Ophthalmological Impairments at Five and a Half Years after Preterm Birth: EPIPAGE-2 Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
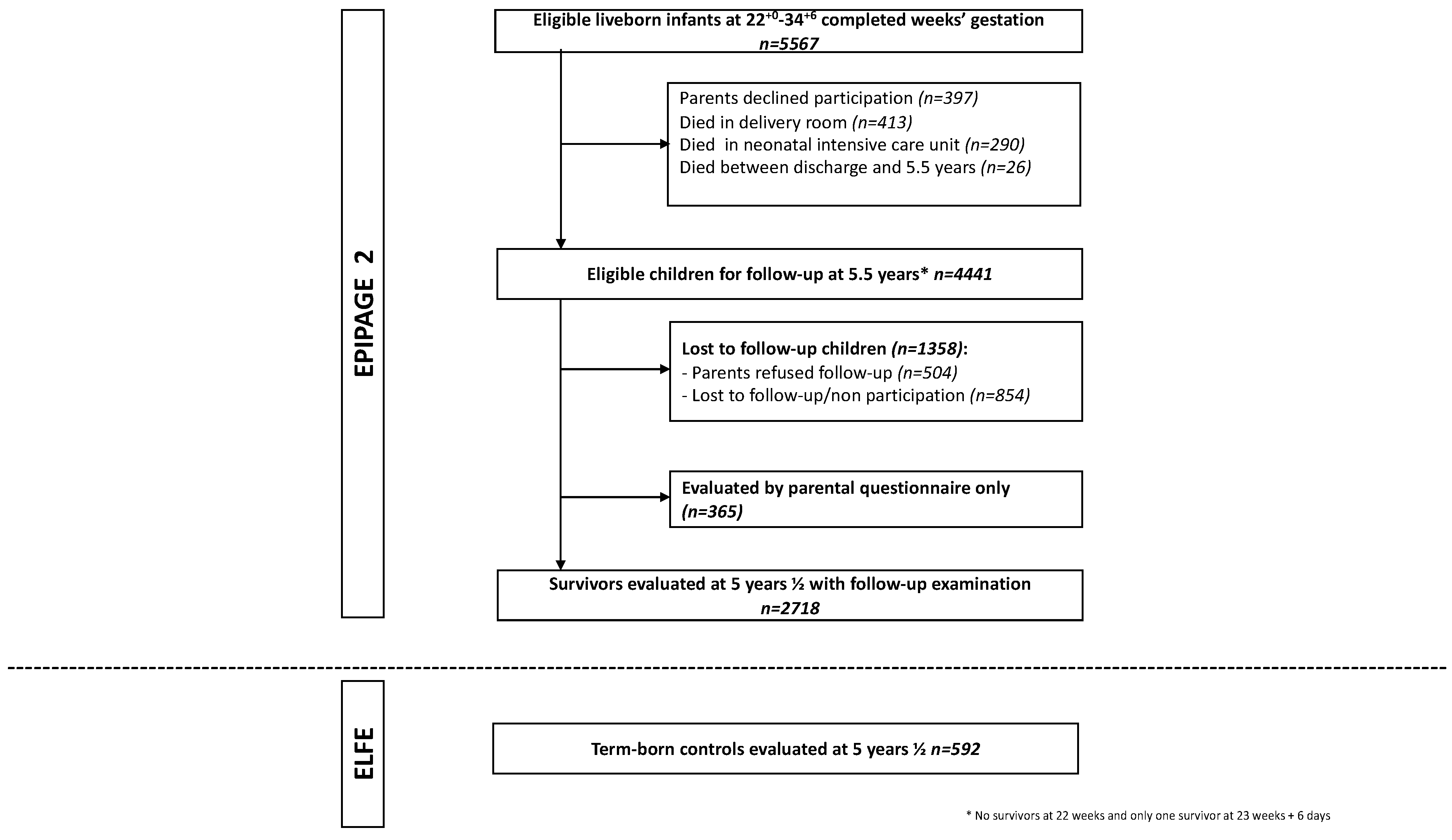
2.1. Study Design and Population
2.2. Data Collection at 5½ Years of Age
2.3. Visual Outcomes at 5½ Years of Age
2.4. Maternal and Children Characteristics
2.5. Data Management and Statistics
2.6. Ethics
3. Results
3.1. Population
3.2. Ophthalmological Impairments and Binocular Visual Acuity
3.3. Ophthalmological Impairments among Children with CP or Previous History of ROP
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pierrat, V.; Marchand-Martin, L.; Marret, S.; Arnaud, C.; Benhammou, V.; Cambonie, G.; Debillon, T.; Dufourg, M.-N.; Gire, C.; Goffinet, F.; et al. Neurodevelopmental outcomes at age 5 among children born preterm: EPIPAGE-2 cohort study. BMJ 2021, 373, n741. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.; Marlow, N. Early and long-term outcome of infants born extremely preterm. Arch. Dis. Child. 2016, 102, 97–102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allotey, J.; Zamora, J.; Cheong-See, F.; Kalidindi, M.; Arroyo-Manzano, D.; Asztalos, E.; Van Der Post, J.A.M.; Mol, B.W.; Moore, D.; Birtles, D.; et al. Cognitive, motor, behavioural and academic performances of children born preterm: A meta-analysis and systematic review involving 64 061 children. BJOG Int. J. Obstet. Gynaecol. 2017, 125, 16–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heydarian, S.; Abbasabadi, M.M.; Khabazkhoob, M.; Hoseini-Yazdi, H.; Gharib, M. Vision Abnormalities in Children and Young Adults with Cerebral Palsy; A Systematic Review. Semin. Ophthalmol. 2022, 3, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Pathai, S.; Cumberland, P.M.; Rahi, J.S. Prevalence of and Early-Life Influences on Childhood Strabismus. Arch. Pediatr. Adolesc. Med. 2010, 164, 250–257. [Google Scholar] [CrossRef] [Green Version]
- Hellgren, K.M.; Tornqvist, K.; Jakobsson, P.G.; Lundgren, P.; Carlsson, B.; Källén, K.; Serenius, F.; Hellström, A.; Holmström, G. Ophthalmologic Outcome of Extremely Preterm Infants at 6.5 Years of Age. JAMA Ophthalmol. 2016, 134, 555–562. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- VanderVeen, D.K.; Allred, E.N.; Wallace, D.K.; Leviton, A.; for the ELGAN Study Investigators. Strabismus at Age 2 Years in Children Born before 28 Weeks’ Gestation. J. Child Neurol. 2015, 31, 451–460. [Google Scholar] [CrossRef] [Green Version]
- Pivodic, A.; Hård, A.-L.; Löfqvist, C.; Smith, L.E.H.; Wu, C.; Bründer, M.-C.; Lagrèze, W.A.; Stahl, A.; Holmström, G.; Albertsson-Wikland, K.; et al. Individual Risk Prediction for Sight-Threatening Retinopathy of Prematurity Using Birth Characteristics. JAMA Ophthalmol. 2020, 138, 21–29. [Google Scholar] [CrossRef] [Green Version]
- Hreinsdottir, J.; Kaul, Y.F.; Hellström-Westas, L.; Rosander, K.; von Hofsten, C.; Holmström, G. Impaired cognitive ability at 2.5 years predicts later visual and ophthalmological problems in children born very preterm. Acta Paediatr. 2017, 107, 822–830. [Google Scholar] [CrossRef]
- Larsson, E.; Rydberg, A.; Holmström, G. Contrast sensitivity in 10 year old preterm and full term children: A population based study. Br. J. Ophthalmol. 2006, 90, 87–90. [Google Scholar] [CrossRef] [Green Version]
- O’Connor, A.; Fielder, A.R. Long term ophthalmic sequelae of prematurity. Early Hum. Dev. 2008, 84, 101–106. [Google Scholar] [CrossRef]
- Williams, C.; Northstone, K.; Sabates, R.; Feinstein, L.; Emond, A.; Dutton, G.N. Visual Perceptual Difficulties and Under-Achievement at School in a Large Community-Based Sample of Children. PLoS ONE 2011, 6, e14772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Webber, A.L.; Wood, J.M.; Gole, G.A.; Brown, B.; Tsui, J.Y.; Dalgard, C.; Van Quill, K.R.; Lee, L.; Grossniklaus, H.E.; Edelhauser, H.F.; et al. The Effect of Amblyopia on Fine Motor Skills in Children. Investig. Opthalmology Vis. Sci. 2008, 49, 594–603. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Inserm collectif. Déficits Visuels: Dépistage et Prise en Charge chez le Jeune Enfant. Rapport 2002. 2002. Available online: http://hdl.handle.net/10608/163 (accessed on 15 January 2022).
- Healthy Child Programme: Pregnancy and the First 5 Years of Life. GOV.UK. Available online: https://www.gov.uk/government/publications/healthy-child-programme-pregnancy-and-the-first-5-years-of-life (accessed on 28 January 2022).
- Recommandations Françaises pour le Depistage de la Retinopathie des Prematures-pdf. Available online: https://docplayer.fr/19824265-Recommandations-francaises-pour-le-depistage-de-la-retinopathie-des-prematures.html (accessed on 18 September 2018).
- NICE Guideline. Development Follow-Up of Children and Young People Born Preterm. 2017. Available online: https://www.nice.org.uk/guidance/ng72 (accessed on 15 January 2022).
- Ancel, P.-Y.; Goffinet, F. EPIPAGE 2: A preterm birth cohort in France in 2011. BMC Pediatr. 2014, 14, 97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lorthe, E.; Benhammou, V.; Marchand-Martin, L.; Pierrat, V.; Lebeaux, C.; Durox, M.; Goffinet, F.; Kaminski, M.; Ancel, P.-Y.; Astruc, D.; et al. Cohort Profile: The Etude Epidémiologique sur les Petits Ages Gestationnels-2 (EPIPAGE-2) preterm birth cohort. Int. J. Epidemiology 2021, 50, 1428–1429. [Google Scholar] [CrossRef] [PubMed]
- Pierrat, V.; Marchand-Martin, L.; Arnaud, C.; Kaminski, M.; Resche-Rigon, M.; Lebeaux, C.; Bodeau-Livinec, F.; Morgan, A.; Goffinet, F.; Marret, S.; et al. Neurodevelopmental outcome at 2 years for preterm children born at 22 to 34 weeks’ gestation in France in 2011: EPIPAGE-2 cohort study. BMJ 2017, 358, j3448. [Google Scholar] [CrossRef] [Green Version]
- Charles, M.A.; Thierry, X.; Lanoe, J.L.; Bois, C.; Dufourg, M.N.; Popa, R.; Cheminat, M.; Zaros, C.; Geay, B. Cohort Profile: The French national cohort of children (ELFE): Birth to 5 years. Int. J. Epidemiol. 2020, 49, 368–369j. [Google Scholar] [CrossRef]
- Zanlonghi, X.; Avital, S.; Sander, M.S. Comparaison de deux échelles logarithmique d’acuité visuelle de loin pour l’enfant: Rossano et Sander-Zanlonghi. J. Français Orthopt. 1999, 31, 199–216. [Google Scholar]
- Vision impairment and Blindness. Available online: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment (accessed on 16 September 2021).
- O’Connor, A.R.; Fielder, A.R. Visual Outcomes and Perinatal Adversity. Semin. Fetal. Neonatal. Med. 2007, 12, 408–414. [Google Scholar] [CrossRef]
- Ego, A.; Prunet, C.; Blondel, B.; Kaminski, M.; Goffinet, F.; Zeitlin, J. Customized and non-customized French intrauterine growth curves. II—Comparison with existing curves and benefits of customization. J. Gynecol. Obstet. Biol. Reprod. 2015, 45, 165–176. [Google Scholar] [CrossRef]
- Ancel, P.-Y.; Goffinet, F.; Kuhn, P.; Langer, B.; Matis, J.; Hernandorena, X.; Chabanier, P.; Joly-Pedespan, L.; Lecomte, B.; EPIPAGE-2 Writing Group; et al. Survival and Morbidity of Preterm Children Born at 22 Through 34 Weeks’ Gestation in France in 2011: Results of the EPIPAGE-2 Cohort Study. JAMA Pediatr. 2015, 169, 230–238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch. Ophthalmol. 2005, 123, 991–999. [Google Scholar] [CrossRef] [PubMed]
- Ghassabian, A.; Sundaram, R.; Bell, E.; Bello, S.C.; Kus, C.; Yeung, E. Gross Motor Milestones and Subsequent Development. Pediatrics 2016, 138, e20154372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, T. Movement Assessment Battery for Children: 2nd Edition (MABC-2). In Encyclopedia of Autism Spectrum Disorders; Springer: New York, NY, USA, 2013; pp. 1925–1939. [Google Scholar]
- Chapron, T.; Caputo, G.; Pierrat, V.; Kermorvant, E.; Barjol, A.; Durox, M.; Ancel, P.-Y.; Torchin, H. Screening for Retinopathy of Prematurity in Very Preterm Children: The EPIPAGE-2 Cohort Study. Neonatology 2021, 118, 80–89. [Google Scholar] [CrossRef] [PubMed]
- White, I.R.; Royston, P.; Wood, A.M. Multiple imputation using chained equations: Issues and guidance for practice. Stat. Med. 2010, 30, 377–399. [Google Scholar] [CrossRef] [PubMed]
- Rubin, D.B. Frontmatter. In Multiple Imputation for Nonresponse in Surveys; John Wiley & Sons, Inc.: New York, NY, USA, 1987; pp. i–xxix. [Google Scholar] [CrossRef]
- Demir, S.T.; Bas, E.K.; Karapapak, M.; Karatas, M.E.; Uslu, H.S.; Bulbul, A.; Guven, D. Effect of Prematurity on Foveal Development in Early School-Age Children. Am. J. Ophthalmol. 2020, 219, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Pétursdóttir, D.; Holmström, G.; Larsson, E. Visual function is reduced in young adults formerly born prematurely: A population-based study. Br. J. Ophthalmol. 2019, 104, 541–546. [Google Scholar] [CrossRef] [Green Version]
- Balasubramanian, S.; Borrelli, E.; Lonngi, M.; Velez, F.; Sarraf, D.; Sadda, S.R.; Tsui, I. Visual Function and Optical Coherence Tomography Angiography Features in Children Born Preterm. Retina 2019, 39, 2233–2239. [Google Scholar] [CrossRef]
- Tremblay, E.; Vannasing, P.; Roy, M.-S.; Lefebvre, F.; Kombate, D.; Lassonde, M.; Lepore, F.; McKerral, M.; Gallagher, A. Delayed Early Primary Visual Pathway Development in Premature Infants: High Density Electrophysiological Evidence. PLoS ONE 2014, 9, e107992. [Google Scholar] [CrossRef]
- Assessment of Visual Function—EFCNI. Available online: https://newborn-health-standards.org/assessment-visual-function/ (accessed on 16 September 2021).
- Eken, P.; van Nieuwenhuizen, O.; van der Graaf, Y.; Schalij-Delfos, N.E.; de Vries, L.S. Relation between neonatal cranial ultrasound abnormalities and cerebral visual impairment in infancy. Dev. Med. Child. Neurol 1994, 36, 3–15. [Google Scholar] [CrossRef]
| N (Total = 2718) * | 24–26 WG † | 27–31 WG | 32–34 WG | p ** | Reference Sample Term–Born Children ‡ | |||
|---|---|---|---|---|---|---|---|---|
| CC | MI | CC | MI | CC | MI | CC | ||
| n/N % (95% CI) | % (95% CI) | n/N % (95% CI) | % (95% CI) | n/N % (95% CI) | % (95% CI) | % (95% CI) | ||
| At least one ophthalmological impairment § | 150/325 46.1 (40.6–51.7) | – 48.5 (43.4–53.6) | 621/1666 37.3 (35.0–39.6) | – 39.7 (37.8–41.4) | 203/664 30.6 (27.1–34.2) | – 32.6 (30.4–34.2) | <0.001 | 23.8 (19.1–29.1) |
| Refractive errors | 133/294 45.2 (39.5–51.1) | – 43.1 (37.6–48.4) | 560/1514 37.0 (34.5–39.5) | – 35.2 (32.7–37.6) | 187/602 31.1 (27.4–35.0) | – 28.4 (25.0–31.8) | <0.001 | 24.1 (19.1–29.7) |
| Strabismus | 48/291 16.5 (12.4–21.3) | – 19.5 (14.6–24.4) | 185/1519 12.2 (10.6–13.9) | – 14.8 (12.9–16.7) | 41/609 6.7 (4.9–9.0) | – 8.3 (6.2–10.4) | <0.001 | 2.8 (1.0–5.3) |
| Amblyopia | 15/278 5.4 (3.1–8.7) | – 9.7 (5.7–13.6) | 65/1439 4.5 (3.5–5.7) | – 8.2 (6.2–10.1) | 24/594 4.0 (2.6–6.0) | – 6.4 (4.2–8.6) | 0.69 | 0.5 (0.3–2.6) |
| Nystagmus | 3/284 1.1 (0.2–3.1) | – 2.7 (0.8–4.7) | 8/1501 0.5 (0.2–1.0) | – 1.6 (0.8–2.3) | 4/609 0.7 (0.2–1.7) | – 1.4 (0.5–2.3) | 0.76 | 0.5 (0.3–2.6) |
| Visual deficiency | 0.43 $ | |||||||
| Severe and moderate VA <3.2/10 | 3 1.0 (0.2–2.8) | – 1.7 (0.2–3.3) | 7 0.4 (0.2–0.9) | – 0.8 (0.3–1.2) | 3 0.5 (0.1–1.3) | – 0.6 (0.0–1.1) | 0.7 (0.0–4.0) | |
| Mild VA 3.2/10–4/10 | 19 6.2 (3.8–9.5) | 8.1 (5.2–11.1) | 82 5.0 (4.0–6.2) | 5.9 (4.8–7.0) | 34 5.2 (3.6–7.2) | 5.4 (3.8–7.1) | 3.0 (1.1–6.3) | |
| None | ||||||||
| VA 5/10–6.3/10 | 124 40.3 (34.7–46.0) | 40.6 (35.3–45.8) | 574 35.1 (32.8–37.5) | 35.8 (33.5–38.1) | 210 32.3 (28.7–36.0) | 33.7 (30.4–37.0) | 17.7 (13.6–22.4) | |
| VA 8/10 | 65 21.1 (16.7–26.1) | 21.0 (16.7–25.2) | 369 22.6 (20.6–24.7) | 22.4 (20.6–24.2) | 157 24.9 (21.7–28.4) | 24.3 (21.2–27.3) | 18.9 (14.6–23.8) | |
| VA 10/10 | 97 31.5 (26.3–37.0) | 28.6 (24.0–33.3) | 603 36.9 (34.5–39.3) | 35.1 (32.8–37.4) | 238 37.1 (33.4–41.0) | 36.0 (32.5–39.5) | 59.7 (53.9–65.4) | |
| Cerebral Palsy | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| None | GMFCS–1 | GMFCS–2 | GMFCS–3–5 | ||||||
| n/N CC % (95% CI) ORa * (95% CI) | MI ‡ % (95% CI) ORa * (95% CI) | n/N CC % (95% CI) ORa * (95% CI) | MI ‡ % (95% CI) ORa * (95% CI) | n/N CC % (95% CI) ORa * (95% CI) | MI ‡ % (95% CI) ORa * (95% CI) | n/N CC % (95% CI) ORa * (95% CI) | MI ‡ % (95% CI) ORa * (95% CI) | p | |
| Refractive errors | 807/2282 32.6 (30.1–35.3) 1 | 29.6 (27.2–32.0) 1 | 29/58 48.8 (30.6–67.2) 1.6 (1.0–2.7) | 49.4 (31.2–67.1) 2.0 (1.2–3.5) | 19/32 60.7 (36.6–81.4) 2.8 (1.3–6.2) | 61.2 (37.9–84.5) 3.2 (1.6–7.9) | 24/31 82.4 (64.6–93.7) 6.0 (2.5–14.4) | 75.8 (48.1–104) 5.5 (1.4–21.7) | <0.001 |
| Strabismus | 232/2294 8.1 (6.7–9.6) 1 | 9.3 (7.7–10.9) 1 | 13/56 13.0 (5.5–24.7) 2.6 (1.4–4.8) | 21.1 (7.3–34.8) 2.8 (1.5–5.2) | 12/33 32.7 (14.0–56.5) 4.6 (2.2–9.8) | 42.3 (20.1–64.5) 5.7 (2.7–12.1) | 17/29 68.4 (47.7–84.8) 11.3 (4.9–26.0) | 64.5 (38.7–90.5) 9.7 (3.5–26.7) | <0.001 |
| Retinopathy of prematurity | |||||||||
| None | ROP stages 1 or 2 | Severe ROP † | |||||||
| n/N CC % (95% CI) ORa * (95% CI) | MI ‡ % (95% CI) ORa * (95% CI) | n/N CC % (95% CI) ORa * (95% CI) | MI ‡ % (95% CI) ORa * (95% CI) | n/N CC % (95% CI) ORa * (95% CI) | MI ‡ % (95% CI) ORa * (95% CI) | ||||
| Refractive errors | 801/2237 33.2 (30.6–35.8) 1 | 30.5 (28.0–33.0) 1 | 62/149 41.3 (33.3–49.7) 1.1 (0.7–1.5) | 41.1 (33.8–48.4) 1.2 (0.9–1.6) | 17/24 70.5 (48.6–87.2) 3.1 (1.2–7.8) | 63.8 (45.8–81.8) 2.5 (1.2–5.5) | <0.001 | ||
| Strabismus | 244/2249 8.6 (7.2–10.1) 1 | 10.3 (8.5–12.0) 1 | 23/150 15.5 (10.1–22.3) 1.2 (0.7–1.9) | 19.4 (13.8–24.9) 1.3 (0.9–1.9) | 7/20 34.8 (15.3–59.1) 3.0 (1.1–8.2) | 43.0 (23.6–62.4) 3.4 (1.5–7.7) | <0.001 | ||
| Cerebral Palsy | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| No Cerebral Palsy | Stage 1 | Stage 2 | Stages 3 or 4 or 5 | ||||||
| CC n/N % (95% CI) ORa * (95% CI) | MI % (95% CI) ORa * (95% CI) | CC n/N % (95% CI) ORa * (95% CI) | MI % (95% CI) ORa * (95% CI) | CC n/N % (95% CI) ORa * (95% CI) | MI % (95% CI) ORa * (95% CI) | CC n/N % (95% CI) ORa * (95% CI) | MI % (95% CI) ORa * (95% CI) | p | |
| Visual deficiency | <0.001 | ||||||||
| Severe and moderate VA <3.2/10 | 11/2481 0.4 (0.1–0.8) 1 | – 0.4 (0.1–0.7) 1 | 0/57 0 0 | – 0 0 | 0/29 0 0 | – 0 0 | 2/22 23.9 (3.0–63.3) 42.9 (5.4–340.0) | – 14.1 (0.0–28.8) 86.1 (13.4–553.4) | |
| Mild VA 3.2/10–4/10 | 120/2481 4.9 (3.8–6.2) 1 | – 5.2 (4.0–6.4) 1 | 4/57 3.5 (0.4–12.1) 1.4 (0.5–3.9) | – 6.3 (0.0–14.0) 1.6 (0.6–4.3) | 6/29 22.2 (5.8–49.2) 9.0 (2.6–31.2) | – 20.0 (4.5–35.4) 7.9 (2.8–22.7) | 4/22 15.4 (3.8–37.1) 10.7 (2.3–49.1) | – 29.3 (11.5–47.1) 30.3 (8.0–115.4) | |
| None | |||||||||
| 5/10–6.3/10 | 863/2481 33.1 (30.6–35.6) 1 | – 34.2 (31.7–36.6) 1 | 23/57 47.0 (28.8–65.7) 1.0 (0.5–1.9) | – 43.5 (28.0–58.9) 1.1 (0.7–2.0) | 12/29 54.4 (29.8–77.5) 2.3 (0.8–6.7) | – 50.2 (29.7–70.7) 2.7 (1.1–6.8) | 9/22 33.7 (15.1–57.0) 2.8 (0.8–10.2) | – 41.5 (22.2–60.8) 6.2 (2.0–19.5) | |
| 8/10 | 578/2481 24.4 (22.2–26.8) 1 | – 24.0 (21.8–26.1) 1 | 8/57 12.0 (3.6–27.1) 0.6 (0.3–1.3) | – 16.4 (5.0–27.9) 0.8 (0.4–1.6) | 5/29 10.6 (2.3–27.7) 1.4 (0.4–4.9) | – 14.8 (2.1–27.6) 1.7 (0.6–4.4) | 4/22 15.4 (3.8–37.1) 1.9 (0.5–6.8) | – 9.0 (0.0–18.3) 2.3 (0.7–8.2) | |
| 10/10 | 909/2481 37.2 (34.6–39.8) 1 | – 36.2 (33.7–38.7) 1 | 22/57 37.5 (21.0–56.5) 1 | – 32.9 (18.3–47.6) 1 | 6/29 12.8 (3.4–30.5) 1 | – 12.9 (1.2–24.6) 1 | 3/22 11.6 (2.0–32.3) 1 | – 6.1 (0.0–15.2) 1 | |
| Retinopathy of prematurity | |||||||||
| No ROP | ROP stages 1 or 2 | Severe ROP† | |||||||
| CC n/N % (95% CI) ORa* (95% CI) | MI % (95% CI) ORa* (95% CI) | CC n/N % (95% CI) ORa* (95% CI) | MI % (95% CI) ORa* (95% CI) | CC n/N % (95% CI) ORa* (95% CI) | MI % (95% CI) ORa* (95% CI) | ||||
| Visual deficiency | 0.11 | ||||||||
| Severe and moderate VA <3.2/10 | 13/2425 0.50 (0.2–1.0) 1 | – 0.6 (0.2–1.0) 1 | 0/152 0 0 | – 0 0 | 0/20 0 0 | – 0 0 | |||
| Mild VA 3.2/10–4/10 | 121/2425 5.1 (4.0–6.4) 1 | – 5.6 (4.3–6.8) 1 | 12/152 7.7 (4.0–13.1) 1.5 (0.7–3.1) | – 9.2 (5.0–13.4) 1.7 (0.9–3.2) | 2/20 10.6 (1.4–32.5) 1.7 (0.3–9.1) | – 15.4 (1.6–29.2) 2.5 (0.7–9.7) | |||
| None | |||||||||
| 5/10–6.3/10 | 842/2425 33.3 (30.8–35.9) 1 | – 34.4 (32.0–36.8) 1 | 59/152 39.3 (31.4–47.5) 1.2 (0.8–1.8) | – 40.6 (33.5–47.8) 1.3 (0.9–1.9) | 8/20 39.4 (18.6–63.4) 0.7 (0.3–2.1) | – 41.2 (23.5–59.0) 1.2 (0.5–3.1) | |||
| 8/10 | 559/2425 24.1 (21.8–26.5) 1 | – 23.6 (21.4–25.8) 1 | 35/152 22.8 (16.4–30.3) 1.2 (0.7–1.9) | – 21.6 (15.5–27.6) 1.2 (0.7–1.8) | 3/20 15.2 (3.3–38.1) 0.6 (0.2–2.3) | – 16.2 (3.1–29.2) 0.9 (0.3–2.7) | |||
| 10/10 | 890/2425 37.0 (34.4–39.6) 1 | – 35.8 (33.3–38.3) 1 | 46/152 30.3 (23.1–38.3) 1 | – 27.7 (21.1–34.2) 1 | 7/20 34.8 (15.3–59.1) 1 | – 24.0 (9.2–38.6) 1 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chapron, T.; Pierrat, V.; Caputo, G.; Letouzey, M.; Kermorvant-Duchemin, E.; Abdelmassih, Y.; Beaumont, W.; Barjol, A.; Le Meur, G.; Benhamou, V.; et al. Ophthalmological Impairments at Five and a Half Years after Preterm Birth: EPIPAGE-2 Cohort Study. J. Clin. Med. 2022, 11, 2139. https://doi.org/10.3390/jcm11082139
Chapron T, Pierrat V, Caputo G, Letouzey M, Kermorvant-Duchemin E, Abdelmassih Y, Beaumont W, Barjol A, Le Meur G, Benhamou V, et al. Ophthalmological Impairments at Five and a Half Years after Preterm Birth: EPIPAGE-2 Cohort Study. Journal of Clinical Medicine. 2022; 11(8):2139. https://doi.org/10.3390/jcm11082139
Chicago/Turabian StyleChapron, Thibaut, Véronique Pierrat, Georges Caputo, Mathilde Letouzey, Elsa Kermorvant-Duchemin, Youssef Abdelmassih, William Beaumont, Amandine Barjol, Guylene Le Meur, Valérie Benhamou, and et al. 2022. "Ophthalmological Impairments at Five and a Half Years after Preterm Birth: EPIPAGE-2 Cohort Study" Journal of Clinical Medicine 11, no. 8: 2139. https://doi.org/10.3390/jcm11082139
APA StyleChapron, T., Pierrat, V., Caputo, G., Letouzey, M., Kermorvant-Duchemin, E., Abdelmassih, Y., Beaumont, W., Barjol, A., Le Meur, G., Benhamou, V., Marchand-Martin, L., Ancel, P.-Y., & Torchin, H. (2022). Ophthalmological Impairments at Five and a Half Years after Preterm Birth: EPIPAGE-2 Cohort Study. Journal of Clinical Medicine, 11(8), 2139. https://doi.org/10.3390/jcm11082139






