Biomechanical Effects of Plastic Heel Cup on Plantar Fasciitis Patients Evaluated by Ultrasound Shear Wave Elastography
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
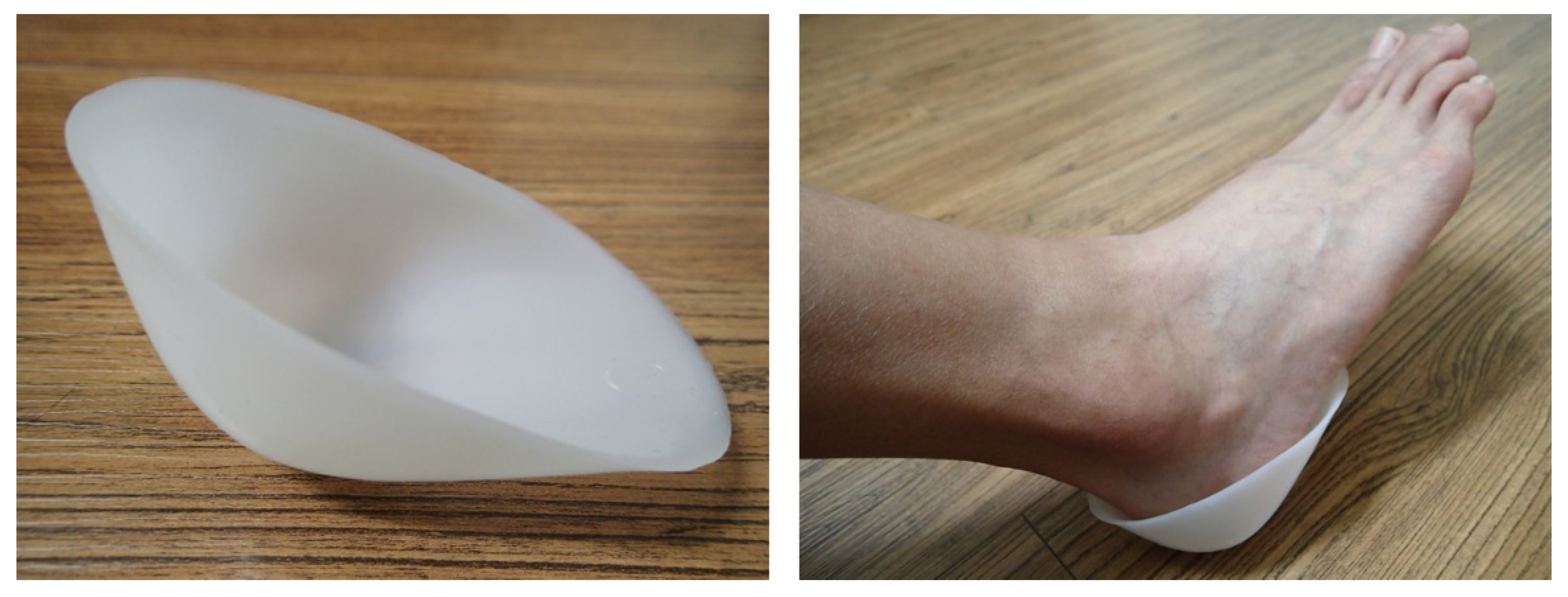
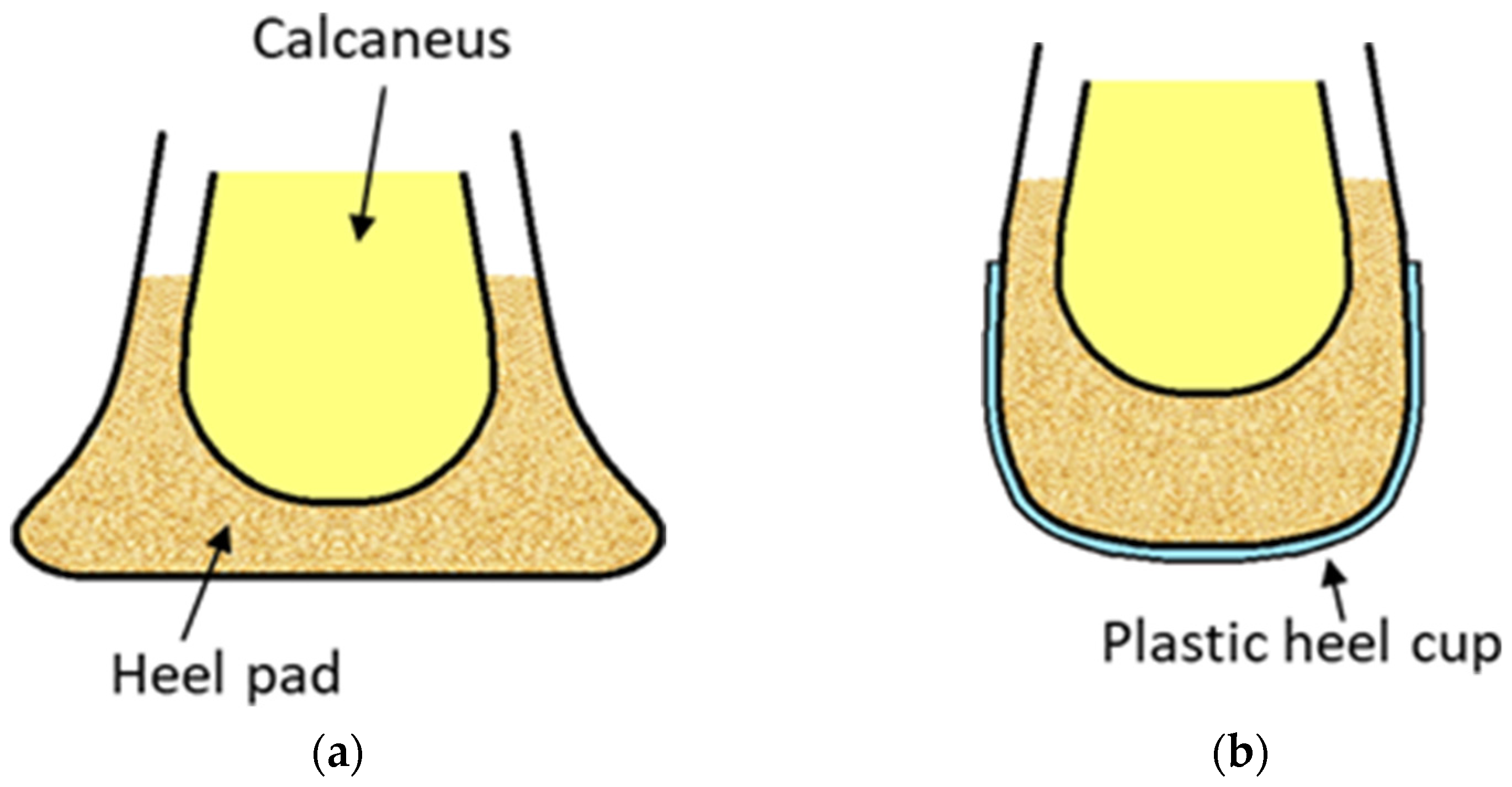
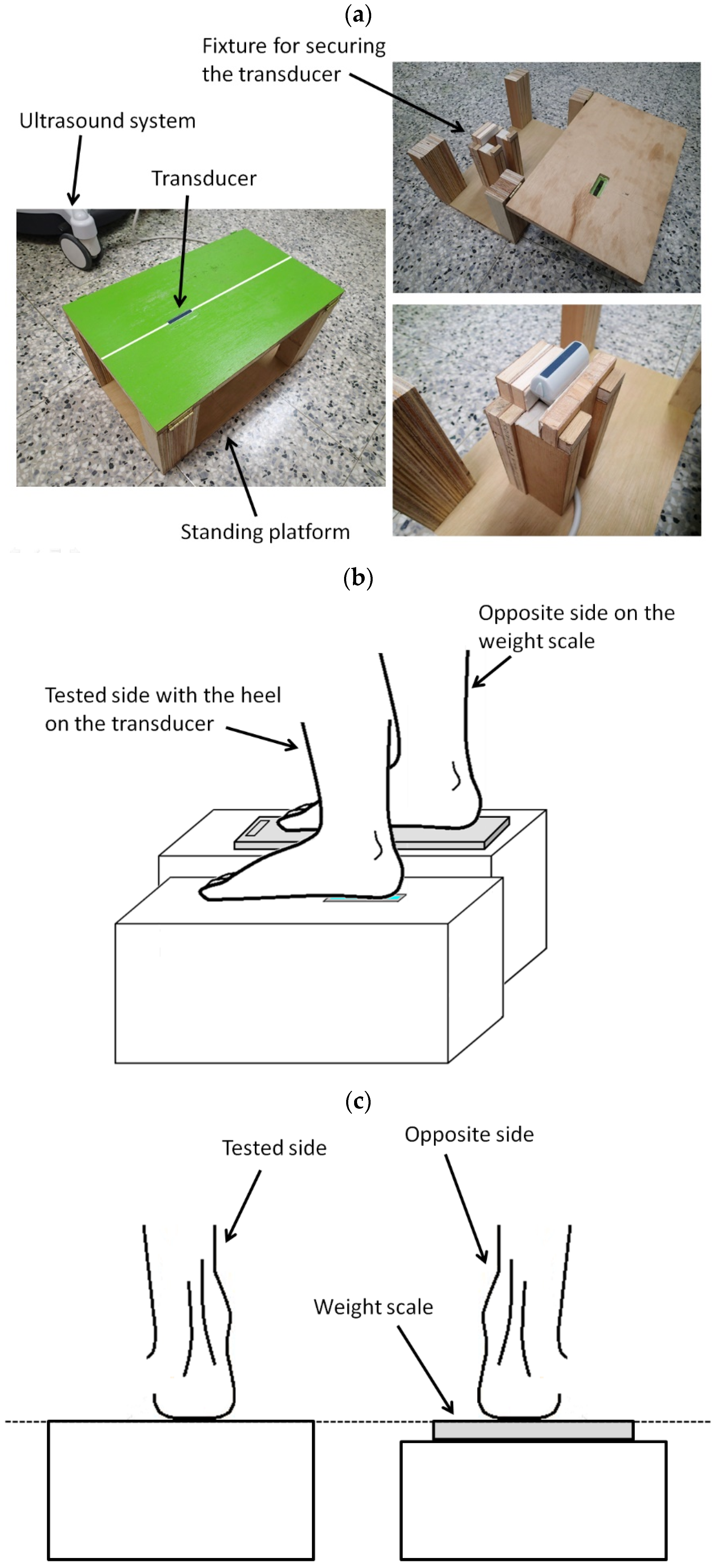
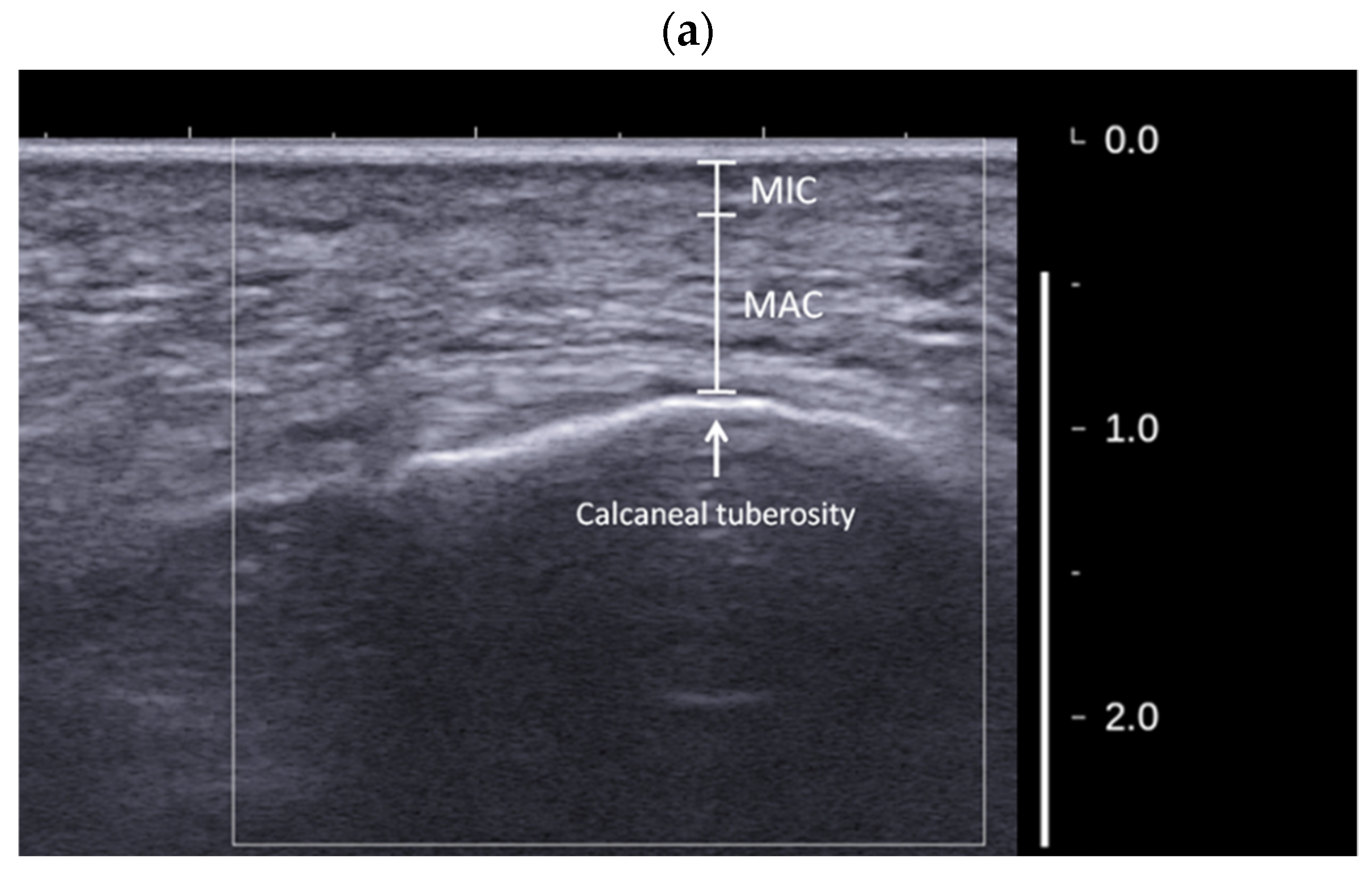
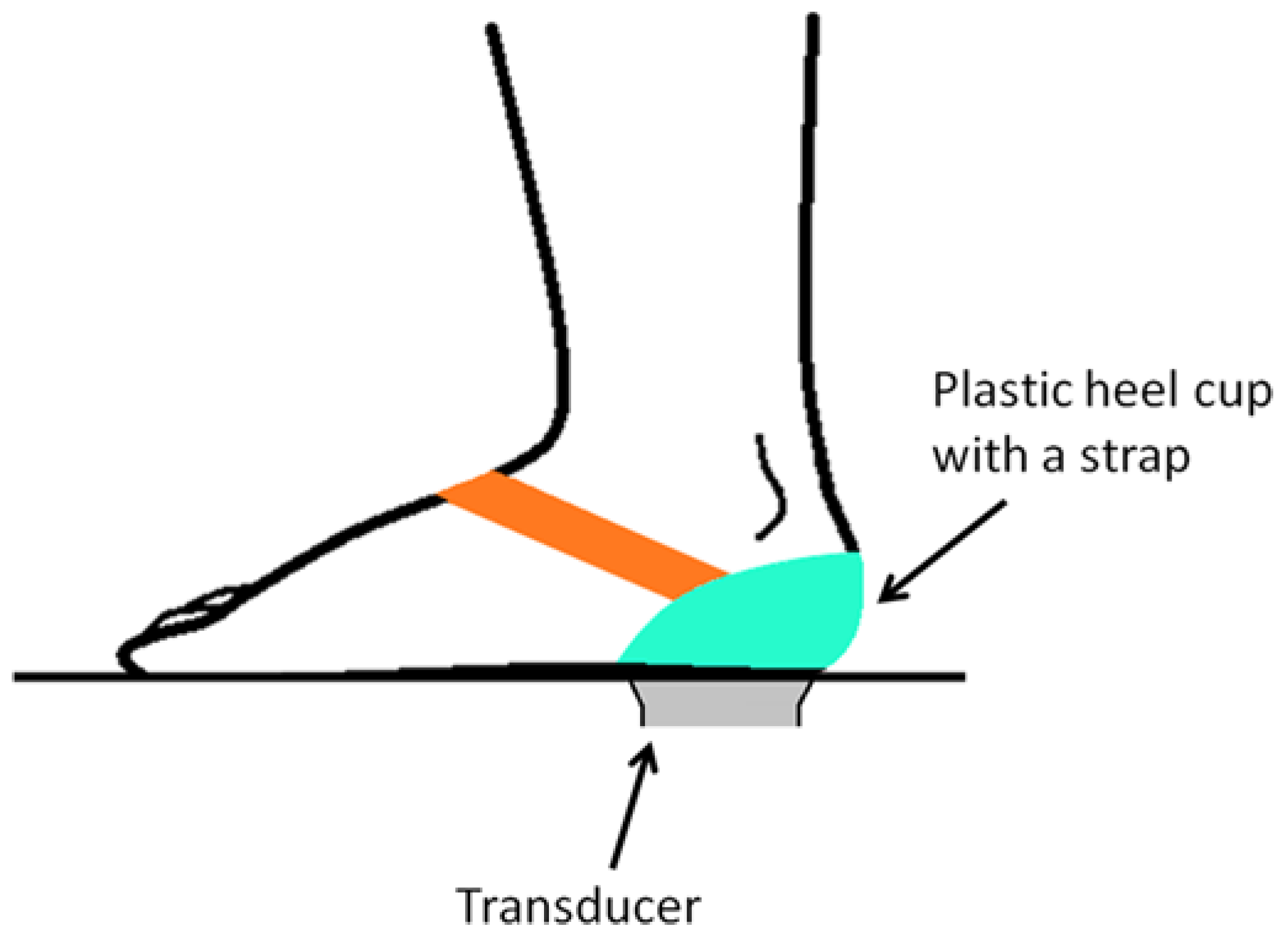
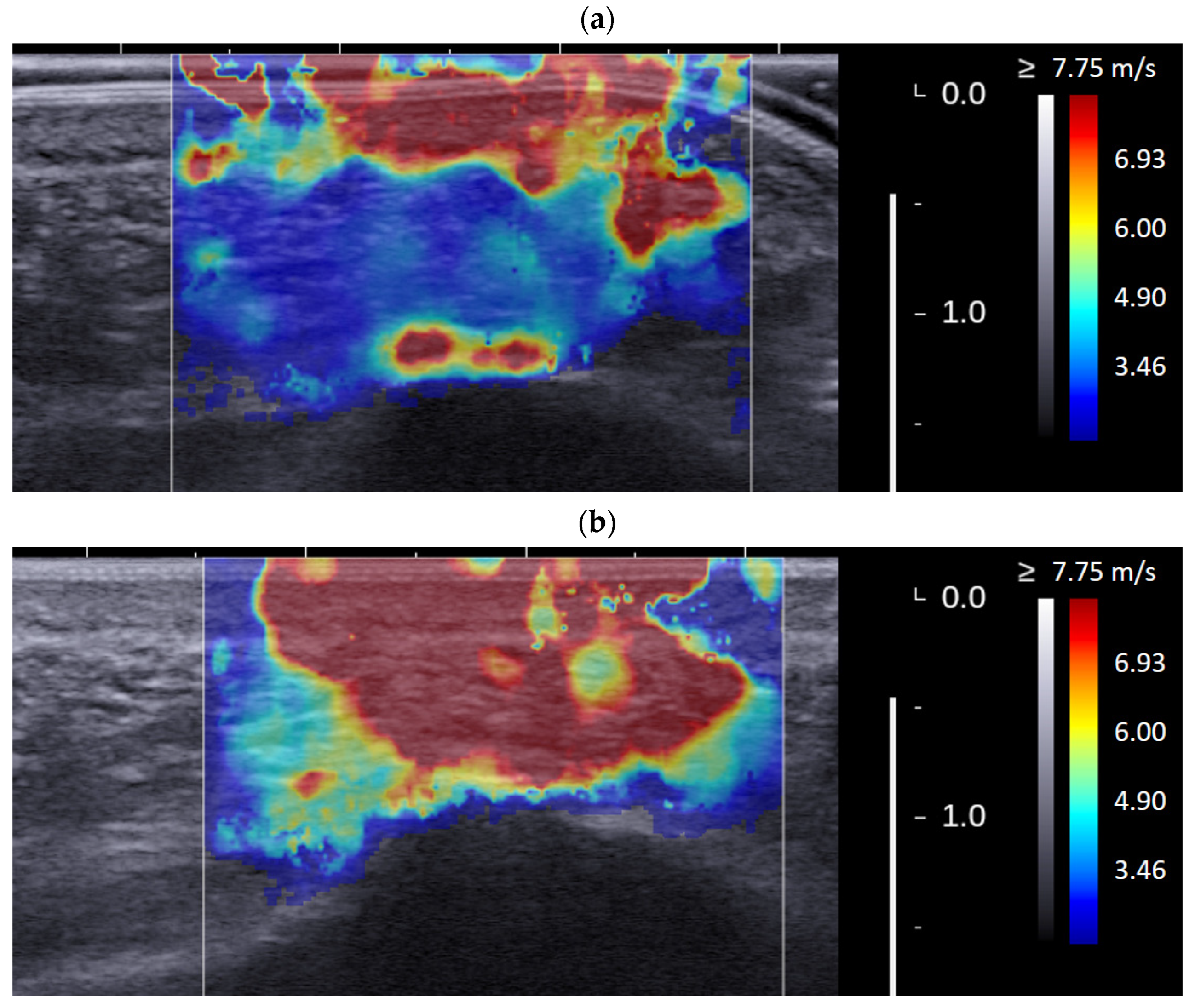
2.2. Experimental Systems and Setups
2.3. Reliability Test of the Measurement Protocol
2.4. Testing Procedure and Analysis Method for Plantar Fasciitis Patients
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cotchett, M.P.; Whittaker, G.; Erbas, B. Psychological variables associated with foot function and foot pain in patients with plantar heel pain. Clin. Rheumatol. 2015, 34, 957–964. [Google Scholar] [CrossRef] [PubMed]
- Whittaker, G.A.; Munteanu, S.E.; Menz, H.B.; Elzarka, A.; Landorf, K.B. Corticosteroid injections compared to foot orthoses for plantar heel pain: Protocol for the SOOTHE heel pain randomised trial. Contemp. Clin. Trials Commun. 2017, 5, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McPoil, T.G.; Martin, R.L.; Cornwall, M.W.; Wukich, D.K.; Irrgang, J.J.; Godges, J.J. Heel pain—plantar fasciitis. J. Orthop. Sports Phys. Ther. 2008, 38, A1–A18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosenbaum, A.J.; DiPreta, J.A.; Misener, D. Plantar heel pain. Med. Clin. 2014, 98, 339–352. [Google Scholar] [CrossRef] [PubMed]
- Snook, G.A.; Chrisman, O.D. The management of subcalcaneal pain. Clin. Orthop. Relat. Res. 1972, 82, 163–168. [Google Scholar] [CrossRef]
- Montgomery, R.M.; Locascio, W.V. Padding and devices for foot comfort. Arch. Dermatol. 1966, 93, 739–743. [Google Scholar] [CrossRef]
- Scranton, P.E., Jr.; Pedegana, L.R.; Whitesel, J.P. Gait analysis: Alterations in support phase forces using supportive devices. Am. J. Sports Med. 1982, 10, 6–11. [Google Scholar] [CrossRef]
- Katoh, Y.; Chao, E.Y.S.; Morrey, B.F.; Laughman, R.K. Objective technique for evaluating painful heel syndrome and its treatment. Foot Ankle 1983, 3, 227–236. [Google Scholar] [CrossRef]
- Jørgensen, U.; Ekstrand, J. Significance of heel pad confinement for the shock absorption at heel strike. Int. J. Sports Med. 1988, 9, 468–473. [Google Scholar] [CrossRef]
- Wang, C.L.; Cheng, C.K.; Tsuang, Y.H.; Hang, Y.S.; Liu, T.K. Cushioning effect of heel cups. Clin. Biomech. 1994, 9, 297–302. [Google Scholar] [CrossRef]
- Telfer, S.; Woodburn, J.; Turner, D.E. Measurement of functional heel pad behaviour in-shoe during gait using orthotic embedded ultrasonography. Gait Posture 2014, 39, 328–332. [Google Scholar] [CrossRef] [PubMed]
- Rome, K. Mechanical properties of the heel pad: Current theory and review of the literature. Foot 1998, 8, 179–185. [Google Scholar] [CrossRef]
- Gefen, A. Plantar soft tissue loading under the medial metatarsals in the standing diabetic foot. Med. Eng. Phys. 2003, 25, 491–499. [Google Scholar] [CrossRef]
- Gefen, A.; Linder-Ganz, E. Diffusion of ulcers in the diabetic foot is promoted by stiffening of plantar muscular tissue under excessive bone compression. Orthopade 2004, 33, 999–1012. [Google Scholar]
- Hsu, C.C.; Tsai, W.C.; Wang, C.L.; Pao, S.H.; Shau, Y.W.; Chuan, Y.S. Microchambers and macrochambers in heel pads: Are they functionally different? J. Appl. Physiol. 2007, 102, 2227–2231. [Google Scholar] [CrossRef]
- Hsu, C.C.; Tsai, W.C.; Hsiao, T.Y.; Tseng, F.Y.; Shau, Y.W.; Wang, C.L.; Lin, S.C. Diabetic effects on microchambers and macrochambers tissue properties in human heel pads. Clin. Biomech. 2009, 24, 682–686. [Google Scholar] [CrossRef]
- Hsu, C.-C.; Chen, C.P.-C.; Lin, S.-C.; Tsai, W.-C.; Liu, H.-T.; Lin, Y.-C.; Lee, H.-J.; Chen, W.-P. Determination of the augmentation effects of hyaluronic acid on different heel structures in amputated lower limbs of diabetic patients using ultrasound elastography. Ultrasound Med. Biol. 2012, 38, 943–952. [Google Scholar] [CrossRef]
- Naemi, R.; Chockalingam, N. Mathematical models to assess foot-ground interaction: An overview. Med. Sci. Sports Exerc. 2013, 45, 1524–1533. [Google Scholar] [CrossRef]
- Teoh, J.C.; Lee, T. Prediction of plantar soft tissue stiffness based on sex, age, bodyweight, height and body mass index. J. Mech. Behav. Biomed. Mater. 2016, 54, 219–222. [Google Scholar] [CrossRef]
- Ahanchian, N.; Nester, C.J.; Howard, D.; Ren, L.; Parker, D. Estimating the material properties of heel pad sub-layers using inverse Finite Element Analysis. Med. Eng. Phys. 2017, 40, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.H.; Lin, C.Y.; Hsiao, M.Y.; Cheng, Y.H.; Chen, W.S.; Wang, T.G. Altered stiffness of microchamber and macrochamber layers in the aged heel pad: Shear wave ultrasound elastography evaluation. J. Formos. Med. Assoc. 2018, 117, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Bercoff, J.; Tanter, M.; Fink, M. Supersonic shear imaging: A new technique for soft tissue elasticity mapping. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2004, 51, 396–409. [Google Scholar] [CrossRef] [PubMed]
- Wells, P.N.; Liang, H.D. Medical ultrasound: Imaging of soft tissue strain and elasticity. J. R. Soc. Interface 2011, 8, 1521–1549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eby, S.F.; Song, P.; Chen, S.; Chen, Q.; Greenleaf, J.F.; An, K.N. Validation of shear wave elastography in skeletal muscle. J. Biomech. 2013, 46, 2381–2387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koo, T.K.; Guo, J.Y.; Cohen, J.H.; Parker, K.J. Relationship between shear elastic modulus and passive muscle force: An ex-vivo study. J. Biomech. 2013, 46, 2053–2059. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.J.; Fu, S.N. Shear elastic modulus on patellar tendon captured from supersonic shear imaging: Correlation with tangent traction modulus computed from material testing system and test–retest reliability. PLoS ONE 2013, 8, e68216. [Google Scholar] [CrossRef] [Green Version]
- Martin, J.A.; Biedrzycki, A.H.; Lee, K.S.; DeWall, R.J.; Brounts, S.H.; Murphy, W.L.; Markel, M.D.; Thelen, D.G. In vivo measures of shear wave speed as a predictor of tendon elasticity and strength. Ultrasound Med. Biol. 2015, 41, 2722–2730. [Google Scholar] [CrossRef] [Green Version]
- Lin, C.Y.; Lin, C.C.; Chou, Y.C.; Chen, P.Y.; Wang, C.L. Heel pad stiffness in plantar heel pain by shear wave elastography. Ultrasound Med. Biol. 2015, 41, 2890–2898. [Google Scholar] [CrossRef]
- Lin, C.Y.; Chen, P.Y.; Shau, Y.W.; Tai, H.C.; Wang, C.L. Spatial-dependent mechanical properties of the heel pad by shear wave elastography. J. Biomech. 2017, 53, 191–195. [Google Scholar] [CrossRef]
- Taş, S.; Bek, N.; Ruhi Onur, M.; Korkusuz, F. Effects of body mass index on mechanical properties of the plantar fascia and heel pad in asymptomatic participants. Foot Ankle Int. 2017, 38, 779–784. [Google Scholar] [CrossRef]
- Taş, S. Effect of gender on mechanical properties of the plantar fascia and heel fat pad. Foot Ankle Spec. 2018, 11, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Taş, S.; Bek, N. Effects of morphological and mechanical properties of plantar fascia and heel pad on balance performance in asymptomatic females. Foot 2018, 36, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Chatzistergos, P.E.; Behforootan, S.; Allan, D.; Naemi, R.; Chockalingam, N. Shear wave elastography can assess the in-vivo nonlinear mechanical behavior of heel-pad. J. Biomech. 2018, 80, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Urban, M.W.; Nenadic, I.Z.; Chen, S.; Greenleaf, J.F. Discrepancies in reporting tissue material properties. J. Ultrasound Med. 2013, 32, 886. [Google Scholar] [CrossRef]
- Luximon, A.; Goonetilleke, R.S.; Zhang, M. 3D foot shape generation from 2D information. Ergonomics 2005, 48, 625–641. [Google Scholar] [CrossRef]
- Lin, C.Y.; Chen, P.Y.; Shau, Y.W.; Wang, C.L. An artifact in supersonic shear wave elastography. Ultrasound Med. Biol. 2017, 43, 517–530. [Google Scholar] [CrossRef]
- Naemi, R.; Chatzistergos, P.; Sundar, L.; Chockalingam, N.; Ramachandran, A. Differences in the mechanical characteristics of plantar soft tissue between ulcerated and non-ulcerated foot. J. Diabetes Complicat. 2016, 30, 1293–1299. [Google Scholar] [CrossRef]
- Naemi, R.; Chatzistergos, P.E.; Chockalingam, N. A mathematical method for quantifying in vivo mechanical behaviour of heel pad under dynamic load. Med. Biol. Eng. Comput. 2016, 54, 341–350. [Google Scholar] [CrossRef]
- Behforootan, S.; Chatzistergos, P.E.; Chockalingam, N.; Naemi, R. A clinically applicable non-invasive method to quantitatively assess the visco-hyperelastic properties of human heel pad, implications for assessing the risk of mechanical trauma. J. Mech. Behav. Biomed. Mater. 2017, 68, 287–295. [Google Scholar] [CrossRef] [Green Version]
- Perhamre, S.; Lundin, F.; Klässbo, M.; Norlin, R. A heel cup improves the function of the heel pad in Sever’s injury: Effects on heel pad thickness, peak pressure and pain. Scand. J. Med. Sci. Sports 2012, 22, 516–522. [Google Scholar] [CrossRef]
- Spears, I.R.; Miller-Young, J.E.; Sharma, J.; Ker, R.F.; Smith, F.W. The potential influence of the heel counter on internal stress during static standing: A combined finite element and positional MRI investigation. J. Biomech. 2007, 40, 2774–2780. [Google Scholar] [CrossRef] [PubMed]
- Tu, P.; Bytomski, J.R. Diagnosis of heel pain. Am. Fam. Phys. 2011, 84, 909–916. [Google Scholar] [PubMed]
- Todros, S.; Biz, C.; Ruggieri, P.; Pavan, P.G. Experimental Analysis of Plantar Fascia Mechanical Properties in Subjects with Foot Pathologies. Appl. Sci. 2021, 11, 1517. [Google Scholar] [CrossRef]
- Stecco, C.; Corradin, M.; Macchi, V.; Morra, A.; Porzionato, A.; Biz, C.; De Caro, R. Plantar fascia anatomy and its relationship with A chilles tendon and paratenon. J. Anat. 2013, 223, 665–676. [Google Scholar] [CrossRef]
- Onwuanyi, O.N. Calcaneal spurs and plantar heel pad pain. Foot 2000, 10, 182–185. [Google Scholar] [CrossRef]
- Johal, K.S.; Milner, S.A. Plantar fasciitis and the calcaneal spur: Fact or fiction? Foot Ankle Surg. 2012, 18, 39–41. [Google Scholar] [CrossRef]
- Stecco, C.; Fede, C.; Macchi, V.; Porzionato, A.; Petrelli, L.; Biz, C.; Stern, R.; De Caro, R. The fasciacytes: A new cell devoted to fascial gliding regulation. Clin. Anat. 2018, 31, 667–676. [Google Scholar] [CrossRef]
- Barnes, A.; Sullivan, J.; Pappas, E.; Adams, R.; Burns, J. Clinical and Functional Characteristics of People with Chronic and Recent-Onset Plantar Heel Pain. PM&R 2017, 9, 1128–1134. [Google Scholar]
- Irving, D.B.; Cook, J.L.; Menz, H.B. Factors associated with chronic plantar heel pain: A systematic review. J. Sci. Med. Sport 2006, 9, 11–22. [Google Scholar] [CrossRef]
- Landorf, K.B. Plantar heel pain and plantar fasciitis. BMJ Clin. Evid. 2015, 2015, 1111. [Google Scholar]
- Gefen, A.; Megido-Ravid, M.; Itzchak, Y. In vivo biomechanical behavior of the human heel pad during the stance phase of gait. J. Biomech. 2001, 34, 1661–1665. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, C.-Y.; Chen, P.-Y.; Wu, S.-H.; Shau, Y.-W.; Wang, C.-L. Biomechanical Effects of Plastic Heel Cup on Plantar Fasciitis Patients Evaluated by Ultrasound Shear Wave Elastography. J. Clin. Med. 2022, 11, 2150. https://doi.org/10.3390/jcm11082150
Lin C-Y, Chen P-Y, Wu S-H, Shau Y-W, Wang C-L. Biomechanical Effects of Plastic Heel Cup on Plantar Fasciitis Patients Evaluated by Ultrasound Shear Wave Elastography. Journal of Clinical Medicine. 2022; 11(8):2150. https://doi.org/10.3390/jcm11082150
Chicago/Turabian StyleLin, Che-Yu, Pei-Yu Chen, Shin-Han Wu, Yio-Wha Shau, and Chung-Li Wang. 2022. "Biomechanical Effects of Plastic Heel Cup on Plantar Fasciitis Patients Evaluated by Ultrasound Shear Wave Elastography" Journal of Clinical Medicine 11, no. 8: 2150. https://doi.org/10.3390/jcm11082150
APA StyleLin, C.-Y., Chen, P.-Y., Wu, S.-H., Shau, Y.-W., & Wang, C.-L. (2022). Biomechanical Effects of Plastic Heel Cup on Plantar Fasciitis Patients Evaluated by Ultrasound Shear Wave Elastography. Journal of Clinical Medicine, 11(8), 2150. https://doi.org/10.3390/jcm11082150





