Implementation of Online Behavior Modification Techniques in the Management of Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
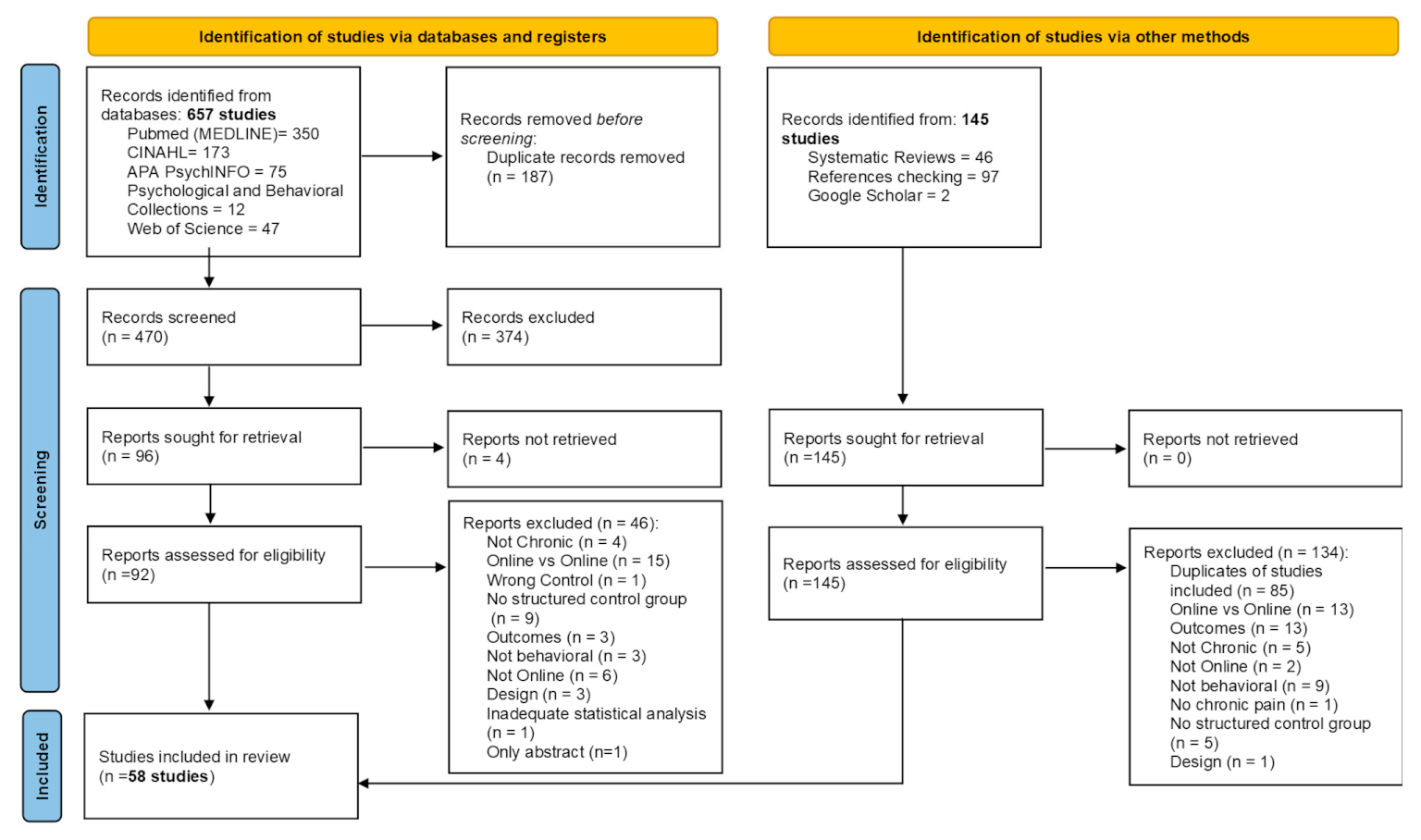
2. Materials and Methods
2.1. Inclusion Criteria
2.1.1. Population
2.1.2. Intervention and Control
2.1.3. Outcomes
2.1.4. Study Design
2.2. Search Strategy
2.3. Selection Criteria and Data Extraction
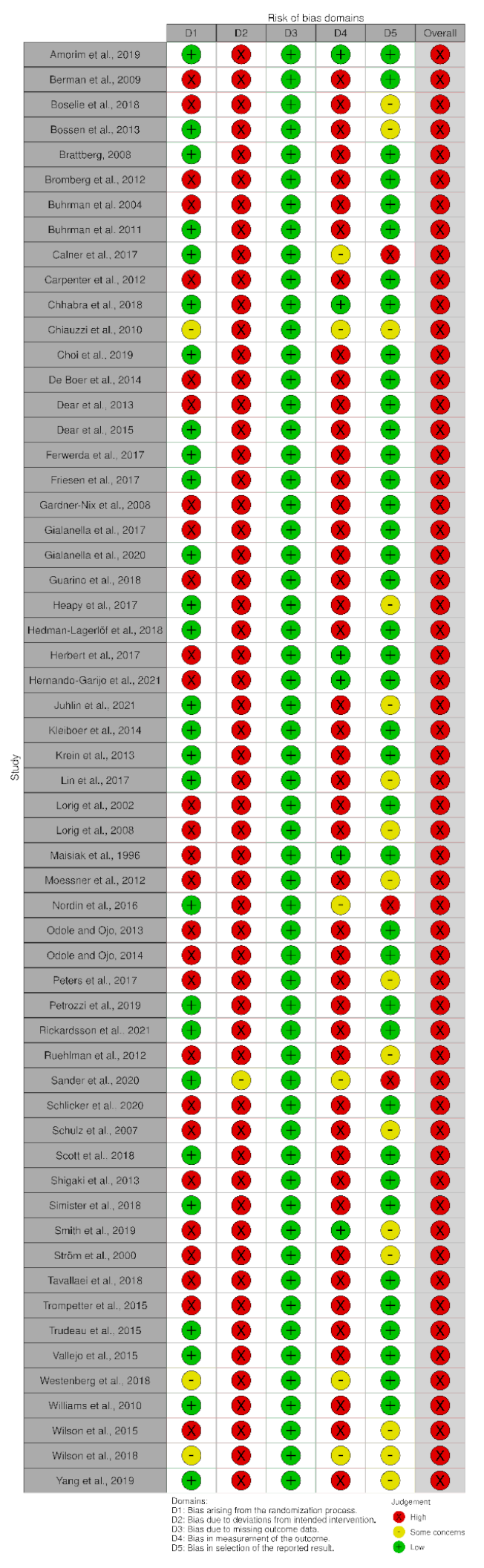
2.4. Risk of Bias and Methodological Quality Assessment
2.5. Certainty of Evidence
2.6. Data Synthesis and Analysis
3. Results
3.1. Characteristics of the Included Studies
3.2. Methodological Quality and Risk of Bias Results
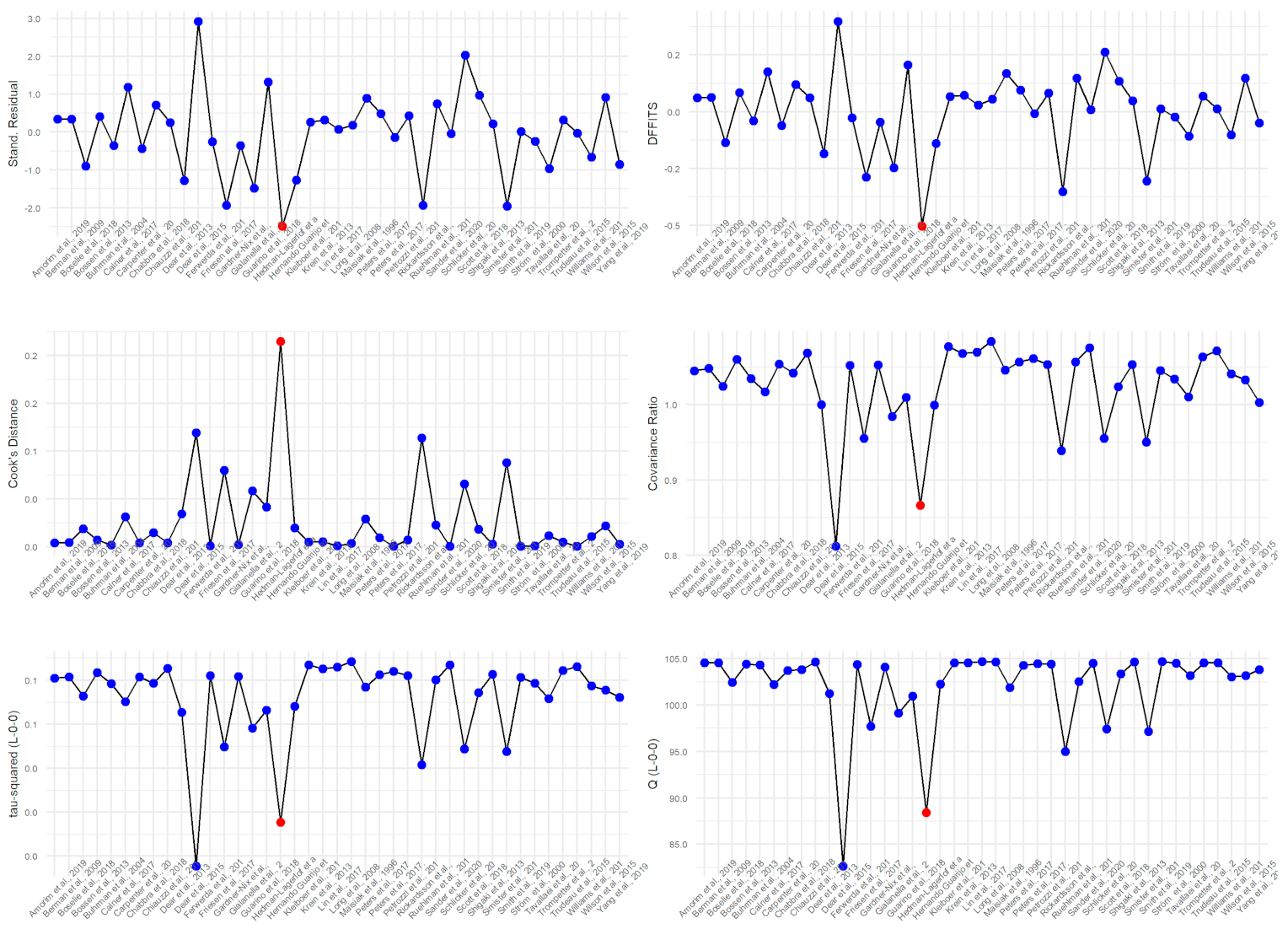
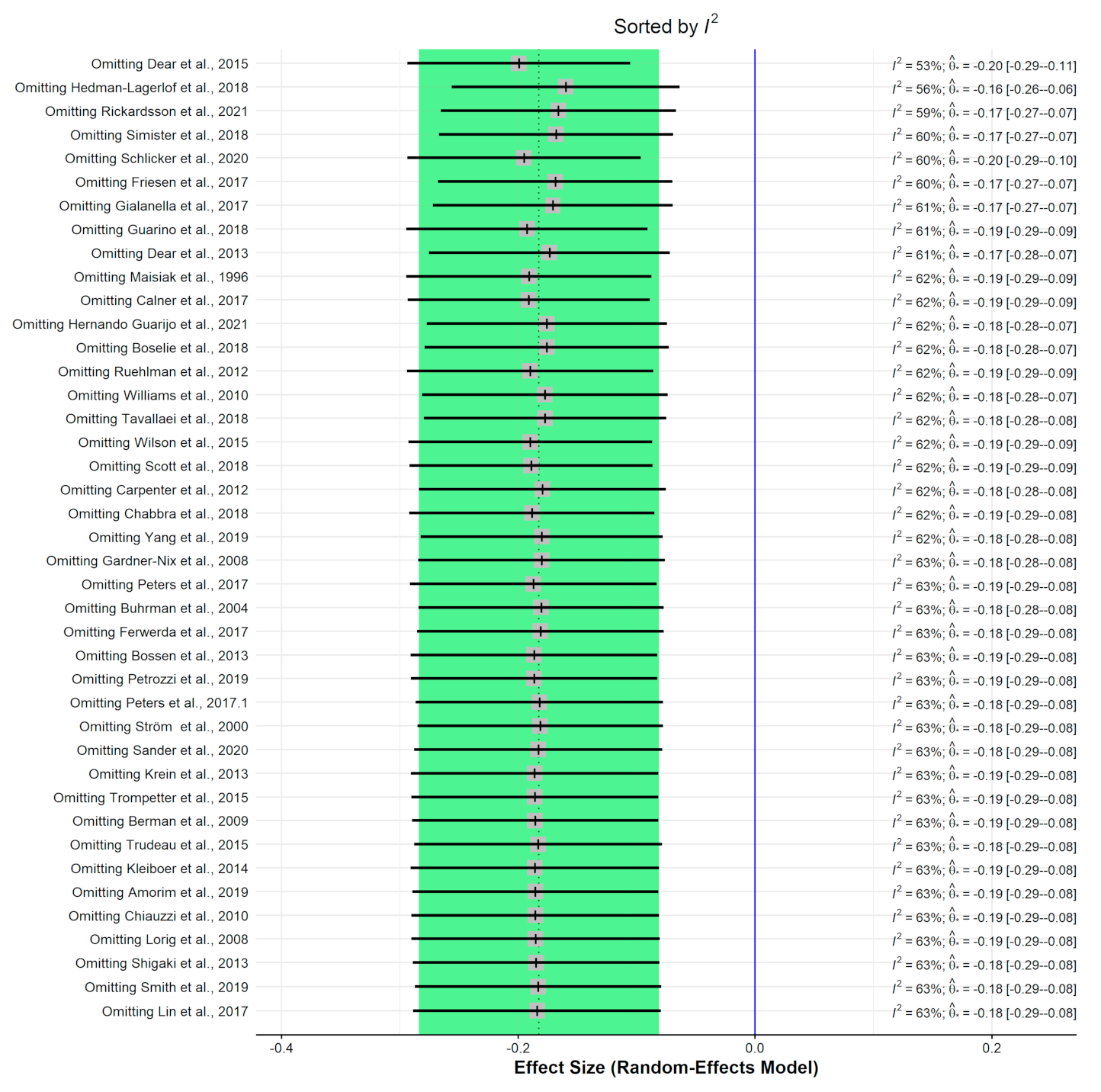
3.3. Meta-Analysis Results
3.3.1. Pain Intensity (vs. Usual Care/Waiting List)
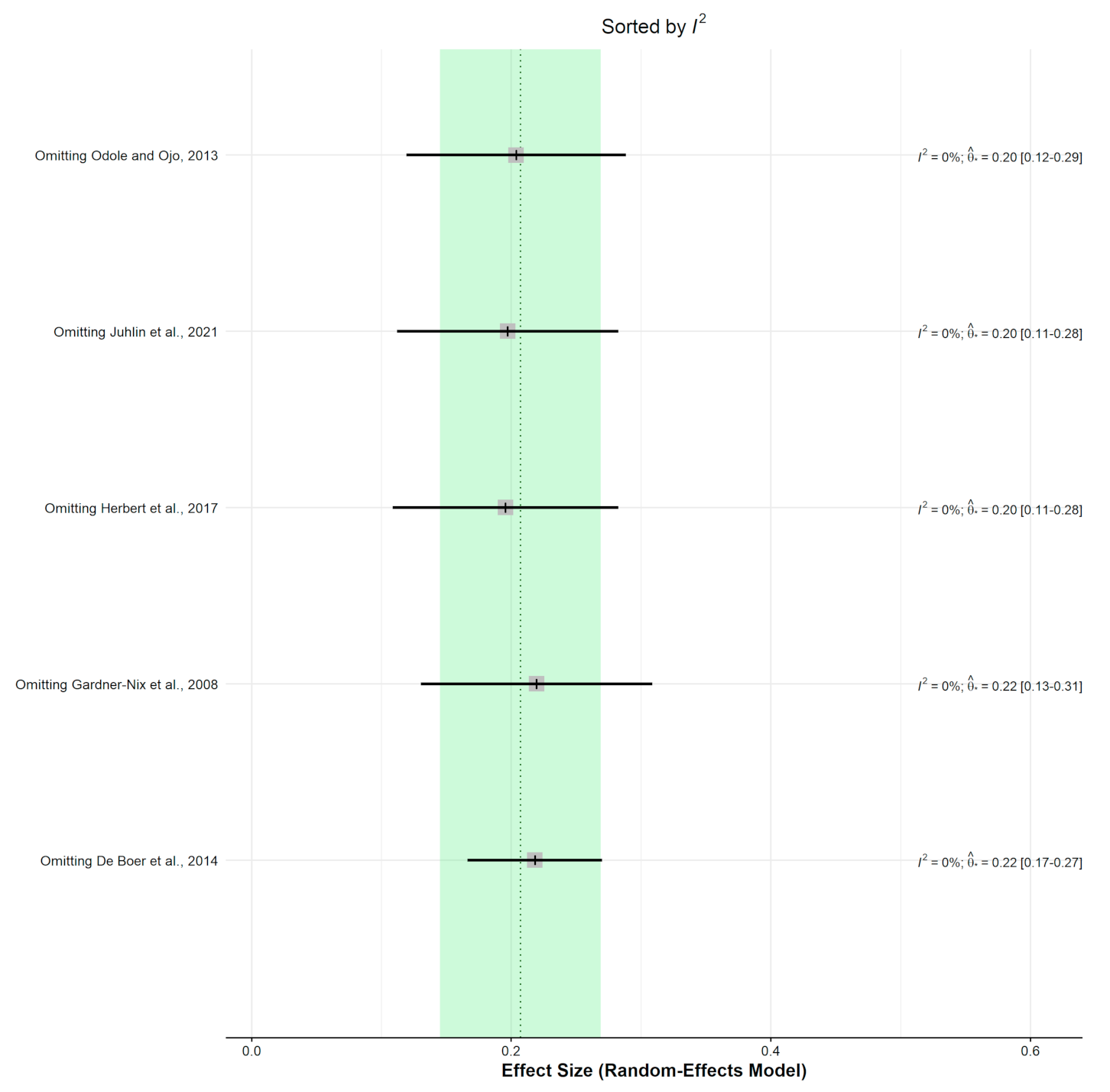
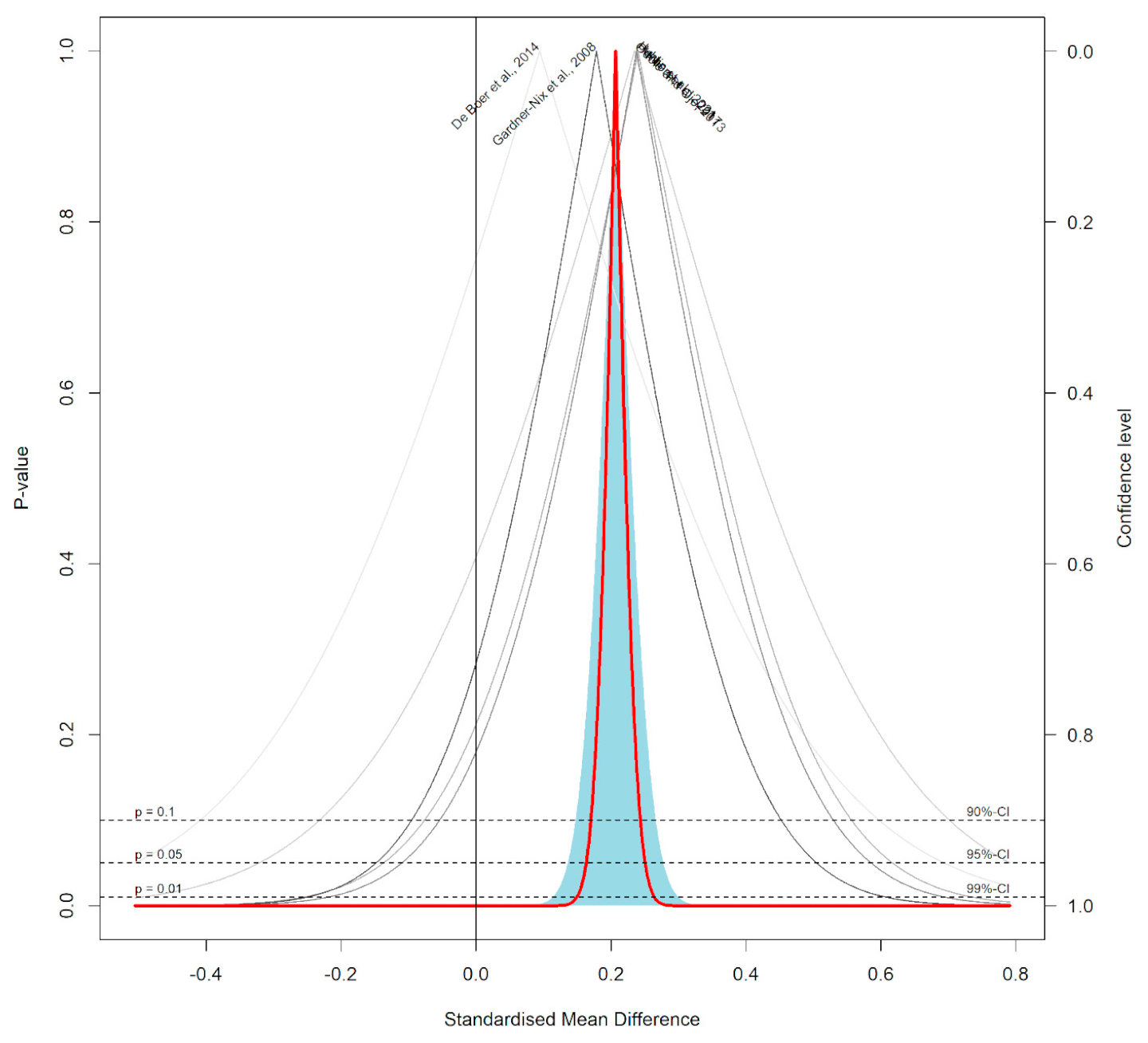
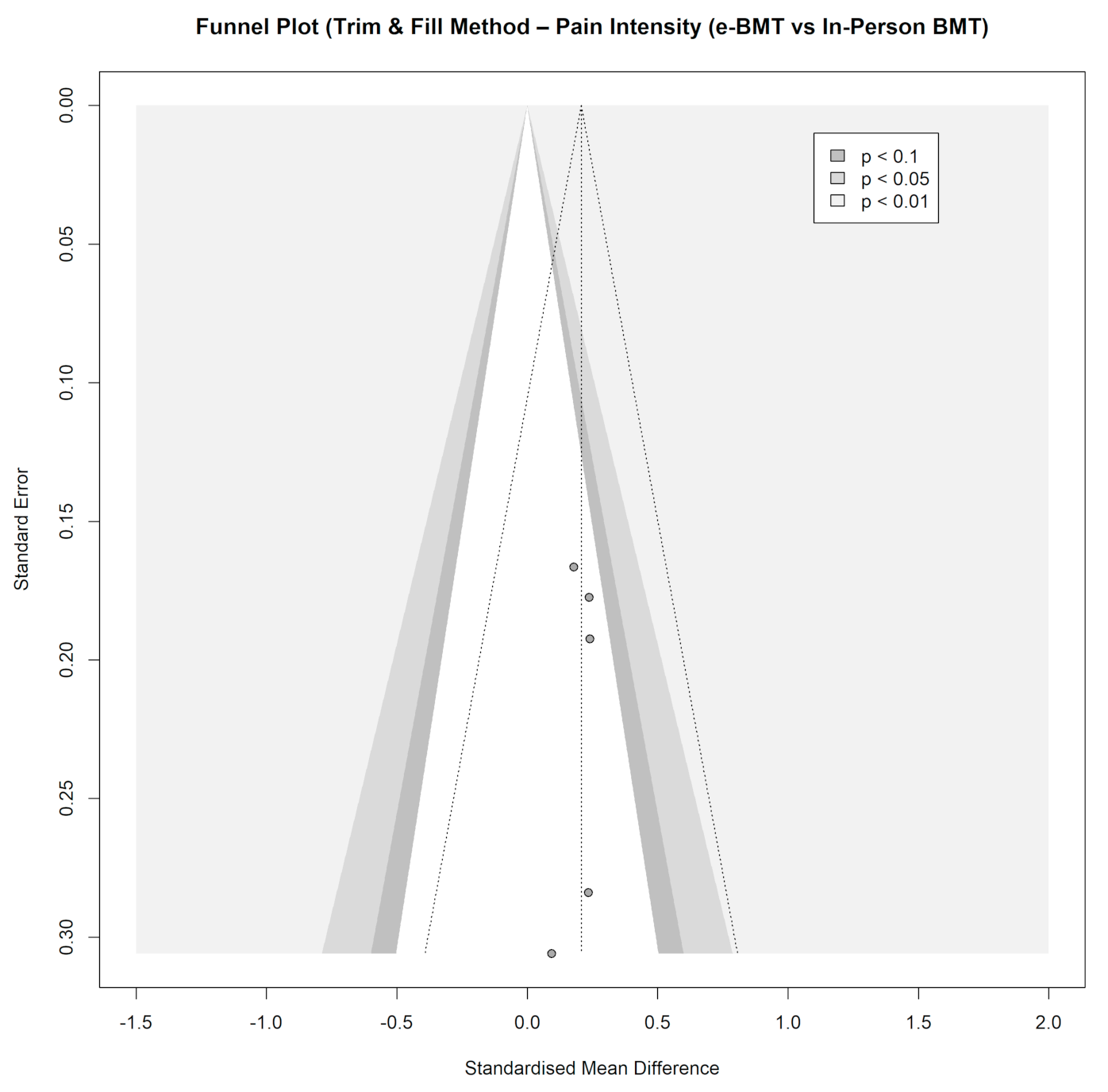
3.3.2. Pain Intensity (vs. In-Person BMT)
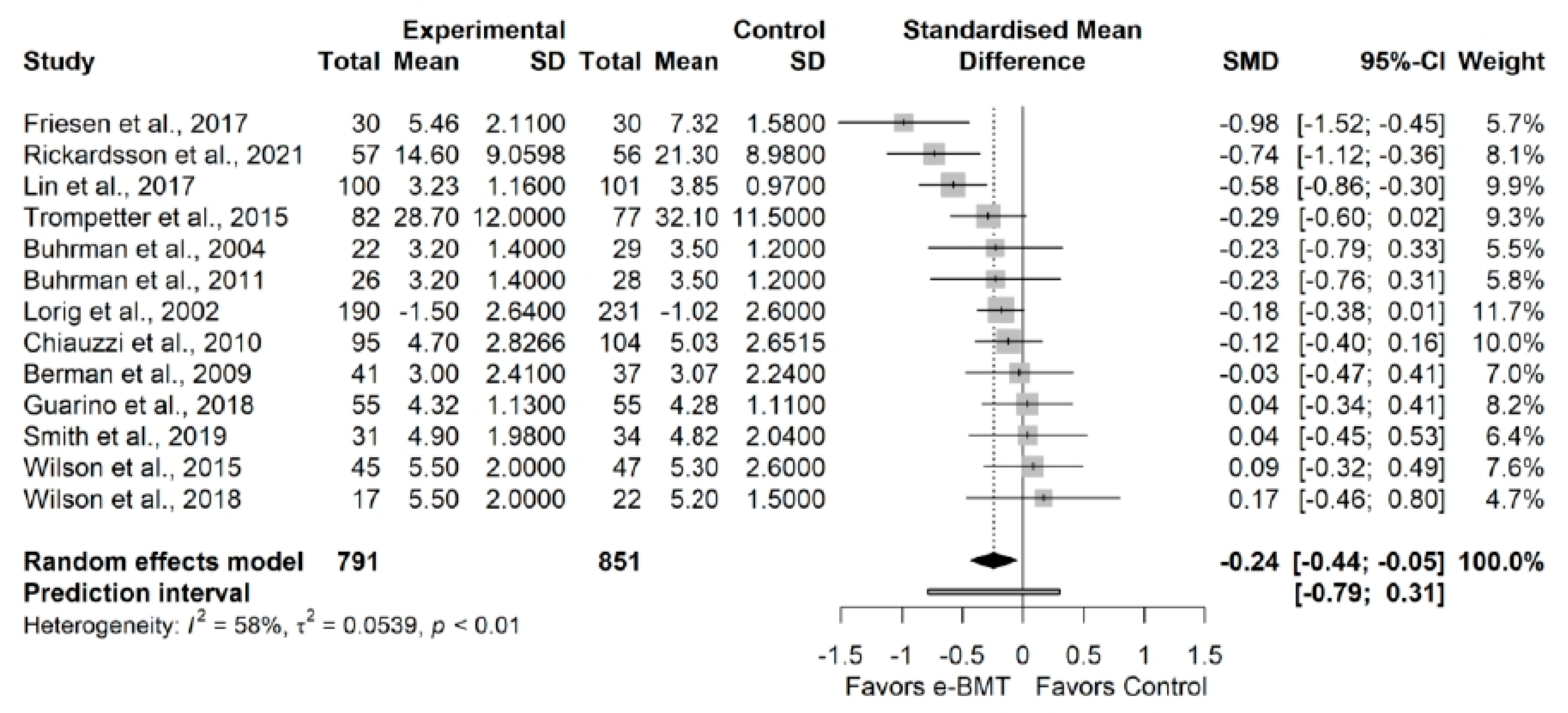
3.3.3. Pain Interference (vs. Usual Care/Waiting List)
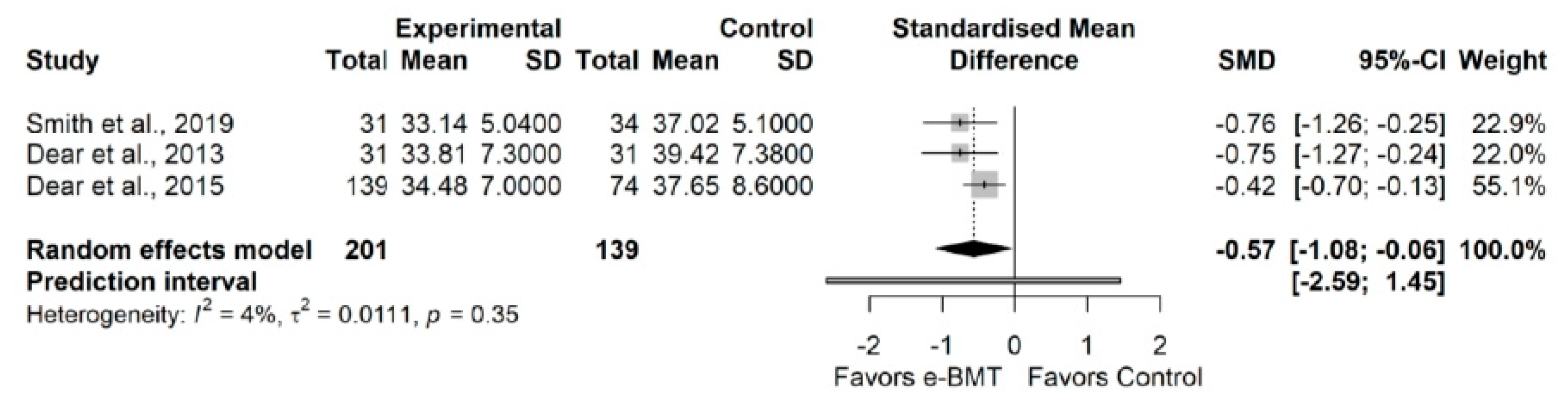
3.3.4. Kinesiophobia (vs. Usual Care/Waiting List)
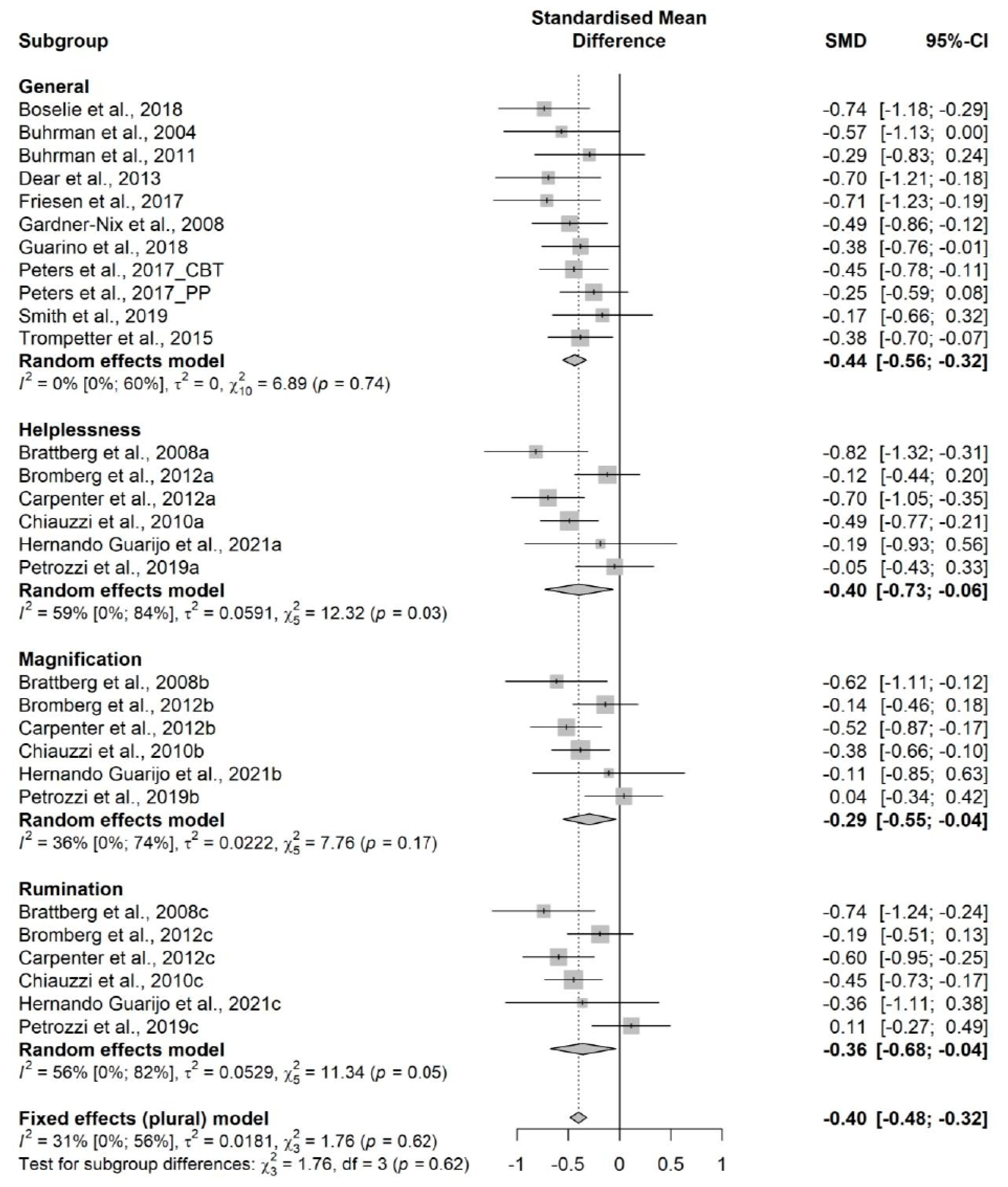
3.3.5. Catastrophizing (vs. Usual Care/Waiting List)
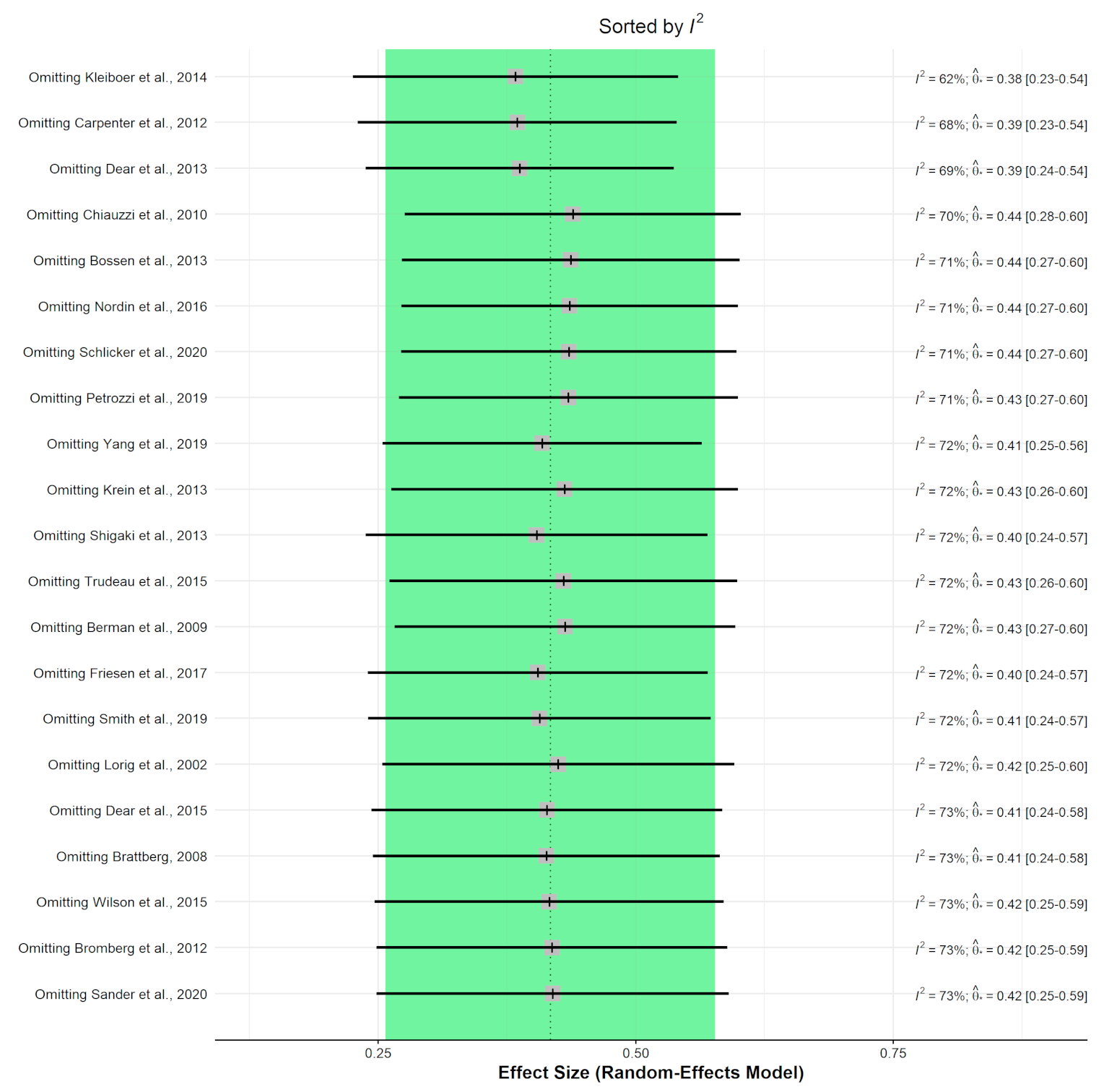
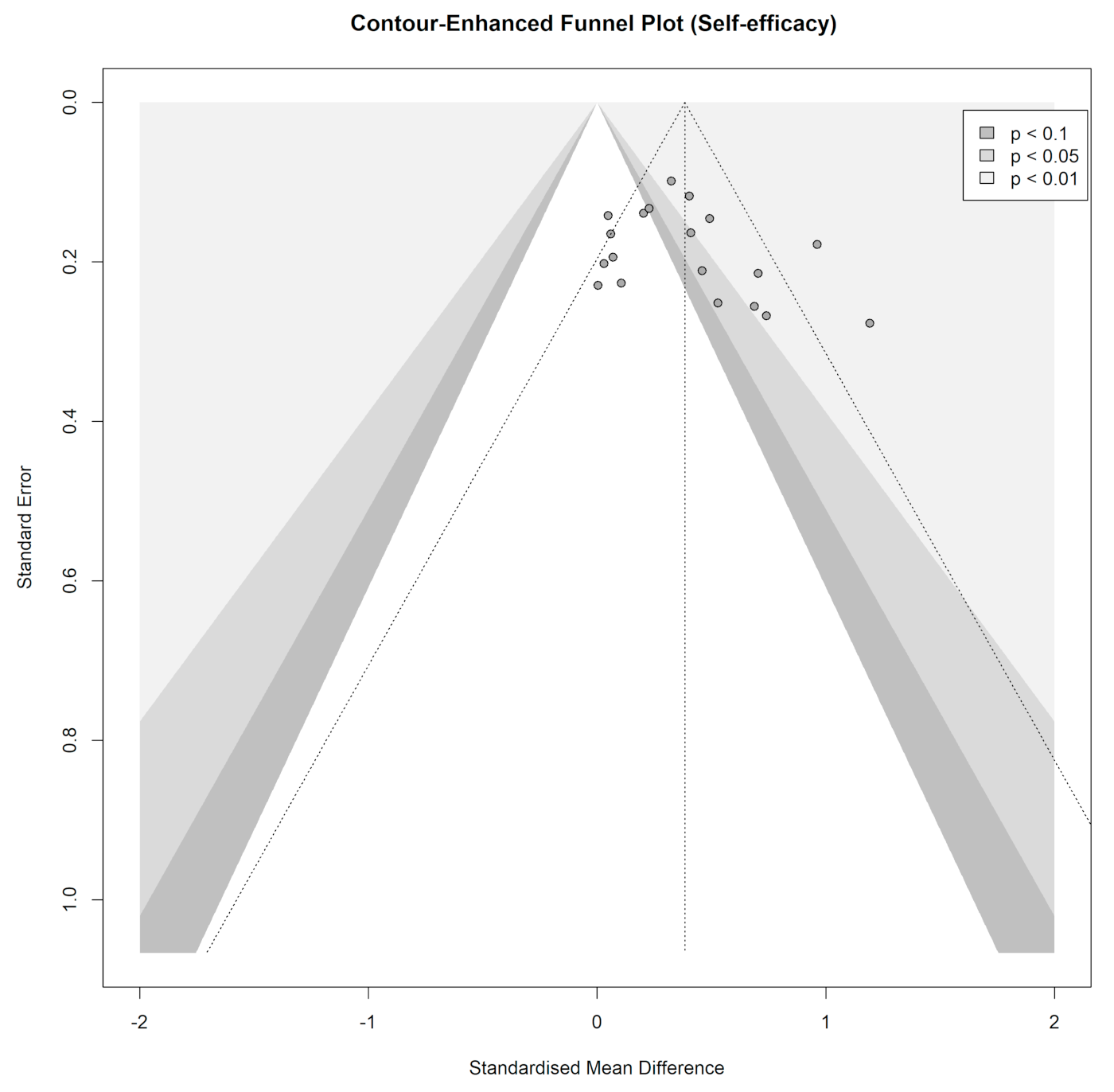
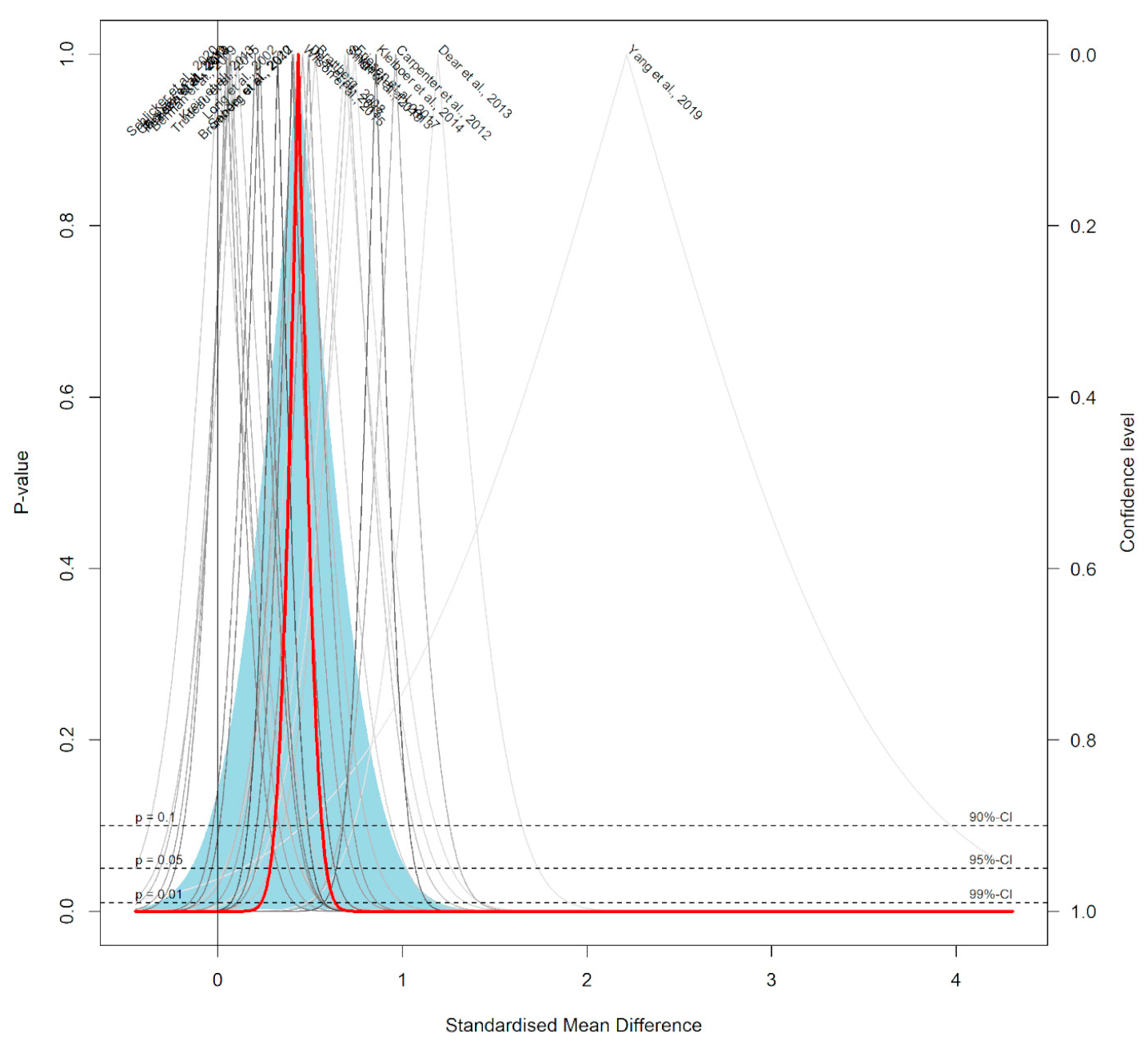
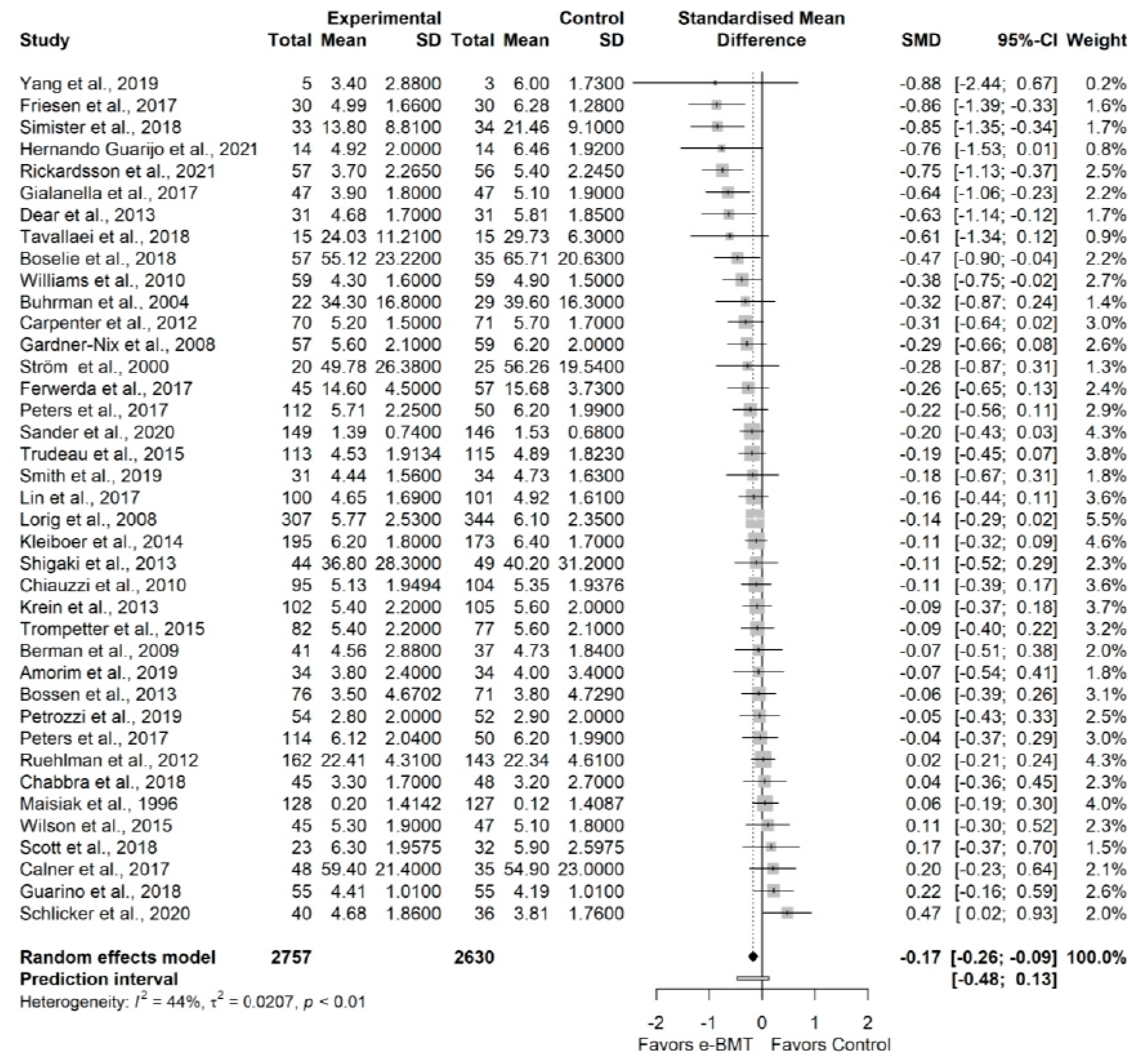
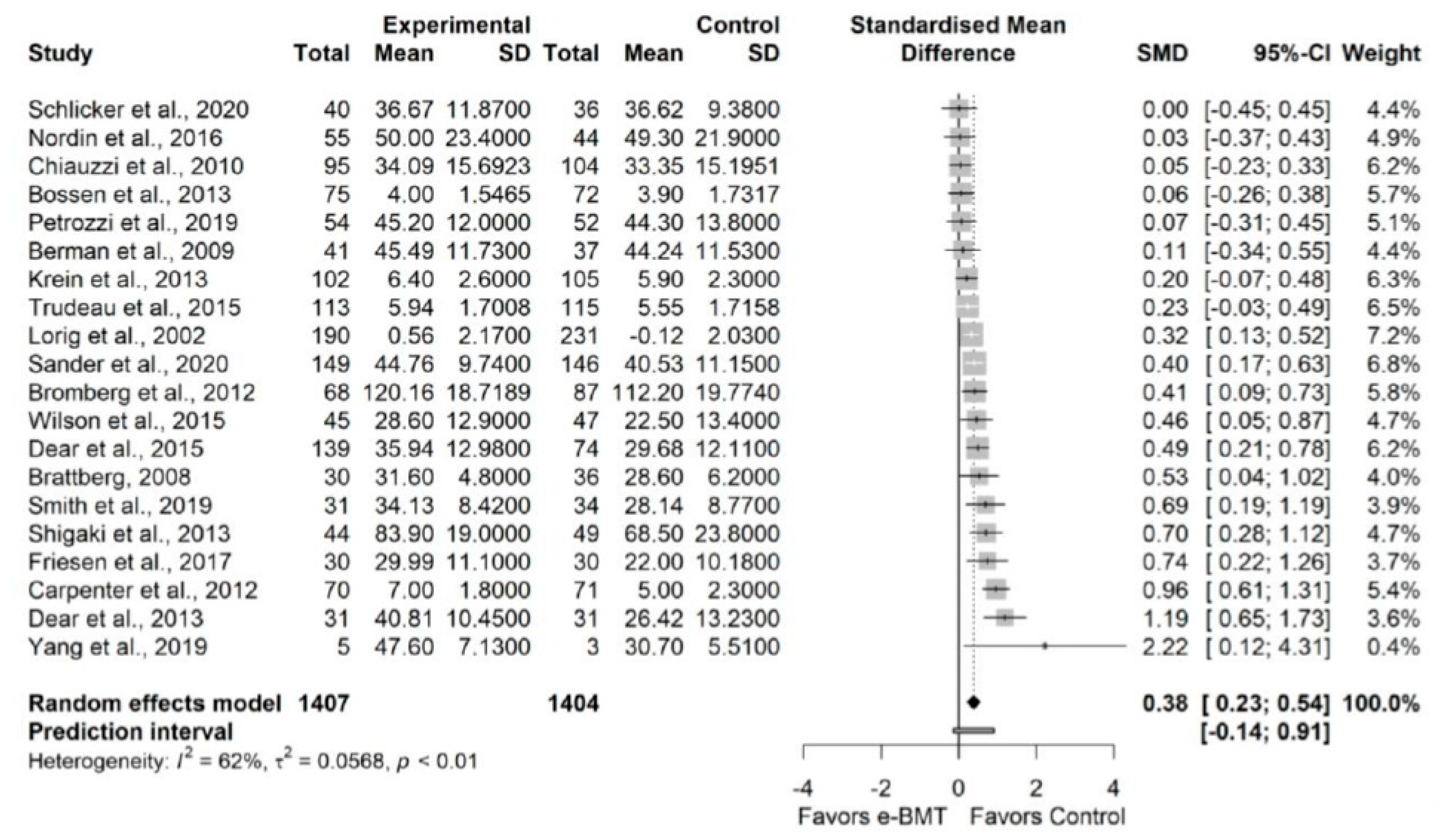
3.3.6. Self-Efficacy (vs. Usual Care/Waiting List)
4. Discussion
4.1. Practical implication
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. PRISMA 2020 Flow Diagram
Appendix B. Search Strategies in the Different Electronic Databases
Appendix C. Details of the Interventions
| Authors, Year | Intervention | Comparator | ||||
|---|---|---|---|---|---|---|
| Format Equipment and Contact Form | Modality and Content | Duration and Frequency, Follow-Up | Format Equipment | Modality and Content | Duration and Frequency, Follow-Up | |
| Amorim et al., 2019 | Mobile application Written, pedometer Telephone call, message | Physical exercise, activity tracker, lessons
| 6 months 1 face-to-face interview andROMANIA2 calls/monthROMANIAFollow-up: N/A | Recommendations Written, brief advice |
| 6 months N/A Follow-up: N/A |
| Berman et al., 2009 | Internet-basedr Images, audio | Self-care. Mind-body exercises and lessons
| 6 weeks ≥ 1 session/week Follow-up: N/A | No intervention N/A | N/A | N/A N/A Follow-up: N/A |
| Boselie et al., 2018 | Internet-based Online platform Telephone call, email | Positive psychology exercises
| 8 weeks Call: weeks 1, 3, 5,7 Email: weeks 2, 4, 6, 8 Follow-up: N/A | Waiting list N/A | N/A | N/A N/A Follow-up: N/A |
| Bossen et al., 2013 | Internet-based Written, video | Behavior graded activity and exercises
| 9 weeks ≥ 1 session/week Follow-up: 12 weeks | Waiting list N/A | N/A | N/A N/A Follow-up: 12 weeks |
| Brattberg, 2008 | Internet-based Written Telephone call, email | Self-management. Emotional Freedom Techniques Self-monitoring of outcome of behavior | 8 weeks 1 time/day Follow-up: N/A | Waiting list | N/A | N/A N/A Follow-up: N/A |
| Bromberg et al., 2012 | Internet-based +usual care Written | Behavior change, physical activity, lessons
| 6 months ≥ 2 sessions/week (first 4 weeks) ≥ 1 sessions/month (final 5 month) Follow-up: N/A | Usual care N/A |
| N/A N/A Follow-up: N/A |
| Buhrman et al., 2004 | Internet-based Slideshow, audio Telephone call | CBT. Physical and psychological exercises, relaxation
| 6 weeks 1 call/week Follow-up: 3 months | Waiting list N/A | N/A | N/A N/A Follow-up: 3 months |
| Buhrman et al., 2011 | Internet-based Written | CBT. Physical exercise, relaxation, cognitive skills
| 8 weeks N/R Follow-up: 12 weeks | Waiting list N/A | N/A | N/A N/A Follow-up: 12 weeks |
| Calner et al., 2017 and Nordin et al., 2016 | Internet-based + multimodal rehabilitation Written, video No contact | Behavior, change, lessons, homework
| 6–8 weeks Internet-based: 1 lesson/week Multimodal: 2–3 sessions/week Follow-up: 12 months | Multimodal rehabilitation N/A |
| 6–8 weeks 2–3 session/week Follow-up: 12 months |
| Carpenter et al., 2012 | Internet-based Written, images, audio | CBT and pain education. Lessons, homework, relaxation
| 3 weeks 2 lessons/week Follow-up: 6 weeks | Waiting list N/A | N/A | N/A N/A Follow-up: 6 weeks |
| Chabbra et al., 2018 | Mobile application Written N/R | Self-management—Physical exercise
| 12 weeks N/R Follow-up: N/A | Usual care Written |
| 12 weeks N/A Follow-up: N/A |
| Chiauzzi et al., 2010 | Internet-based Written | CBT and self-management. Lessons, homework
| 4 weeks 2 sessions/week Follow-up: 6 months | Recommendations Written |
| 4 weeks N/A Follow-up: 6 months |
| Choi et al., 2019 | Mobile application + NSAIDs Video, audio N/R | Physical exercise, NSAIDs
| 2 months 2–3 times/day Follow-up: 3 months | Physical exercise, NSAIDs Images | Exercise
| 2 months 2–3 times/day Follow-up: 3 months |
| De Boer et al., 2014 | Internet-based Multimedia applications Telephone call, email | CBT. Lessons, homework and relaxation
| 7 weeks 1 session/week Email: after modules 2, 4, 7, 8 Follow-up: 2 months | Face-to-face Book |
| 7 weeks 1 session/week Follow-up: 2 months |
| Dear et al., 2013 | Internet-based Written Telephone call | CBT. Lessons, homework
| 8 weeks 1 lesson/7–10 days 1 call/week Follow-up: 3 months | Waiting list N/A | N/A | N/A N/A Follow-up: 3 months |
| Dear et al., 2015 | Internet-based
Telephone call, email | CBT. Lessons, homework
| 8 weeks 1 lesson/7–10 days G1: 1 call/week G2: as-needed calls G3: no contact Follow-up: 3 months | Waiting list N/A | N/A | N/A N/A Follow-up: 3 months |
| Ferwerda et al., 2017 | Internet-based Written | CBT. Lessons, homework
| 17 to 32 weeks 1 email/1–2 weeks Follow-up: 12 months | Usual care N/R |
| N/R N/R Follow-up: 12 months |
| Friesen et al., 2017 | Internet-based Slideshow Telephone call, email | CBT. Lessons, homework
| 8 weeks 1 email and call/week Follow-up: N/A | Waiting list N/A | N/A | N/A N/A Follow up: N/A |
| Gardner-Nix et al., 2008 | Videoconferencing N/R N/R | Mindfulness lessons
| 10 weeks 2 h/week Follow-up: N/A | G1: Face-to-face N/R G2: Waiting list N/A |
| G1: 10 weeks 2 h/week G2: N/A Follow-up: N/A |
| Gialanella et al., 2017 and 2020 | Telephone call Written, images Telephone call | Physical exercise
| 6 months ≥2 calls/month Follow-up: 12 months | Physical exercise + recommendations N/R |
| 6 months N/A Follow-up: 12 months |
| Guarino et al., 2018 | Internet-based + usual care Written, images, audio Telephone call, email | CBT. Lessons, relaxation
| 12 weeks 2 lessons/week Follow-up: 3 months | Usual care N/A |
| 12 weeks N/A Follow-up: 3 months |
| Heapy et al., 2017 | Interactive voice response Written, images, audio, pedometer Telephone call | CTB. Lessons, relaxation
| 10 weeks 1 call/day Follow-up: 9 months | Face-to-face Written, images, audio, pedometer | CBT. Lessons, relaxation
| 10 weeks 1 session/week Follow-up: 9 months |
| Hedman-Lagerlöf et al., 2018 | Internet-based Written Telephone call, message | Lessons, homework, mindfulness
| 10 weeks 1–3 contacts/week Follow-up: 12 months | Waiting list N/A | N/A | N/A N/A Follow-up: 12 months |
| Herbert et al., 2017 | Videoconferencing Written N/R | ACT. Mindfulness, lessons
| 8 weeks 1 session/week Follow-up: 6 months | Face-to-face Written | ACT. Mindfulness, lessons
| 8 weeks 1 session/week Follow-up: 6 months |
| Hernando-Garijo et al., 2021 | Videoconferencing + usual care Video Video call | Aerobic exercise
| 15 weeks 2 session/week Follow-up: N/A | Usual care N/A |
| 15 weeks N/A Follow-up: NA |
| Juhlin et al., 2021 | Internet-based Digital platform Message | Person-centered intervention. Physical and psychological exercises
| 6 months 1 contact/week Follow-up: N/A | Face-to-face (1 session) N/A |
| 6 months N/A Follow-up: N/A |
| Kleiboer et al., 2014 | Internet-based Written, audio, video | Behavioral training. Exercises, lessons, homework, relaxation
| 3.6 months on average 8 lessons, 1 lesson/7–10 days Follow-up: N/A | Waiting list N/A | N/A | N/A N/A Follow-up: N/A |
| Krein et al., 2013 | Internet-based + pedometer Written, imagen, digital platform Message, discussion group | E-community. Step-count, lessons
| N/R 1 upload data/week Follow-up: 12 month | Pedometer N/A |
| N/R 1 upload data/month Follow-up: 12 month |
| Lin et al., 2017 | Internet-based Written, audio, video Email, message | ACT. Lessons, mindfulness
| 9 weeks 1 session/week Follow-up: 6 months | Waiting list N/A | N/A | N/A N/A Follow-up: 6 months |
| Lorig et al., 2002 | Internet-based Written, video Email discussion group | E-community. Physical exercises, lessons
| 6 weeks Frequency determined by user interactions Follow-up: 12 months | Usual care N/A |
| 6 weeks N/A Follow-up: 12 months |
| Lorig et al., 2008 | Internet-based Written Email, internet chat | Self-management. Physical exercise, lessons, relaxation
| 6 weeks ≥3 sessions/week Follow-up: 12 months | Usual care N/A |
| 6 weeks N/A Follow-up: 12 months |
| Maisiak et al., 1996 | Telephone call Written Telephone call, email | Counseling strategy
| 9 months 2 contact/month (first 3 months) 1 contact/month (final 6 months) Follow-up: N/A | Usual care N/A |
| 9 months N/A Follow-up: N/A |
| Moessner et al., 2012 | Internet-based N/R Internet guided chat | Self-monitoring. Lessons
| 12–15 weeks 1 session/week Follow-up: 6 months | Usual care N/A | N/R | 12–15 weeks 1 session/week Follow-up: 6 months |
| Odole and Ojo, 2013 and 2014 | Telephone call N/R Telephone call | Physical therapy: exercises
| 6 weeks 3 calls/week Follow-up: N/A | Face-to-face N/A |
| 6 weeks 3 sessions/week Follow-up: N/A |
| Peters et al., 2017 | Internet-based Written Telephone call, email | G1: Positive psychology. Psychological exercises
| 8 weeks 1 lesson/week Call: weeks 1, 3, 5, 7 Email: weeks: 2, 4, 6, 8 Follow-up: 6 months | Waiting list N/A | N/A | N/A N/A Follow-up: 6 months |
| Petrozzi et al., 2019 | Internet-based + usual care Written Telephone call | CBT. Lessons, homework
| 8 weeks 1 lesson/week 1 call/week Follow-up: 12 months | Usual care N/A |
| 8 weeks 12 sessions (variable frequency) Follow-up: 12 months |
| Rickardsson et al., 2021 | Internet-based Written, image, audio Telephone call, message | ACT. Lessons
| 8 weeks 7 sessions/week ≥2 messages/week Follow-up: 12 months | Waiting list N/A |
| N/A N/A Follow-up: 12 months |
| Ruehlman et al., 2012 | Internet-based Written, image Email, message | Self-management + e-community. Physical exercise, lessons, homework, relaxation
| 6 weeks N/R Follow-up: 14 weeks | Usual care N/A | N/R | 6 weeks N/A Follow-up: 14 weeks |
| Sander et al., 2020 | Internet-based + usual care Written, audio, video Telephone call, email, message | CBT. Lessons, homework, relaxation
| 9 weeks 7 sessions/week Follow-up: 12 months | Usual care N/A |
| 9 weeks N/R Follow-up: 12 months |
| Schlickler et al., 2020 | Internet-based + mobile-based N/R Email, message | CBT. Lessons, mindfulness, relaxation
| 9 weeks 7 lessons/week Follow-up: 6 months | Waiting list N/A | N/A | N/A N/A Follow-up: 6 months |
| Schulz et al., 2007 | Internet-based Multimedia materials Email, forum | Physical exercise, lessons, homework
| 5 months N/R Follow-up: N/A | No treatment N/A | N/A | N/A N/A Follow-up: N/A |
| Scott et al., 2018 | Internet-based + usual care Video Telephone call, email | ACT. Lessons
| 5 weeks 2 lesson/week (first 3 weeks), 1 lesson/week (final 2 weeks) Follow-up: 9 months | Usual care N/A |
| 5 weeks N/A Follow-up: 9 months |
| Shigaki et al., 2013 | Internet-based Slideshow Telephone call, message, online chat | Lessons, homework
| 10 weeks 1 lesson/week 1 call/week Follow-up: N/A | Waiting list | N/A | N/A N/A Follow-up: N/A |
| Simister al., 2018 | Internet-based + usual care Written, audio, video | ACT. Lessons, homework
| 8 weeks N/R Follow-up: 3 months | Usual care N/A |
| 8 weeks N/A Follow-up: 3 months |
| Smith et al., 2019 | Internet-based Written, image, audio, video Telephone call, email | CBT and self-management. Multidisciplinary program with physical exercise, lessons, homework, relaxation
Physical therapy, psychologist | 4 months 2 lessons/month Follow-up: 7 months | Usual care N/A |
| 4 months N/A Follow-up: 7 months |
| Ström et al., 2000 | Internet-based Written | Lessons, relaxation
| 6 weeks 1 lesson/week Follow-up: N/A | Waiting list N/A | N/A | N/A N/A Follow-up: N/A |
| Tavallaei et al., 2018 | Internet-based Written N/R | Mindfulness-based stress reduction bibliotherapy
| 8 weeks 1 lesson/week Follow-up: N/A | Usual care N/A |
| 8 weeks N/A Follow-up: N/A |
| Trompetter et al., 2015 | Internet-based Written | ACT. Lessons, mindfulness
| 3 months ≥ 3 h/week Follow-up: 6 months | Waiting list N/A | N/A | N/A N/A Follow-up: 6 months |
| Trudeau et al., 2015 | Internet-based Multimedia materials Telephone call, email | Self-management. Lessons
| 6 months ≥2 sessions/week (1 month) 1 session/month (5 months) Follow-up: N/A | Waiting list N/A | N/A | N/A N/A Follow-up: N/A |
| Vallejo et al., 2015 | Internet-based + usual care Written, images, audio Message | CBT. Lessons, homework, relaxation
| 10 weeks 1 session/week Follow-up: 12 months | G1: Face-to-face + usual care Written, images, audio G2: Usual care N/A | G1: CBT. Lessons, homework, relaxation
| 10 weeks G1: 1 session/week G2: N/A Follow-up (only G1): 12 months |
| Westenberg et al., 2018 | Internet-based Written, video N/R | Mindfulness
| 60-s video N/R Follow-up: N/A | Attention control Written |
| 60-s read N/R Follow-up: N/A |
| Williams et al., 2010 | Internet-based + usual care Written, audio, video No contact | Self-management. Lessons, homework, relaxation
| 6 months N/R Follow-up: N/A | Usual care |
| 6 months N/A Follow-up: N/A |
| Wilson et al., 2015 | Internet-based N/R N/R | Self-management. Lessons, exercises, relaxation
| 8 weeks N/R Follow-up: N/A | Usual care N/A | N/A | 8 weeks N/R Follow-up: N/A |
| Wilson et al., 2018 | Internet-based Written Interactive activity | Self-management. Lessons, homework
| 8 weeks N/R Follow-up: N/A | Waiting list Written |
| 8 weeks 1 email/week Follow-up: N/A |
| Yang et al., 2019 | Mobile application + face-to-face N/R | Self-management. Physical exercise
| 4 weeks Exercises: 4 times/week Physiotherapy: N/R Follow-up: N/A | Face-to-face N/A |
| 4 weeks N/R Follow-up: N/A |
Appendix D. Assessment of the Studies Quality Based on PEDro Scale
| Items | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Articles | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total |
| Amorim et al., 2019 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 7 | |
| Berman et al., 2009 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 | |
| Boselie et al., 2018 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 | |
| Bossen et al., 2013 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 6 | |
| Brattberg, 2008 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | |
| Bromberg et al., 2012 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 | |
| Buhrman et al., 2004 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 | |
| Buhrman et al., 2011 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | |
| Calner et al., 2017 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 5 | |
| Carpenter et al., 2012 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 | |
| Chhabra et al., 2018 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 | |
| Chiauzzi et al., 2010 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 | |
| Choi et al., 2019 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | |
| De Boer et al., 2014 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 | |
| Dear et al., 2013 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 | |
| Dear et al., 2015 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 | |
| Ferwerda et al., 2017 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | |
| Friesen et al., 2017 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 | |
| Gardner-Nix et al., 2008 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 | |
| Gialanella et al., 2017 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 | |
| Gialanella et al., 2020 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 | |
| Guarino et al., 2018 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 | |
| Heapy et al., 2017 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 6 | |
| Hedman-Lagerlöf et al., 2018 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 | |
| Herbert et al., 2017 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7 | |
| Hernando-Garijo et al., 2021 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7 | |
| Juhlin et al., 2021 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 6 | |
| Kleiboer et al., 2014 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | |
| Krein et al., 2013 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | |
| Lin et al., 2017 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 6 | |
| Lorig et al., 2002 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 | |
| Lorig et al., 2008 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 | |
| Maisiak et al., 1996 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6 | |
| Moessner et al., 2012 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 | |
| Nordin et al., 2016 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | |
| Odole and Ojo, 2013 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 | |
| Odole and Ojo, 2014 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 | |
| Peters et al., 2017 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 | |
| Petrozzi et al., 2019 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | |
| Rickardsson et al., 2021 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | |
| Ruehlman et al., 2012 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 | |
| Sander et al., 2020 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 7 | |
| Schlicker et al., 2020 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 | |
| Schulz et al., 2007 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 | |
| Scott et al., 2018 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | |
| Shigaki et al., 2013 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4 | |
| Simister et al., 2018 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | |
| Smith et al., 2019 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 6 | |
| Ström et al., 2000 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 | |
| Tavallaei et al., 2018 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4 | |
| Trompetter et al., 2015 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 | |
| Trudeau et al., 2015 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | |
| Vallejo et al., 2015 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 | |
| Westenberg et al., 2018 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | |
| Williams et al., 2010 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | |
| Wilson et al., 2015 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 | |
| Wilson et al., 2018 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 | |
| Yang et al., 2019 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 6 | |
Appendix E. Risk of Bias Summary according to the ROB2 Scale

Appendix F. Statistical Exploration of Heterogeneity, Outliers, Robustness and Publication Bias for the Pain Intensity Variable


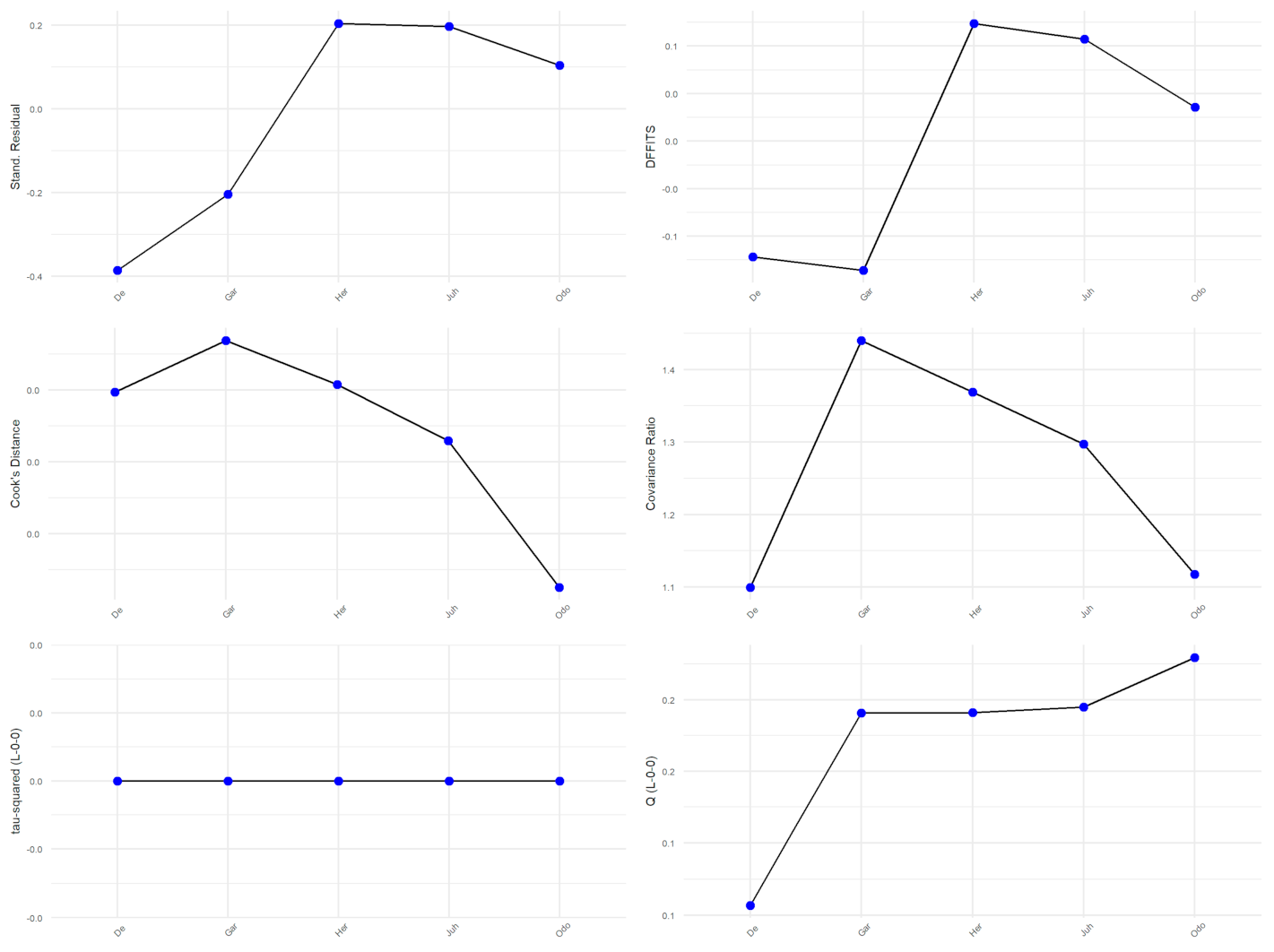
Appendix G. Statistical Exploration of Heterogeneity, Outliers, Robustness and Publication Bias for the Pain Intensity Variable (e-BMT vs. In-Person BMT)


Appendix H. Statistical Exploration of Heterogeneity, Outliers, Robustness and Publication Bias for the Pain Interference Variable


Appendix I. Statistical Exploration of Heterogeneity, Outliers, Robustness and Publication Bias for the Kinesiophobia Variable


Appendix J. Statistical Exploration of Heterogeneity, Outliers, Robustness and Publication Bias for the Catastrophizing Variable






Appendix K. Statistical Exploration of Heterogeneity, Outliers, Robustness and Publication Bias for the Self-Efficacy





References
- Wade, D.T. Rehabilitation after COVID-19: An evidence-based approach. Clin. Med. 2020, 20, 359. [Google Scholar] [CrossRef] [PubMed]
- Mechanic, O.J.; Persaud, Y.; Kimball, A.B. Telehealth Systems. In Treasure Island; StatPearls Publishing LLC: Treasure Island, FL, USA, 2021. [Google Scholar]
- Mead, N.; Bower, P. Patient-centredness: A conceptual framework and review of the empirical literature. Soc. Sci. Med. 2000, 51, 1087–1110. [Google Scholar] [CrossRef]
- Pear, J.J.; Martin, G.L. Behavior Modification, Behavior Therapy, Applied Behavior Analysis and Learning. In Encyclopedia of the Sciences of Learning; Seel, N.M., Ed.; Springer: Boston, MA, USA, 2012. [Google Scholar] [CrossRef]
- Moyer, R.; Ikert, K.; Long, K.; Marsh, J. The Value of Preoperative Exercise and Education for Patients Undergoing Total Hip and Knee Arthroplasty: A Systematic Review and Meta-Analysis. JBJS Rev. 2017, 5, e2. [Google Scholar] [CrossRef] [PubMed]
- Bunzli, S.; Gillham, D.; Esterman, A. Physiotherapy-provided operant conditioning in the management of low back pain disability: A systematic review. Physiother. Res. Int. 2011, 16, 4–19. [Google Scholar] [CrossRef]
- Willett, M.; Duda, J.; Fenton, S.; Gautrey, C.; Greig, C.; Rushton, A. Effectiveness of behaviour change techniques in physiotherapy interventions to promote physical activity adherence in lower limb osteoarthritis patients: A systematic review. PLoS ONE 2019, 14, e0219482. [Google Scholar] [CrossRef]
- Meade, L.B.; Bearne, L.M.; Sweeney, L.H.; Alageel, S.H.; Godfrey, E.L. Behaviour change techniques associated with adherence to prescribed exercise in patients with persistent musculoskeletal pain: Systematic review. Br. J. Health Psychol. 2019, 24, 10–30. [Google Scholar] [CrossRef]
- Marley, J.; Tully, M.A.; Porter-Armstrong, A.; Bunting, B.; O’Hanlon, J.; Atkins, L.; Howes, S.; McDonough, S.M. The effectiveness of interventions aimed at increasing physical activity in adults with persistent musculoskeletal pain: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2017, 18, 482. [Google Scholar] [CrossRef] [Green Version]
- Button, K.; Roos, P.E.; Spasić, I.; Adamson, P.; van Deursen, R.W.M. The clinical effectiveness of self-care interventions with an exercise component to manage knee conditions: A systematic review. Knee 2015, 22, 360–371. [Google Scholar] [CrossRef] [Green Version]
- Leite, H.; Hodgkinson, I.R.; Gruber, T. New development: ‘Healing at a distance’—Telemedicine and COVID-19. Public Money Manag. 2020, 40, 483–485. [Google Scholar] [CrossRef] [Green Version]
- Smith, A.C.; Thomas, E.; Snoswell, C.L.; Haydon, H.; Mehrotra, A.; Clemensen, J.; Caffery, L.J. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J. Telemed. Telecare 2020, 26, 309–313. [Google Scholar] [CrossRef] [Green Version]
- Lacasse, A.; Pagé, M.G.; Dassieu, L.; Sourial, N.; Janelle-Montcalm, A.; Dorais, M.; Nguena Nguefack, H.L.; Godbout-Parent, M.; Hudspith, M.; Moor, G.; et al. Impact of the COVID-19 pandemic on the pharmacological, physical, and psychological treatments of pain: Findings from the Chronic Pain & COVID-19 Pan-Canadian Study. Pain Rep. 2021, 6, e891. [Google Scholar]
- Eccleston, C.; Blyth, F.M.; Dear, B.F.; Fisher, E.A.; Keefe, F.J.; Lynch, M.E.; Palermo, T.M.; Reid, M.C.; de C Williams, A.C. Managing patients with chronic pain during the COVID-19 outbreak: Considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain 2020, 161, 889–893. [Google Scholar] [CrossRef] [PubMed]
- Nieto, R.; Pardo, R.; Sora, B.; Feliu-Soler, A.; Luciano, J.V. Impact of COVID-19 Lockdown Measures on Spanish People with Chronic Pain: An Online Study Survey. J. Clin. Med. 2020, 9, 3558. [Google Scholar] [CrossRef] [PubMed]
- Karos, K.; McParland, J.L.; Bunzli, S.; Devan, H.; Hirsh, A.; Kapos, F.P.; Keogh, E.; Moore, D.; Tracy, L.M.; Ashton-James, C.E. The social threats of COVID-19 for people with chronic pain. Pain 2020, 161, 2229–2235. [Google Scholar] [CrossRef]
- Varangot-Reille, C.; Suso-Martí, L.; Romero-Palau, M.; Suárez-Pastor, P.; Cuenca-Martínez, F. Effects of Different Therapeutic Exercise Modalities on Migraine or Tension-Type Headache: A Systematic Review and Meta-Analysis with a Replicability Analysis. J. Pain 2021. [Google Scholar] [CrossRef]
- Coulter, I.D.; Crawford, C.; Hurwitz, E.L.; Vernon, H.; Khorsan, R.; Suttorp Booth, M.; Herman, P.M. Manipulation and mobilization for treating chronic low back pain: A systematic review and meta-analysis. Spine J. 2018, 18, 866–879. [Google Scholar] [CrossRef] [Green Version]
- Panunzio, A.; Tafuri, A.; Mazzucato, G.; Cerrato, C.; Orlando, R.; Pagliarulo, V.; Antonelli, A.; Cerruto, M.A. Botulinum Toxin-A Injection in Chronic Pelvic Pain Syndrome Treatment: A Systematic Review and Pooled Meta-Analysis. Toxins 2022, 14, 25. [Google Scholar] [CrossRef]
- Varangot-Reille, C.; Suso-Martí, L.; Dubuis, V.; Cuenca-Martínez, F.; Blanco-Díaz, M.; Salar-Andreu, C.; Casaña, J.; Calatayud, J. Exercise and Manual Therapy for the Treatment of Primary Headache: An Umbrella and Mapping Review. Phys. Ther. 2022. [Google Scholar] [CrossRef]
- Dupeyron, A.; Ribinik, P.; Gélis, A.; Genty, M.; Claus, D.; Hérisson, C.; Coudeyre, E. Education in the management of low back pain: Literature review and recall of key recommendations for practice. Ann. Phys. Rehabil. Med. 2011, 54, 319–335. [Google Scholar] [CrossRef] [Green Version]
- Wood, L.; Hendrick, P.A. A systematic review and meta-analysis of pain neuroscience education for chronic low back pain: Short-and long-term outcomes of pain and disability. Eur. J. Pain 2019, 23, 234–249. [Google Scholar] [CrossRef]
- Hall, M.; Dobson, F.; Plinsinga, M.; Mailloux, C.; Starkey, S.; Smits, E.; Hodges, P.; Vicenzino, B.; Schabrun, S.M.; Masse-Alarie, H. Effect of exercise on pain processing and motor output in people with knee osteoarthritis: A systematic review and meta-analysis. Osteoarthr. Cartil. 2020, 28, 1501–1513. [Google Scholar] [CrossRef] [PubMed]
- Du, S.; Hu, L.; Dong, J.; Xu, G.; Chen, X.; Jin, S.; Zhang, H.; Yin, H. Self-management program for chronic low back pain: A systematic review and meta-analysis. Patient Educ. Couns. 2017, 100, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Ariza-Mateos, M.J.; Cabrera-Martos, I.; Prados-Román, E.; Granados-Santiago, M.; Rodríguez-Torres, J.; Carmen Valenza, M. A systematic review of internet-based interventions for women with chronic pain. Br. J. Occup. Ther. 2020, 84, 6–14. [Google Scholar] [CrossRef]
- White, V.; Linardon, J.; Stone, J.E.; Holmes-Truscott, E.; Olive, L.; Mikocka-Walus, A.; Hendrieckx, C.; Evans, S.; Speight, J. Online psychological interventions to reduce symptoms of depression, anxiety, and general distress in those with chronic health conditions: A systematic review and meta-analysis of randomized controlled trials. Psychol. Med. 2022, 52, 548–573. [Google Scholar] [CrossRef]
- Dario, A.B.; Moreti Cabral, A.; Almeida, L.; Ferreira, M.L.; Refshauge, K.; Simic, M.; Pappas, E.; Ferreira, P.H. Effectiveness of telehealth-based interventions in the management of non-specific low back pain: A systematic review with meta-analysis. Spine J. 2017, 17, 1342–1351. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar]
- Stone, P.W. Popping the (PICO) question in research and evidence-based practice. Appl. Nurs. Res. 2002, 15, 197–198. [Google Scholar] [CrossRef]
- Shariff, S.Z.; Bejaimal, S.A.; Sontrop, J.M.; Iansavichus, A.V.; Haynes, R.B.; Weir, M.A.; Garg, A.X. Retrieving clinical evidence: A comparison of PubMed and Google Scholar for quick clinical searches. J. Med. Internet Res. 2013, 15, e164. [Google Scholar] [CrossRef]
- Haddaway, N.R.; Collins, A.M.; Coughlin, D.; Kirk, S. The Role of Google Scholar in Evidence Reviews and Its Applicability to Grey Literature Searching. PLoS ONE 2015, 10, e0138237. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Pham, B.; Jones, A.; Cook, D.J.; Jadad, A.R.; Moher, M.; Tugwell, P.; Klassen, T.P. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet 1998, 352, 609–613. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Furlan, A.D.; Pennick, V.; Bombardier, C.; van Tulder, M. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine 2009, 34, 1929–1941. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; Version 5.1.0; The Cochrane Collaboration: London, UK, 2008. [Google Scholar]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef] [Green Version]
- Hariohm, K.; Prakash, V.; Saravankumar, J. Quantity and quality of randomized controlled trials published by Indian physiotherapists. Perspect. Clin. Res. 2015, 6, 91. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. An Application of Hierarchical Kappa-type Statistics in the Assessment of Majority Agreement among Multiple Observers. Biometrics 1977, 33, 363. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE Working Group GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef] [Green Version]
- Andrews, J.; Guyatt, G.; Oxman, A.D.; Alderson, P.; Dahm, P.; Falck-Ytter, Y.; Nasser, M.; Meerpohl, J.; Post, P.N.; Kunz, R.; et al. GRADE guidelines: 14. Going from evidence to recommendations: The significance and presentation of recommendations. J. Clin. Epidemiol. 2013, 66, 719–725. [Google Scholar] [CrossRef]
- Balshem, H.; Helfand, M.; Schünemann, H.J.; Oxman, A.D.; Kunz, R.; Brozek, J.; Vist, G.E.; Falck-Ytter, Y.; Meerpohl, J.; Norris, S.; et al. GRADE guidelines: 3. Rating the quality of evidence. J. Clin. Epidemiol. 2011, 64, 401–406. [Google Scholar] [CrossRef]
- Sanabria, A.J.; Rigau, D.; Rotaeche, R.; Selva, A.; Marzo-Castillejo, M.; Alonso-Coello, P. GRADE: Methodology for formulating and grading recommendations in clinical practice. Aten. Primaria 2015, 47, 48–55. [Google Scholar] [CrossRef] [Green Version]
- Harrer, M.; Cuijpers, P.; Furukawa, T.A.; Ebert, D.D. Doing Meta-Analysis with R: A Hands-On Guide, 1st ed.; Chapman & Hall/CRC Press: Boca Raton, FL, USA; London, UK, 2021; ISBN 978-0-367-61007-4. [Google Scholar]
- Hedges, L. Estimation of effect size from a series of independent experiments. Psychol. Bull. 1982, 92, 490–499. [Google Scholar] [CrossRef]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive statistics for studies in sports medicine and exercise science. Med. Sci. Sports Exerc. 2009, 41, 3–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, J.P.; Li, T.; Deeks, J.J. 6.5.2.3 Obtaining Standard Deviations from Standard Errors, Confidence Intervals, t Statistics and p Values for Differences in Means. Available online: https://handbook-5-1.cochrane.org/chapter_7/7_7_3_3_obtaining_standard_deviations_from_standard_errors.htm (accessed on 23 February 2022).
- Viechtbauer, W. Bias and Efficiency of Meta-Analytic Variance Estimators in the Random-Effects Model. J. Educ. Behav. Stat. 2005, 30, 261–293. [Google Scholar] [CrossRef]
- Veroniki, A.A.; Jackson, D.; Viechtbauer, W.; Bender, R.; Bowden, J.; Knapp, G.; Kuss, O.; Higgins, J.P.T.; Langan, D.; Salanti, G. Methods to estimate the between-study variance and its uncertainty in meta-analysis. Res. Synth. Methods 2016, 7, 55–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Knapp, G.; Hartung, J. Improved tests for a random effects meta-regression with a single covariate. Stat. Med. 2003, 22, 2693–2710. [Google Scholar] [CrossRef]
- Sidik, K.; Jonkman, J.N. A simple confidence interval for meta-analysis. Stat. Med. 2002, 21, 3153–3159. [Google Scholar] [CrossRef]
- Sullivan, M.J.L.; Bishop, S.R.; Pivik, J. The Pain Catastrophizing Scale: Development and validation. Psychol. Assess. 1995, 7, 524–532. [Google Scholar] [CrossRef]
- Borenstein, M.; Higgins, J.P.T. Meta-Analysis and Subgroups. Prev. Sci. 2013, 14, 134–143. [Google Scholar] [CrossRef]
- Hoaglin, D. Misunderstandings about Q and “Cochran’s Q test” in meta-analysis. Stat. Med. 2016, 35, 485–495. [Google Scholar] [CrossRef]
- Borenstein, M.; Higgins, J.P.T.; Hedges, L.V.; Rothstein, H.R. Basics of meta-analysis: I(2) is not an absolute measure of heterogeneity. Res. Synth. Methods 2017, 8, 5–18. [Google Scholar] [CrossRef] [Green Version]
- IntHout, J.; Ioannidis, J.P.A.; Rovers, M.M.; Goeman, J.J. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open 2016, 6, e010247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Viechtbauer, W.; Cheung, M.W.-L. Outlier and influence diagnostics for meta-analysis. Res. Synth. Methods 2010, 1, 112–125. [Google Scholar] [CrossRef]
- Rücker, G.; Schwarzer, G. Beyond the forest plot: The drapery plot. Res. Synth. Methods 2021, 12, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Doi, S.A. Rendering the Doi plot properly in meta-analysis. Int. J. Evid.-Based. Healthc. 2018, 16, 242–243. [Google Scholar] [CrossRef] [PubMed]
- Furuya-Kanamori, L.; Barendregt, J.J.; Doi, S.A.R. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int. J. Evid. Based. Healthc. 2018, 16, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Amorim, A.B.; Pappas, E.; Simic, M.; Ferreira, M.L.; Jennings, M.; Tiedemann, A.; Carvalho-E-Silva, A.P.; Caputo, E.; Kongsted, A.; Ferreira, P.H. Integrating Mobile-health, health coaching, and physical activity to reduce the burden of chronic low back pain trial (IMPACT): A pilot randomised controlled trial. BMC Musculoskelet. Disord. 2019, 20, 71. [Google Scholar] [CrossRef] [Green Version]
- Berman, R.L.H.; Iris, M.A.; Bode, R.; Drengenberg, C. The Effectiveness of an Online Mind-Body Intervention for Older Adults with Chronic Pain. J. Pain 2009, 10, 68–79. [Google Scholar] [CrossRef]
- Chiauzzi, E.; Pujol, L.A.; Wood, M.; Bond, K.; Black, R.; Yiu, E.; Zacharoff, K. PainACTION-Back Pain: A self-management website for people with chronic back pain. Pain Med. 2010, 11, 1044–1058. [Google Scholar] [CrossRef]
- Dear, B.F.; Titov, N.; Perry, K.N.; Johnston, L.; Wootton, B.M.; Terides, M.D.; Rapee, R.M.; Hudson, J.L. The Pain Course: A randomised controlled trial of a clinician-guided Internet-delivered cognitive behaviour therapy program for managing chronic pain and emotional well-being. Pain 2013, 154, 942–950. [Google Scholar] [CrossRef]
- Dear, B.F.; Gandy, M.; Karin, E.; Staples, L.G.; Johnston, L.; Fogliati, V.J.; Wootton, B.M.; Terides, M.D.; Kayrouz, R.; Perry, K.N.; et al. The Pain Course: A randomised controlled trial examining an internet-delivered pain management program when provided with different levels of clinician support. Pain 2015, 156, 1920–1935. [Google Scholar] [CrossRef] [PubMed]
- De Boer, M.J.; Versteegen, G.J.; Vermeulen, K.M.; Sanderman, R.; Struys, M.M.R.F. A randomized controlled trial of an Internet-based cognitive-behavioural intervention for non-specific chronic pain: An effectiveness and cost-effectiveness study. Eur. J. Pain 2014, 18, 1440–1451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferwerda, M.; Van Beugen, S.; Van Middendorp, H.; Spillekom-Van Koulil, S.; Donders, A.R.T.; Visser, H.; Taal, E.; Creemers, M.C.W.; Van Riel, P.C.L.M.; Evers, A.W.M. A tailored-guided internet-based cognitive-behavioral intervention for patients with rheumatoid arthritis as an adjunct to standard rheumatological care: Results of a randomized controlled trial. Pain 2017, 158, 868–878. [Google Scholar] [CrossRef] [PubMed]
- Friesen, L.N.; Hadjistavropoulos, H.D.; Schneider, L.H.; Alberts, N.M.; Titov, N.; Dear, B.F. Examination of an internet-delivered cognitive behavioural pain management course for adults with fibromyalgia: A randomized controlled trial. Pain 2017, 158, 593–604. [Google Scholar] [CrossRef] [PubMed]
- Gardner-Nix, J.; Backman, S.; Barbati, J.; Grummitt, J. Evaluating distance education of a mindfulness-based meditation programme for chronic pain management. J. Telemed. Telecare 2008, 14, 88–92. [Google Scholar] [CrossRef]
- Gialanella, B.; Ettori, T.; Faustini, S.; Baratti, D.; Bernocchi, P.; Comini, L.; Scalvini, S. Home-Based Telemedicine in Patients with Chronic Neck Pain. Am. J. Phys. Med. Rehabil. 2017, 96, 327–332. [Google Scholar] [CrossRef]
- Gialanella, B.; Comini, L.; Olivares, A.; Gelmini, E.; Ubertini, E.; Grioni, G. Pain, disability and adherence to home exercises in patients with chronic neck pain: Long term effects of phone surveillance. A randomized controlled study. Eur. J. Phys. Rehabil. Med. 2020, 56, 104–111. [Google Scholar] [CrossRef]
- Guarino, H.; Fong, C.; Marsch, L.A.; Acosta, M.C.; Syckes, C.; Moore, S.K.; Cruciani, R.A.; Portenoy, R.K.; Turk, D.C.; Rosenblum, A. Web-based cognitive behavior therapy for chronic pain patients with aberrant drug-related behavior: Outcomes from a randomized controlled trial. Pain Med. 2018, 19, 2423–2437. [Google Scholar] [CrossRef]
- Bossen, D.; Veenhof, C.; van Beek, K.E.; Spreeuwenberg, P.M.; Dekker, J.; de Bakker, D.H. Effectiveness of a web-based physical activity intervention in patients with knee and/or hip osteoarthritis: Randomized controlled trial. J. Med. Internet Res. 2013, 15, e257. [Google Scholar] [CrossRef]
- Heapy, A.A.; Higgins, D.M.; Goulet, J.L.; La Chappelle, K.M.; Driscoll, M.A.; Czlapinski, R.A.; Buta, E.; Piette, J.D.; Krein, S.L.; Kerns, R.D. Interactive voice response-based self-management for chronic back Pain: The Copes noninferiority randomized trial. JAMA Intern. Med. 2017, 177, 765–773. [Google Scholar] [CrossRef] [Green Version]
- Herbert, M.S.; Afari, N.; Liu, L.; Heppner, P.; Rutledge, T.; Williams, K.; Eraly, S.; VanBuskirk, K.; Nguyen, C.; Bondi, M.; et al. Telehealth Versus In-Person Acceptance and Commitment Therapy for Chronic Pain: A Randomized Noninferiority Trial. J. Pain 2017, 18, 200–211. [Google Scholar] [CrossRef] [PubMed]
- Hernando-Garijo, I.; Ceballos-Laita, L.; Mingo-Gómez, M.T.; Medrano-De-la-fuente, R.; Estébanez-De-miguel, E.; Martínez-Pérez, M.N.; Jiménez-Del-barrio, S. Immediate effects of a telerehabilitation program based on aerobic exercise in women with fibromyalgia. Int. J. Environ. Res. Public Health 2021, 18, 2075. [Google Scholar] [CrossRef] [PubMed]
- Juhlin, S.; Bergenheim, A.; Gjertsson, I.; Larsson, A.; Mannerkorpi, K. Physical activity with person-centred guidance supported by a digital platform for persons with chronic widespread pain: A randomized controlled trial. J. Rehabil. Med. 2021, 53, jrm00175. [Google Scholar] [CrossRef] [PubMed]
- Kleiboer, A.; Sorbi, M.; van Silfhout, M.; Kooistra, L.; Passchier, J. Short-term effectiveness of an online behavioral training in migraine self-management: A randomized controlled trial. Behav. Res. Ther. 2014, 61, 61–69. [Google Scholar] [CrossRef]
- Krein, S.L.; Kadri, R.; Hughes, M.; Kerr, E.A.; Piette, J.D.; Holleman, R.; Kim, H.M.; Richardson, C.R. Pedometer-based internet-mediated intervention for adults with chronic low back pain: Randomized controlled trial. J. Med. Internet Res. 2013, 15, e181. [Google Scholar] [CrossRef]
- Lin, J.; Paganini, S.; Sander, L.; Lüking, M.; Daniel Ebert, D.; Buhrman, M.; Andersson, G.; Baumeister, H. An Internet-based intervention for chronic pain—A three-arm randomized controlled study of the effectiveness of guided and unguided acceptance and commitment therapy. Dtsch. Arztebl. Int. 2017, 114, 681–688. [Google Scholar]
- Lorig, K.R.; Laurent, D.D.; Deyo, R.A.; Marnell, M.E.; Minor, M.A.; Ritter, P.L. Can a back pain e-mail discussion group improve health status and lower health care costs? A randomized study. Arch. Intern. Med. 2002, 162, 792–796. [Google Scholar] [CrossRef] [Green Version]
- Lorig, K.R.; Ritter, P.L.; Laurent, D.D.; Plant, K. The internet-based arthritis self-management program: A one-year randomized trial for patients with arthritis or fibromyalgia. Arthritis Care Res. 2008, 59, 1009–1017. [Google Scholar] [CrossRef]
- Maisiak, R.; Austin, J.; Heck, L. Health outcomes of two telephone interventions for patients with rheumatoid arthritis or osteoarthritis. Arthritis Rheum. 1996, 39, 1391–1399. [Google Scholar] [CrossRef]
- Buhrman, M.; Fältenhag, S.; Ström, L.; Andersson, G. Controlled trial of Internet-based treatment with telephone support for chronic back pain. Pain 2004, 111, 368–377. [Google Scholar] [CrossRef]
- Moessner, M.; Schiltenwolf, M.; Neubauer, E. Internet-based aftercare for patients with back pain—A pilot study. Telemed. e-Health 2012, 18, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.; Nam, J.; Yang, D.; Jung, W.; Lee, H.R.; Kim, S.H. Effect of smartphone application-supported self-rehabilitation for frozen shoulder: A prospective randomized control study. Clin. Rehabil. 2019, 33, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Odole, A.C.; Ojo, O.D. A Telephone-based Physiotherapy Intervention for Patients with Osteoarthritis of the Knee. Int. J. Telerehabilit. 2013, 5, 11–20. [Google Scholar] [CrossRef] [Green Version]
- Odole, A.C.; Ojo, O.D. Is telephysiotherapy an option for improved quality of life in patients with osteoarthritis of the knee? Int. J. Telemed. Appl. 2014, 2014, 903816. [Google Scholar] [CrossRef] [Green Version]
- Peters, M.L.; Smeets, E.; Feijge, M.; Van Breukelen, G.; Andersson, G.; Buhrman, M.; Linton, S.J. Happy Despite Pain: A Randomized Controlled Trial of an 8-Week Internet-delivered Positive Psychology Intervention for Enhancing Well-being in Patients with Chronic Pain. Clin. J. Pain 2017, 33, 962–975. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petrozzi, M.J.; Leaver, A.; Ferreira, P.H.; Rubinstein, S.M.; Jones, M.K.; Mackey, M.G. Addition of MoodGYM to physical treatments for chronic low back pain: A randomized controlled trial. Chiropr. Man. Ther. 2019, 27, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Rickardsson, J.; Gentili, C.; Holmström, L.; Zetterqvist, V.; Andersson, E.; Persson, J.; Lekander, M.; Ljótsson, B.; Wicksell, R.K. Internet-delivered acceptance and commitment therapy as microlearning for chronic pain: A randomized controlled trial with 1-year follow-up. Eur. J. Pain 2021, 25, 1012–1030. [Google Scholar] [CrossRef]
- Ruehlman, L.S.; Karoly, P.; Enders, C. A randomized controlled evaluation of an online chronic pain self management program. Pain 2012, 153, 319–330. [Google Scholar] [CrossRef] [Green Version]
- Sander, L.B.; Paganini, S.; Terhorst, Y.; Schlicker, S.; Lin, J.; Spanhel, K.; Buntrock, C.; Ebert, D.D.; Baumeister, H. Effectiveness of a Guided Web-Based Self-help Intervention to Prevent Depression in Patients with Persistent Back Pain: The PROD-BP Randomized Clinical Trial. JAMA Psychiatry 2020, 77, 1001–1011. [Google Scholar] [CrossRef]
- Schlicker, S.; Baumeister, H.; Buntrock, C.; Sander, L.; Paganini, S.; Lin, J.; Berking, M.; Lehr, D.; Ebert, D.D. A Web- and mobile-Based intervention for comorbid, recurrent depression in patients with chronic back pain on sick leave (get.back): Pilot randomized controlled trial on feasibility, user satisfaction, and effectiveness. JMIR Ment. Health 2020, 7, e16398. [Google Scholar] [CrossRef] [Green Version]
- Buhrman, M.; Nilsson-Ihrfelt, E.; Jannert, M.; Ström, L.; Andersson, G. Guided internet-based cognitive behavioural treatment for chronic back pain reduces pain catastrophizing: A randomized controlled trial. J. Rehabil. Med. 2011, 43, 500–505. [Google Scholar] [PubMed] [Green Version]
- Schulz, P.J.; Rubinell, S.; Hartung, U. An internet-based approach to enhance self-management of chronic low back pain in the Italian-speaking population of Switzerland: Results from a pilot study. Int. J. Public Health 2007, 52, 286–294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simister, H.D.; Tkachuk, G.A.; Shay, B.L.; Vincent, N.; Pear, J.J.; Skrabek, R.Q. Randomized Controlled Trial of Online Acceptance and Commitment Therapy for Fibromyalgia. J. Pain 2018, 19, 741–753. [Google Scholar] [CrossRef]
- Smith, J.; Faux, S.G.; Gardner, T.; Hobbs, M.J.; James, M.A.; Joubert, A.E.; Kladnitski, N.; Newby, J.M.; Schultz, R.; Shiner, C.T.; et al. Reboot Online: A Randomized Controlled Trial Comparing an Online Multidisciplinary Pain Management Program with Usual Care for Chronic Pain. Pain Med. 2019, 20, 2385–2396. [Google Scholar] [CrossRef] [PubMed]
- Ström, L.; Pettersson, R.; Andersson, G. A controlled trial of self-help treatment of recurrent headache conducted via the Internet. J. Consult. Clin. Psychol. 2000, 68, 722–727. [Google Scholar] [CrossRef]
- Tavallaei, V.; Rezapour-Mirsaleh, Y.; Rezaiemaram, P.; Saadat, S.H. Mindfulness for female outpatients with chronic primary headaches: An internet-based bibliotherapy. Eur. J. Transl. Myol. 2018, 28, 175–184. [Google Scholar] [CrossRef]
- Trompetter, H.R.; Bohlmeijer, E.T.; Veehof, M.M.; Schreurs, K.M.G. Internet-based guided self-help intervention for chronic pain based on Acceptance and Commitment Therapy: A randomized controlled trial. J. Behav. Med. 2015, 38, 66–80. [Google Scholar] [CrossRef]
- Trudeau, K.J.; Pujol, L.A.; DasMahapatra, P.; Wall, R.; Black, R.A.; Zacharoff, K. A randomized controlled trial of an online self-management program for adults with arthritis pain. J. Behav. Med. 2015, 38, 483–496. [Google Scholar] [CrossRef] [Green Version]
- Vallejo, M.A.; Ortega, J.; Rivera, J.; Comeche, M.I.; Vallejo-Slocker, L. Internet versus face-to-face group cognitive-behavioral therapy for fibromyalgia: A randomized control trial. J. Psychiatr. Res. 2015, 68, 106–113. [Google Scholar] [CrossRef]
- Westenberg, R.F.; Zale, E.L.; Heinhuis, T.J.; Ozkan, S.; Nazzal, A.; Lee, S.G.; Chen, N.C.; Vranceanu, A.M. Does a brief mindfulness exercise improve outcomes in upper extremity patients? A randomized controlled trial. Clin. Orthop. Relat. Res. 2018, 476, 790–798. [Google Scholar] [CrossRef]
- Wilson, M.; Roll, J.M.; Corbett, C.; Barbosa-Leiker, C. Empowering Patients with Persistent Pain Using an Internet-based Self-Management Program. Pain Manag. Nurs. 2015, 16, 503–514. [Google Scholar] [CrossRef] [Green Version]
- Bromberg, J.; Wood, M.E.; Black, R.A.; Surette, D.A.; Zacharoff, K.L.; Chiauzzi, E.J. A randomized trial of a web-based intervention to improve migraine self-management and coping. Headache 2012, 52, 244–261. [Google Scholar] [CrossRef]
- Wilson, M.; Finlay, M.; Orr, M.; Barbosa-Leiker, C.; Sherazi, N.; Roberts, M.L.A.; Layton, M.; Roll, J.M. Engagement in online pain self-management improves pain in adults on medication-assisted behavioral treatment for opioid use disorders. Addict. Behav. 2018, 86, 130–137. [Google Scholar] [CrossRef]
- Yang, J.; Wei, Q.; Ge, Y.; Meng, L.; Zhao, M. Smartphone-Based Remote Self-Management of Chronic Low Back Pain: A Preliminary Study. J. Healthc. Eng. 2019, 2019, 4632946. [Google Scholar] [CrossRef]
- Hedman-Lagerlöf, M.; Hedman-Lagerlöf, E.; Axelsson, E.; Ljotsson, B.; Engelbrektsson, J.; Hultkrantz, S.; Lundbäck, K.; Björkander, D.; Wicksell, R.K.; Flink, I.; et al. Internet-Delivered Exposure Therapy for Fibromyalgia a Randomized Controlled Trial. Clin. J. Pain 2018, 34, 532–542. [Google Scholar] [CrossRef]
- Williams, D.A.; Kuper, D.; Segar, M.; Mohan, N.; Sheth, M.; Clauw, D.J. Internet-enhanced management of fibromyalgia: A randomized controlled trial. Pain 2010, 151, 694–702. [Google Scholar] [CrossRef] [PubMed]
- Shigaki, C.L.; Smarr, K.L.; Siva, C.; Ge, B.; Musser, D.; Johnson, R. RAHelp: An online intervention for individuals with rheumatoid arthritis. Arthritis Care Res. 2013, 65, 1573–1581. [Google Scholar] [CrossRef] [PubMed]
- Brattberg, G. Self-administered EFT (Emotional Freedom Techniques) in individuals with fibromyalgia: A randomized trial. Integr. Med. 2008, 7, 30–35. [Google Scholar]
- Calner, T.; Nordin, C.; Eriksson, M.K.; Nyberg, L.; Gard, G.; Michaelson, P. Effects of a self-guided, web-based activity programme for patients with persistent musculoskeletal pain in primary healthcare: A randomized controlled trial. Eur. J. Pain 2017, 21, 1110–1120. [Google Scholar] [CrossRef] [PubMed]
- Nordin, C.A.; Michaelson, P.; Gard, G.; Eriksson, M.K. Effects of the web behavior change program for activity and multimodal pain rehabilitation: Randomized controlled trial. J. Med. Internet Res. 2016, 18, e265. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, K.M.; Stoner, S.A.; Mundt, J.M.; Stoelbc, B. An online self-help CBT intervention for chronic lower back pain. Clin. J. Pain 2012, 28, 14–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chhabra, H.S.; Sharma, S.; Verma, S. Smartphone app in self-management of chronic low back pain: A randomized controlled trial. Eur. Spine J. 2018, 27, 2862–2874. [Google Scholar] [CrossRef] [PubMed]
- Boselie, J.J.L.M.; Vancleef, L.M.G.; Peters, M.L. Filling the glass: Effects of a positive psychology intervention on executive task performance in chronic pain patients. Eur. J. Pain 2018, 22, 1268–1280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scott, W.; Chilcot, J.; Guildford, B.; Daly-Eichenhardt, A.; McCracken, L.M. Feasibility randomized-controlled trial of online Acceptance and Commitment Therapy for patients with complex chronic pain in the United Kingdom. Eur. J. Pain 2018, 22, 1473–1484. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef]
- Murray, C.J.L.; Piot, P. The Potential Future of the COVID-19 Pandemic: Will SARS-CoV-2 Become a Recurrent Seasonal Infection? JAMA 2021, 325, 1249–1250. [Google Scholar] [CrossRef]
- Skegg, D.; Gluckman, P.; Boulton, G.; Hackmann, H.; Karim, S.S.A.; Piot, P.; Woopen, C. Future scenarios for the COVID-19 pandemic. Lancet 2021, 397, 777–778. [Google Scholar] [CrossRef]
- Shanthanna, H.; Strand, N.H.; Provenzano, D.A.; Lobo, C.A.; Eldabe, S.; Bhatia, A.; Wegener, J.; Curtis, K.; Cohen, S.P.; Narouze, S. Caring for patients with pain during the COVID-19 pandemic: Consensus recommendations from an international expert panel. Anaesthesia 2020, 75, 935–944. [Google Scholar] [CrossRef] [Green Version]
- Fu, Y.; Mcnichol, E.; Marczewski, K.; Closs, J. Patient—Professional partnerships and chronic back pain self-management: A qualitative systematic review and synthesis. Health Soc. Care Community 2016, 24, 247–259. [Google Scholar] [CrossRef]
- Lewis, Y.D.; Elran-barak, R.; Tov, R.G.; Zubery, E. The abrupt transition from face-to-face to online treatment for eating disorders: A pilot examination of patients’ perspectives during the COVID-19 lockdown. J. Eat. Disord. 2021, 9, 31. [Google Scholar] [CrossRef]
- Schünemann, H.; Brożek, J.; Guyatt, G.; Oxman, A. Manual GRADE para Calificar la Calidad de la Evidencia y la Fuerza de la Recomendación (1ª Ed. en Español). P.A Orrego & M.X. Rojas (Translator) March 2017. 2013. Available online: http://gdt.guidelinedevelopment.org/app/handbook/handbook.html (accessed on 23 February 2022).

| Authors, Year Design Country | Participants Sample Size (n) Age (Mean (SD)) Gender Condition | Intervention Modality Format | Comparator | Outcomes | Results |
|---|---|---|---|---|---|
| Amorim et al., 2019 Pilot RCT Australia | N = 68 58.3 (13.4) yrs 50%F/50%M Chronic LBP | Tailored-plan treatment with activity tracker and monitoring application. + Telephone follow-up Mobile application | Advice to stay active and booklet about benefits of physical activity |
| No significant differences in pain intensity. |
| Berman et al., 2009 RCT USA | N = 89 65.8 (N/R) yrs 87%F/13%M Unspecified chronic pain | Self-care intervention Internet-based | No intervention |
| Significant difference in pain intensity (Self-care: p < 0.01 and control: p < 0.05) and pain interference (both p < 0.01), but without differences between group. Small no-significant improvement in self-efficacy in both groups (p > 0.05). |
| Boselie et al., 2018 RCT The Netherlands | N = 33 N/R yrs N/R %F/N/R %M Unspecified chronic pain | Positive psychology Internet-based | Waiting list |
| Intervention group effect was non-significant for pain intensity (p = 0.16). |
| Bossen et al., 2013 RCT The Netherlands | N = 199 62.0 (5.7) yrs 65%F/35%M Knee and hip OA | Behavior graded activity program Internet-based | Waiting list |
| No significant differences in pain intensity and self-efficacy. |
| Brattberg, 2008 RCT Sweden | N = 66 43.8 (8.8) yrs 100%F Unspecified chronic pain | Emotional freedom techniques Internet-based | Waiting list |
| Statistically significant time × group interaction in the different subscales of the pain catastrophizing scale (p < 0.001, p = 0.006 and p < 0.001). There was no statistically significant difference in self-efficacy. |
| Bromberg et al., 2012 RCT USA | N = 189 42.6 (11.5) yrs 89%F/11%M Chronic migraine | Structured behavior changes program +Usual care Internet-based | Usual care |
| They also showed less feeling of helplessness (p = 0.003) and rumination (p = 0.0003), globally, there was a higher improvement of catastrophizing (p = 0.0006). There was also a higher improvement of self-efficacy (p < 0.0001). |
| Buhrman et al., 2004 RCT Sweden | n = 56 44.6 (10.4) yrs 63%F/37%M Chronic back pain | Online CBT + Relaxation with CDs + Telephone calls about goals Internet-based | Waiting list |
| Significant effect of intervention group on catastrophizing (p < 0.01). There was no significant main effects difference on multidimensional pain inventory. Both groups reduced their average and highest pain intensity (p < 0.05) without significant differences. |
| Buhrman et al., 2011 RCT Sweden | N = 54 43.2 (9.8) yrs 69%F/32%M Chronic back pain | Online CBT Internet-based | Waiting list |
| There is a significant interaction for the intervention group (p = 0.0001) on catastrophizing. However, there were no significant differences between group for multidimensional pain inventory. |
| Calner et al., 2017 & Nordin et al., 2016 RCT Sweden | N = 99 43.1 (10.5) yrs 85%F/15%M Unspecified chronic pain | Multimodal pain rehabilitation + Behavior change program Internet-based | Multimodal pain rehabilitation |
| There were no statistically significant differences over time on pain intensity. |
| Carpenter et al., 2012 RCT USA | N = 164 42.5 (10.3) yrs 83%F/17%M Chronic LBP | Interactive self-help intervention (pain education and CBT) Internet-based | Waiting list |
| Both groups improved significantly all the outcomes. |
| Chabbra et al., 2018 RCT India | N = 93 41.2 (14.1) yrs N/R %F/N/R %M Chronic LBP | Daily activity goals with exercises Mobile application | Prescription about medicines and advice about physical activity |
| Both groups showed a significant decrease of pain intensity (p < 0.001) but without differences. |
| Chiauzzi et al., 2010 RCT USA | N = 209 46.1 (12.0) yrs 68%F/32%M Chronic back pain | Online CBT and self-management website Internet-based | Standard back pain management text materials |
| There was no statistically significant effect on self-efficacy, pain intensity, and pain catastrophizing. |
| Choi et al., 2019 RCT | N = 84 54.5 (x) yrs 68%F/32%M Frozen shoulder | NSAIDs + Self-Exercise+ mobile-based guided exercise Mobile application | NSAIDs + Exercise | Pain intensity: VAS | There were no significant differences between groups in any outcomes. |
| De Boer et al., 2014 RCT The Netherlands | N = 50 52.1 (11.2) yrs 64%F/36%M Unspecified chronic pain | CBT Internet-based | CBT Face-to-Face |
| Online group showed a statistically significant interaction on catastrophizing (p = 0.023), pain intensity (p = 0.020), however there was no interaction in other outcomes. |
| Dear et al., 2013 RCT Australia | N = 63 49.0 (13) yrs 85%F/15%M Unspecified chronic pain | Online CBT Internet-based | Waiting list |
| Intervention had a significantly higher post-treatment improvement self-efficacy (p < 0.001), kinesiophobia (p < 0.001) and the catastrophizing subscale of the PRSS (p = 0.005). |
| Dear et al., 2015 RCT Australia | N = 490 50 (13) yrs 80%F/20%M Unspecified chronic pain | G1: Online CBT + Regular online contact G2: Online CBT + optimal online contact G3: Online CBT Internet-based | Waiting list |
| Intervention groups had significantly a significantly lower scores of pain intensity average than waiting list (p ≤ 0.03). All treatment groups, without control group, showed a significant improvement of self-efficacy and kinesiophobia (p ≤ 0.046). |
| Ferwerda et al., 2017 RCT The Netherlands | N = 133 56.4 (10) yrs 64%F/36%M Rheumatoid arthritis | CBT Internet-based | Usual care |
| There was no statistically significant improvement of pain intensity (p = 0.35). |
| Friesen et al., 2017 RCT Canada | N = 60 48.0 (11.0) yrs 95%F/5%M Fibromyalgia | CBT + Telephone calls Internet-based | Waiting list |
| Intervention group had a significantly higher improvement of pain intensity (p = 0.037). However, there was not for pain interference. There was also a statistically significant time by group interaction for kinesiophobia (p < 0.001). Other outcomes were not significant. |
| Gardner-Nix et al., 2008 RCT Canada | N = 163 50.0–55.0 yrs 81%F/19%M Unspecific chronic pain | Mindfulness Videoconferencing | CG1:Mindfulness Face-to-Face CG2: Waiting list |
| Both mindfulness group improved more catastrophizing than waiting list (p < 0.01) post-treatment but without significant differences between them. Both mindfulness group showed lower pain-intensity than control group post-treatment (p < 0.01 and p < 0.05), but face-to-face showed also lower pain score than online treatment (p < 0.05). |
| Gialanella et al., 2017 and 2020 RCT Italy | N = 94 58.1 (12.7) yrs 89%F/11%M Chronic neck pain | Exercise + Telephone calls with a therapist Telephone | Exercise + Recommendations to continue to exercise |
| Both groups had statistically significant lower pain intensity post-treatment (p < 0.001), but it was lower in the intervention group (p < 0.001). |
| Guarino et al., 2018 RCT USA | N = 110 51.3 (10.9) yrs 60%F/40%M Unspecific chronic pain | Online CBT + Usual care Internet-based | Usual care |
| Both groups significantly improved pain severity and interference, but without difference between them. However, patients with the online treatment showed a statistically significant reduction catastrophizing (p = 0.040) in comparation with control group. |
| Heapy et al., 2017 RCT USA | N = 125 57.9 (11.6) yrs 22%F/78%M Chronic back pain | CBT Interactive voice response | Face-to-Face CBT |
| CBT through interactive voice response was noninferior to in-person CBT in post-treatment pain intensity. There were no significant differences between e-CBT and face-to-face CBT in pain interference. |
| Hedman-Lagerlöf et al., 2018 RCT Sweden | N = 140 98%F/2%M 50.8 (24–77) yrs Fibromyalgia | Online exposure therapy Internet-based | Waiting list |
| There were statistically significant interactions in favor of intervention group on pain intensity according to the FIQ, (p < 0.001). |
| Herbert et al., 2017 RCT USA | N = 128 18%F/82%M 52.0 (13.3) yrs Unspecific chronic pain | ACT Video teleconferencing | Face-to-face ACT |
| VTC-ACT was noninferior to face-to-face ACT on pain interference. Also, there were no significant differences on any other outcomes, except on the activity subscale of the MPI (p = 0.03). |
| Hernando-Garijo et al., 2021 RCT Spain | N = 34 53.4 (8.8) yrs 100%F Fibromyalgia | Video-guided aerobic training + usual medical prescription Videos | Usual medical prescription |
| There was a statistically significant higher improvement of pain intensity (p = 0.021). There was no statistically significant difference in catastrophizing. |
| Juhlin et al., 2021 RCT Sweden | N = 139 47.6 (10.1) yrs 90%F/10%M Chronic widespread pain | Person-centered intervention supported by online platform Internet-based | Person-centered intervention |
| There were no significant differences between group on pain intensity (p = 0.39) or other outcomes. |
| Kleiboer et al., 2014 RCT The Netherlands | N = 368 43.6 (11.5) yrs 85%F/15%M Migraine | Online behavioral training Internet-based | Waiting list |
| There were no significant differences between groups except for self-efficacy (p < 0.001). |
| Krein et al., 2013 RCT USA | N = 229 51.6 (12.6) yrs 12%F/88%M Chronic LBP | Pedometer, online goal-setting and feedback platform and e-community Internet-based | Pedometer |
| Intervention group showed no statistically significant on pain interference (p = 0.09). Intervention group showed a higher exercise self-efficacy post-treatment (p = 0.01) who failed to maintain at 12 months. There were no more significant differences. |
| Lin et al., 2017 RCT Germany | N = 201 51.0 (12.4) yrs 86%F/14%M Unspecific chronic pain | Online guided ACT Internet-based | Waiting list |
| There was a significant interaction effect for group x time on the pain interference (p < 0.01), but also on pain intensity (p < 0.05), in favor of intervention group. |
| Lorig et al., 2002 RCT USA | N = 580 45.5 (N/R) yrs 38%F/62%M Chronic back pain | Back pain textbook via e-mail + videotapes about back pain experiences + e-community Online textbook and videotapes and internet-based | Usual care + subscription to a non-health-related magazine |
| There was a statistically significant higher improvement in pain intensity (p < 0.05) in intervention group. There was also a significant higher improvement of self-efficacy (p = 0.003). |
| Lorig et al., 2008 RCT USA | N = 855 52.3 (11.6) yrs 90%F/10%M Fibromyalgia | Web-based self-management instruction and discussion Internet-based | Usual care |
| There was a significant time by group interaction on pain intensity (p < 0.001). |
| Maisiak et al., 1996 RCT USA | N = 255 60.3 (N/R) yrs 92%F/8%M Hip or Knee OA or Rheumatoid Arthritis | Telephone counseling strategy Telephone | Usual care |
| Patients in the telephone counselling had higher improvement in total AIMS2 score (p < 0.01). |
| Moessner et al., 2012 RCT Germany | N = 75 45.9 (9.1) yrs 56%F/44%M Chronic back pain | Self-monitoring + Online guided chat Internet-based | Usual care |
| Patients had a statistically significant lower score of pain according to the SF536 Pain subscale. However, there were no differences in other outcomes. |
| Odole and Ojo, 2013 and 2014 RCT Nigeria | N = 50 55.5 (7.6) yrs 48%F/52%M Knee OA | Phone-based Physical Therapy Telephone | Face-to-face physical therapy |
| Both groups showed statistically significant improvement of their pain intensity. |
| Peters et al., 2017 RCT Sweden | N = 284 48.6 (12.0) yrs 85%F/15%M Chronic back, neck or shoulder pain | G1: Online Positive psychology G2: Online CBT Internet-based | Waiting list |
| There were significant differences in pain catastrophizing and helplessness. There was no statistically significant time, group, or time by group effect on pain intensity. |
| Petrozzi et al., 2019 RCT New Zealand | N = 108 50.4 (13.6) yrs 50%F/50%M Chronic LBP | Online CBT+ Usual care Internet-based | Usual care |
| There were no statistically significant differences between the two groups on self-efficacy (p = 0.52), pain intensity (p = 0.95) and catastrophizing (p = 0.89) at any time-points. |
| Rickardsson et al., 2021 RCT Sweden | N = 113 49.5 (12.1) yrs 75%F/25%M Unspecific chronic pain | Online ACT Internet-based | Waiting list |
| The intervention group showed significant interaction effects of time x group for pain interference (p < 0.001) and pain intensity (p = 0.004). |
| Ruehlman et al., 2012 RCT USA | N = 305 44.9 (x) yrs 64%F/36%M Unspecific chronic pain | Online program about chronic pain with self-management tools and a e-community Internet-based | Usual care |
| Intervention group showed a significant group × time interaction in pain interference (p = 0.00) and pain severity (p = 0.01). Intervention group also showed a significant group × time interaction in catastrophizing (p = 0.01) |
| Sander et al., 2020 RCT Germany | N = 295 52.8 (7.7) yrs 62%F/38%M Unspecific chronic pain | Online CBT + Usual care Internet-based | Usual Care |
| Online training showed small to medium effect sizes in all the outcomes, except for pain intensity. |
| Schlickler et al., 2020 RCT Germany | N = 76 50.8 (7.9) yrs 55%F/45%M Chronic back pain | Online CBT-based intervention Internet-based and mobile-based | Waiting list |
| There were no statistically significant differences in any other outcome. |
| Schulz et al., 2007 RCT Switzerland | N = 35 45.3 (N/R) yrs 29%F/71%M Chronic low back pain | Online social and educational about pain management website Internet-based | No treatment |
| Pain intensity in the treatment group has decreased, however, there was no change in the control group. |
| Shigaki et al., 2013 RCT USA | N = 108 49.8 (11.9) yrs 94%F/6%M Rheumatoid arthritis | Education and social network website + Telephone calls Internet-based | Waiting list |
| There were significant differences post-treatment in favor of the intervention group in self-efficacy (p = 0.000) and quality of life (p = 0.003), who maintained at 9 months (p = 0.000 and p = 0.004, respectively). |
| Scott et al., 2018 RCT UK | N = 63 45.5 (14.0) yrs 64%F/36%M Unspecific chronic pain | Online ACT + Usual care Internet-based | Usual care |
| Pain interference and pain intensity showed small effect size in favor of intervention group. |
| Simister al., 2018 RCT | N = 67 39.7 (9.4) yrs 95%F/5%M Fibromyalgia | Online ACT + Usual care Internet-based | Usual care |
| Intervention group significantly improved, relative to control group, kinesiophobia (p < 0.001). Small effect size for pain in favor of intervention group (0.11). There was only a tendency to improvement in favor of online group on catastrophizing (p = 0.051). |
| Smith et al., 2019 RCT Australia | N = 80 45.0 (13.9) yrs 88%F/12%M Unspecific chronic pain | Online self-management and CBT-based intervention Internet-based | Usual care |
| There were significant time-by-group interactions on pain self-efficacy (p < 0.05), pain severity (p < 0.05), kinesiophobia (p < 0.01), in favor of intervention group. However, there were no interactions for pain interference. |
| Ström et al., 2000 RCT Sweden | N = 45 36.7 (N/R) yrs 69%F/31%M Recurrent headache sufferers | Online relaxation and problem-solving intervention Internet-based | Wait-list |
| There was a statistically significant difference between groups at post treatment for pain intensity (p = 0.009). |
| Tavallaei et al., 2018 RCT Iran | N = 30 33.7 (9.0) yrs 100%F Migraine and tension-type headache | Mindfulness-based Stress Reduction Bibliotherapy Internet-based | Usual care |
| There was a significant difference between both groups in favor of the online group in pain intensity (p = 0.035). |
| Trompetter et al., 2015 RCT The Netherlands | N = 238 52.7 (12.4) yrs 76%F/24%M Unspecific chronic pain | Online ACT Internet-based | Waiting list |
| There was no significant difference in pain interference, however there was in pain intensity (p = 0.35) and catastrophizing (p = 0.019). |
| Trudeau et al., 2015 RCT USA | N = 228 49.9 (11.6) 68%F/32%M Arthritis | Online self-management intervention Internet-based | Waiting List |
| There were statistically significant interactions group-by-time in favor of intervention group on self-efficacy (p = 0.0293) and catastrophizing (p = 0.0055). |
| Vallejo et al., 2015 RCT Spain | N = 60 51.6 (9.9) yrs 100%F Fibromyalgia | Online CBT + Usual care Internet-based | G1: Face-to-face CBT + Usual care G2: Usual care |
| Both CBT groups showed improvement in catastrophizing (both, p < 0.001). Only the online group showed improvement of self-efficacy (p < 0.001). |
| Westenberg et al., 2018 RCT USA | N = 126 54.5 (15.0) yrs 50%F/50%M | Online Mindfulness | Attention control |
| Online Mindfulness showed a statistically significant higher improvement of pain intensity (p = 0.008). However, the difference in pain intensity did not reach the minimal clinically important difference. |
| Williams et al., 2010 RCT USA | N = 118 50.5 (11.5) yrs 95%F/5%M Fibromyalgia | Online self-management + Usual care Internet-based | Usual care |
| Patients in the intervention group shown statistically significant improvement of pain intensity (p < 0.01). |
| Wilson et al., 2015 RCT USA | N = 114 49.3 (11.6) yrs 78%F/12%M Unspecific chronic pain | Online pain self-management program Internet-based | Usual care |
| There was not a statistically significant interaction group by time on pain interference and pain intensity. However, there was a significant interaction group by time on self-efficacy (p = 0.00) in favor of the online group. |
| Wilson et al., 2018 RCT USA | N = 60 44.3 (12.0) yrs 44%F/56%M Unspecific chronic pain | Online self-management program Internet-based | Waiting-list |
| Intervention group showed higher level of pain interference, and pain severity, than control group. |
| Yang et al., 2019 RCT China | N = 8 40.8 (12.5) yrs 88%F/12%M Chronic LBP | Online self-management + Face-to-face Physiotherapy Mobile application | Face-to-face physiotherapy |
| There were no significant differences on pain intensity. Additionally, there were no significant interaction effects on self-efficacy. |
| Certainty Assessment | No. of Participants | Effect | Certainty | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome (No. of Studies) | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | e-BMT | Control | Absolute (95% CI) | |
| Pain intensity (vs. Usual care/Waiting list) (n = 38) | RCT | Serious | Not serious | Not serious | Not serious | Serious | 2757 | 2580 | −0.17 (−0.26; −0.09) | Low ⊕⊕ |
| Pain intensity (vs. In person BMT) (n = 5) | RCT | Serious | Not serious | Not serious | Not serious | Not serious | 217 | 269 | 0.21 (0.15; 0.27) | Moderate ⊕⊕⊕ |
| Pain interference (vs. Usual care/Waiting list) (n = 13) | RCT | Serious | Serious | Not serious | Not serious | Not serious | 791 | 851 | −0.24 (−0.44; −0.05) | Low ⊕⊕ |
| Kinesiophobia (vs. Usual care/Waiting list) (n = 3) | RCT | Serious | Not serious | Not serious | Not serious | Not serious | 201 | 139 | −0.57 (−1.08; −0.06) | Moderate ⊕⊕⊕ |
| Catastrophizing (vs. Usual care/Waiting list) (n = 16) | RCT | Serious | Not serious | Not serious | Not serious | Not serious | 826 | 787 | −0.40 (−0.48; −0.32) | Moderate ⊕⊕⊕ |
| Self-efficacy (vs. Usual care/Waiting list) (n = 20) | RCT | Serious | Serious | Not serious | Not serious | Not serious | 1407 | 1404 | 0.38 (0.23; 0.54) | Low ⊕⊕ |
| Outcomes (Contrast)—Subanalysis | N Studies | SMD | Lower Limit 95%CI | Upper Limit 95% CI | Q | I2 |
|---|---|---|---|---|---|---|
| Pain intensity (vs. Usual Care/Waiting List)—Treatment | ||||||
| ACT | 5 | −0.33 | −0.86 | 0.19 | 15.40 | 74% |
| CBT | 12 | −0.18 | −0.38 | 0.02 | 23.16 | 53% |
| Positive Psychology | 2 | −0.23 | −2.96 | 2.50 | 2.45 | 59% |
| Self-management | 8 | −0.11 | −0.23 | 0.008 | 6.48 | 0% |
| Mindfulness | 2 | −0.35 | −1.97 | 1.26 | 0.58 | 0% |
| Other types of treatment | 10 | −0.11 | −0.27 | 0.05 | 15.40 | 74% |
| Pain intensity (vs. Usual Care/Waiting List) —Chronic Musculoskeletal disorder | ||||||
| Unspecific back pain | 6 | −0.16 | −0.50 | 0.19 | 13.21 | 62% |
| Fibromyalgia | 4 | −0.66 | −1.06 | −0.25 | 3.28 | 9% |
| Headache | 3 | −0.16 | −0.55 | 0.23 | 1.79 | 0% |
| Low Back Pain | 6 | −0.12 | −0.28 | 0.04 | 3.34 | 0% |
| Rheumatic disorders | 5 | −0.09 | −0.25 | 0.07 | 2.74 | 0% |
| Unspecified chronic pain | 15 | −0.14 | −0.29 | 0.01 | 27.33 | 49% |
| Pain intensity (vs. Usual Care/Waiting List)—Online Modality | ||||||
| Mobile application | 3 | −0.04 | −0.57 | 0.50 | 1.31 | 0% |
| Internet | 30 | −0.18 | −0.26 | −0.10 | 44.29 | 35% |
| Multi-device | 2 | 0.33 | −1.40 | 2.07 | 0.72 | 0% |
| Videoconference | 2 | −0.40 | −2.92 | 2.13 | 1.17 | 15% |
| Telephone | 2 | −0.27 | −4.71 | 4.16 | 8.08 | 88% |
| Pain intensity (vs. Usual Care/Waiting List)—Intervention duration (without Krein et al.) | ||||||
| More than 3 months | 11 | −0.16 | −0.32 | −0.002 | 16.60 | 40% |
| Between 1 and 3 months | 24 | −0.18 | −0.32 | −0.05 | 48.79 | 53% |
| Less than 1 month | 3 | −0.21 | −0.61 | 0.20 | 1.54 | 0% |
| Pain interference (vs. Usual Care/Waiting List)—Treatment | ||||||
| ACT | 3 | −0.52 | −1.07 | 0.03 | 3.53 | 43% |
| CBT | 6 | −0.22 | −0.59 | 0.16 | 10.89 | 54% |
| Self-Management | 4 | −0.09 | −0.32 | 0.14 | 2.29 | 0% |
| Self-efficacy (vs. Usual Care/Waiting List)—Treatment | ||||||
| CBT | 9 | 0.49 | 0.17 | 0.80 | 33.21 | 76% |
| Self-management | 6 | 0.32 | 0.13 | 0.50 | 5.65 | 12% |
| Other types of treatment | 5 | 0.27 | −0.06 | 0.59 | 8.06 | 50% |
| Self-efficacy (vs. Usual Care/Waiting List)—Chronic Musculoskeletal disorder | ||||||
| Unspecific back pain | 4 | 0.24 | −0.06 | 0.54 | 5.37 | 44% |
| Fibromyalgia | 2 | 0.63 | −0.72 | 1.97 | 0.33 | 0% |
| LBP | 4 | 0.52 | −0.54 | 1.58 | 17.75 | 83% |
| Headache | 1 | 0.41 | 0.09 | 0.73 | N/A | N/A |
| Rheumatic disorders | 4 | 0.24 | −0.22 | 0.70 | 6.93 | 57% |
| Unspecified chronic pain | 5 | 0.56 | 0.09 | 1.02 | 9.75 | 59% |
| Self-efficacy (vs. Usual Care/Waiting List)—Intervention duration (without Krein et al.) | ||||||
| More than 3 months | 3 | 0.37 | −0.13 | 0.87 | 2.72 | 27% |
| Between 1 and 3 months | 13 | 0.37 | 0.17 | 0.56 | 27.17 | 56% |
| Less than 1 month | 3 | 0.74 | −1.49 | 2.97 | 18.97 | 90% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cuenca-Martínez, F.; López-Bueno, L.; Suso-Martí, L.; Varangot-Reille, C.; Calatayud, J.; Herranz-Gómez, A.; Romero-Palau, M.; Casaña, J. Implementation of Online Behavior Modification Techniques in the Management of Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 1806. https://doi.org/10.3390/jcm11071806
Cuenca-Martínez F, López-Bueno L, Suso-Martí L, Varangot-Reille C, Calatayud J, Herranz-Gómez A, Romero-Palau M, Casaña J. Implementation of Online Behavior Modification Techniques in the Management of Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2022; 11(7):1806. https://doi.org/10.3390/jcm11071806
Chicago/Turabian StyleCuenca-Martínez, Ferran, Laura López-Bueno, Luis Suso-Martí, Clovis Varangot-Reille, Joaquín Calatayud, Aida Herranz-Gómez, Mario Romero-Palau, and José Casaña. 2022. "Implementation of Online Behavior Modification Techniques in the Management of Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 11, no. 7: 1806. https://doi.org/10.3390/jcm11071806
APA StyleCuenca-Martínez, F., López-Bueno, L., Suso-Martí, L., Varangot-Reille, C., Calatayud, J., Herranz-Gómez, A., Romero-Palau, M., & Casaña, J. (2022). Implementation of Online Behavior Modification Techniques in the Management of Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 11(7), 1806. https://doi.org/10.3390/jcm11071806










