatment of Heart Failure in Patients with Chronic Kidney Disease: Doubts and New Developments from the Last ESC Guidelines. Journal of Clinical Medicine. 2022; 11(8):2243. https://doi.org/10.3390/jcm11082243
Chicago/Turabian StyleBeltrami, Matteo, Massimo Milli, Lorenzo Lupo Dei, and Alberto Palazzuoli. 2022. "The Treatment of Heart Failure in Patients with Chronic Kidney Disease: Doubts and New Developments from the Last ESC Guidelines" Journal of Clinical Medicine 11, no. 8: 2243. https://doi.org/10.3390/jcm11082243
APA StyleBeltrami, M., Milli, M., Dei, L. L., & Palazzuoli, A. (2022). The Treatment of Heart Failure in Patients with Chronic Kidney Disease: Doubts and New Developments from the Last ESC Guidelines. Journal of Clinical Medicine, 11(8), 2243. https://doi.org/10.3390/jcm11082243






