Association between Sagittal Cervical Spinal Alignment and Degenerative Cervical Spondylosis: A Retrospective Study Using a New Scoring System
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Scoring System (Degenerative Cervical Spondylosis [DCS] Score)
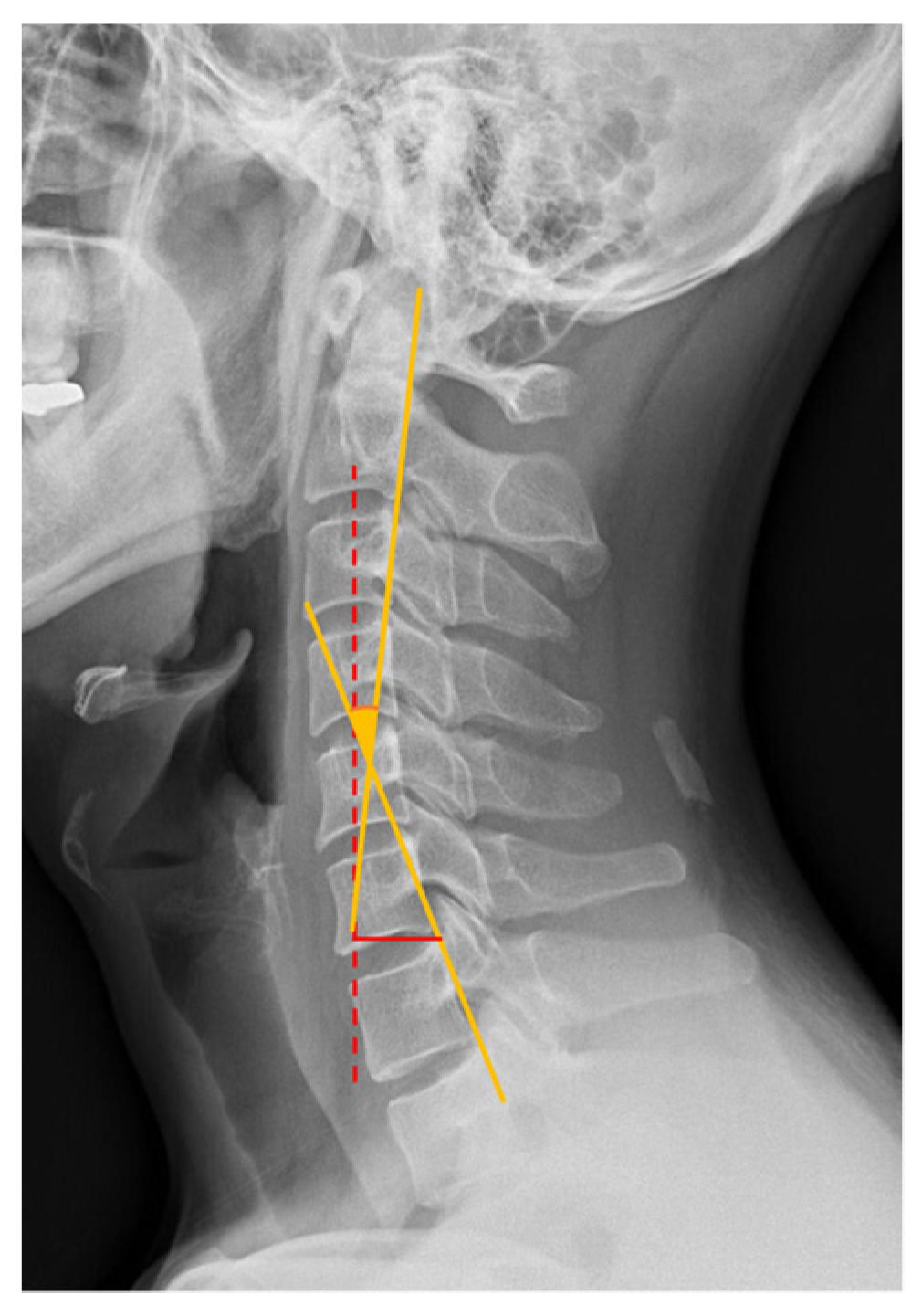
2.3. Assessment of Sagittal Cervical Alignment
2.4. Statistical Analyses
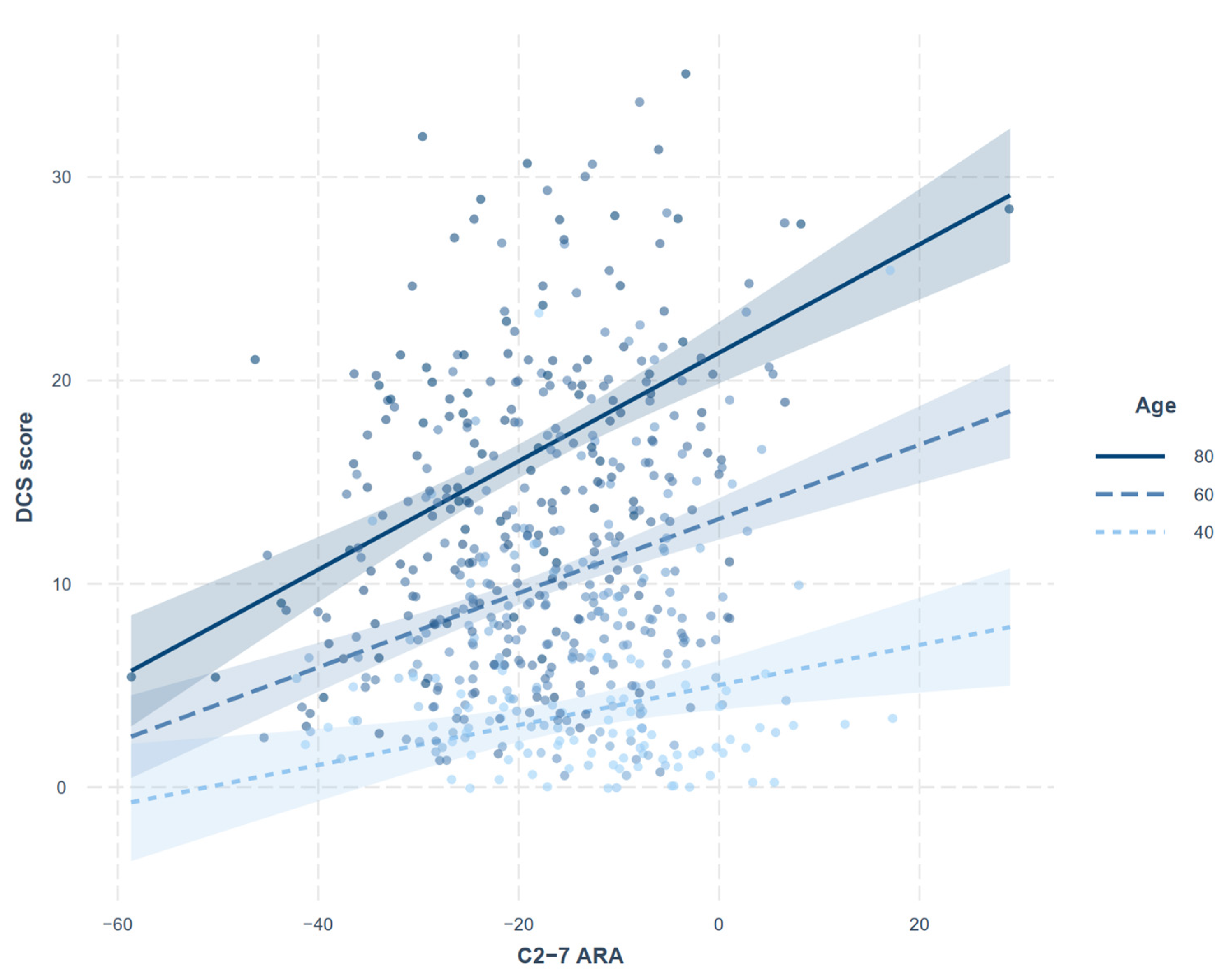
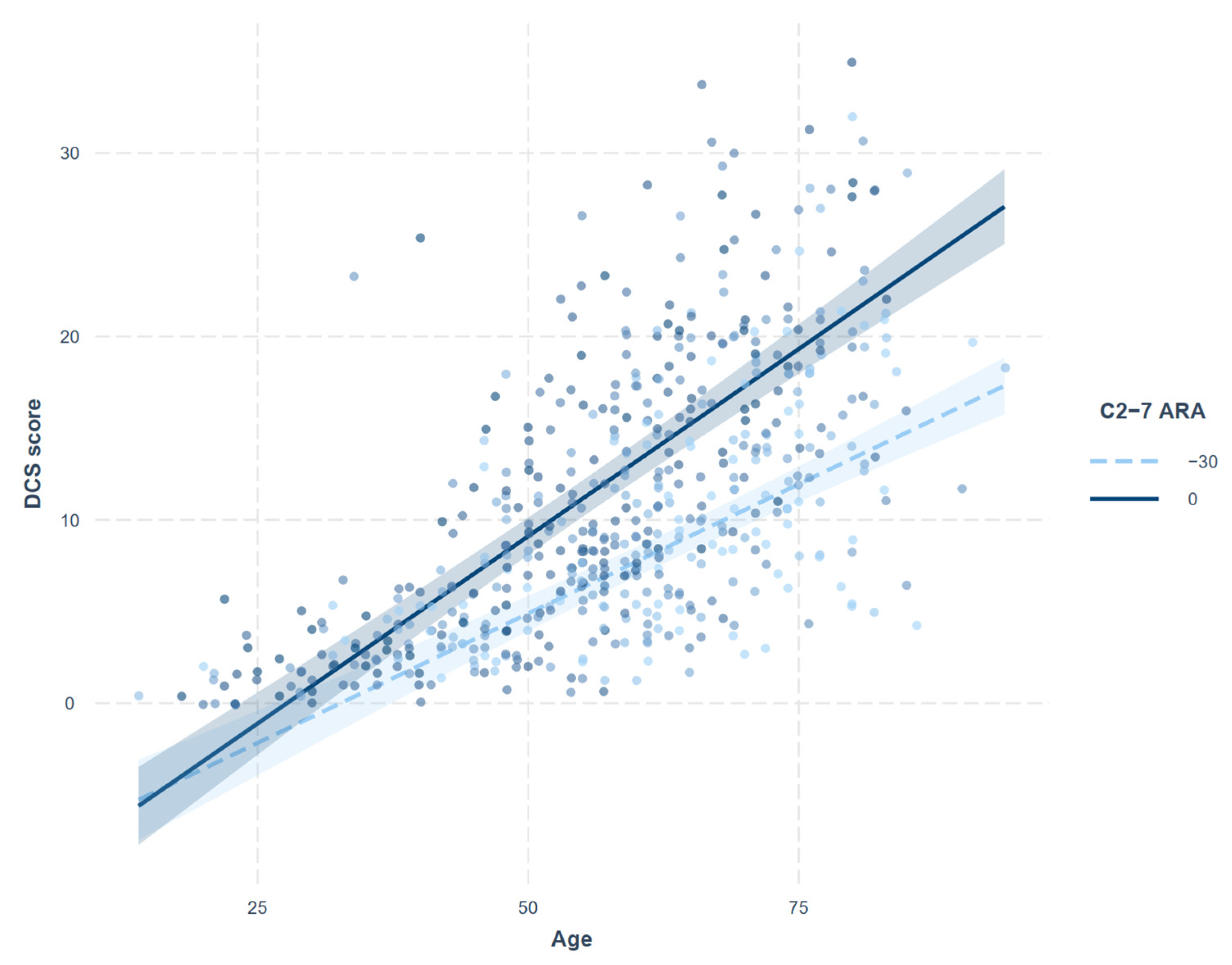
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Benoist, M. Natural history of the aging spine. Eur. Spine J. 2003, 12 (Suppl. 2), S86–S89. [Google Scholar] [CrossRef] [PubMed]
- Theodore, N. Degenerative Cervical Spondylosis. N. Engl. J. Med. 2020, 383, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Tang, R.; Ye, I.B.; Cheung, Z.B.; Kim, J.S.; Cho, S.K. Age-related Changes in Cervical Sagittal Alignment: A Radiographic Analysis. Spine 2019, 44, E1144–E1150. [Google Scholar] [CrossRef]
- Park, M.S.; Moon, S.H.; Lee, H.M.; Kim, S.W.; Kim, T.H.; Lee, S.Y.; Riew, K.D. The effect of age on cervical sagittal alignment: Normative data on 100 asymptomatic subjects. Spine 2013, 38, E458–E463. [Google Scholar] [CrossRef] [PubMed]
- Yukawa, Y.; Kato, F.; Suda, K.; Yamagata, M.; Ueta, T. Age-related changes in osseous anatomy, alignment, and range of motion of the cervical spine. Part I: Radiographic data from over 1200 asymptomatic subjects. Eur. Spine J. 2012, 21, 1492–1498. [Google Scholar] [CrossRef] [PubMed]
- Charles, Y.P.; Prost, S.; Pesenti, S.; Iharreborde, B.; Bauduin, E.; Laouissat, F.; Riouallon, G.; Wolff, S.; Challier, V.; Obeid, I.; et al. Variation of cervical sagittal alignment parameters according to gender, pelvic incidence and age. Eur. Spine J. 2022, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Szeto, G.; Dai, J. Prevalence and risk factors associated with musculoskeletal complaints among users of mobile handheld devices: A systematic review. Appl. Ergon. 2017, 59, 132–142. [Google Scholar] [CrossRef]
- Zhuang, L.; Wang, L.; Xu, D.; Wang, Z.; Liang, R. Association between excessive smartphone use and cervical disc degeneration in young patients suffering from chronic neck pain. J. Orthop. Sci. 2021, 26, 110–115. [Google Scholar] [CrossRef]
- Koh, M.J.; Park, S.Y.; Woo, Y.S.; Kang, S.H.; Park, S.H.; Chun, H.J.; Park, E.J. Assessing the Prevalence of Recurrent Neck and Shoulder Pain in Korean High School Male Students: A Cross-sectional Observational Study. Korean J. Pain 2012, 25, 161–167. [Google Scholar] [CrossRef]
- Guan, X.; Fan, G.; Wu, X.; Zeng, Y.; Su, H.; Gu, G.; Zhou, Q.; Gu, X.; Zhang, H.; He, S. Photographic measurement of head and cervical posture when viewing mobile phone: A pilot study. Eur. Spine J. 2015, 24, 2892–2898. [Google Scholar] [CrossRef]
- Lee, S.; Kang, H.; Shin, G. Head flexion angle while using a smartphone. Ergonomics 2015, 58, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Barrett, J.M.; McKinnon, C.; Callaghan, J.P. Cervical spine joint loading with neck flexion. Ergonomics 2020, 63, 101–108. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Ofiram, E.; Garvey, T.A.; Schwender, J.D.; Denis, F.; Perra, J.H.; Transfeldt, E.E.; Winter, R.B.; Wroblewski, J.M. Cervical degenerative index: A new quantitative radiographic scoring system for cervical spondylosis with interobserver and intraobserver reliability testing. J. Orthop. Traumatol. 2009, 10, 21–26. [Google Scholar] [CrossRef]
- Harrison, D.E.; Harrison, D.D.; Cailliet, R.; Troyanovich, S.J.; Janik, T.J.; Holland, B. Cobb Method or Harrison Posterior Tangent Method: Which to Choose for Lateral Cervical Radiographic Analysis. Spine 2000, 25, 2072–2078. [Google Scholar] [CrossRef]
- Ames, C.P.; Blondel, B.; Scheer, J.K.; Schwab, F.J.; Le Huec, J.C.; Massicotte, E.M.; Patel, A.A.; Traynelis, V.C.; Kim, H.J.; Shaffrey, C.I.; et al. Cervical radiographical alignment: Comprehensive assessment techniques and potential importance in cervical myelopathy. Spine 2013, 38, S149–S160. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Imai, K.; Keele, L.; Yamamoto, T. Identification, inference and sensitivity analysis for causal mediation effects. Stat. Sci. 2010, 25, 51–71. [Google Scholar] [CrossRef]
- Tingley, D.; Yamamoto, T.; Hirose, K.; Keele, L.; Imai, K. Mediation: R Package for Causal Mediation Analysis. J. Stat. Softw. 2014, 59, 1–38. [Google Scholar] [CrossRef]
- Lehto, I.J.; Tertti, M.O.; Komu, M.E.; Paajanen, H.E.K.; Tuominen, J.; Kormano, M.J. Age-related MRI changes at 0.1 T in cervical discs in asymptomatic subjects. Neuroradiology 1994, 36, 49–53. [Google Scholar] [CrossRef]
- Kato, F.; Yukawa, Y.; Suda, K.; Yamagata, M.; Ueta, T. Normal morphology, age-related changes and abnormal findings of the cervical spine. Part II: Magnetic resonance imaging of over 1200 asymptomatic subjects. Eur. Spine J. 2012, 21, 1499–1507. [Google Scholar] [CrossRef] [PubMed]
- Okada, E.; Matsumoto, M.; Ichihara, D.; Chiba, K.; Toyama, Y.; Fujiwara, H.; Momoshima, S.; Nishiwaki, Y.; Hashimoto, T.; Ogawa, J.; et al. Aging of the cervical spine in healthy volunteers: A 10-year longitudinal magnetic resonance imaging study. Spine 2009, 34, 706–712. [Google Scholar] [CrossRef] [PubMed]
- Oe, S.; Togawa, D.; Nakai, K.; Yamada, T.; Arima, H.; Banno, T.; Yasuda, T.; Kobayasi, S.; Yamato, Y.; Hasegawa, T.; et al. The Influence of Age and Sex on Cervical Spinal Alignment Among Volunteers Aged Over 50. Spine 2015, 40, 1487–1494. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Lenke, L.G.; Oshima, Y.; Chuntarapas, T.; Mesfin, A.; Hershman, S.; Fogelson, J.L.; Riew, K.D. Cervical Lordosis Actually Increases With Aging and Progressive Degeneration in Spinal Deformity Patients. Spine Deform. 2014, 2, 410–414. [Google Scholar] [CrossRef]
- Al-Hadidi, F.; Bsisu, I.; AlRyalat, S.A.; Al-Zu’bi, B.; Bsisu, R.; Hamdan, M.; Kanaan, T.; Yasin, M.; Samarah, O. Association between mobile phone use and neck pain in university students: A cross-sectional study using numeric rating scale for evaluation of neck pain. PLoS ONE 2019, 14, e0217231. [Google Scholar] [CrossRef]
- Bonney, R.A.; Corlett, E.N. Head posture and loading of the cervical spine. Appl. Ergon. 2002, 33, 415–417. [Google Scholar] [CrossRef]
- Przybyla, A.S.; Skrzypiec, D.; Pollintine, P.; Dolan, P.; Adams, M.A. Strength of the cervical spine in compression and bending. Spine 2007, 32, 1612–1620. [Google Scholar] [CrossRef]
- Shin, Y.; Han, K.; Lee, Y.H. Temporal Trends in Cervical Spine Curvature of South Korean Adults Assessed by Deep Learning System Segmentation, 2006–2018. JAMA Netw. Open 2020, 3, e2020961. [Google Scholar] [CrossRef]
- Pinter, Z.W.; Salmons, H.I., IV; Townsley, S.E.; Xiong, A.; Michalopoulos, G.D.; El Sammak, S.; Currier, B.; Nassr, A.; Freedman, B.A.; Bydon, M.; et al. Improved Sagittal Alignment is Associated with Early Postoperative Neck Disability and Pain Related Patient Reported Outcomes following Posterior Cervical Decompression and Fusion for Myelopathy. World Neurosurg. 2022. [Google Scholar] [CrossRef]
- Gao, K.; Zhang, J.; Lai, J.; Liu, W.; Lyu, H.; Wu, Y.; Lin, Z.; Cao, Y. Correlation between cervical lordosis and cervical disc herniation in young patients with neck pain. Medicine 2019, 98, e16545. [Google Scholar] [CrossRef]
- Yin, M.; Xu, C.; Ma, J.; Ye, J.; Mo, W. A Bibliometric Analysis and Visualization of Current Research Trends in the Treatment of Cervical Spondylotic Myelopathy. Glob. Spine J. 2021, 11, 988–998. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, S.E.; Cole, D.A. Bias in cross-sectional analyses of longitudinal mediation. Psychol. Methods 2007, 12, 23–44. [Google Scholar] [CrossRef] [PubMed]
- MacKinnon, D. Introduction to Statistical Mediation Analysis; Routledge: New York, NY, USA, 2012. [Google Scholar]
- O’Laughlin, K.D.; Martin, M.J.; Ferrer, E. Cross-sectional analysis of longitudinal mediation processes. Multivar. Behav. Res. 2018, 53, 375–402. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Lee, J.W.; Chai, J.W.; Yoo, H.J.; Kang, Y.; Seo, J.; Ahn, J.M.; Kang, H.S. A New MRI Grading System for Cervical Foraminal Stenosis Based on Axial T2-Weighted Images. Korean J. Radiol. 2015, 16, 1294–1302. [Google Scholar] [CrossRef]
- Gellhorn, A.C.; Katz, J.N.; Suri, P. Osteoarthritis of the spine: The facet joints. Nat. Rev. Rheumatol. 2013, 9, 216–224. [Google Scholar] [CrossRef]

| Disc Degeneration | ||
|---|---|---|
| Sclerosis | None | 0 |
| Detectable | 1 | |
| Definite (with irregularity) | 2 | |
| Narrowing 1 | <25% | 0 |
| 25~50% | 1 | |
| 51~75% | 2 | |
| >75% | 3 | |
| Anterior osteophytes | None | 0 |
| <2 mm | 1 | |
| ≥2 mm | 2 | |
| Posterior osteophytes 2,3 | None | 0 |
| <50% | 1 | |
| ≥50% | 2 | |
| Listhesis 4 | None | 0 |
| Present | 1 | |
| Facet joint | ||
| None or mild sclerotic change | 0 | |
| Mild narrowing or irregularity | 1 | |
| Severe narrowing | 2 |
| Sex | Female | Male | p |
|---|---|---|---|
| (n = 317) | (n = 244) | ||
| Age (yr), median [IQR] | 60.0 [49.0–69.0] | 58.0 [46.0–68.5] | 0.222 |
| Department, n (%) | 0.147 | ||
| Anesthesiology and pain medicine | 23 (7.3) | 15 (6.1) | |
| Neurology | 42 (3.2) | 25 (10.2) | |
| Neurosurgery | 49 (5.5) | 53 (21.7) | |
| Orthopedic | 165 (52.1) | 130 (53.3) | |
| Rheumatology | 19 (6.0) | 6 (2.5) | |
| Rehabilitation medicine | 19 (6.0) | 15 (6.1) | |
| DCS score, median [IQR] | |||
| Endplate sclerosis | 1.7 [1.0–3.0] | 2.3 [1.0–3.7] | 0.003 |
| Disc space narrowing | 0.7 [0.0–1.7] | 1.0 [0.0–2.3] | 0.036 |
| Anterior osteophyte | 1.3 [0.3–3.0] | 2.3 [0.7–4.3] | <0.001 |
| Posterior osteophyte | 2.0 [1.0–3.0] | 2.8 [1.7–4.0] | <0.001 |
| Listhesis | 1.0 [0.3–1.7] | 1.0 [0.7–2.0] | 0.012 |
| Facet joint | 0.7 [0.3–1.7] | 1.3 [0.3–2.7] | <0.001 |
| Total score | 8.3 [4.0–13.3] | 11.3 [6.0–18.0] | <0.001 |
| Sagittal alignment, mean ± SD | |||
| C2-7 ARA (°) | −17.5 ± 11.9 | −16.2 ± 11.0 | 0.179 |
| C2-7 SVA (mm) | 15.5 ± 9.3 | 21.7 ± 10.9 | <0.001 |
| Age | C2-7ARA | C2-7SVA | |
|---|---|---|---|
| C2-7ARA | −0.25 * | ||
| C2-7SVA | 0.14 * | 0.22 * | |
| DCS score | 0.66 * | 0.04 | 0.18 * |
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Estimate | p | Estimate | p | |
| (Intercept) | −7.472 | −11.318 | ||
| Male | 3.526 | <0.001 | 2.622 | 0.001 |
| Age | 0.346 | <0.001 | 0.408 | <0.001 |
| C2-7ARA | 0.168 | <0.001 | 0.070 | 0.318 |
| C2-7SVA | −0.034 | 0.136 | NA | NA |
| C2-7ARA * Age | NA | NA | 0.004 | <0.001 |
| C2-7ARA * Male | NA | NA | −0.041 | 0.284 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oh, C.; Lee, M.; Hong, B.; Song, B.-S.; Yun, S.; Kwon, S.; Ko, Y.; Lee, S.Y.; Noh, C. Association between Sagittal Cervical Spinal Alignment and Degenerative Cervical Spondylosis: A Retrospective Study Using a New Scoring System. J. Clin. Med. 2022, 11, 1772. https://doi.org/10.3390/jcm11071772
Oh C, Lee M, Hong B, Song B-S, Yun S, Kwon S, Ko Y, Lee SY, Noh C. Association between Sagittal Cervical Spinal Alignment and Degenerative Cervical Spondylosis: A Retrospective Study Using a New Scoring System. Journal of Clinical Medicine. 2022; 11(7):1772. https://doi.org/10.3390/jcm11071772
Chicago/Turabian StyleOh, Chahyun, Minwook Lee, Boohwi Hong, Byong-Sop Song, Sangwon Yun, Sanghun Kwon, Youngkwon Ko, Sun Yeul Lee, and Chan Noh. 2022. "Association between Sagittal Cervical Spinal Alignment and Degenerative Cervical Spondylosis: A Retrospective Study Using a New Scoring System" Journal of Clinical Medicine 11, no. 7: 1772. https://doi.org/10.3390/jcm11071772
APA StyleOh, C., Lee, M., Hong, B., Song, B.-S., Yun, S., Kwon, S., Ko, Y., Lee, S. Y., & Noh, C. (2022). Association between Sagittal Cervical Spinal Alignment and Degenerative Cervical Spondylosis: A Retrospective Study Using a New Scoring System. Journal of Clinical Medicine, 11(7), 1772. https://doi.org/10.3390/jcm11071772






