Influence of Sexual Dimorphism, Aging, and Differential Cell Capture Efficiency of Blood Separation Systems on the Quality of Platelet-Rich Plasma
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Volunteers
2.2. Study Procedures
2.3. Statistical Analysis
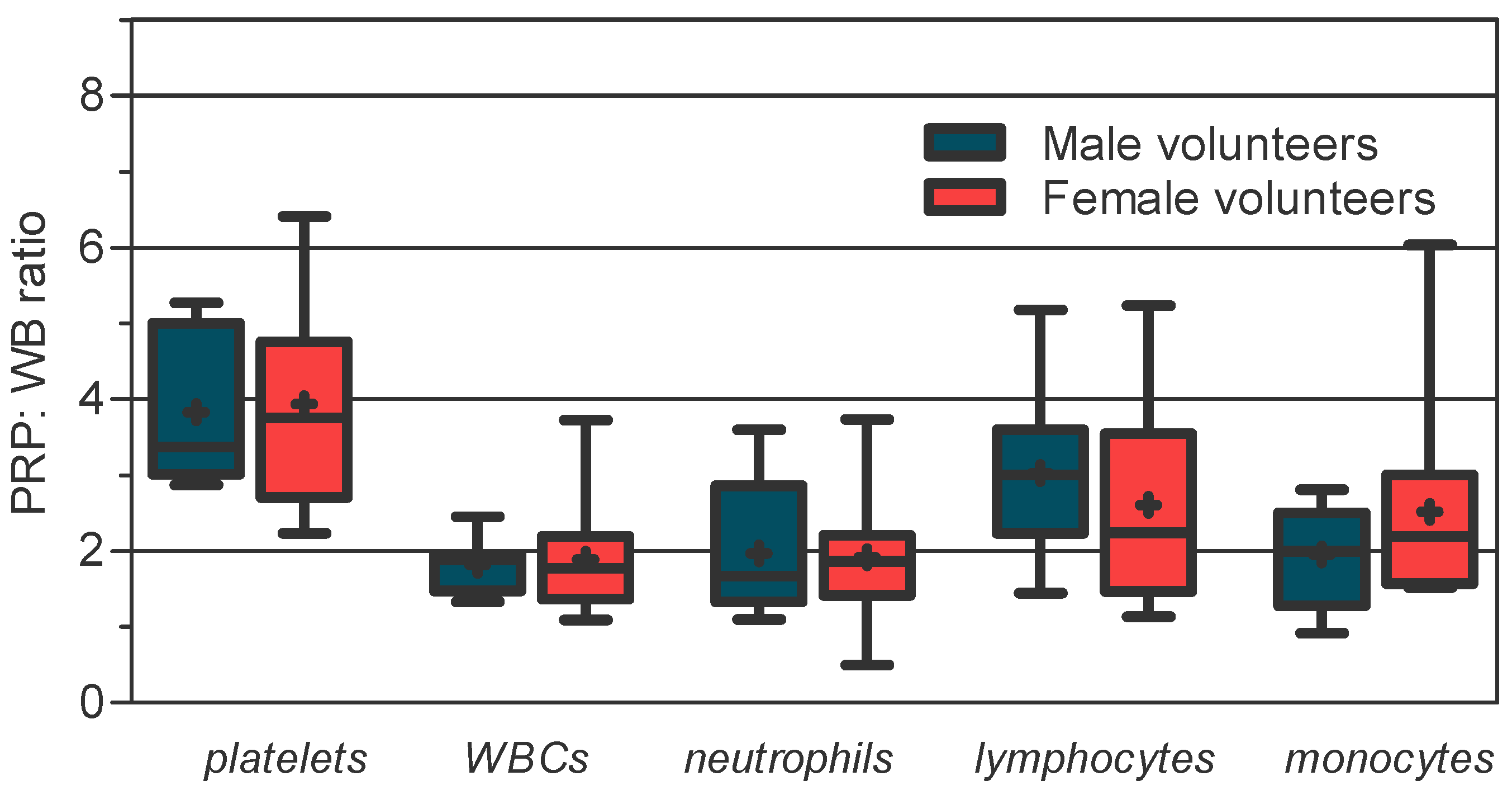
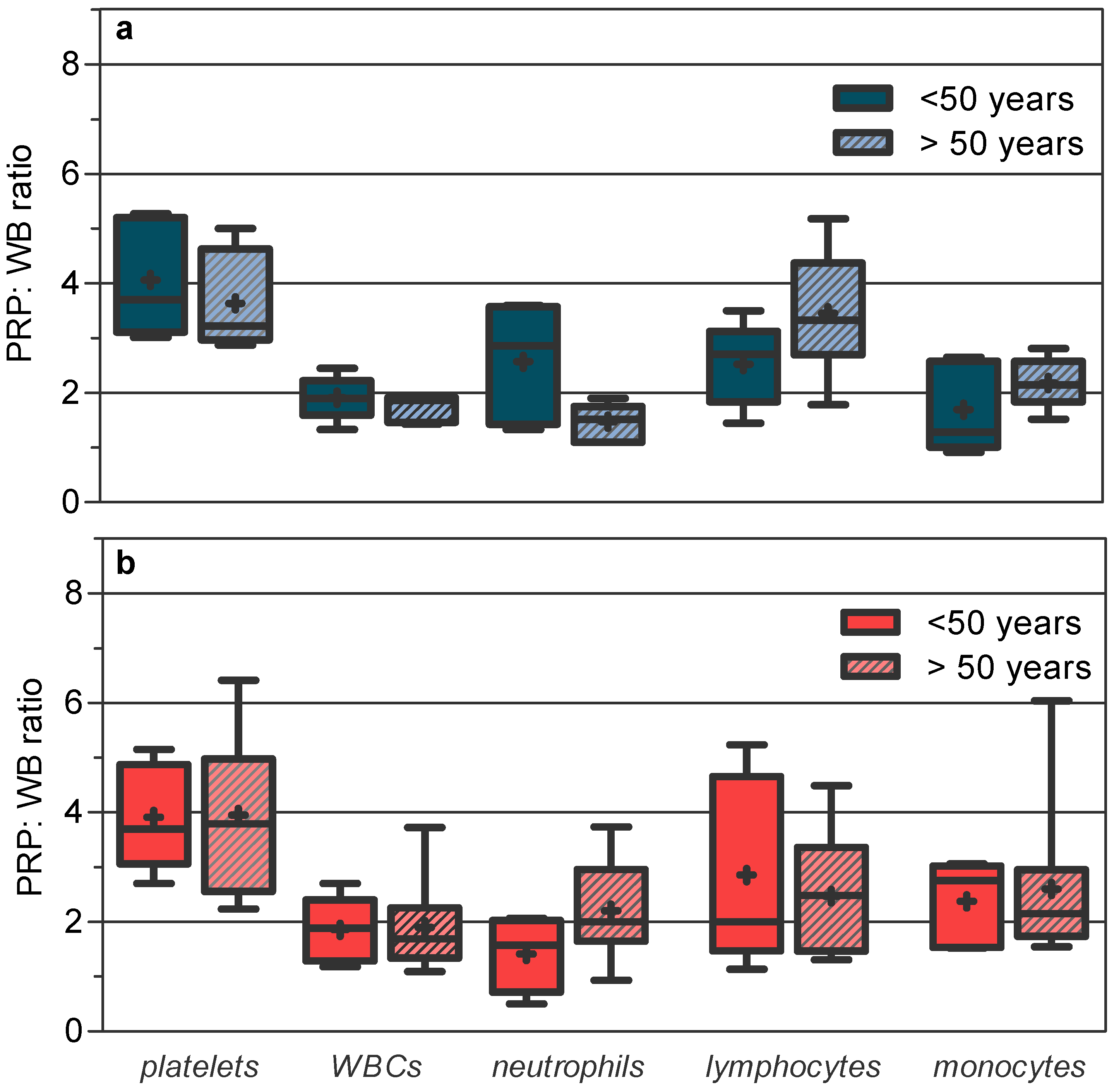
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Filardo, G.; Kon, E.; Roffi, A.; Di Matteo, B.; Merli, M.L.; Marcacci, M. Platelet-rich plasma: Why intra-articular? A systematic review of preclinical studies and clinical evidence on PRP for joint degeneration. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 2459–2474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramaswamy Reddy, S.H.; Reddy, R.; Babu, N.C.; Ashok, G.N. Stem-cell therapy and platelet-rich plasma in regenerative medicines: A review on pros and cons of the technologies. J. Oral Maxillofac. Pathol. 2018, 22, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Albanese, A.; Licata, M.E.; Polizzi, B.; Campisi, G. Platelet-rich plasma (PRP) in dental and oral surgery: From the wound healing to bone regeneration. Immun. Ageing 2013, 10, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhanot, S.; Alex, J.C. Current applications of platelet gels in facial plastic surgery. Facial Plast. Surg. 2002, 18, 27–33. [Google Scholar] [CrossRef]
- Foster, T.E.; Puskas, B.L.; Mandelbaum, B.R.; Gerhardt, M.B.; Rodeo, S.A. Platelet-rich plasma: From basic science to clinical applications. Am. J. Sports Med. 2009, 37, 2259–2272. [Google Scholar] [CrossRef]
- Mehta, S.; Watson, J.T. Platelet rich concentrate: Basic science and current clinical applications. J. Orthop. Trauma 2008, 22, 432–438. [Google Scholar] [CrossRef]
- Mishra, A.; Pavelko, T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am. J. Sports Med. 2006, 34, 1774–1778. [Google Scholar] [CrossRef]
- Wang, S.Z.; Fan, W.M.; Jia, J.; Ma, L.Y.; Yu, J.B.; Wang, C. Is exclusion of leukocytes from platelet-rich plasma (PRP) a better choice for early intervertebral disc regeneration? Stem Cell Res. Ther. 2018, 9, 199. [Google Scholar] [CrossRef] [Green Version]
- Hesseler, M.J.; Shyam, N. Platelet-rich plasma and its utility in medical dermatology: A systematic review. J. Am. Acad. Dermatol. 2019, 81, 834–846. [Google Scholar] [CrossRef] [Green Version]
- Hirase, T.; Ruff, E.; Surani, S.; Ratnani, I. Topical application of platelet-rich plasma for diabetic foot ulcers: A systematic review. World J. Diabetes 2018, 9, 172–179. [Google Scholar] [CrossRef]
- Pinto, N.R.; Ubilla, M.; Zamora, Y.; Del Rio, V.; Dohan Ehrenfest, D.M.; Quirynen, M. Leucocyte- and platelet-rich fibrin (L-PRF) as a regenerative medicine strategy for the treatment of refractory leg ulcers: A prospective cohort study. Platelets 2018, 29, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Marx, R.E.; Carlson, E.R.; Eichstaedt, R.M.; Schimmele, S.R.; Strauss, J.E.; Georgeff, K.R. Platelet-rich plasma: Growth factor enhancement for bone grafts. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1998, 85, 638–646. [Google Scholar] [CrossRef]
- Mazzucco, L.; Balbo, V.; Cattana, E.; Borzini, P. Platelet-rich plasma and platelet gel preparation using Plateltex. Vox Sang. 2008, 94, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Fadadu, P.P.; Mazzola, A.J.; Hunter, C.W.; Davis, T.T. Review of concentration yields in commercially available platelet-rich plasma (PRP) systems: A call for PRP standardization. Reg. Anesth. Pain Med. 2019, 44, 652–659. [Google Scholar] [CrossRef] [PubMed]
- Mazzocca, A.D.; McCarthy, M.B.; Chowaniec, D.M.; Cote, M.P.; Romeo, A.A.; Bradley, J.P.; Arciero, R.A.; Beitzel, K. Platelet-rich plasma differs according to preparation method and human variability. J. Bone Jt. Surg. Am. 2012, 94, 308–316. [Google Scholar] [CrossRef]
- Xiong, G.; Lingampalli, N.; Koltsov, J.C.B.; Leung, L.L.; Bhutani, N.; Robinson, W.H.; Chu, C.R. Men and Women Differ in the Biochemical Composition of Platelet-Rich Plasma. Am. J. Sports Med. 2018, 46, 409–419. [Google Scholar] [CrossRef]
- Fortier, L.A.; Barker, J.U.; Strauss, E.J.; McCarrel, T.M.; Cole, B.J. The role of growth factors in cartilage repair. Clin. Orthop. Relat. Res. 2011, 469, 2706–2715. [Google Scholar] [CrossRef] [Green Version]
- O’Shaughnessey, K.; Matuska, A.; Hoeppner, J.; Farr, J.; Klaassen, M.; Kaeding, C.; Lattermann, C.; King, W.; Woodell-May, J. Autologous protein solution prepared from the blood of osteoarthritic patients contains an enhanced profile of anti-inflammatory cytokines and anabolic growth factors. J. Orthop. Res. 2014, 32, 1349–1355. [Google Scholar] [CrossRef]
- Fitzpatrick, J.; Bulsara, M.K.; McCrory, P.R.; Richardson, M.D.; Zheng, M.H. Analysis of Platelet-Rich Plasma Extraction: Variations in Platelet and Blood Components Between 4 Common Commercial Kits. Orthop. J. Sports Med. 2017, 5, 2325967116675272. [Google Scholar] [CrossRef] [Green Version]
- Zimmermann, R.; Arnold, D.; Strasser, E.; Ringwald, J.; Schlegel, A.; Wiltfang, J.; Eckstein, R. Sample preparation technique and white cell content influence the detectable levels of growth factors in platelet concentrates. Vox Sang. 2003, 85, 283–289. [Google Scholar] [CrossRef]
- Mlynarek, R.A.; Kuhn, A.W.; Bedi, A. Platelet-Rich Plasma (PRP) in Orthopedic Sports Medicine. Am. J. Orthop. 2016, 45, 290–326. [Google Scholar]
- Moraes, V.Y.; Lenza, M.; Tamaoki, M.J.; Faloppa, F.; Belloti, J.C. Platelet-rich therapies for musculoskeletal soft tissue injuries. In Cochrane Database of Systematic Reviews; John Wiley and Sons Ltd.: Hoboken, NJ, USA, 2013; Volume 2013. [Google Scholar]
- Reurink, G.; Goudswaard, G.J.; Moen, M.H.; Weir, A.; Verhaar, J.A.; Bierma-Zeinstra, S.M.; Maas, M.; Tol, J.L. Rationale, secondary outcome scores and 1-year follow-up of a randomised trial of platelet-rich plasma injections in acute hamstring muscle injury: The Dutch Hamstring Injection Therapy study. Br. J. Sports Med. 2015, 49, 1206–1212. [Google Scholar] [CrossRef] [PubMed]
- Sandrey, M.A. Autologous growth factor injections in chronic tendinopathy. J. Athl. Train. 2014, 49, 428–430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, X.; Jones, I.A.; Park, C.; Vangsness, C.T., Jr. The Efficacy of Platelet-Rich Plasma on Tendon and Ligament Healing: A Systematic Review and Meta-analysis with Bias Assessment. Am. J. Sports Med. 2018, 46, 2020–2032. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Huang, H.; Pan, J.; Lin, J.; Zeng, L.; Liang, G.; Yang, W.; Liu, J. Meta-analysis Comparing Platelet-Rich Plasma vs Hyaluronic Acid Injection in Patients with Knee Osteoarthritis. Pain Med. 2019, 20, 1418–1429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piao, L.; Park, H.; Jo, C.H. Theoretical prediction and validation of cell recovery rates in preparing platelet-rich plasma through a centrifugation. PLoS ONE 2017, 12, e0187509. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castillo, T.N.; Pouliot, M.A.; Kim, H.J.; Dragoo, J.L. Comparison of growth factor and platelet concentration from commercial platelet-rich plasma separation systems. Am. J. Sports Med. 2011, 39, 266–271. [Google Scholar] [CrossRef]
- Trevissón, B.; Becerro-de-Bengoa-Vallejo, R.; Sevillano, D.; González, N.; Losa- Iglesias, M.; López-López, D.; Alou, L. Commercial blood cell separation systems vs tuve centrifugation methods for the prepration of platelet-rich plasma: A preliminary cross-sectional study. Rev. Assoc. Med. Bras. 2021, 67, 536–541. [Google Scholar] [CrossRef]
- Hsu, W.K.; Mishra, A.; Rodeo, S.R.; Fu, F.; Terry, M.A.; Randelli, P.; Canale, S.T.; Kelly, F.B. Platelet-rich plasma in orthopaedic applications: Evidence-based recommendations for treatment. J. Am. Acad. Orthop. Surg. 2013, 21, 739–748. [Google Scholar] [CrossRef] [Green Version]
- Evanson, J.R.; Guyton, M.K.; Oliver, D.L.; Hire, J.M.; Topolski, R.L.; Zumbrun, S.D.; McPherson, J.C.; Bojescul, J.A. Gender and age differences in growth factor concentrations from platelet-rich plasma in adults. Mil. Med. 2014, 179, 799–805. [Google Scholar] [CrossRef] [Green Version]
- Weibrich, G.; Kleis, W.K.; Hafner, G.; Hitzler, W.E. Growth factor levels in platelet-rich plasma and correlations with donor age, sex, and platelet count. J. Cranio-Maxillofac. Surg. 2002, 30, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zhang, Y.; Zhao, G.; Chen, C.; Yang, P.; Ye, S.; Tan, X. Difference in Leukocyte Composition between Women before and after Menopausal Age, and Distinct Sexual Dimorphism. PLoS ONE 2016, 11, e0162953. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldspink, G.; Harridge, S.D. Growth factors and muscle ageing. Exp. Gerontol. 2004, 39, 1433–1438. [Google Scholar] [CrossRef] [PubMed]
- Gilliver, S.C.; Ashcroft, G.S. Sex steroids and cutaneous wound healing: The contrasting influences of estrogens and androgens. Climacteric 2007, 10, 276–288. [Google Scholar] [CrossRef]
- Payne, K.A.; Didiano, D.M.; Chu, C.R. Donor sex and age influence the chondrogenic potential of human femoral bone marrow stem cells. Osteoarthr. Cartil. 2010, 18, 705–713. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ashcroft, G.S.; Dodsworth, J.; van Boxtel, E.; Tarnuzzer, R.W.; Horan, M.A.; Schultz, G.S.; Ferguson, M.W. Estrogen accelerates cutaneous wound healing associated with an increase in TGF-beta1 levels. Nat. Med. 1997, 3, 1209–1215. [Google Scholar] [CrossRef]
- Hirokawa, K.; Utsuyama, M.; Hayashi, Y.; Kitagawa, M.; Makinodan, T.; Fulop, T. Slower immune system aging in women versus men in the Japanese population. Immun. Ageing 2013, 10, 19. [Google Scholar] [CrossRef] [Green Version]
- Bain, B.J. Ethnic and sex differences in the total and differential white cell count and platelet count. J. Clin. Pathol. 1996, 49, 664–666. [Google Scholar] [CrossRef]
- Lin, Y.; Kim, J.; Metter, E.J.; Nguyen, H.; Truong, T.; Lustig, A.; Ferrucci, L.; Weng, N.P. Changes in blood lymphocyte numbers with age in vivo and their association with the levels of cytokines/cytokine receptors. Immun. Ageing 2016, 13, 24. [Google Scholar] [CrossRef] [Green Version]
- Larsson, S.; Nordenson, A.; Glader, P.; Yoshihara, S.; Lindén, A.; Slinde, F. A gender difference in circulating neutrophils in malnourished patients with COPD. Int. J. Chronic Obstruct. Pulmon. Dis. 2011, 6, 83–88. [Google Scholar] [CrossRef] [Green Version]
- Kobayashi, Y.; Saita, Y.; Nishio, H.; Ikeda, H.; Takazawa, Y.; Nagao, M.; Takaku, T.; Komatsu, N.; Kaneko, K. Leukocyte concentration and composition in platelet-rich plasma (PRP) influences the growth factor and protease concentrations. J. Orthop. Sci. 2016, 21, 683–689. [Google Scholar] [CrossRef] [PubMed]
- Wilgus, T.A.; Roy, S.; McDaniel, J.C. Neutrophils and Wound Repair: Positive Actions and Negative Reactions. Adv. Wound Care 2013, 2, 379–388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moojen, D.J.; Everts, P.A.; Schure, R.M.; Overdevest, E.P.; van Zundert, A.; Knape, J.T.; Castelein, R.M.; Creemers, L.B.; Dhert, W.J. Antimicrobial activity of platelet-leukocyte gel against Staphylococcus aureus. J. Orthop. Res. 2008, 26, 404–410. [Google Scholar] [CrossRef] [PubMed]
- Falanga, V. Wound healing and its impairment in the diabetic foot. Lancet 2005, 366, 1736–1743. [Google Scholar] [CrossRef]
- Kalan, L.R.; Meisel, J.S.; Loesche, M.A.; Horwinski, J.; Soaita, I.; Chen, X.; Uberoi, A.; Gardner, S.E.; Grice, E.A. Strain- and Species-Level Variation in the Microbiome of Diabetic Wounds Is Associated with Clinical Outcomes and Therapeutic Efficacy. Cell Host Microbe 2019, 25, 641.e5–655.e5. [Google Scholar] [CrossRef]
- Molloy, E.J.; O’Neill, A.J.; Grantham, J.J.; Sheridan-Pereira, M.; Fitzpatrick, J.M.; Webb, D.W.; Watson, R.W. Sex-specific alterations in neutrophil apoptosis: The role of estradiol and progesterone. Blood 2003, 102, 2653–2659. [Google Scholar] [CrossRef] [Green Version]
- Gubbels Bupp, M.R. Sex, the aging immune system, and chronic disease. Cell. Immunol. 2015, 294, 102–110. [Google Scholar] [CrossRef]
| Male Group n = 13 | Female Group n = 13 | p Value | ||||||
|---|---|---|---|---|---|---|---|---|
| Blood Cell Line | Mean ± SD (Range) | Median (IQR) | SW * | Mean ± SD (Range) | Median (IQR) | SW * | ||
| Platelets | WB | 252.00 ± 81.88 (161.00–382.00) | 228.00 [158.00] | 0.081 | 198.60 ± 72.39 (56.00–334.00) | 188.00 [104.80] | 0.731 | 0.097 b |
| PRP product | 926.00 ± 222.40 (462.70–1222.00) | 945.00 [337.50] | 0.760 | 757.10 ± 329.60 (359.00–1317.00) | 674.90 [602.80] | 0.177 | 0.159 b | |
| WBCs | WB | 7.99 ± 1.97 (1.02–11.70) | 7.53 [3.09] | 0.466 | 7.06 ± 2.88 (3.90–14.80) | 6.35 [3.02] | 0.029 | 0.171 a |
| PRP product | 14.55 ± 4.72 (4.59–24.00) | 13.80 [5.43] | 0.092 | 12.67 ± 5.29 (7.08–23.64) | 9.48 [9.15] | 0.036 | 0.180 a | |
| Neutrophils | WB | 4.83 ± 1.66 (2.26–8.70) | 4.93 [3.03] | 0.737 | 3.47 ± 1.57 (1.81–6.59) | 2.81 [2.30] | 0.025 | 0.035 a |
| PRP product | 8.33 ± 1.60 (4.08–16.99) | 8.12 [3.46] | 0.313 | 5.98 ± 2.70 (2.36–11.70) | 5.51 [3.46] | 0.277 | 0.018 b | |
| Lymphocytes | WB | 1.94 ± 0.85 (0.77–3.06) | 1.93 [1.66] | 0.196 | 2.19 ± 1.15 (0.72–5.45) | 2.20 [1.27] | 0.026 | 0.848 a |
| PRP product | 5.23 ± 1.68 (3.67–8.26) | 4.88 [2.79] | 0.014 | 4.99 ± 2.48 (2.23–11.98) | 4.34 [2.89] | 0.014 | 0.460 a | |
| Monocytes | WB | 0.58 ± 0.17 (0.31–0.84) | 0.57 [0.27] | 0.721 | 0.45 ± 0.15 (0.20–0.73) | 0.45 [0.25] | 0.956 | 0.042 b |
| PRP product | 1.07 ± 0.31 (0.67–1.60) | 0.97 [0.63] | 0.351 | 1.08 ± 0.50 (0.41–2.24) | 0.91 [0.79] | 0.207 | 0.947 b | |
| Male Volunteers | Female Volunteers | |||||||
|---|---|---|---|---|---|---|---|---|
| Blood Cell Line | ≤50 Years (n = 5) a | >50 Years (n = 8) b | ≤50 Years (n = 5) c | >50 Years (n = 8) d | ||||
| WB | PRP Product | WB | PRP Product | WB | PRP Product | WB | PRP Product | |
| Platelets | 269.40 ± 97.17 228.00 [186.50] | 1026.00 ± 197.10 1096.00 [374.20] | 237.50 ± 72.79 212.00 [132.80] | 842.40 ± 222.30 911.30 [383.80] | 236.40 ± 72.73 207 [133.50] | 905.10 ± 292.40 902.40 [540.50] | 177.70 ± 66.96 173.00 [77.50] | 674.80 ± 335.30 624.00 [534.00] |
| WBCs | 8.44 ± 2.36 & 8.10 [4.46] | 16.43 ±6.68 & 16.20 [13.24] | 7.62 ± 1.73 7.52 [3.38] | 13.00 ± 1.54 + 13.42 [3.01] | 9.03 ± 3.44 * 7.60 [5.52] | 15.86 ± 4.42 17.40 [7.68] | 5.96 ± 1.95 5.60 [2.33] | 10.90 ± 5.08 9.48 [3.49] |
| Neutrophils | 4.45 ± 2.07 & 3.95 [4.00] | 9.64 ± 1.14 &&,** 10.14 [2.12] | 5.14 ± 1.35 +++ 5.04 [2.35] | 7.24 ± 0.97 6.86 [1.80] | 5.27 ± 1.15 ** 4.90 [2.23] | 6.91 ± 2.68 6.24 [4.97] | 2.47 ± 0.43 2.40 [0.65] | 5.46 ± 2.72 4.39 [2.84] |
| Lymphocytes | 2.56 ± 0.48 *,& 2.70 [0.93] | 6.37 ± 1.93 * 6.75 [3.76] | 1.42 ± 0.73 & 1.25 [0.80] | 4.29 ± 0.56 & 4.08 [1.04] | 3.01 ± 1.43 * 2.50 [2.19] | 7.23 ± 2.84 ** 6.23 [4.40] | 1.73 ± 0.70 1.70 [1.19] | 3.74 ± 1.04 3.64 [1.34] |
| Monocytes | 0.63 ± 0.22 & 0.61 [0.40] | 0.96 ± 0.34 0.78 [0.57] | 0.54 ± 0.11 + 0.53 [0.18] | 1.17 ± 0.28 1.06 [0.51] | 0.58 ± 0.11 ** 0.61 [0.22] | 1.32 ± 0.34 1.24 [0.60] | 0.37 ± 0.11 0.35 [0.17] | 0.95 ± 0.54 0.76 [0.64] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trevissón, B.; Becerro-de-Bengoa-Vallejo, R.; Sevillano, D.; González, N.; Losa-Iglesias, M.E.; López-López, D.; Alou, L. Influence of Sexual Dimorphism, Aging, and Differential Cell Capture Efficiency of Blood Separation Systems on the Quality of Platelet-Rich Plasma. J. Clin. Med. 2022, 11, 1683. https://doi.org/10.3390/jcm11061683
Trevissón B, Becerro-de-Bengoa-Vallejo R, Sevillano D, González N, Losa-Iglesias ME, López-López D, Alou L. Influence of Sexual Dimorphism, Aging, and Differential Cell Capture Efficiency of Blood Separation Systems on the Quality of Platelet-Rich Plasma. Journal of Clinical Medicine. 2022; 11(6):1683. https://doi.org/10.3390/jcm11061683
Chicago/Turabian StyleTrevissón, Bibiana, Ricardo Becerro-de-Bengoa-Vallejo, David Sevillano, Natalia González, Marta Elena Losa-Iglesias, Daniel López-López, and Luis Alou. 2022. "Influence of Sexual Dimorphism, Aging, and Differential Cell Capture Efficiency of Blood Separation Systems on the Quality of Platelet-Rich Plasma" Journal of Clinical Medicine 11, no. 6: 1683. https://doi.org/10.3390/jcm11061683
APA StyleTrevissón, B., Becerro-de-Bengoa-Vallejo, R., Sevillano, D., González, N., Losa-Iglesias, M. E., López-López, D., & Alou, L. (2022). Influence of Sexual Dimorphism, Aging, and Differential Cell Capture Efficiency of Blood Separation Systems on the Quality of Platelet-Rich Plasma. Journal of Clinical Medicine, 11(6), 1683. https://doi.org/10.3390/jcm11061683







