Total Hysterectomy by Low-Impact Laparoscopy to Decrease Opioids Consumption: A Prospective Cohort Study
Abstract
:1. Introduction
2. Methods
2.1. Population
2.2. Surgical Details
2.3. Anesthesia Protocol
2.4. Outcome Measures
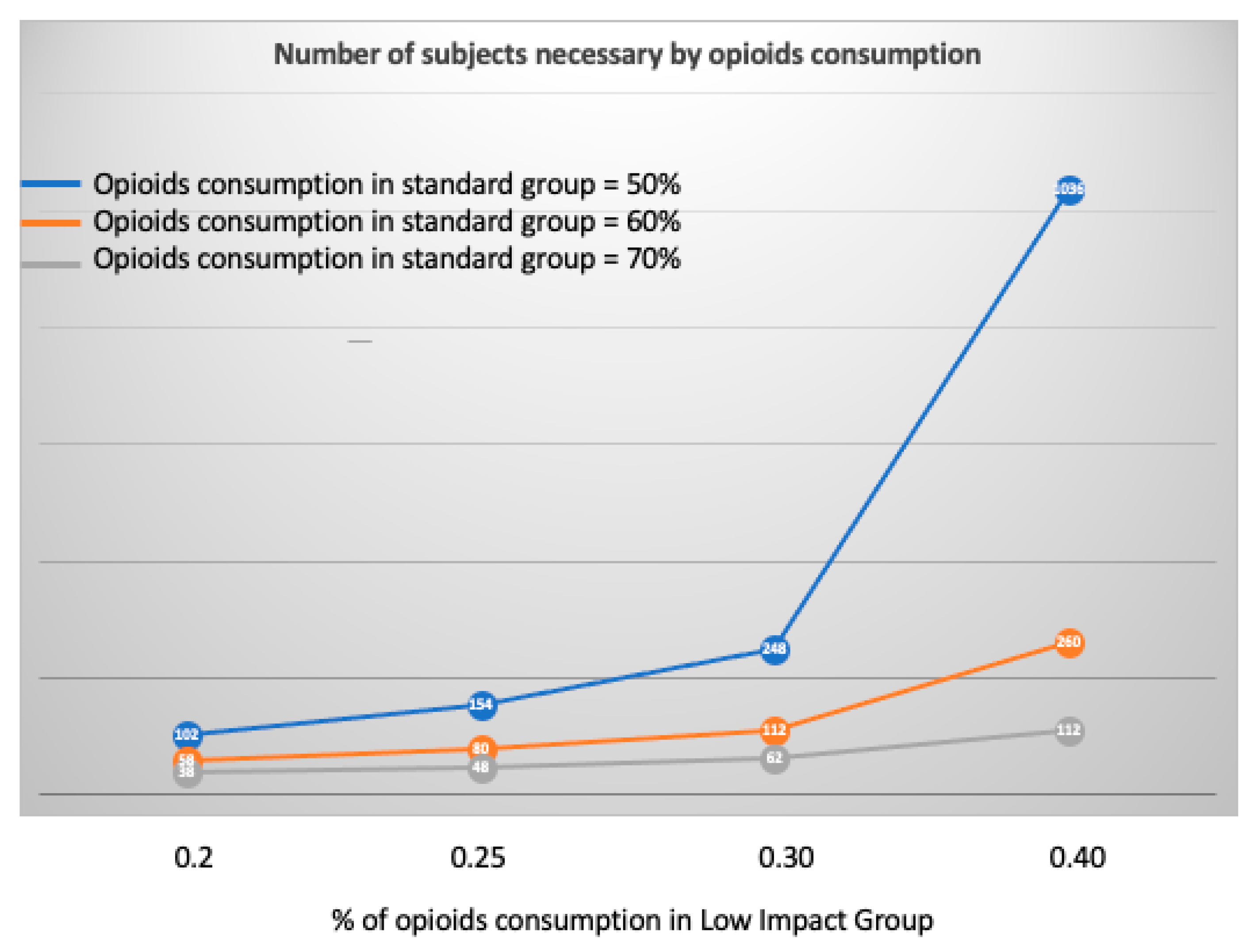
2.5. Statistical Analysis
3. Results
3.1. Clinical Characteristics and Surgical Parameters
3.2. Postoperative Pain and Opioid Consumption
3.3. Factors Associated with Postoperative Opioid Consumption
4. Discussion
4.1. Main Findings
4.2. Interpretation
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Madhvani, K.; Curnow, T.; Carpenter, T. Route of hysterectomy: A retrospective, cohort study in English NHS hospitals from 2011 to 2017. BJOG Int. J. Obstet. Gynaecol. 2019, 126, 795–802. [Google Scholar] [CrossRef] [PubMed]
- Moawad, G.; Liu, E.; Song, C.; Fu, A.Z. Movement to outpatient hysterectomy for benign indications in the United States, 2008–2014. PLoS ONE 2017, 12, e0188812. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luchristt, D.; Brown, O.; Kenton, K.; Bretschneider, C.E. Trends in operative time and outcomes in minimally invasive hysterectomy from 2008 to 2018. Am. J. Obstet. Gynecol. 2021, 224, 202.e1–202.e12. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, N.Z.; Byrnes, G.; Naqvi, S.A. A meta-analysis of ambulatory versus inpatient laparoscopic cholecystectomy. Surg. Endosc. 2008, 22, 1928–1934. [Google Scholar] [CrossRef] [PubMed]
- Crawford, D.C.; Li, C.S.; Sprague, S.; Bhandari, M. Clinical and cost implications of inpatient versus outpatient orthopedic surgeries: A systematic review of the published literature. Orthop. Rev. 2015, 7, 6177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, D.J.; Forner, D.; End, C.; Yao, C.M.K.L.; Samargandy, S.; Monteiro, E.; Witterick, I.J.; Freeman, J.L. Outpatient versus inpatient superficial parotidectomy: Clinical and pathological characteristics. J. Otolaryngol.-Head Neck Surg. J. Oto-Rhino-Laryngol. Chir. Cervico-Faciale 2021, 50, 10. [Google Scholar] [CrossRef] [PubMed]
- Clarke, H.; Soneji, N.; Ko, D.T.; Yun, L.; Wijeysundera, D.N. Rates and risk factors for prolonged opioid use after major surgery: Population based cohort study. BMJ 2014, 348, g1251. [Google Scholar] [CrossRef] [Green Version]
- Brummett, C.M.; Waljee, J.F.; Goesling, J.; Moser, S.; Lin, P.; Englesbe, M.J.; Bohnert, A.S.B.; Kheterpal, S.; Nallamothu, B.K. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017, 152, e170504. [Google Scholar] [CrossRef]
- Reich, H.; DeCAPRIO, J.; McGLYNN, F. Laparoscopic hysterectomy. J. Gynecol. Surg. 1989, 5, 213–216. [Google Scholar] [CrossRef] [Green Version]
- de’Angelis, N.; Petrucciani, N.; Giannandrea, G.; Brunetti, F. The protocol of low-impact laparoscopic cholecystectomy: The combination of mini-laparoscopy and low-pressure pneumoperitoneum. Updat. Surg. 2018, 70, 553–556. [Google Scholar] [CrossRef]
- Hua, J.; Gong, J.; Yao, L.; Zhou, B.; Song, Z. Low-pressure versus standard-pressure pneumoperitoneum for laparoscopic cholecystectomy: A systematic review and meta-analysis. Am. J. Surg. 2014, 208, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Sroussi, J.; Elies, A.; Rigouzzo, A.; Louvet, N.; Mezzadri, M.; Fazel, A.; Benifla, J.-L. Low pressure gynecological laparoscopy (7mmHg) with AirSeal® System versus a standard insufflation (15mmHg): A pilot study in 60 patients. J. Gynecol. Obstet. Hum. Reprod. 2017, 46, 155–158. [Google Scholar] [CrossRef] [PubMed]
- Luketina, R.R.; Knauer, M.; Köhler, G.; Koch, O.O.; Strasser, K.; Egger, M.; Emmanuel, K. Comparison of a standard CO₂ pressure pneumoperitoneum insufflator versus AirSeal: Study protocol of a randomized controlled trial. Trials 2014, 15, 239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horstmann, M.; Horton, K.; Kurz, M.; Padevit, C.; John, H. Prospective comparison between the AirSeal® System valve-less Trocar and a standard VersaportTM Plus V2 Trocar in robotic-assisted radical prostatectomy. J. Endourol. 2013, 27, 579–582. [Google Scholar] [CrossRef] [PubMed]
- Hjermstad, M.J.; Fayers, P.M.; Haugen, D.F.; Caraceni, A.; Hanks, G.W.; Loge, J.H.; Fainsinger, R.; Aass, N.; Kaasa, S.; European Palliative Care Research Collaborative (EPCRC). Studies comparing numerical rating scales, verbal rating scales, and visual analogue scales for assessment of pain intensity in adults: A systematic literature review. J. Pain Symptom Manage. 2011, 41, 1073–1093. [Google Scholar] [CrossRef]
- Ferreira-Valente, M.A.; Pais-Ribeiro, J.L.; Jensen, M.P. Validity of four pain intensity rating scales. Pain 2011, 152, 2399–2404. [Google Scholar] [CrossRef]
- Breivik, E.K.; Björnsson, G.A.; Skovlund, E. A Comparison of pain rating scales by sampling from clinical trial data. Clin. J. Pain 2000, 16, 22–28. [Google Scholar] [CrossRef]
- Thong, I.S.K.; Jensen, M.P.; Miró, J.; Tan, G. The validity of pain intensity measures: What do the NRS, VAS, VRS, and FPS-R measure? Scand. J. Pain 2018, 18, 99–107. [Google Scholar] [CrossRef]
- Bijen, C.B.M.; Vermeulen, K.M.; Mourits, M.J.E.; de Bock, G.H. Costs and effects of abdominal versus laparoscopic hysterectomy: Systematic review of controlled trials. PLoS ONE 2009, 4, e7340. [Google Scholar] [CrossRef] [Green Version]
- Walker, J.L.; Piedmonte, M.R.; Spirtos, N.M.; Eisenkop, S.M.; Schlaerth, J.B.; Mannel, R.S.; Spiegel, G.; Barakat, R.; Pearl, M.L.; Sharma, S.K. Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic oncology group study LAP2. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2009, 27, 5331–5336. [Google Scholar] [CrossRef]
- Desai, V.B.; Xu, X. An update on inpatient hysterectomy routes in the United States. Am. J. Obstet. Gynecol. 2015, 213, 742–743. [Google Scholar] [CrossRef] [PubMed]
- Tyan, P.; Klebanoff, J.S.; Frangieh, M.; North, A.; Smith, S.; Amdur, R.; Kazma, J.; Moawad, G.N. Safety and feasibility of the three-port robot-assisted hysterectomy across uterine weights. J. Robot. Surg. 2021, 15, 259–264. [Google Scholar] [CrossRef]
- Casarin, J.; Cimmino, C.; Artuso, V.; Cromi, A.; Ghezzi, F. Minilaparoscopy in gynecology: Applications, benefits and limitations. Minerva Ginecol. 2021, 73, 179–184. [Google Scholar] [CrossRef] [PubMed]
- West-Sussex-Drug-Related-Deaths-Audit-2019.Pdf. Available online: https://jsna.westsussex.gov.uk/updates/drug-related-deaths-audit-2019/ (accessed on 1 March 2022).
- Hinther, A.; Abdel-Rahman, O.; Cheung, W.Y.; Quan, M.L.; Dort, J.C. Chronic postoperative opioid use: A systematic review. World J. Surg. 2019, 43, 2164–2174. [Google Scholar] [CrossRef] [PubMed]
- Neuman, M.D.; Bateman, B.T.; Wunsch, H. Inappropriate opioid prescription after surgery. Lancet Lond. Engl. 2019, 393, 1547–1557. [Google Scholar] [CrossRef]
- Feinberg, A.E.; Chesney, T.R.; Srikandarajah, S.; Acuna, S.A.; McLeod, R.S.; Best Practice in Surgery Group. Opioid use after discharge in postoperative patients: A systematic review. Ann. Surg. 2018, 267, 1056–1062. [Google Scholar] [CrossRef] [PubMed]
- Blanton, E.; Lamvu, G.; Patanwala, I.; Barron, K.I.; Witzeman, K.; Tu, F.F.; As-Sanie, S. Non-opioid pain management in benign minimally invasive hysterectomy: A systematic review. Am. J. Obstet. Gynecol. 2017, 216, 557–567. [Google Scholar] [CrossRef]
- Ng, Y.W.; Lim, L.M.; Fong, Y.F. Minilaparoscopic hysterectomy made easy: First report on alternative instrumentation and new integrated energy platform. J. Obstet. Gynaecol. Res. 2014, 40, 1436–1440. [Google Scholar] [CrossRef]
- Uccella, S.; Cromi, A.; Casarin, J.; Bogani, G.; Serati, M.; Gisone, B.; Pinelli, C.; Fasola, M.; Ghezzi, F. Minilaparoscopic versus standard laparoscopic hysterectomy for uteri ≥16 weeks of gestation: Surgical outcomes, postoperative quality of life, and cosmesis. J. Laparoendosc. Adv. Surg. Tech. A 2015, 25, 386–391. [Google Scholar] [CrossRef]
- Hypólito, O.H.M.; Azevedo, J.L.M.C.; de Lima Alvarenga Caldeira, F.M.S.; de Azevedo, O.C.; Miyahira, S.A.; Miguel, G.P.S.; Becker, O.M.; Machado, A.C.C.G.; Nunes Filho, G.P.; Azevedo, G.C. Creation of pneumoperitoneum: Noninvasive monitoring of clinical effects of elevated intraperitoneal pressure for the insertion of the first trocar. Surg. Endosc. 2010, 24, 1663–1669. [Google Scholar] [CrossRef]
- Neudecker, J.; Sauerland, S.; Neugebauer, E.; Bergamaschi, R.; Bonjer, H.J.; Cuschieri, A.; Fuchs, K.-H.; Jacobi, C.; Jansen, F.W.; Koivusalo, A.-M.; et al. The European Association for Endoscopic Surgery clinical practice guideline on the pneumoperitoneum for laparoscopic surgery. Surg. Endosc. 2002, 16, 1121–1143. [Google Scholar] [CrossRef] [PubMed]
- Esmat, M.E.; Elsebae, M.M.A.; Nasr, M.M.A.; Elsebaie, S.B. Combined low pressure pneumoperitoneum and intraperitoneal infusion of normal saline for reducing shoulder tip pain following laparoscopic cholecystectomy. World J. Surg. 2006, 30, 1969–1973. [Google Scholar] [CrossRef] [PubMed]
- Ibraheim, O.A.; Samarkandi, A.H.; Alshehry, H.; Faden, A.; Farouk, E.O. Lactate and acid base changes during laparoscopic cholecystectomy. Middle East J. Anaesthesiol. 2006, 18, 757–768. [Google Scholar] [PubMed]
- Eryılmaz, H.B.; Memiş, D.; Sezer, A.; Inal, M.T. The effects of different insufflation pressures on liver functions assessed with LiMON on patients undergoing laparoscopic cholecystectomy. Sci. World J. 2012, 2012, 172575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schietroma, M.; Carlei, F.; Mownah, A.; Franchi, L.; Mazzotta, C.; Sozio, A.; Amicucci, G. Changes in the blood coagulation, fibrinolysis, and cytokine profile during laparoscopic and open cholecystectomy. Surg. Endosc. 2004, 18, 1090–1096. [Google Scholar] [CrossRef] [PubMed]
| Conventional Laparoscopy N = 77 (%) | Low-Impact Laparoscopy N = 32 (%) | p-Value | |
|---|---|---|---|
| Age, median (sd) | 48.3 (13.0) | 52.9 (12.5) | 0.74 |
| BMI ≥30 | 15 (19.5) | 4 (12.5) | 0.58 |
| Menopausal | 32 (41.6) | 17 (53.1) | 0.30 |
| ASA physical status * | 0.06 | ||
| Class 1 | 29 (37.7) | 20 (62.5) | |
| Class 2 | 42 (54.5) | 11 (34.4) | |
| Class 3 | 6 (7.8) | 1 (3.1) | |
| Comorbidity ** | 24 (31.2) | 8 (25) | 0.65 |
| Increased bleeding risk | 7 (9.1) | 0 | |
| Systemic disease | 3 (3.9) | 3 (9.4) | |
| Diabetes | 5 (6.5) | 0 | |
| Hypertension | 13 (16.9) | 3 (9.4) | |
| Other | 1 (1.3) | 2 (6.3) | |
| Cesarean section | 0.18 | ||
| Category 1 | 14 (18.2) | 2 (6.3) | |
| Category 2 | 9 (11.7) | 6 (18.8) | |
| Category 3 | 1 (1.3) | 0 | |
| History of abdominal surgery | |||
| Laparoscopy | 22 (28.6) | 10 (31.3) | 0.9 |
| Pfannenstiel laparotomy (except cesarean section) | 10 (13.0) | 1 (3.1) | 0.17 |
| Median laparotomy | 7 (9.1) | 2 (6.3) | 1 |
| Variables | Conventional N = 77 (%) | Low Impact N = 32 (%) | p-Value |
|---|---|---|---|
| Indication for surgery | 0.01 | ||
| Endometrial neoplasm | |||
| Endometrial cancer | 12 (15.6) | 10 (31.3) | |
| Atypical endometrial hyperplasia | 2 (2.6) | 4 (12.5) | |
| Other conditions | |||
| Cervical dysplasia | 6 (7.8) | 1 (3.1) | |
| Symptomatic Fibroma | 37 (48.1) | 10 (31.3) | |
| Adenomyosis | 13 (16.9) | 4 (12.5) | |
| Other | 7 (9.1) | 3 (9.4) | |
| Mean intraoperative pressure | <0.001 | ||
| <10 | 18 (23.4) | 28 (87.4) | |
| 10–12 | 59 (76.6) | 2 (6.3) | |
| >12 | 0 | 2 (6.3) | |
| Parietal adherences | 20 (26.0) | 6 (18.8) | 0.57 |
| Pelvic adherences | 17 (22.1) | 8 (25) | 0.93 |
| Deep pelvic endometriosis | 1 (1.3) | 3 (9.4) | 0.08 |
| Associated perioperative surgery * | |||
| Uterosacral ligament resection | 1 (1.3) | 0 | |
| Ureterolysis | 1 (1.3) | 5 (15.6) | <0.001 |
| Parametrial resection | 0 | 1 (3.1) | |
| Omentectomy, appendicectomy | 0 | 2 (6.3) | |
| Median duration of anesthesia in minutes (Q1; Q3) | 193 (167; 210.5) | 174 (147; 206) | 0.03 |
| Median duration of surgery in minutes (Q1; Q3) | 140 (118; 162) | 129 (107; 151) | 0.08 |
| Median duration of pneumoperitoneum in minutes (Q1; Q3) | 121 (98; 144) | 105 (93; 129) | 0.3 |
| Median uterus size in mm (sd) | 65 (22.5) | 63 (21.3) | 0.61 |
| Median weight of the uterus in grammes (sd) | 130 (108) | 107 (136) | 0.37 |
| Conventional Laparoscopy N = 77 (%) | Low-Impact Laparoscopy N = 32 (%) | p-Value | |
|---|---|---|---|
| Median length of stay in PACU in minutes (Q1; Q3) | 136.5 (115; 161.2) | 133 (114; 169) | 0.74 |
| Length of hospitalization (days) | <0.001 | ||
| Outpatient | 1 (1.3) | 29 (90.6) | |
| 24 h | 39 (50.6) | 2 (6.3) | |
| 48 h | 30 (39.0) | 1 (3.1) | |
| >48 h | 7 (9.1) | 0 | |
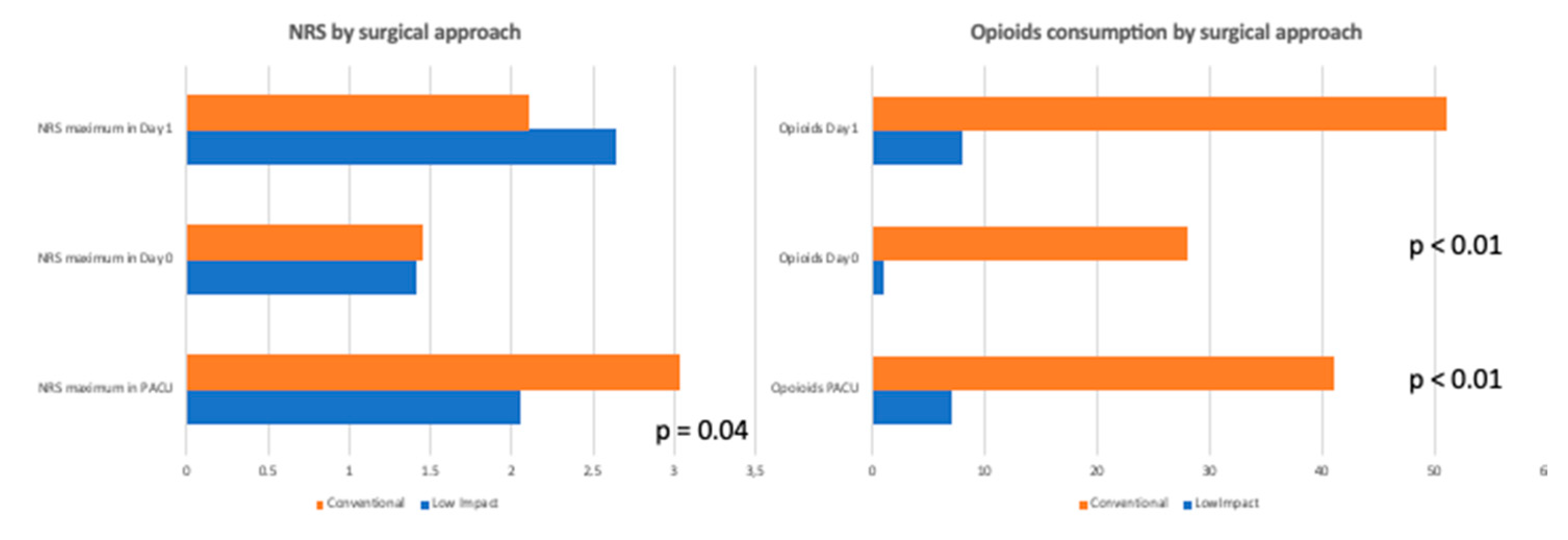
| Postoperative pain | |||
| Maximum in PACU (mean; sd) | 3.04; 2.46 | 2.06; 2.19 | 0.04 |
| Maximum pain on Day 0 (mean; sd) | 1.45; 1.84 | 1.42; 1.69 | 0.92 |
| Maximum pain on Day 1 (mean; sd) | 2.11; 1.95 | 2.64; 2.4 | 0.32 |
| Ropivacaine port infusion | 56 (72.7) | 19 (59.4) | 0.25 |
| Analgesic Consumption | |||
| Paracetamol | |||
| PACU | 22 (28.6) | 9 (28.1) | 0.96 |
| Day 0 | 14 (18.2) | 0 | < 0.001 |
| Day 1 | 17 (22.1) | 2 (6.3) | 0.055 |
| Weak or strong opioid consumption anytime | 49 (63.6) | 10 (31.3) | p < 0.01 |
| Weak opioids (Tramadol) | |||
| PACU | 6 (7.8) | 0 | <0.001 |
| Day 0 | 8 (10.4) | 0 | <0.001 |
| Day 1 | 23 (30.0) | 4 (12.5) | 0.09 |
| Strong Opioids | |||
| PACU | 35 (45.5) | 7 (21.9) | 0.03 |
| Day 0 | 20 (26.0) | 1 (3.1) | <0.01 |
| Day 1 | 28 (36.4) | 4 (12.5) | 0.02 |
| Variables | Univariable Analysis | |
|---|---|---|
| OR (95% CI) | p-Value | |
| Age | 1.0 (0.99–1.01) | 0.76 |
| BMI | 1.01 (0.99–1.03) | 0.20 |
| Comorbidities | 0.94 (0.77–1.16) | 0.58 |
| Indication for hysterectomy | 1.04 (0.98–1.10) | 0.20 |
| Surgical approach | 1.38 (1.13–1.69) | 0.002 |
| Mean intraoperative pneumoperitoneum pressure | ||
| 6–8 | ref | |
| ≥9 | 1.25 (1.03–1.51) | 0.026 |
| Mean intraoperative pressure (continuous) | 1.043 (1.001–1.087) | 0.046 |
| Uterus size | 1.00 (0.99–1.00) | 0.58 |
| Adherences | 1.01 (0.83–1.23) | 0.92 |
| Duration of pneumoperitoneum | 1.00 (0.99–1.00) | 0.44 |
| Ropivacaine port infiltration | 1.11 (0.90–1.37) | 0.33 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dabi, Y.; Ouasti, S.; Didelot, H.; Wohrer, H.; Skalli, D.; Miailhe, G.; Uzan, J.; Ferrier, C.; Bendifallah, S.; Haddad, B.; et al. Total Hysterectomy by Low-Impact Laparoscopy to Decrease Opioids Consumption: A Prospective Cohort Study. J. Clin. Med. 2022, 11, 2165. https://doi.org/10.3390/jcm11082165
Dabi Y, Ouasti S, Didelot H, Wohrer H, Skalli D, Miailhe G, Uzan J, Ferrier C, Bendifallah S, Haddad B, et al. Total Hysterectomy by Low-Impact Laparoscopy to Decrease Opioids Consumption: A Prospective Cohort Study. Journal of Clinical Medicine. 2022; 11(8):2165. https://doi.org/10.3390/jcm11082165
Chicago/Turabian StyleDabi, Yohann, Samia Ouasti, Hélène Didelot, Henri Wohrer, Dounia Skalli, Gregoire Miailhe, Jennifer Uzan, Clément Ferrier, Sofiane Bendifallah, Bassam Haddad, and et al. 2022. "Total Hysterectomy by Low-Impact Laparoscopy to Decrease Opioids Consumption: A Prospective Cohort Study" Journal of Clinical Medicine 11, no. 8: 2165. https://doi.org/10.3390/jcm11082165
APA StyleDabi, Y., Ouasti, S., Didelot, H., Wohrer, H., Skalli, D., Miailhe, G., Uzan, J., Ferrier, C., Bendifallah, S., Haddad, B., Daraï, E., & Touboul, C. (2022). Total Hysterectomy by Low-Impact Laparoscopy to Decrease Opioids Consumption: A Prospective Cohort Study. Journal of Clinical Medicine, 11(8), 2165. https://doi.org/10.3390/jcm11082165






