Overlooked but Serious Gallbladder Disease during Extracorporeal Membrane Oxygenation: A Retrospective Analysis
Abstract
:1. Introduction
2. Methods
2.1. Study Population
2.2. Statistical Analyses
3. Results
3.1. Incidence and Clinical Features of Symptomatic GB Disease during ECMO Therapy
3.2. Patient Characteristics
3.3. Risk Factors for GB Disease during ECMO Therapy
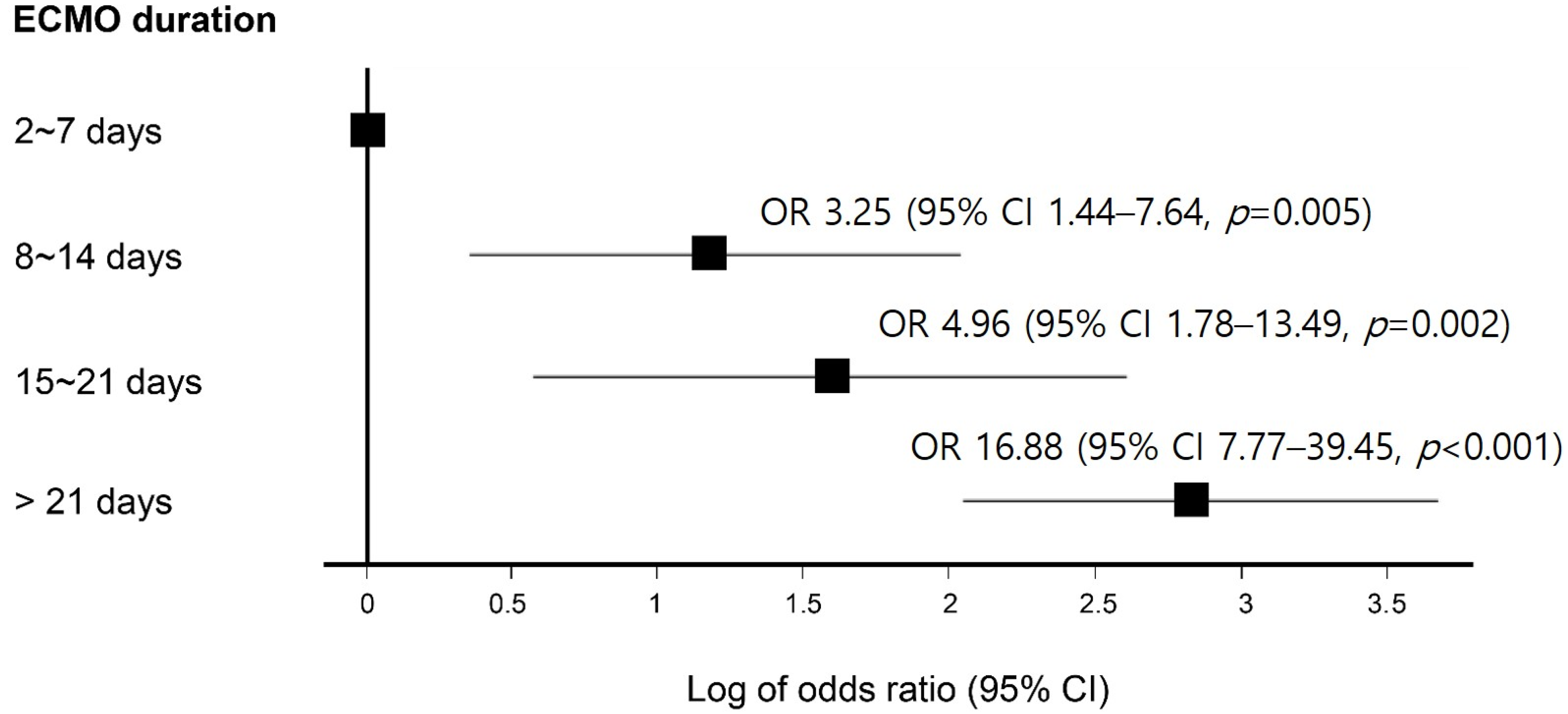
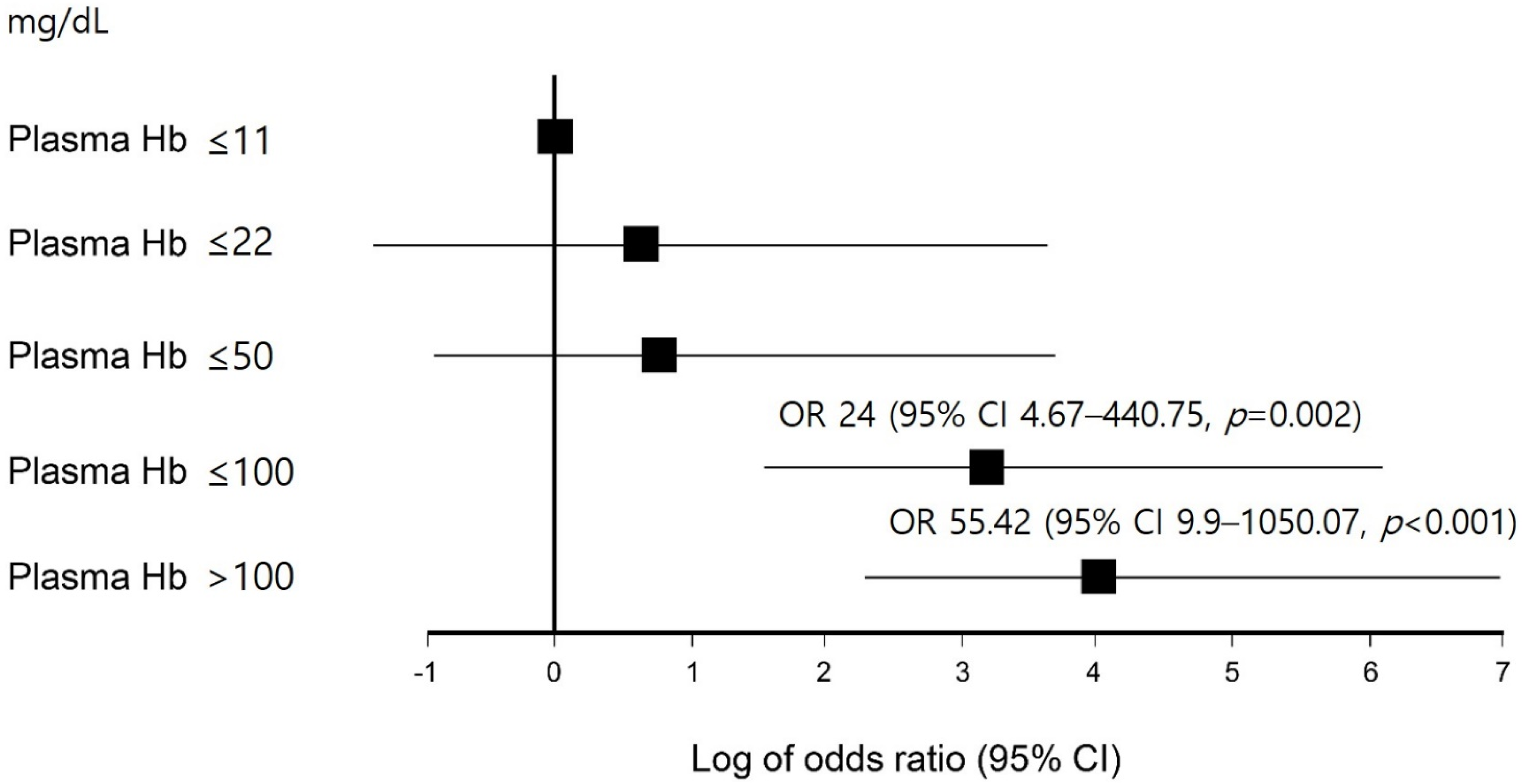
3.4. Impact of GB Disease during ECMO Therapy on Clinical Outcomes
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- MacLaren, G.; Combes, A.; Bartlett, R.H. Contemporary extracorporeal membrane oxygenation for adult respiratory failure: Life support in the new era. Intensive Care Med. 2012, 38, 210–220. [Google Scholar] [CrossRef] [PubMed]
- Makdisi, G.; Wang, I.-W. Extra corporeal membrane oxygenation (ECMO) review of a lifesaving technology. J. Thorac. Dis. 2015, 7, E166. [Google Scholar] [PubMed]
- Kim, D.H.; Cho, W.H.; Son, J.; Lee, S.K.; Yeo, H.J. Catastrophic mechanical complications of extracorporeal membrane oxygenation. ASAIO J. 2021, 67, 1000–1005. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.; Cho, W.H.; Kim, D.; Jeon, D.; Kim, Y.S.; Yeo, H.J. Microbial Colonization of Oxygenator and Clinical Outcomes in Extracorporeal Membrane Oxygenation. ASAIO J. 2021, 67, 930–934. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Kim, Y.H.; Cho, W.H.; Son, B.S.; Yeo, H.J. Biofilm microbiome in extracorporeal membrane oxygenator catheters. PLoS ONE 2021, 16, e0257449. [Google Scholar] [CrossRef] [PubMed]
- Yeo, H.J.; Kim, D.H.; Jeon, D.; Kim, Y.S.; Cho, W.H. Low-dose heparin during extracorporeal membrane oxygenation treatment in adults. Intensive Care Med. 2015, 41, 2020. [Google Scholar] [CrossRef]
- Boland, G.; Lee, M.; Mueller, P. Acute cholecystitis in the intensive care unit. New Horiz. (Baltim. Md.) 1993, 1, 246–260. [Google Scholar]
- Laurila, J.; Syrjälä, H.; Laurila, P.A.; Saarnio, J.; Ala-Kokko, T.I. Acute acalculous cholecystitis in critically ill patients. Acta Anaesthesiol. Scand. 2004, 48, 986–991. [Google Scholar] [CrossRef]
- Kim, S.J.; Lee, S.J.; Lee, S.H.; Lee, J.H.; Chang, J.H.; Ryu, Y.J. Clinical characteristics of patients with newly developed acute cholecystitis after admission to the intensive care unit. Aust. Crit. Care 2019, 32, 223–228. [Google Scholar] [CrossRef]
- Hazem, Z.M. Acute biliary pancreatitis: Diagnosis and treatment. Saudi J. Gastroenterol. Off. J. Saudi Gastroenterol. Assoc. 2009, 15, 147. [Google Scholar] [CrossRef]
- Kimura, Y.; Takada, T.; Kawarada, Y.; Nimura, Y.; Hirata, K.; Sekimoto, M.; Yoshida, M.; Mayumi, T.; Wada, K.; Miura, F.; et al. Definitions, pathophysiology, and epidemiology of acute cholangitis and cholecystitis: Tokyo Guidelines. J. Hepato-Biliary-Pancreat. Surg. 2007, 14, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Molenat, F.; Boussuges, A.; Valantin, V.; Sainty, J.M. Gallbladder abnormalities in medical ICU patients: An ultrasonographic study. Intensive Care Med. 1996, 22, 356–358. [Google Scholar] [CrossRef] [PubMed]
- Raunest, J.; Imhof, M.; Rauen, U.; Ohmann, C.; Thon, K.P.; Bürrig, K.F. Acute cholecystitis: A complication in severely injured intensive care patients. J. Trauma 1992, 32, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Theodorou, P.; Maurer, C.A.; Spanholtz, T.A.; Phan, T.Q.; Amini, P.; Perbix, W.; Maegele, M.; Lefering, R.; Spilker, G. Acalculous cholecystitis in severely burned patients: Incidence and predisposing factors. Burns 2009, 35, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Huffman, J.L.; Schenker, S. Acute acalculous cholecystitis: A review. Clin. Gastroenterol. Hepatol. 2010, 8, 15–22. [Google Scholar] [CrossRef]
- Ganpathi, I.S.; Diddapur, R.K.; Eugene, H.; Karim, M. Acute acalculous cholecystitis: Challenging the myths. Hpb 2007, 9, 131–134. [Google Scholar] [CrossRef]
- Warren, B. Small vessel occlusion in acute acalculous cholecystitis. Surgery 1992, 111, 163–168. [Google Scholar]
- Hakala, T.; Nuutinen, P.; Ruokonen, E.; Alhava, E. Microangiopathy in acute acalculous cholecystitis. J. Br. Surg. 1997, 84, 1249–1252. [Google Scholar]
- Barie, P.S.; Eachempati, S.R. Acute acalculous cholecystitis. Gastroenterol. Clin. 2010, 39, 343–357. [Google Scholar] [CrossRef]
- Lehle, K.; Philipp, A.; Zeman, F.; Lunz, D.; Lubnow, M.; Wendel, H.P.; Göbölös, L.; Schmid, C.; Müller, T. Technical-induced hemolysis in patients with respiratory failure supported with veno-venous ECMO–prevalence and risk factors. PLoS ONE 2015, 10, e0143527. [Google Scholar] [CrossRef]
- Appelt, H.; Philipp, A.; Mueller, T.; Foltan, M.; Lubnow, M.; Lunz, D.; Zeman, F.; Lehle, K. Factors associated with hemolysis during extracorporeal membrane oxygenation (ECMO)—Comparison of VA-versus VV ECMO. PLoS ONE 2020, 15, e0227793. [Google Scholar] [CrossRef] [PubMed]
- Zangrillo, A.; Landoni, G.; Biondi-Zoccai, G.; Greco, M.; Greco, T.; Frati, G.; Patroniti, N.; Antonelli, M.; Pesenti, A.; Pappalardo, F. A meta-analysis of complications and mortality of extracorporeal membrane oxygenation. Crit. Care Resusc. 2013, 15, 172–178. [Google Scholar] [PubMed]
- Murphy, D.A.; Hockings, L.E.; Andrews, R.K.; Aubron, C.; Gardiner, E.E.; Pellegrino, V.A.; Davis, A.K. Extracorporeal membrane oxygenation—hemostatic complications. Transfus. Med. Rev. 2015, 29, 90–101. [Google Scholar] [CrossRef] [PubMed]
- Almond, P.S.; Adolph, V.R.; Steiner, R.; Hill, C.B.; Falterman, K.W.; Arensman, R.M. Calculous disease of the biliary tract in infants after neonatal extracorporeal membrane oxygenation. J. Perinatol. 1992, 12, 18–20. [Google Scholar] [PubMed]
- Shneider, B.; Cronin, J.; Van Marter, L.; Maller, E.; Truog, R.; Jacobson, M.; Kevy, S. A prospective analysis of cholestasis in infants supported with extracorporeal membrane oxygenation. J. Pediatr. Gastroenterol. Nutr. 1991, 13, 285–289. [Google Scholar] [CrossRef]
- Akbar, A.; Baron, T.H. Ischemic biliary injury following extra-corporeal membrane oxygenation (ECMO). Dig. Liver Dis. 2012, 44, 705. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, U.Y.; Jassim, H.M.; Baig, A.A.; Khorsheed, R.M.; Al-Khayat, A.M.; Sulong, A.F.; Abed, N.F.; Yassin, W.A. Gallstones in patients with inherited hemolytic diseases. Int. J. Pharm. Pharm. Sci. 2015, 7, 9–15. [Google Scholar]
- Trowbridge, R.L.; Rutkowski, N.K.; Shojania, K.G. Does this patient have acute cholecystitis? JAMA 2003, 289, 80–86. [Google Scholar] [CrossRef]
- Tazuma, S. Epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic). Best Pract. Res. Clin. Gastroenterol. 2006, 20, 1075–1083. [Google Scholar] [CrossRef]
- Lammert, F.; Gurusamy, K.; Ko, C.W.; Miquel, J.F.; Méndez-Sánchez, N.; Portincasa, P.; Van Erpecum, K.J.; Van Laarhoven, C.J.; Wang, D.Q. Gallstones. Nat. Rev. Dis. Primers 2016, 2, 1–17. [Google Scholar] [CrossRef]
- Barie, P.S.; Fischer, E. Acute acalculous cholecystitis. J. Am. Coll. Surg. 1995, 180, 232–244. [Google Scholar]
- Ambe, P.; Weber, S.A.; Christ, H.; Wassenberg, D. Cholecystectomy for acute cholecystitis. How time-critical are the so called “golden 72 hours”? Or better “golden 24 hours” and “silver 25–72 hour”? A case control study. World J. Emerg. Surg. 2014, 9, 60. [Google Scholar] [CrossRef] [PubMed]
- Gutt, C.N.; Encke, J.; Köninger, J.; Harnoss, J.C.; Weigand, K.; Kipfmüller, K.; Schunter, O.; Götze, T.; Golling, M.T.; Menges, M.; et al. Acute cholecystitis: Early versus delayed cholecystectomy, a multicenter randomized trial (ACDC study, NCT00447304). Ann. Surg. 2013, 258, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Kiriyama, S.; Takada, T.; Strasberg, S.M.; Solomkin, J.S.; Mayumi, T.; Pitt, H.A.; Gouma, D.J.; Garden, O.J.; Büchler, M.W.; Yokoe, M.; et al. TG13 guidelines for diagnosis and severity grading of acute cholangitis (with videos). J. Hepato-Biliary-Pancreat. Sci. 2013, 20, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Everhart, J.E.; Khare, M.; Hill, M.; Maurer, K.R. Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology 1999, 117, 632–639. [Google Scholar] [CrossRef]

| Variables | G Group (n = 62) | N Group (n = 384) | p |
|---|---|---|---|
| Age (years) | 62 (54.8–69.3) | 57 (47.3–66) | 0.006 |
| Elderly | 27 (43.5) | 104 (27.1) | 0.008 |
| Male | 39 (62.9) | 228 (59.4) | 0.599 |
| BMI (kg/m2) | 22.5 (19.9–25.1) | 23.0 (20.8–25.6) | 0.300 |
| APACHE II | 11.5 (9–16.3) | 13 (9–17) | 0.601 |
| SOFA score | 12 (9–13) | 11 (8–13) | 0.256 |
| Vasopressor | 43 (69.4) | 283 (73.7) | 0.474 |
| CRRT | 36 (58.1) | 184 (47.9) | 0.138 |
| Indication of ECMO | 0.965 | ||
| Respiratory | 34 (54.8) | 209 (54.4) | |
| Cardiac | 19 (30.6) | 123 (32.0) | |
| E-CPR | 9(14.5) | 52 (13.5) | |
| ECMO mode | 0.502 | ||
| VV | 34 (54.8) | 180 (46.9) | |
| VA | 25 (40.3) | 180 (46.9) | |
| VVA | 0 | 7(1.8) | |
| other | 3(4.8) | 17 (4.4) | |
| Mechanical ventilator | 62 (100) | 374 (97.4) | 0.199 |
| Risk factors of GB disease | |||
| Diuretics | 54 (87.1) | 304 (79.2) | 0.145 |
| LC | 7 (11.3) | 26 (6.8) | 0.207 |
| TPN | 40 (64.5) | 182 (47.4) | 0.012 |
| Duration of TPN (days) | 3 (0–9.3) | 0 (0–4) | 0.001 |
| Fasting | 56 (90.3) | 350 (91.1) | 0.833 |
| Duration of fasting (days) | 3.5 (2–6.3) | 3 (1–5) | 0.055 |
| Total bilirubin before ECMO | 0.6 (0.4–1.3) | 0.6 (0.3–1.1) | 0.476 |
| Univariate | Multivariate | |||
|---|---|---|---|---|
| Variables | HR (95% CI) | p | HR (95% CI) | p |
| Long-term ECMO | 3.34 (1.91–5.82) | <0.001 | 2.95 (1.69–5.15) | <0.001 |
| Plasma Hb > 50 mg/dL | 2.43 (1.39–4.25) | 0.002 | 2.12 (1.18–3.78) | 0.012 |
| NPO > 7 days | 2.75 (1.53–4.96) | 0.001 | ||
| Variables | G Group (n = 62) | N Group (n = 124) | p |
|---|---|---|---|
| Age (years) | 62 (54.8–69.3) | 59 (50–67) | 0.120 |
| Elderly | 27 (43.5) | 41 (33.1) | 0.162 |
| Male | 39 (62.9) | 75 (60.5) | 0.749 |
| BMI (kg/m2) | 22.5 (19.9–25.1) | 22.2 (19.8–25.8) | 1.000 |
| APACHE II | 11.5 (9–16.3) | 12 (9–17) | 0.756 |
| SOFA score | 12 (9–13) | 12 (9–15.8) | 0.832 |
| Vasopressor | 43 (69.4) | 94 (75.8) | 0.346 |
| CRRT | 36 (58.1) | 68 (54.8) | 0.676 |
| Indication of ECMO | 0.391 | ||
| Respiratory | 34 (54.8) | 73 (58.9) | |
| Cardiac | 19 (30.6) | 41 (33.1) | |
| E-CPR | 9 (14.5) | 10 (8.1) | |
| ECMO mode | 0.460 | ||
| VV | 34 (54.8) | 59 (47.6) | |
| VA | 25 (40.3) | 54 (43.5) | |
| VVA | 0 | 4 (3.2) | |
| other | 3 (4.8) | 7 (5.6) | |
| Mechanical ventilator | 62 (100) | 124 (100) | |
| Risk factors of GB disease | |||
| Diuretics | 54 (87.1) | 102 (82.3) | 0.398 |
| LC | 7 (11.3) | 10 (8.1) | 0.472 |
| TPN | 40 (64.5) | 68 (54.8) | 0.207 |
| Duration of TPN (days) | 3 (0–9.3) | 2 (0–6.8) | 0.464 |
| Fasting | 56 (90.3) | 116 (93.5) | 0.432 |
| Duration of fasting (days) | 3.5 (2–6.3) | 3.5 (1–7) | 1.000 |
| Total bilirubin before ECMO | 0.6 (0.4–1.3) | 0.7 (0.3–1.6) | 0.836 |
| Variables | G Group (n = 62) | N Group (n = 124) | p |
|---|---|---|---|
| Duration of ECMO, days | 7 (4–16.3) | 8 (4–14) | 0.835 |
| Long-term ECMO (≥2 weeks) | 19 (30.6) | 32 (25.8) | 0.486 |
| Duration of mechanical ventilation, days | 29.5 (11.6–51.2) | 17.0 (7.2–35.8) | 0.013 |
| Length of ICU stay, days | 32.1 (17–52) | 23.5 (11–43.7) | 0.120 |
| ICU survival | 40 (64.5) | 105 (84.7) | 0.002 |
| Survival discharge | 37 (59.7) | 101 (81.5) | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.Y.; Jang, J.W.; Kim, H.-J.; Cho, W.H.; Ha, M.; Son, B.S.; Yeo, H.J. Overlooked but Serious Gallbladder Disease during Extracorporeal Membrane Oxygenation: A Retrospective Analysis. J. Clin. Med. 2022, 11, 2199. https://doi.org/10.3390/jcm11082199
Kim HY, Jang JW, Kim H-J, Cho WH, Ha M, Son BS, Yeo HJ. Overlooked but Serious Gallbladder Disease during Extracorporeal Membrane Oxygenation: A Retrospective Analysis. Journal of Clinical Medicine. 2022; 11(8):2199. https://doi.org/10.3390/jcm11082199
Chicago/Turabian StyleKim, Hee Young, Jin Wook Jang, Hye-Jin Kim, Woo Hyun Cho, Mihyang Ha, Bong Soo Son, and Hye Ju Yeo. 2022. "Overlooked but Serious Gallbladder Disease during Extracorporeal Membrane Oxygenation: A Retrospective Analysis" Journal of Clinical Medicine 11, no. 8: 2199. https://doi.org/10.3390/jcm11082199
APA StyleKim, H. Y., Jang, J. W., Kim, H.-J., Cho, W. H., Ha, M., Son, B. S., & Yeo, H. J. (2022). Overlooked but Serious Gallbladder Disease during Extracorporeal Membrane Oxygenation: A Retrospective Analysis. Journal of Clinical Medicine, 11(8), 2199. https://doi.org/10.3390/jcm11082199





