Outcome-Affecting Parameters of Hip Arthroscopy for Femoroacetabular Impingement with Concomitant Cartilage Damage—Data Analysis from the German Cartilage Registry
Abstract
:1. Introduction
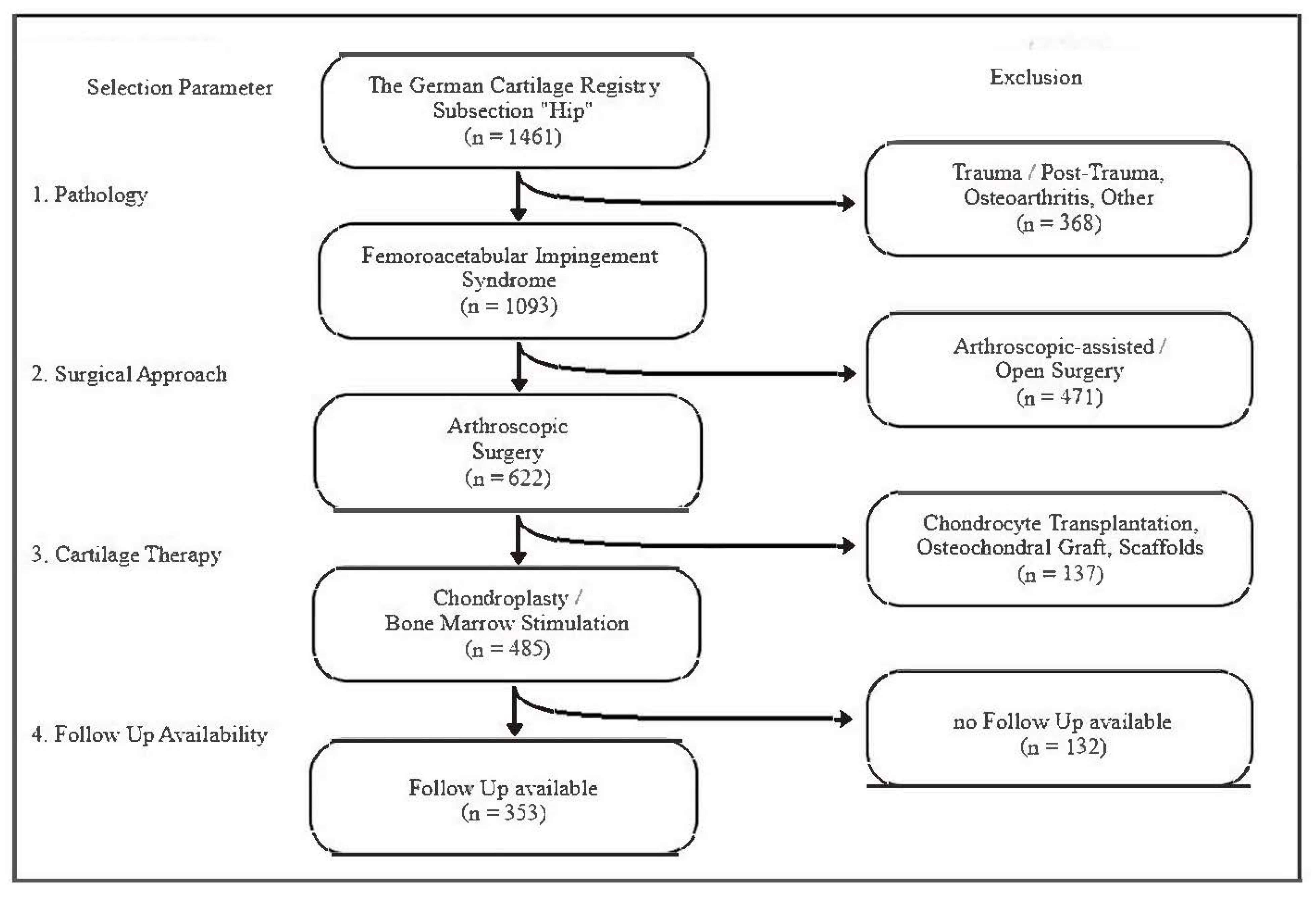
2. Materials and Methods
3. Results
3.1. Study Collective and Patient Demographics
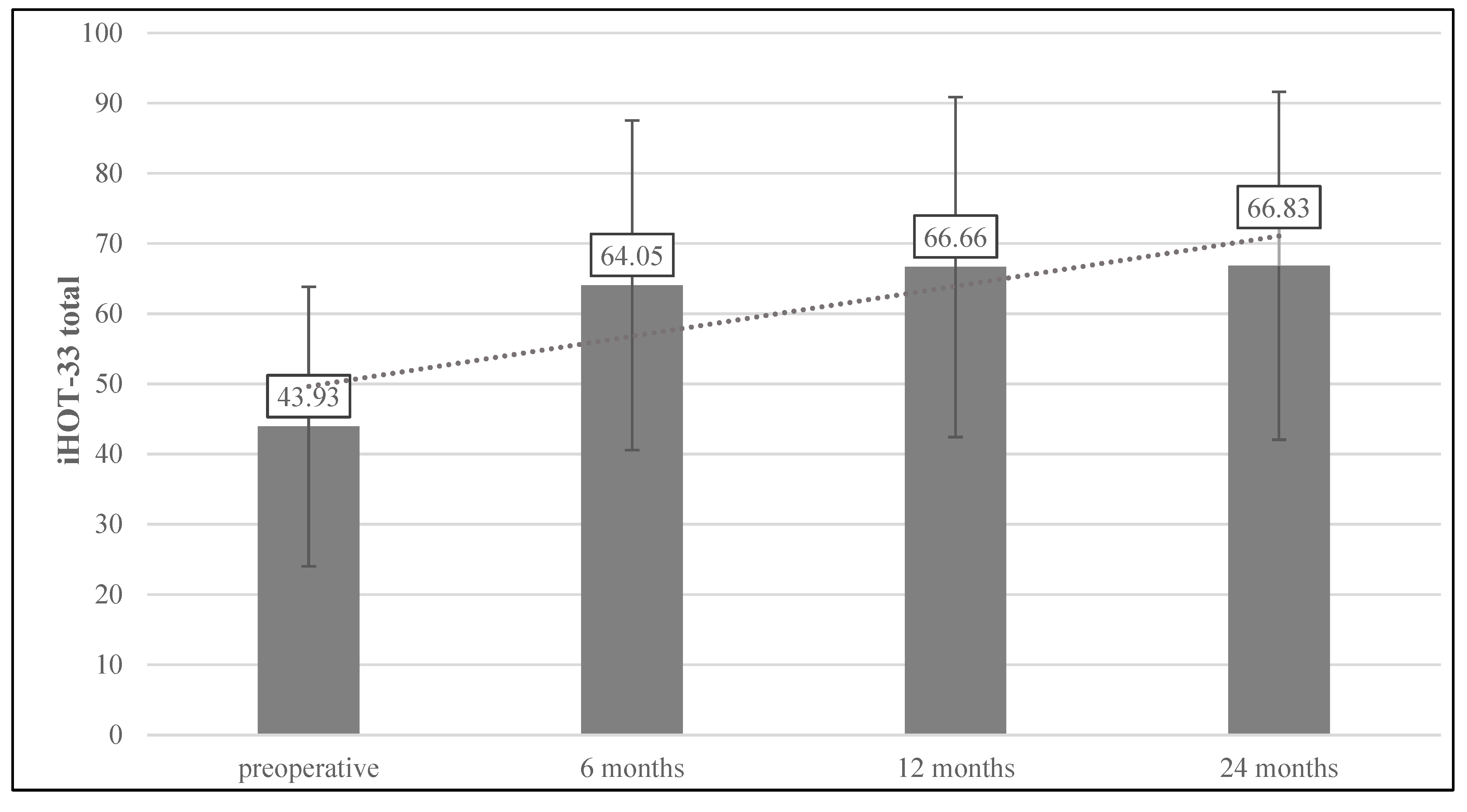
3.2. Functional Outcomes
3.3. Revision Surgery
3.4. Multiple Regression Analysis of Factors Potentially Affecting the Postoperative iHOT-33
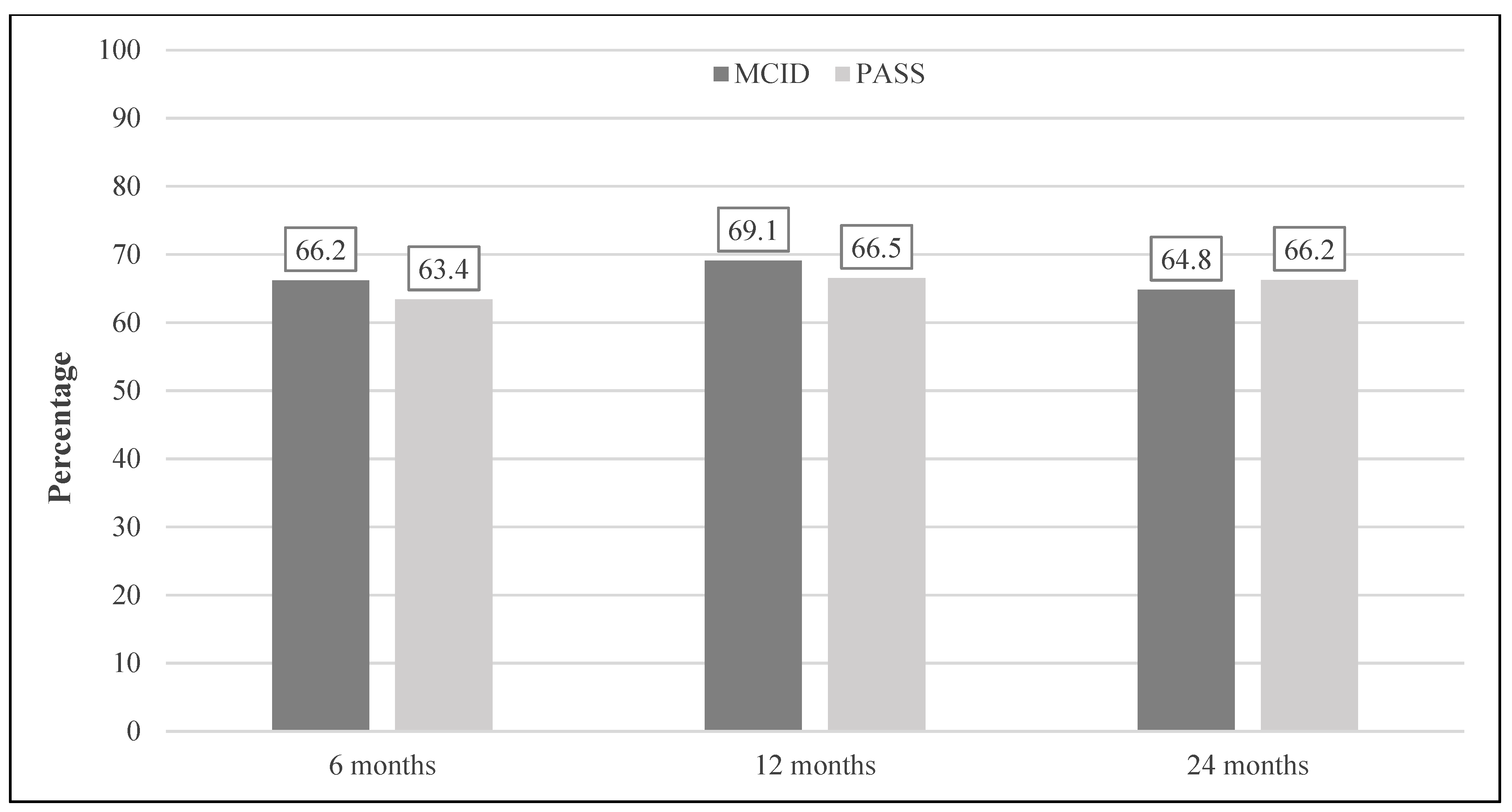
3.5. Binary Logistic Regression Analysis of Factors and Achievement of the MCID and the PASS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Leunig, M.; Beaulé, P.E.; Ganz, R. The Concept of Femoroacetabular Impingement: Current Status and Future Perspectives. Clin. Orthop. Relat. Res. 2009, 467, 616–622. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beck, M.; Kalhor, M.; Leunig, M.; Ganz, R. Hip morphology influences the pattern of damage to the acetabular cartilage. J. Bone Jt. Surg. 2005, 87, 1012–1018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agricola, R.; Heijboer, M.P.; Bierma-Zeinstra, S.M.A.; Verhaar, J.A.N.; Weinans, H.; Waarsing, J.H. Cam impingement causes osteoarthritis of the hip: A nationwide prospective cohort study (CHECK). Ann. Rheum. Dis. 2013, 72, 918–923. [Google Scholar] [CrossRef] [PubMed]
- Clohisy, J.C.; Dobson, M.A.; Robison, J.F.; Warth, L.C.; Zheng, J.; Liu, S.S.; Yehyawi, T.M.; Callaghan, J.J. Radiographic Structural Abnormalities Associated with Premature, Natural Hip-Joint Failure. J. Bone Jt. Surg. 2011, 93, 3–9. [Google Scholar] [CrossRef] [Green Version]
- Fayad, T.E.; Khan, M.A.A.; Haddad, F.S. Femoroacetabular impingement. Bone Jt. J. 2013, 95, 26–30. [Google Scholar] [CrossRef] [Green Version]
- Minkara, A.A.; Westermann, R.; Rosneck, J.; Lynch, T.S. Systematic Review and Meta-analysis of Outcomes after Hip Arthroscopy in Femoroacetabular Impingement. Am. J. Sports Med. 2019, 47, 488–500. [Google Scholar] [CrossRef]
- Claßen, T.; Körsmeier, K.; Kamminga, M.; Beck, S.; Rekowski, J.; Jäger, M.; Landgraeber, S. Is early treatment of cam-type femoroacetabular impingement the key to avoiding associated full thickness isolated chondral defects? Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2332–2337. [Google Scholar] [CrossRef]
- Migliorini, F.; Maffulli, N. Arthroscopic Management of Femoroacetabular Impingement in Adolescents: A Systematic Review. Am. J. Sports Med. 2021, 49, 3708–3715. [Google Scholar] [CrossRef]
- Griffin, D.R.; Dickenson, E.J.; Wall, P.; Achana, F.; Donovan, J.L.; Griffin, J.; Hobson, R.; Hutchinson, C.E.; Jepson, M.; Parsons, N.; et al. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): A multicentre randomised controlled trial. Lancet 2018, 391, 2225–2235. [Google Scholar] [CrossRef]
- Sogbein, O.A.; Shah, A.; Kay, J.; Memon, M.; Simunovic, N.; Belzile, E.L.; Ayeni, O.R. Predictors of Outcomes After Hip Arthroscopic Surgery for Femoroacetabular Impingement: A Systematic Review. Orthop. J. Sports Med. 2019, 7, 2325967119848982. [Google Scholar] [CrossRef]
- Cvetanovich, G.L.; Weber, A.E.; Kuhns, B.; Alter, J.; Harris, J.D.; Mather, I.R.C.; Nho, S.J. Hip Arthroscopic Surgery for Femoroacetabular Impingement with Capsular Management: Factors Associated with Achieving Clinically Significant Outcomes. Am. J. Sports Med. 2017, 46, 288–296. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Redmond, J.M.; Stake, C.E.; Dunne, K.F.; Domb, B.G. Does Primary Hip Arthroscopy Result in Improved Clinical Outcomes? 2-Year Clinical Follow-up on a Mixed Group of 738 Consecutive Primary Hip Arthroscopies Performed at a High-Volume Referral Center. Am. J. Sports Med. 2015, 44, 74–82. [Google Scholar] [CrossRef] [PubMed]
- Nwachukwu, B.U.; Chang, B.; Fields, K.; Rebolledo, B.J.; Nawabi, D.H.; Kelly, B.T.; Ranawat, A.S. Defining the “Substantial Clinical Benefit” After Arthroscopic Treatment of Femoroacetabular Impingement. Am. J. Sports Med. 2017, 45, 1297–1303. [Google Scholar] [CrossRef] [PubMed]
- Frank, R.M.; Lee, S.; Bush-Joseph, C.A.; Salata, M.J.; Mather, R.C.; Nho, S.J. Outcomes for Hip Arthroscopy According to Sex and Age. A Comparative Matched-Group Analysis. J. Bone Jt. Surg. 2016, 98, 797–804. [Google Scholar] [CrossRef]
- Malviya, A.; Stafford, G.H.; Villar, R.N. Impact of arthroscopy of the hip for femoroacetabular impingement on quality of life at a mean follow-up of 3.2 years. J. Bone Jt. Surg. Br. Vol. 2012, 94, 466–470. [Google Scholar] [CrossRef]
- Philippon, M.J.; Ejnisman, L.; Ellis, H.B.; Briggs, K.K. Outcomes 2 to 5 Years Following Hip Arthroscopy for Femoroacetabular Impingement in the Patient Aged 11 to 16 Years. Arthrosc. J. Arthrosc. Relat. Surg. 2012, 28, 1255–1261. [Google Scholar] [CrossRef]
- Maerz, T.; Nepple, J.J.; Bedi, A.; Zaltz, I.; Belzile, E.; Beaulé, P.E.; Sink, E.L.; Clohisy, J.C. Sex Differences in Clinical Outcomes Following Surgical Treatment of Femoroacetabular Impingement. J. Bone Jt. Surg. 2021, 103, 415–423. [Google Scholar] [CrossRef]
- Saltzman, B.M.; Kuhns, B.D.; Basques, B.; Leroux, T.; Alter, J.; Mather, R.C.; Salata, M.J.; Nho, S.J. The Influence of Body Mass Index on Outcomes After Hip Arthroscopic Surgery with Capsular Plication for the Treatment of Femoroacetabular Impingement. Am. J. Sports Med. 2017, 45, 2303–2311. [Google Scholar] [CrossRef]
- Levy, D.M.; Kuhns, B.; Chahal, J.; Philippon, M.J.; Kelly, B.T.; Nho, S.J. Hip Arthroscopy Outcomes with Respect to Patient Acceptable Symptomatic State and Minimal Clinically Important Difference. Arthrosc. J. Arthrosc. Relat. Surg. 2016, 32, 1877–1886. [Google Scholar] [CrossRef]
- Lynch, T.S.; Terry, M.A.; Bedi, A.; Kelly, B.T. Hip Arthroscopic Surgery. Am. J. Sports Med. 2013, 41, 1174–1189. [Google Scholar] [CrossRef]
- Philippon, M.J.; Briggs, K.; Yen, Y.-M.; Kuppersmith, D.A. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction. J. Bone Jt. Surg. 2009, 91, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Mohtadi, N.G.; Griffin, D.R.; Pedersen, M.E.; Chan, D.; Safran, M.R.; Parsons, N.; Sekiya, J.K.; Kelly, B.T.; Werle, J.R.; Leunig, M.; et al. The Development and Validation of a Self-Administered Quality-of-Life Outcome Measure for Young, Active Patients with Symptomatic Hip Disease: The International Hip Outcome Tool (iHOT-33). Arthrosc. J. Arthrosc. Relat. Surg. 2012, 28, 595–610.e1. [Google Scholar] [CrossRef] [PubMed]
- Baumann, F.; Weber, J.; Zeman, F.; Muller, M.; Lahner, M.; Nerlich, M.; Fickert, S. Validation of a German version of the International Hip Outcome Tool (G-iHOT33) according to the COSMIN checklist: How much improvement is clinically relevant? Arch. Orthop. Trauma. Surg. 2015, 136, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Dwyer, M.K.; Green, M.; McCarthy, J.C. Assessing outcomes following arthroscopic labral debridement--what can the IHOT-33 reveal? J. Hip Preserv. Surg. 2015, 2, 152–157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maxwell, S.; Pergaminelis, N.; Renouf, J.; Tirosh, O.; Tran, P. Identification of a Patient Acceptable Symptomatic State Score for the International Hip Outcome Tool in People Undergoing Hip Arthroscopy. Arthrosc. J. Arthrosc. Relat. Surg. 2018, 34, 3024–3029. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.D.; Taylor, J.; Almqvist, K.F.; Erggelet, C.; Knutsen, G.; Portabella, M.G.; Smith, T.; Richardson, J.B. Arthroscopic Assessment of Cartilage Repair: A Validation Study of 2 Scoring Systems. Arthrosc. J. Arthrosc. Relat. Surg. 2005, 21, 1462–1467. [Google Scholar] [CrossRef]
- Brittberg, M.; Winalski, C.S. Evaluation of Cartilage Injuries and Repair. J. Bone Jt. Surg. 2003, 85, 58–69. [Google Scholar] [CrossRef]
- Nwachukwu, B.U.; Chang, B.; Kahlenberg, C.A.; Fields, K.; Nawabi, D.H.; Kelly, B.T.; Ranawat, A.S. Arthroscopic Treatment of Femoroacetabular Impingement in Adolescents Provides Clinically Significant Outcome Improvement. Arthrosc. J. Arthrosc. Relat. Surg. 2017, 33, 1812–1818. [Google Scholar] [CrossRef]
- De Geus, S.W.; Sachs, T.E.; Tseng, J.F. Big Data vs. Clinical Trials in HPB Surgery. J. Gastrointest. Surg. 2020, 24, 1127–1137. [Google Scholar] [CrossRef]
- Nwachukwu, B.U.; Chang, B.; Adjei, J.; Schairer, W.W.; Ranawat, A.S.; Kelly, B.T.; Nawabi, D.H. Time Required to Achieve Minimal Clinically Important Difference and Substantial Clinical Benefit After Arthroscopic Treatment of Femoroacetabular Impingement. Am. J. Sports Med. 2018, 46, 2601–2606. [Google Scholar] [CrossRef]
- Chahal, J.; van Thiel, G.S.; Mather, I.R.C.; Lee, S.; Song, S.H.; Davis, A.; Salata, M.; Nho, S.J. The Patient Acceptable Symptomatic State for the Modified Harris Hip Score and Hip Outcome Score Among Patients Undergoing Surgical Treatment for Femoroacetabular Impingement. Am. J. Sports Med. 2015, 43, 1844–1849. [Google Scholar] [CrossRef] [PubMed]
- Joseph, R.; Pan, X.; Cenkus, K.; Brown-Taylor, L.; Ellis, T.; Di Stasi, S. Sex Differences in Self-Reported Hip Function Up to 2 Years After Arthroscopic Surgery for Femoroacetabular Impingement. Am. J. Sports Med. 2015, 44, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Bryan, A.J.; Krych, A.J.; Reardon, P.J.; Berardelli, R.; Pareek, A.; Levy, B.A. Are Short-term Outcomes of Hip Arthroscopy in Patients 55 Years and Older Inferior to Those in Younger Patients? Am. J. Sports Med. 2016, 44, 2526–2530. [Google Scholar] [CrossRef]
- Domb, B.G.; Linder, D.; Finley, Z.; Botser, I.B.; Chen, A.; Williamson, J.; Gupta, A. Outcomes of Hip Arthroscopy in Patients Aged 50 Years or Older Compared with a Matched-Pair Control of Patients Aged 30 Years or Younger. Arthrosc. J. Arthrosc. Relat. Surg. 2015, 31, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Declet, V.; Mu, B.; Chen, A.W.; Litrenta, J.; Perets, I.; Yuen, L.C.; Domb, B.G. Should the Capsule Be Repaired or Plicated After Hip Arthroscopy for Labral Tears Associated with Femoroacetabular Impingement or Instability? A Systematic Review. Arthrosc. J. Arthrosc. Relat. Surg. 2018, 34, 303–318. [Google Scholar] [CrossRef]
- Larson, C.M.; Giveans, M.R.; Stone, R.M. Arthroscopic Debridement Versus Refixation of the Acetabular Labrum Associated with Femoroacetabular Impingement. Am. J. Sports Med. 2012, 40, 1015–1021. [Google Scholar] [CrossRef]
- Nakashima, H.; Utsunomiya, H.; Kanezaki, S.; Suzuki, H.; Nakamura, E.; Larson, C.M.; Sakai, A.; Uchida, S. Is Arthroscopic Hip Labral Repair/Reconstruction Surgery Effective for Treating Femoroacetabular Impingement in the Presence of Osteoarthritis? Clin. J. Sport Med. 2021, 31, 367–373. [Google Scholar] [CrossRef]
- Larson, C.M.; Giveans, R.M.; Taylor, M. Does Arthroscopic FAI Correction Improve Function with Radiographic Arthritis? Clin. Orthop. Relat. Res. 2011, 469, 1667–1676. [Google Scholar] [CrossRef] [Green Version]
- Horisberger, M.; Brunner, A.; Herzog, R.F. Arthroscopic Treatment of Femoral Acetabular Impingement in Patients with Preoperative Generalized Degenerative Changes. Arthrosc. J. Arthrosc. Relat. Surg. 2010, 26, 623–629. [Google Scholar] [CrossRef]

| Parameter | Mean ± SD or n (%) | |
|---|---|---|
Age, years Sex, male/female Body Mass Index, kg/m2 Cartilage defect size, mm2 Cartilage defect grade, ICRS | I II III IV | 38.6 ± 11.4 235 (66.6)/118 (33.4) 25.9 ± 9.1 162.5 ± 169.9 25 (7.1) 83 (23.5) 187 (53.0) 58 (16.4) |
| Procedure | 6 Months | 12 Months | 24 Months | Total |
|---|---|---|---|---|
| n (% of Follow up group) | n (% of Study group) | |||
| Revision hip arthroscopy Total hip arthroplasty Others | 2 (0.7) 2 (0.7) 2 (0.7) (1× Lipoma, 1× Osteonecrosis) | 2 (0.8) 1 (0.4) 2 (0.8 1× Scar revision, 1× n.a.) | 2 (1.3) 5 (3.2) 1 (0.6) (1× Derotation osteotomy) | 6 (1.7) 8 (2.3) 5 (1.4) |
| Total | 6 (2.0) | 5 (2.0) | 8 (5.1) | 19 (5.4) |
| Parameter | iHOT-33 Total | ||
|---|---|---|---|
| 6 Months | 12 Months | 24 Months | |
| Age b (default) b (robust) SE(b) p Sex (coding: 1 male, 2 female) b (default) b (robust) SE(b) p Body mass index b (default) b (robust) SE(b) p Cartilage defect size b (default) b (robust) SE(b) p Cartilage defect grade, ICRS b (default) b (robust) SE(b) p Constant b (default) | Eliminated from model −0.665 * −0.139 * 0.289 0.022 −0.087 * −0.142 * 0.037 0.019 Eliminated from model Eliminated from model 9.577 *** | −0.033 * −0.151 * 0.014 0.022 −0.596 −0.151 0.331 0.073 −0.033 * −0.151 * 0.014 0.022 Eliminated from model Eliminated from model 9.638 *** | −0.037 * −0.173 * 0.018 0.039 Eliminated from model Eliminated from model Eliminated from model Eliminated from model 8.161 *** |
R2 Adjusted R2 F Statistic | 0.030 0.023 4.400 * (df = 2; 281) | 0.062 0.049 4.897 ** (df = 3; 223) | 0.030 0.023 4.358 * (df = 1; 141) |
| Parameter | Odds Ratio | 95% CI | p-Value | |
|---|---|---|---|---|
MCID 6 months PASS 6 months MCID 12 months PASS 12 months MCID 24 months PASS 24 months | Sex Body Mass Index Sex Body Mass Index Age Body Mass Index Age Body Mass Index Age Age | 1.24 0.98 0.54 0.93 1.00 0.97 0.97 0.98 0.98 0.95 | 0.71–2.16 0.91–1.05 0.32–0.91 0.87–0.99 0.98–1.03 0.92–1.03 0.94–0.99 0.94–1.01 0.95–1.02 0.92–0.98 | 0.453 0.499 0.019 * 0.018 * 0.751 0.316 0.010 ** 0.209 0.304 0.003 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Serong, S.; Fickert, S.; Niemeyer, P.; Banke, I.J.; Goronzy, J.; Sobau, C.; Zinser, W.; Landgraeber, S. Outcome-Affecting Parameters of Hip Arthroscopy for Femoroacetabular Impingement with Concomitant Cartilage Damage—Data Analysis from the German Cartilage Registry. J. Clin. Med. 2022, 11, 1532. https://doi.org/10.3390/jcm11061532
Serong S, Fickert S, Niemeyer P, Banke IJ, Goronzy J, Sobau C, Zinser W, Landgraeber S. Outcome-Affecting Parameters of Hip Arthroscopy for Femoroacetabular Impingement with Concomitant Cartilage Damage—Data Analysis from the German Cartilage Registry. Journal of Clinical Medicine. 2022; 11(6):1532. https://doi.org/10.3390/jcm11061532
Chicago/Turabian StyleSerong, Sebastian, Stefan Fickert, Philipp Niemeyer, Ingo J. Banke, Jens Goronzy, Christian Sobau, Wolfgang Zinser, and Stefan Landgraeber. 2022. "Outcome-Affecting Parameters of Hip Arthroscopy for Femoroacetabular Impingement with Concomitant Cartilage Damage—Data Analysis from the German Cartilage Registry" Journal of Clinical Medicine 11, no. 6: 1532. https://doi.org/10.3390/jcm11061532
APA StyleSerong, S., Fickert, S., Niemeyer, P., Banke, I. J., Goronzy, J., Sobau, C., Zinser, W., & Landgraeber, S. (2022). Outcome-Affecting Parameters of Hip Arthroscopy for Femoroacetabular Impingement with Concomitant Cartilage Damage—Data Analysis from the German Cartilage Registry. Journal of Clinical Medicine, 11(6), 1532. https://doi.org/10.3390/jcm11061532






