Clinical Outcomes after Surgical Resection Combined with Brachytherapy for Uveal Melanomas
Abstract
:1. Introduction
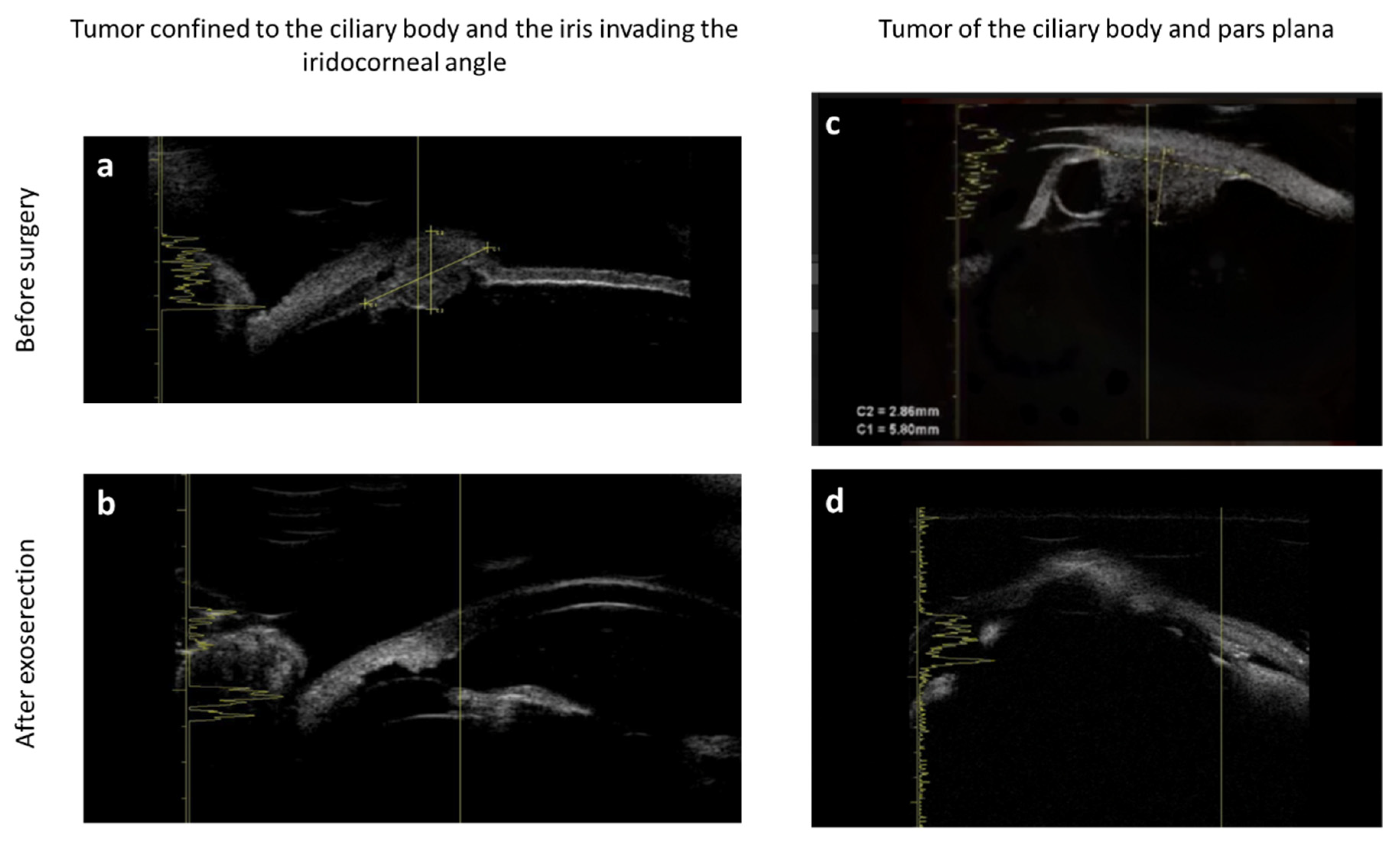
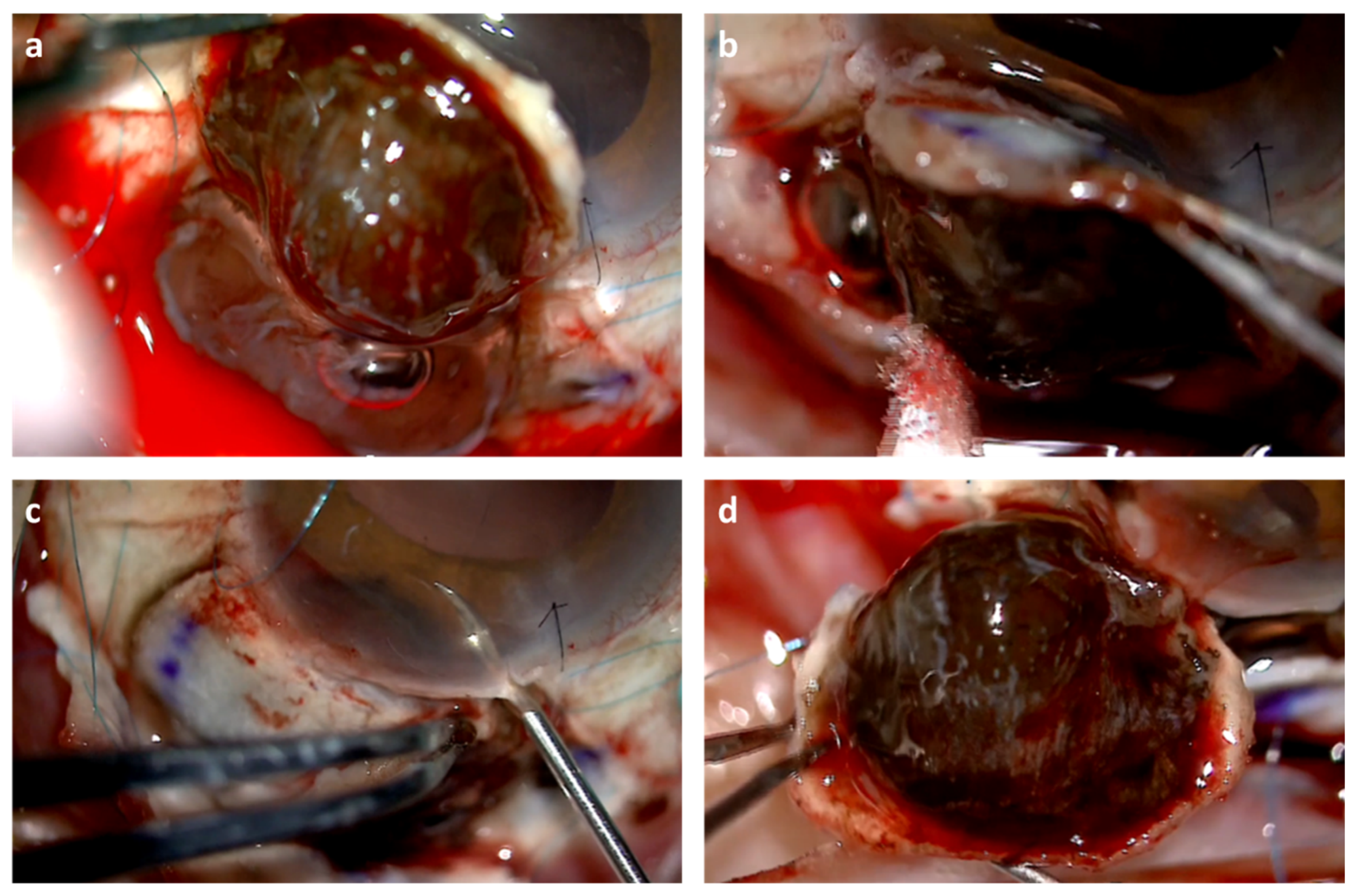
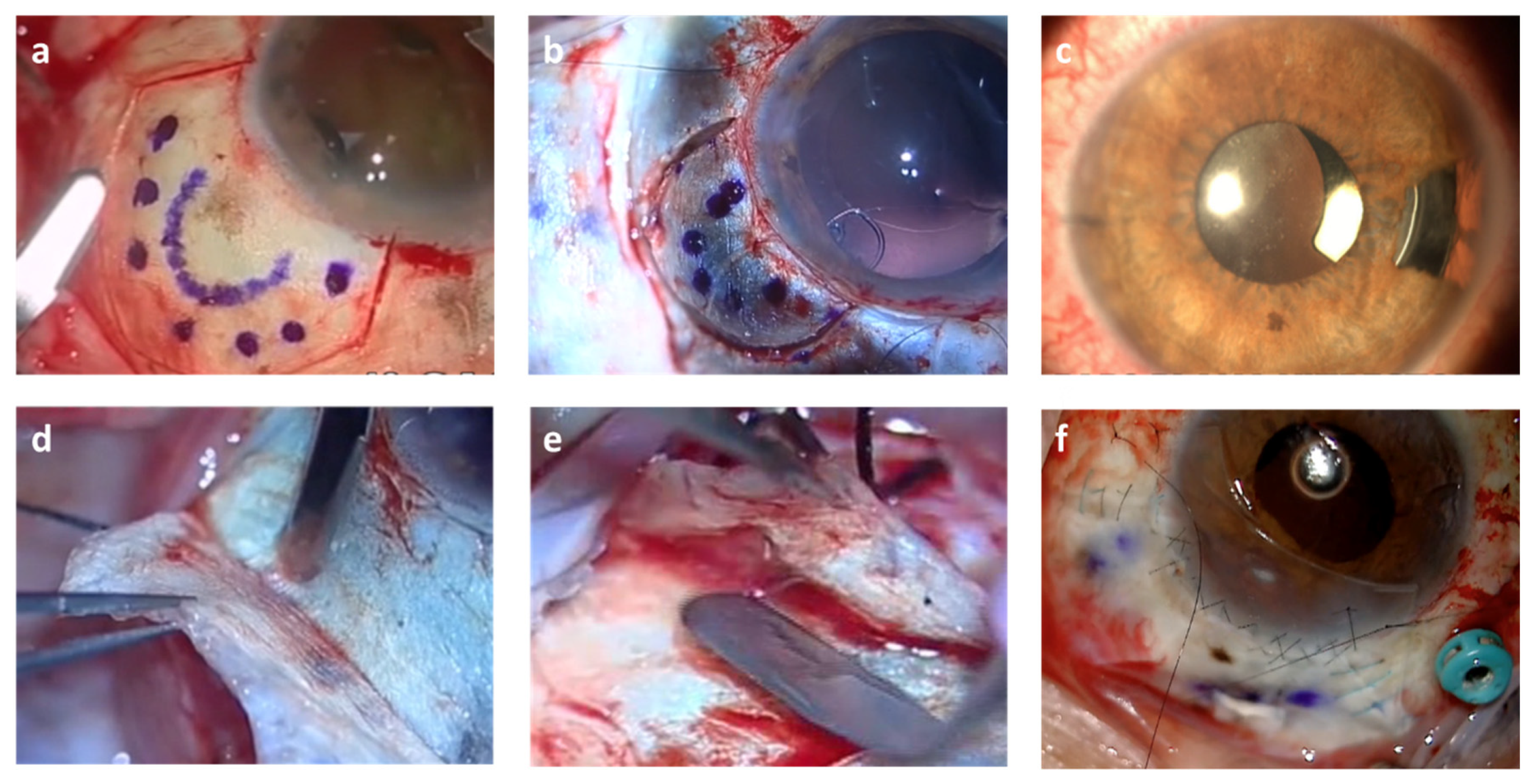
2. Methods
2.1. Procedures
2.2. Follow-Up
2.3. Ethics
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jensen, A.W.; Petersen, I.A.; Kline, R.W.; Stafford, S.L.; Schomberg, P.J.; Robertson, D.M. Radiation complications and tumor control after 125i plaque brachytherapy for ocular melanoma. Int. J. Radiat. Oncol. Biol. Phys. 2005, 63, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Sieving, P.A. Fifteen years of work: The coms outcomes for medium-sized choroidal melanoma. Arch. Ophthalmol. 2001, 119, 1067–1068. [Google Scholar] [CrossRef] [PubMed]
- Popovic, M.; Ahmed, I.I.K.; DiGiovanni, J.; Shields, C.L. Radiotherapeutic and surgical management of iris melanoma: A review. Surv. Ophthalmol. 2017, 62, 302–311. [Google Scholar] [CrossRef] [PubMed]
- Xu, T.T.; Pulido, J.S.; Deufel, C.L.; Corbin, K.S.; Petersen, I.A.; Dalvin, L.A. Clinical outcomes of modified collaborative ocular melanoma study iris plaques for treatment of iris, iridociliary, and ciliary body melanoma. Eye 2021, 35, 2754–2762. [Google Scholar] [CrossRef] [PubMed]
- Gündüz, K.; Bechrakis, N.E. Exoresection and endoresection for uveal melanoma. Middle East Afr. J. Ophthalmol. 2010, 17, 210–216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jager, M.J.; Shields, C.L.; Cebulla, C.M.; Abdel-Rahman, M.H.; Grossniklaus, H.E.; Stern, M.H.; Carvajal, R.D.; Belfort, R.N.; Jia, R.; Shields, J.A.; et al. Uveal melanoma. Nat. Rev. Dis. Primers 2020, 6, 24. [Google Scholar] [CrossRef] [PubMed]
- Damato, B. Ocular treatment of choroidal melanoma in relation to the prevention of metastatic death—A personal view. Prog. Retin. Eye Res. 2018, 66, 187–199. [Google Scholar] [CrossRef]
- Relimpio-López, M.I.; Garrido-Hermosilla, A.M.; Espejo-Arjona, F.; Coca-Gutiérrez, L.M.; Díaz-Granda, M.J.; Rodríguez-de-la-Rúa-Franch, E. Sclerouvectomy plus intraoperative ophthalmic brachytherapy for iris-ciliary body melanomas. Surg. Oncol. 2021, 36, 113–114. [Google Scholar] [CrossRef] [PubMed]
- Amin, M.B.; Edge, S.B.; Greene, F.L.; Byrd, D.R.; Brookland, R.K.; Washington, M.K.; Gershenwald, J.E.; Compton, C.C.; Hess, K.R.; Sullivan, D.C.; et al. Ajcc Cancer Staging Manual; Springer: New York, NY, USA, 2017; pp. 805–817. [Google Scholar]
- Groenewald, C.; Konstantinidis, L.; Damato, B. Effects of radiotherapy on uveal melanomas and adjacent tissues. Eye 2013, 27, 163–171. [Google Scholar] [CrossRef]
- Toivonen, P.; Kivela, T. Pigmented episcleral deposits after brachytherapy of uveal melanoma. Ophthalmology 2006, 113, 865–873. [Google Scholar] [CrossRef]
- Damato, B. The role of eyewall resection in uveal melanoma management. Int. Ophthalmol. Clin. 2006, 46, 81–93. [Google Scholar] [CrossRef] [PubMed]
- The american brachytherapy society consensus guidelines for plaque brachytherapy of uveal melanoma and retinoblastoma. Brachytherapy 2014, 13, 1–14. [CrossRef] [PubMed] [Green Version]
- Schulze-Bonsel, K.; Feltgen, N.; Burau, H.; Hansen, L.; Bach, M. Visual acuities “hand motion” and “counting fingers” can be quantified with the freiburg visual acuity test. Investig. Ophthalmol. Vis. Sci. 2006, 47, 1236–1240. [Google Scholar] [CrossRef] [PubMed]
- Karimi, S.; Arabi, A.; Shahraki, T. Plaque brachytherapy in iris and iridociliary melanoma: A systematic review of efficacy and complications. J. Contemp. Brachyther. 2021, 13, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Torkashvand, A.; Riazi-Esfahani, H.; Ghassemi, F.; Khalili Pour, E.; Masoomian, B.; Zarei, M.; Fadakar, K.; Arjmand, M.; Tayebi, F.; Ekradi, L.; et al. Evaluation of radiation maculopathy after treatment of choroidal melanoma with ruthenium-106 using optical coherence tomography angiography. BMC Ophthalmol. 2021, 21, 385. [Google Scholar] [CrossRef] [PubMed]
- Karimi, S.; Arabi, A.; Siavashpour, Z.; Shahraki, T.; Ansari, I. Efficacy and complications of ruthenium-106 brachytherapy for uveal melanoma: A systematic review and meta-analysis. J. Contemp. Brachyther. 2021, 13, 358–364. [Google Scholar] [CrossRef] [PubMed]
- Shields, J.A.; Shields, C.L. Surgical approach to lamellar sclerouvectomy for posterior uveal melanomas: The 1986 schoenberg lecture. Ophthalmic Surg. 1988, 19, 774–780. [Google Scholar] [CrossRef] [PubMed]
- Mirzayev, I.; Gündüz, A.K.; Okçu Heper, A. Partial lamellar sclerouvectomy surgery for anteriorly located uveal tumour resection: A 20-year experience. Eye 2021. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.K., Jr.; Di Nicola, M. Ocular oncology-primary and metastatic malignancies. Med. Clin. N. Am. 2021, 105, 531–550. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, T.M.; Walter, S.D.; Mruthyunjaya, P. Pigmented iridociliary lesion and increased intraocular pressure. JAMA Ophthalmol. 2017, 135, 805–806. [Google Scholar] [CrossRef]
- Damato, B.E. Local resection of uveal melanoma. Dev. Ophthalmol. 2012, 49, 66–80. [Google Scholar] [CrossRef] [PubMed]
- Branisteanu, D.C.; Bogdanici, C.M.; Branisteanu, D.E.; Maranduca, M.A.; Zemba, M.; Balta, F.; Branisteanu, C.I.; Moraru, A.D. Uveal melanoma diagnosis and current treatment options (review). Exp. Ther. Med. 2021, 22, 1428. [Google Scholar] [CrossRef] [PubMed]
- Konstantinidis, L.; Groenewald, C.; Coupland, S.E.; Damato, B. Trans-scleral local resection of toxic choroidal melanoma after proton beam radiotherapy. Br. J. Ophthalmol. 2014, 98, 775–779. [Google Scholar] [CrossRef] [PubMed]
- Damato, B.; Groenewald, C.; McGalliard, J.; Wong, D. Endoresection of choroidal melanoma. Br. J. Ophthalmol. 1998, 82, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Walter, S.D.; Chao, D.L.; Feuer, W.; Schiffman, J.; Char, D.H.; Harbour, J.W. Prognostic implications of tumor diameter in association with gene expression profile for uveal melanoma. JAMA Ophthalmol. 2016, 134, 734–740. [Google Scholar] [CrossRef] [Green Version]
- Stewart, F.A.; Akleyev, A.V.; Hauer-Jensen, M.; Hendry, J.H.; Kleiman, N.J.; Macvittie, T.J.; Aleman, B.M.; Edgar, A.B.; Mabuchi, K.; Muirhead, C.R.; et al. Icrp publication 118: Icrp statement on tissue reactions and early and late effects of radiation in normal tissues and organs--threshold doses for tissue reactions in a radiation protection context. Ann. ICRP 2012, 41, 1–322. [Google Scholar] [CrossRef]


| Variable | Total Sample * (n = 35) | Brachytherapy + Surgery * (n = 26) | Brachytherapy Alone * (n = 9) | p Value ¶ |
|---|---|---|---|---|
| Gender (male) | 16 (45.7%) | 12 (46%) | 4 (44.4%) | 0.62 |
| Age (years) | 58.0 (15) | 57.3 (15.5) | 60 (13.9) | 0.86 |
| Operated eye (right) | 13 (37%) | 9 (34.6%) | 4 (44.4%) | 0.69 |
| Anatomical extension: | ||||
| Iris | 26 (74.3%) | 24 (92%) | 2 (22%) | <0.001 |
| Ciliary body | 28 (80%) | 20 (77%) | 8 (89%) | 0.64 |
| Choroid | 2 (5.7%) | 1 (4%) | 1 (11%) | 0.45 |
| Anatomical extension groups: | <0.001 | |||
| Iris only | 6 (17%) | 6 (23%) | 0 (0%) | |
| Iris and ciliary body | 20 (57%) | 18 (69%) | 2 (22%) | |
| Ciliary body only | 7 (20%) | 1 (4%) | 6 (66.7%) | |
| Ciliary body and choroid | 1 (3%) | 1 (4%) | 0 (0%) | |
| Choroid only | 1 (3%) | 0 (0%) | 1 (11%) | |
| Radial size (mm) | 6.6 (2.3) | 6.1 (1.6) | 8.2 (3.3) | 0.17 |
| Circumferential size (mm) | 7.1 (2.4) | 6.5 (1.8) | 9.0 (3.2) | 0.022 |
| Apex height (mm) | 2.6 (1.5) | 2.2 (1.0) | 4.2 (1.8) | <0.001 |
| Retinal surface (%) | 3.1 (2.4) | 2.5 (1.6) | 5.0 (3.6) | 0.044 |
| T Staging ‡: | 0.579 | |||
| T1 | 9 (25.7%) | 7 (27%) | 2 (22%) | |
| T2 | 26 (74.3%) | 19 (73%) | 7 (78%) |
| Variable | Total Sample * (n = 35) | Brachytherapy + Surgery * (n = 26) | Brachytherapy Alone * (n = 9) | p Value ¶ |
|---|---|---|---|---|
| Isotope used: | 0.013 | |||
| Ru-106 | 32 (91.4%) | 26 (100%) | 6 (66.7%) | |
| I-125 | 3 (8.6%) | 0 (0%) | 3 (33.3%) | |
| Dose in sclera (Gy) | 350.4 (182.9) | 294.2 (118.9) | 512.6 (241.3) | <0.001 |
| Dose in sclera according to COMS study (Gy) † | 247.9 (124.5) | 205.5 (73.8) | 370.7 (161.5) | <0.001 |
| Optic nerve dose, n = 4 (Gy) | 12.1 (8.4) | 9.3 (13.1) | 14.8 (2.9) | 0.99 |
| Dose in the macula, n = 3 (Gy) | 19.9 (4.0) | 23.2 | 18.3 (4.1) | 0.67 |
| Lens dose (Gy) | 20.3 (14.0) | 15.6 (7.9) | 33.7 (19.2) | 0.023 |
| Dose to opposite retina, n = 3 (Gy) | 12.4 (1.8) | 13.2 | 12.1 (2.4) | 0.99 |
| Outcome after brachytherapy: | ||||
| Enucleation | 3 (8.6%) | 2 (7.7%) | 1 (11%) | 0.6 |
| Local tumor recurrence | 3 (8.6%) | 0 (0%) | 3 (33.3%) | 0.013 |
| Variable | Total Sample * (n = 35) | Brachytherapy + Surgery * (n = 26) | Brachytherapy Alone * (n = 9) | p Value ¶ |
|---|---|---|---|---|
| Follow-up time (years) | 5.9 (3.0) | 5.7 (1.9) | 6.5 (5.1) | 0.59 |
| Relapse | 3 (8.5%) | 0 (0%) | 3 (33.3%) | 0.013 |
| Metastasis | 1 (3%) | 1 (4%) | 0 (0%) | 0.74 |
| Initial visual acuity | 0.6 (0.2) | 0.6 (0.3) | 0.6 (0.1) | 0.53 |
| Visual acuity at 3 months | 0.4 (0.2) | 0.4 (0.2) | 0.3 (0.3) | 0.65 |
| Visual acuity at 6 months | 0.3 (0.3) | 0.4 (0.3) | 0.1 (0.2) | 0.06 |
| Visual acuity at 12 months | 0.3 (0.3) | 0.4 (0.3) | 0.1 (0.2) | 0.025 |
| Visual acuity at 36 months | 0.3 (0.3) | 0.3 (0.4) | 0.3 | 0.9 |
| Visual acuity at the end of follow-up | 0.3 (0.3) | 0.4 (0.3) | 0.07 (0.1) | 0.07 |
| Complications: | ||||
| Scleromalacia | 14 (40%) | 12 (46%) | 2 (22%) | 0.26 |
| Bullous keratopathy | 11 (31.4%) | 9 (34.6%) | 2 (22%) | 0.68 |
| Retinal toxicity | 11 (31.4%) | 8 (31%) | 3 (33.3%) | 0.13 |
| Cataracts | 9 (25.7%) | 5 (19%) | 4 (44.4%) | 0.19 |
| Hypotonia | 7 (20%) | 5 (19%) | 2 (22%) | 0.59 |
| Photophobia | 5 (14.3%) | 2 (7.7%) | 1 (11%) | 0.6 |
| Glaucoma | 3 (8.6%) | 5 (19%) | 0 (0%) | 0.29 |
| Infection | 1 (3%) | 1 (4%) | 0 (0%) | 0.74 |
| Irreducible retinal detachment | 1 (3%) | 1 (4%) | 0 (0%) | 0.74 |
| Others | 19 (54.3%) | 16 (61.5%) | 3 (33.3%) | 0.24 |
| Survival: | 0.99 | |||
| At five years | 35 (100%) | 26 (100%) | 9 (100%) | |
| At seven years | 35 (100%) | 26 (100%) | 9 (100%) | |
| At 10 years | 34 (97%) | 25 (96%) | 9 (100%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Relimpio-López, I.; Garrido-Hermosilla, A.M.; Espejo, F.; Gessa-Sorroche, M.; Coca, L.; Domínguez, B.; Díaz-Granda, M.J.; Ponte, B.; Cano, M.J.; Rodríguez de la Rúa, E.; et al. Clinical Outcomes after Surgical Resection Combined with Brachytherapy for Uveal Melanomas. J. Clin. Med. 2022, 11, 1616. https://doi.org/10.3390/jcm11061616
Relimpio-López I, Garrido-Hermosilla AM, Espejo F, Gessa-Sorroche M, Coca L, Domínguez B, Díaz-Granda MJ, Ponte B, Cano MJ, Rodríguez de la Rúa E, et al. Clinical Outcomes after Surgical Resection Combined with Brachytherapy for Uveal Melanomas. Journal of Clinical Medicine. 2022; 11(6):1616. https://doi.org/10.3390/jcm11061616
Chicago/Turabian StyleRelimpio-López, Isabel, Antonio Manuel Garrido-Hermosilla, Francisco Espejo, María Gessa-Sorroche, Lourdes Coca, Belen Domínguez, María Jesús Díaz-Granda, Beatriz Ponte, María José Cano, Enrique Rodríguez de la Rúa, and et al. 2022. "Clinical Outcomes after Surgical Resection Combined with Brachytherapy for Uveal Melanomas" Journal of Clinical Medicine 11, no. 6: 1616. https://doi.org/10.3390/jcm11061616
APA StyleRelimpio-López, I., Garrido-Hermosilla, A. M., Espejo, F., Gessa-Sorroche, M., Coca, L., Domínguez, B., Díaz-Granda, M. J., Ponte, B., Cano, M. J., Rodríguez de la Rúa, E., Carrasco-Peña, F., Míguez, C., Saavedra, J., Ontanilla, A., Caparrós-Escudero, C., Ríos, J. J., & Terrón, J. A. (2022). Clinical Outcomes after Surgical Resection Combined with Brachytherapy for Uveal Melanomas. Journal of Clinical Medicine, 11(6), 1616. https://doi.org/10.3390/jcm11061616






