Comparison between Prehospital Mechanical Cardiopulmonary Resuscitation (CPR) Devices and Manual CPR for Out-of-Hospital Cardiac Arrest: A Systematic Review, Meta-Analysis, and Trial Sequential Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Exclusion Criteria
2.3. Search Methods
2.4. Selection of Studies
2.5. Data Extraction
2.6. Literature Quality Evaluation
2.7. Statistical Analysis
2.8. Trial Sequential Analysis
2.9. Grading of the Certainty of Evidence
3. Results
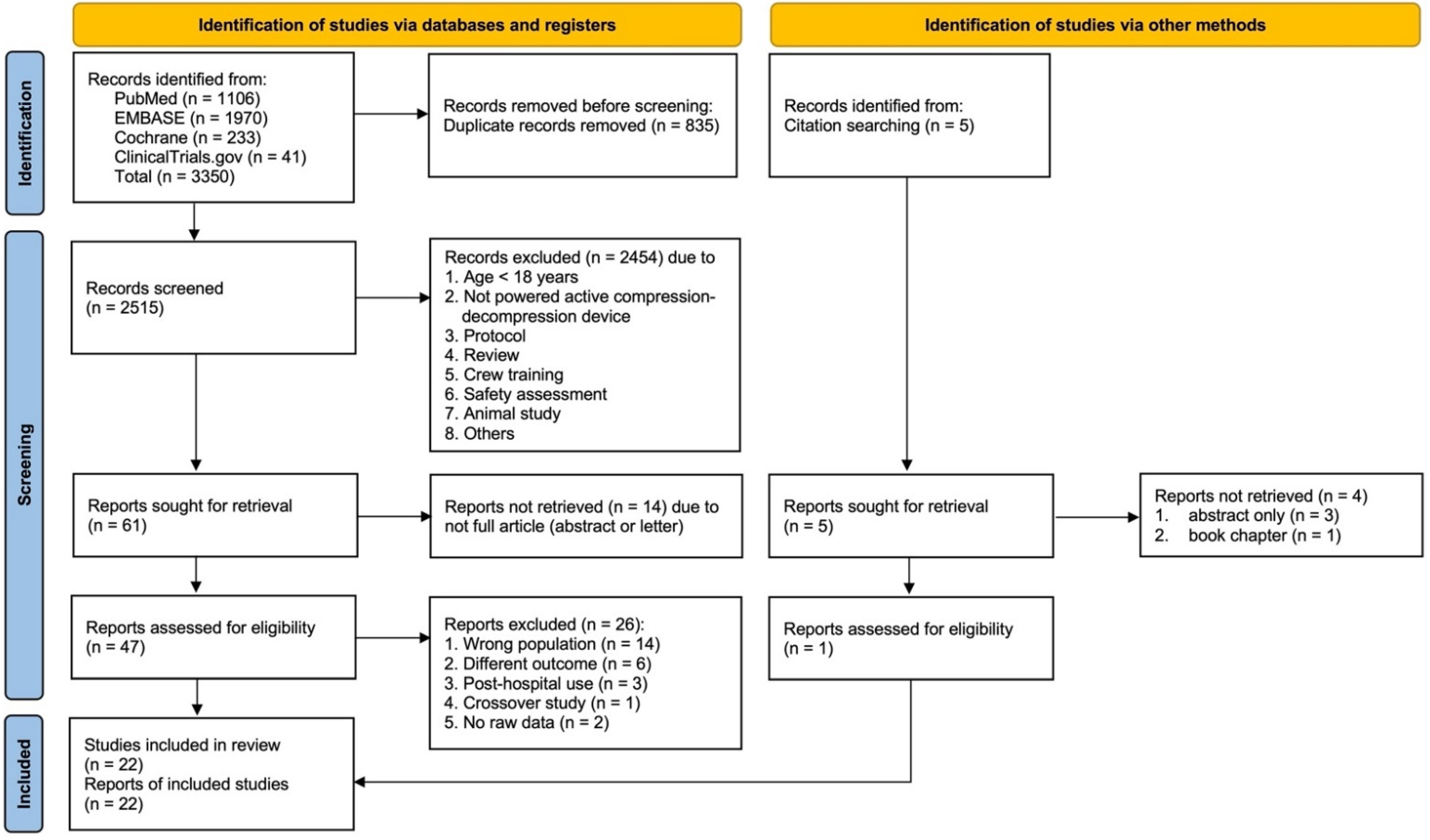
3.1. Results of the Literature Search
3.2. Risk of Bias Assessment
3.3. Outcomes
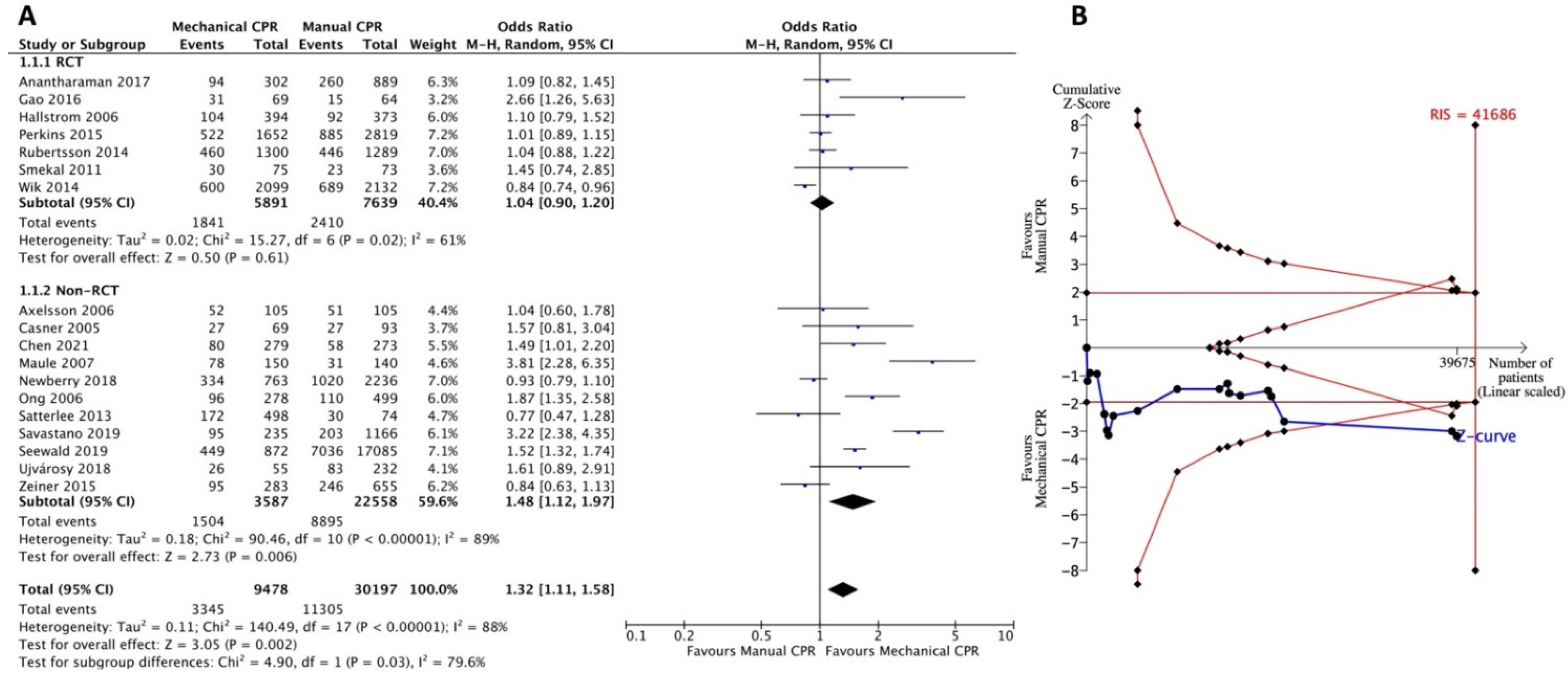
3.3.1. Primary Outcome: Return of Spontaneous Circulation
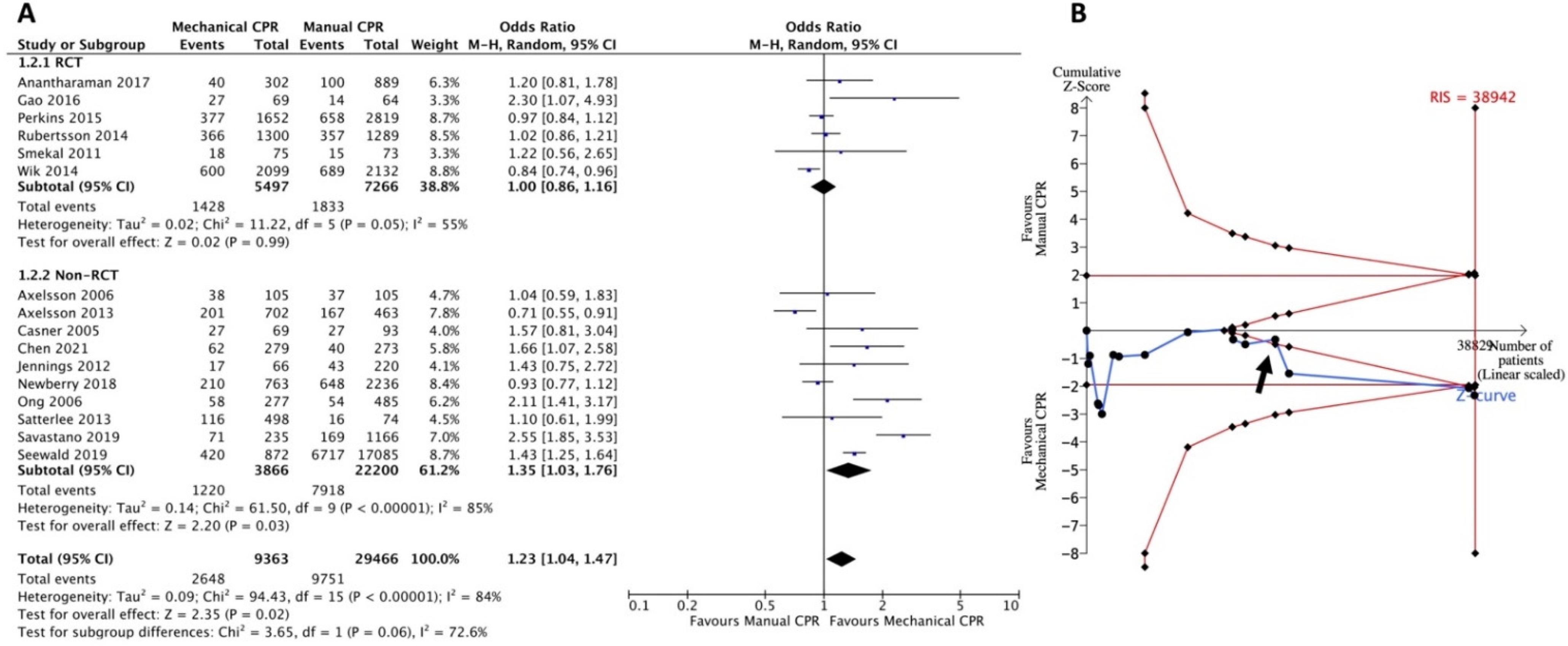
3.3.2. Primary Outcome: Survival to Hospital Admission
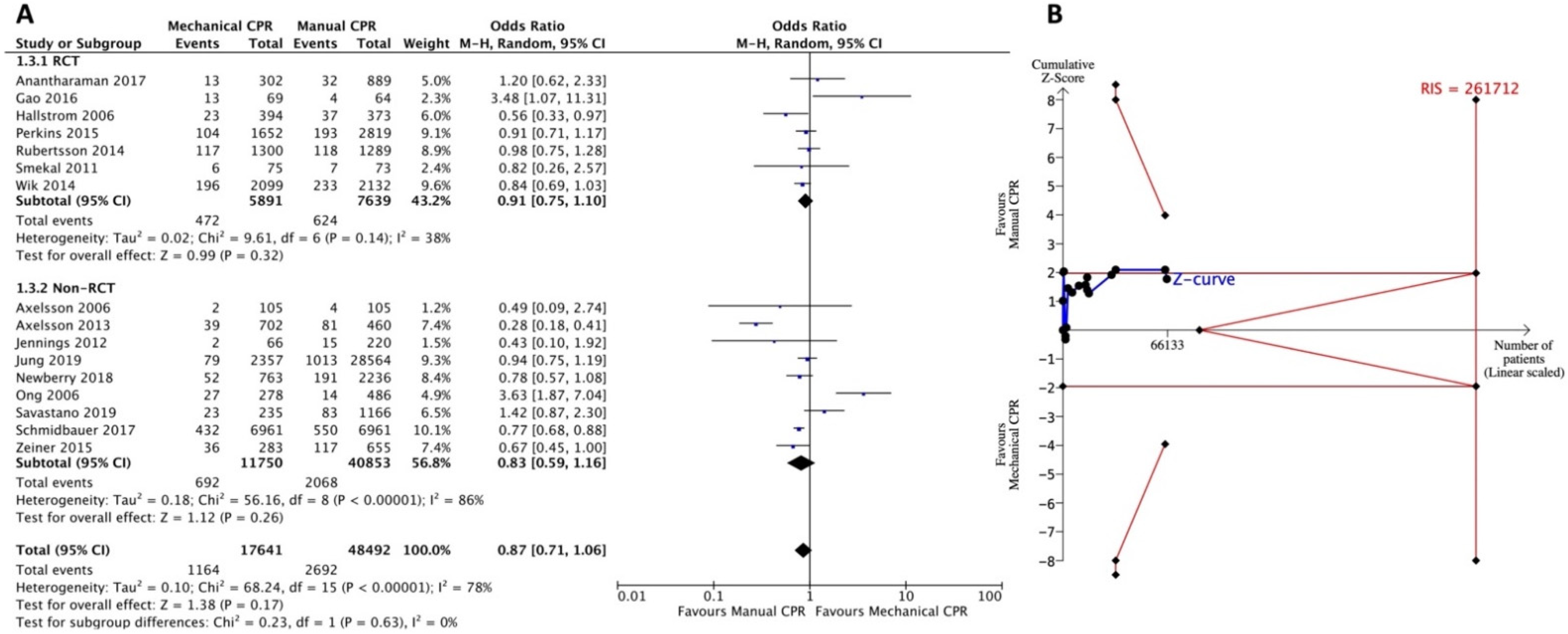
3.3.3. Secondary Outcome: Survival to Discharge
3.3.4. Secondary Outcome: Survival to Discharge with Favorable Neurologic Status
3.4. Subgroup and Sensitivity Analysis
3.5. GRADE Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kudenchuk, P.J.; Sandroni, C.; Drinhaus, H.R.; Böttiger, B.W.; Cariou, A.; Sunde, K.; Dworschak, M.; Taccone, F.S.; Deye, N.; Friberg, H.; et al. Breakthrough in Cardiac Arrest: Reports From the 4th Paris International Conference. Ann. Intensive Care 2015, 5, 22. [Google Scholar] [CrossRef] [PubMed]
- Kiguchi, T.; Okubo, M.; Nishiyama, C.; Maconochie, I.; Ong, M.E.H.; Kern, K.B.; Wyckoff, M.H.; McNally, B.; Christensen, E.F.; Tjelmeland, I.; et al. Out-of-Hospital Cardiac Arrest Across the World: First Report From the International Liaison Committee on Resuscitation (ILCOR). Resuscitation 2020, 152, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Berdowski, J.; Berg, R.A.; Tijssen, J.G.; Koster, R.W. Global Incidences of Out-of-Hospital Cardiac Arrest and Survival Rates: Systematic Review of 67 Prospective Studies. Resuscitation 2010, 81, 1479–1487. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.; Gan, Y.; Jiang, N.; Wang, R.; Chen, Y.; Luo, Z.; Zong, Q.; Chen, S.; Lv, C. The Global Survival Rate Among Adult Out-of-Hospital Cardiac Arrest Patients Who Received Cardiopulmonary Resuscitation: A Systematic Review and Meta-Analysis. Crit. Care 2020, 24, 61. [Google Scholar] [CrossRef]
- Merchant, R.M.; Topjian, A.A.; Panchal, A.R.; Cheng, A.; Aziz, K.; Berg, K.M.; Lavonas, E.J.; Magid, D.J.; Adult Basic and Advanced Life Support, Pediatric Basic and Advanced Life Support, Neonatal Life Support, Resuscitation Education Science, and Systems of Care Writing Groups. Circulation 2020-Part 1: Executive summary: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2020, 142, S337–S357. [Google Scholar] [CrossRef]
- Kahn, P.A.; Dhruva, S.S.; Rhee, T.G.; Ross, J.S. Use of Mechanical Cardiopulmonary Resuscitation Devices for Out-of-Hospital Cardiac Arrest, 2010–2016. JAMA Netw. Open. 2019, 2, e1913298. [Google Scholar] [CrossRef]
- Edelson, D.P.; Sasson, C.; Chan, P.S.; Atkins, D.L.; Aziz, K.; Becker, L.B.; Berg, R.A.; Bradley, S.M.; Brooks, S.C.; Cheng, A.; et al. Interim Guidance for Basic and Advanced Life Support in Adults, Children, and Neonates With Suspected or Confirmed COVID-19: From the Emergency Cardiovascular Care Committee and Get With the Guidelines-Resuscitation Adult and Pediatric Task Forces of the American Heart Association. Circulation 2020, 141, e933–e943. [Google Scholar] [CrossRef]
- Zhu, N.; Chen, Q.; Jiang, Z.; Liao, F.; Kou, B.; Tang, H.; Zhou, M. A Meta-Analysis of the Resuscitative Effects of Mechanical and Manual Chest Compression in Out-of-Hospital Cardiac Arrest Patients. Crit. Care 2019, 23, 100. [Google Scholar] [CrossRef]
- Wang, P.; Brooks, S. Cochrane Corner: Are Mechanical Compressions Better Than Manual Compressions in Cardiac Arrest? Heart 2020, 106, 559–561. [Google Scholar] [CrossRef]
- Bonnes, J.L.; Brouwer, M.A.; Navarese, E.P.; Verhaert, D.V.; Verheugt, F.W.; Smeets, J.L.; de Boer, M.J. Manual Cardiopulmonary Resuscitation Versus CPR Including a Mechanical Chest Compression Device in Out-of-Hospital Cardiac Arrest: A Comprehensive Meta-Analysis From Randomized and Observational Studies. Ann. Emerg. Med. 2016, 67, 349–360.e3. [Google Scholar] [CrossRef]
- Liu, M.; Shuai, Z.; Ai, J.; Tang, K.; Liu, H.; Zheng, J.; Gou, J.; Lv, Z. Mechanical Chest Compression With LUCAS Device Does Not Improve Clinical Outcome in Out-of-Hospital Cardiac Arrest Patients: A Systematic Review and Meta-Analysis. Medicine 2019, 98, e17550. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Wang, D.; Yu, Y.; Zhao, X.; Jing, X. Mechanical Versus Manual Chest Compressions for Cardiac Arrest: A Systematic Review and Meta-Analysis. Scand. J. Trauma Resusc. Emerg. Med. 2016, 24, 10. [Google Scholar] [CrossRef] [PubMed]
- Hayashida, K.; Tagami, T.; Fukuda, T.; Suzuki, M.; Yonemoto, N.; Kondo, Y.; Ogasawara, T.; Sakurai, A.; Tahara, Y.; Nagao, K.; et al. Mechanical Cardiopulmonary Resuscitation and Hospital Survival Among Adult Patients With Nontraumatic Out-of-Hospital Cardiac Arrest Attending the Emergency Department: A Prospective, Multicenter, Observational Study in Japan (SOS-KANTO [Survey of Survivors after Out-Of-Hospital Cardiac Arrest in Kanto Area] 2012 Study). J. Am. Heart Assoc. 2017, 6, e007420. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.T.; Kim, J.G.; Jang, Y.S.; Kang, G.H.; Kim, W.; Choi, H.Y.; Jun, G.S. Comparison of in-Hospital Use of Mechanical Chest Compression Devices for Out-of-Hospital Cardiac Arrest Patients: AUTOPULSE vs LUCAS. Medicine 2019, 98, e17881. [Google Scholar] [CrossRef]
- Lin, C.K.; Huang, M.C.; Feng, Y.T.; Jeng, W.H.; Chung, T.C.; Lau, Y.W.; Cheng, K.I. Effectiveness of Mechanical Chest Compression for Out-of-Hospital Cardiac Arrest Patients in an Emergency Department. J. Chin. Med. Assoc. 2015, 78, 360–363. [Google Scholar] [CrossRef]
- Ogawa, Y.; Shiozaki, T.; Hirose, T.; Ohnishi, M.; Nakamori, Y.; Ogura, H.; Shimazu, T. Load-Distributing-Band Cardiopulmonary Resuscitation for Out-of-Hospital Cardiac Arrest Increases Regional Cerebral Oxygenation: A Single-Center Prospective Pilot Study. Scand. J. Trauma Resusc. Emerg. Med. 2015, 23, 99. [Google Scholar] [CrossRef][Green Version]
- Seewald, S.; Obermaier, M.; Lefering, R.; Bohn, A.; Georgieff, M.; Muth, C.M.; Gräsner, J.T.; Masterson, S.; Scholz, J.; Wnent, J. Application of Mechanical Cardiopulmonary Resuscitation Devices and Their Value in Out-of-Hospital Cardiac Arrest: A Retrospective Analysis of the German Resuscitation Registry. PLoS ONE 2019, 14, e0208113. [Google Scholar] [CrossRef]
- Chen, Y.R.; Liao, C.J.; Huang, H.C.; Tsai, C.H.; Su, Y.S.; Liu, C.H.; Hsu, C.F.; Tsai, M.J. The Effect of Implementing Mechanical Cardiopulmonary Resuscitation Devices on Out-of-Hospital Cardiac Arrest Patients in an Urban City of Taiwan. Int. J. Environ. Res. Public Health 2021, 18, 3636. [Google Scholar] [CrossRef]
- Anantharaman, V.; Ng, B.L.; Ang, S.H.; Lee, C.Y.; Leong, S.H.; Ong, M.E.; Chua, S.J.; Rabind, A.C.; Anjali, N.B.; Hao, Y. Prompt Use of Mechanical Cardiopulmonary Resuscitation in Out-of-Hospital Cardiac Arrest: The MECCA Study Report. Singap. Med. J. 2017, 58, 424–431. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. Robins-I: A Tool for Assessing Risk of Bias in Non-Randomised Studies of Interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Brok, J.; Thorlund, K.; Wetterslev, J.; Gluud, C. Apparently Conclusive Meta-Analyses May Be Inconclusive-Trial Sequential Analysis Adjustment of Random Error Risk Due to Repetitive Testing of Accumulating Data in Apparently Conclusive Neonatal Meta-Analyses. Int. J. Epidemiol. 2009, 38, 287–298. [Google Scholar] [CrossRef]
- Kang, H. Trial Sequential Analysis: Novel Approach for Meta-Analysis. Anesth. Pain Med. 2021, 16, 138–150. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J.; GRADE Working Group. GRADE: An Emerging Consensus on Rating Quality of Evidence and Strength of Recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Axelsson, C.; Herrera, M.J.; Fredriksson, M.; Lindqvist, J.; Herlitz, J. Implementation of Mechanical Chest Compression in Out-of-Hospital Cardiac Arrest in an Emergency Medical Service System. Am. J. Emerg. Med. 2013, 31, 1196–1200. [Google Scholar] [CrossRef]
- Axelsson, C.; Nestin, J.; Svensson, L.; Axelsson, A.B.; Herlitz, J. Clinical Consequences of the Introduction of Mechanical Chest Compression in the EMS System for Treatment of Out-of-Hospital Cardiac Arrest-A Pilot Study. Resuscitation 2006, 71, 47–55. [Google Scholar] [CrossRef]
- Maule, Y. Mechanical External Chest Compression: A New Adjuvant Technology in Cardiopulmonary Resuscitation. Urgences Accueil. 2007, 7, 4–7. [Google Scholar]
- Newberry, R.; Redman, T.; Ross, E.; Ely, R.; Saidler, C.; Arana, A.; Wampler, D.; Miramontes, D. No Benefit in Neurologic Outcomes of Survivors of Out-of-Hospital Cardiac Arrest With Mechanical Compression Device. Prehosp. Emerg. Care 2018, 22, 338–344. [Google Scholar] [CrossRef]
- Satterlee, P.A.; Boland, L.L.; Johnson, P.J.; Hagstrom, S.G.; Page, D.I.; Lick, C.J. Implementation of a Mechanical Chest Compression Device as Standard Equipment in a Large Metropolitan Ambulance Service. J. Emerg. Med. 2013, 45, 562–569. [Google Scholar] [CrossRef]
- Schmidbauer, S.; Herlitz, J.; Karlsson, T.; Axelsson, C.; Friberg, H. Use of Automated Chest Compression Devices After Out-of-Hospital Cardiac Arrest in Sweden. Resuscitation 2017, 120, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Ujvárosy, D.; Sebestyén, V.; Pataki, T.; Ötvös, T.; Lőrincz, I.; Paragh, G.; Szabó, Z. Cardiovascular Risk Factors Differently Affect the Survival of Patients Undergoing Manual or Mechanical Resuscitation. BMC Cardiovasc. Disord. 2018, 18, 227. [Google Scholar] [CrossRef] [PubMed]
- Smekal, D.; Johansson, J.; Huzevka, T.; Rubertsson, S. A Pilot Study of Mechanical Chest Compressions With the LUCAS™ Device in Cardiopulmonary Resuscitation. Resuscitation 2011, 82, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Rubertsson, S.; Lindgren, E.; Smekal, D.; Östlund, O.; Silfverstolpe, J.; Lichtveld, R.A.; Boomars, R.; Ahlstedt, B.; Skoog, G.; Kastberg, R.; et al. Mechanical Chest Compressions and Simultaneous Defibrillation vs Conventional Cardiopulmonary Resuscitation in Out-of-Hospital Cardiac Arrest: The LINC Randomized Trial. JAMA 2014, 311, 53–61. [Google Scholar] [CrossRef]
- Perkins, G.D.; Lall, R.; Quinn, T.; Deakin, C.D.; Cooke, M.W.; Horton, J.; Lamb, S.E.; Slowther, A.M.; Woollard, M.; Carson, A.; et al. Mechanical Versus Manual Chest Compression for Out-of-Hospital Cardiac Arrest (PARAMEDIC): A Pragmatic, Cluster Randomised Controlled Trial. Lancet 2015, 385, 947–955. [Google Scholar] [CrossRef]
- Wik, L.; Olsen, J.A.; Persse, D.; Sterz, F.; Lozano, M.; Brouwer, M.A.; Westfall, M.; Souders, C.M.; Malzer, R.; van Grunsven, P.M.; et al. Manual vs. Integrated Automatic Load-Distributing Band CPR With Equal Survival After out of Hospital Cardiac Arrest. The Randomized CIRC Trial. Resuscitation 2014, 85, 741–748. [Google Scholar] [CrossRef]
- Hallstrom, A.; Rea, T.D.; Sayre, M.R.; Christenson, J.; Anton, A.R.; Mosesso, V.N.; Van Ottingham, L.; Olsufka, M.; Pennington, S.; White, L.J.; et al. Manual Chest Compression vs Use of an Automated Chest Compression Device During Resuscitation Following Out-of-Hospital Cardiac Arrest: A Randomized Trial. JAMA 2006, 295, 2620–2628. [Google Scholar] [CrossRef]
- Gao, C.; Chen, Y.; Peng, H.; Chen, Y.; Zhuang, Y.; Zhou, S. Clinical Evaluation of the AutoPulse Automated Chest Compression Device for Out-of-Hospital Cardiac Arrest in the Northern District of Shanghai, China. Arch. Med. Sci. 2016, 12, 563–570. [Google Scholar] [CrossRef]
- Savastano, S.; Baldi, E.; Palo, A.; Raimondi, M.; Belliato, M.; Compagnoni, S.; Buratti, S.; Cacciatore, E.; Canevari, F.; Iotti, G.; et al. Load Distributing Band Device for Mechanical Chest Compressions: An Utstein-Categories Based Analysis of Survival to Hospital Discharge. Int. J. Cardiol. 2019, 287, 81–85. [Google Scholar] [CrossRef]
- Ong, M.E.; Ornato, J.P.; Edwards, D.P.; Dhindsa, H.S.; Best, A.M.; Ines, C.S.; Hickey, S.; Clark, B.; Williams, D.C.; Powell, R.G.; et al. Use of an Automated, Load-Distributing Band Chest Compression Device for Out-of-Hospital Cardiac Arrest Resuscitation. JAMA 2006, 295, 2629–2637. [Google Scholar] [CrossRef]
- Jennings, P.A.; Harriss, L.; Bernard, S.; Bray, J.; Walker, T.; Spelman, T.; Smith, K.; Cameron, P. An Automated CPR Device Compared With Standard Chest Compressions for Out-of-Hospital Resuscitation. BMC Emerg. Med. 2012, 12, 8. [Google Scholar] [CrossRef] [PubMed]
- Casner, M.; Andersen, D.; Isaacs, S.M. The Impact of a New CPR Assist Device on Rate of Return of Spontaneous Circulation in Out-of-Hospital Cardiac Arrest. Prehosp. Emerg. Care 2005, 9, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Zeiner, S.; Sulzgruber, P.; Datler, P.; Keferböck, M.; Poppe, M.; Lobmeyr, E.; van Tulder, R.; Zajicek, A.; Buchinger, A.; Polz, K.; et al. Mechanical Chest Compression Does Not Seem to Improve Outcome After Out-Of Hospital Cardiac Arrest. A Single Center Observational Trial. Resuscitation 2015, 96, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Jung, E.; Park, J.H.; Lee, S.Y.; Ro, Y.S.; Hong, K.J.; Song, K.J.; Ryu, H.H.; Shin, S.D. Mechanical Chest Compression Device for Out-of-Hospital Cardiac Arrest: A Nationwide Observational Study. J. Emerg. Med. 2020, 58, 424–431. [Google Scholar] [CrossRef]
- Sheraton, M.; Columbus, J.; Surani, S.; Chopra, R.; Kashyap, R. Effectiveness of Mechanical Chest Compression Devices Over Manual Cardiopulmonary Resuscitation: A Systematic Review With Meta-Analysis and Trial Sequential Analysis. West. J. Emerg. Med. 2021, 22, 810–819. [Google Scholar] [CrossRef]
- Khan, S.U.; Lone, A.N.; Talluri, S.; Khan, M.Z.; Khan, M.U.; Kaluski, E. Efficacy and Safety of Mechanical Versus Manual Compression in Cardiac Arrest—A Bayesian Network Meta-Analysis. Resuscitation 2018, 130, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Couper, K.; Yeung, J.; Nicholson, T.; Quinn, T.; Lall, R.; Perkins, G.D. Mechanical Chest Compression Devices at in-Hospital Cardiac Arrest: A Systematic Review and Meta-Analysis. Resuscitation 2016, 103, 24–31. [Google Scholar] [CrossRef]
- Ong, M.E.; Mackey, K.E.; Zhang, Z.C.; Tanaka, H.; Ma, M.H.; Swor, R.; Shin, S.D. Mechanical CPR Devices Compared to Manual CPR During Out-of-Hospital Cardiac Arrest and Ambulance Transport: A Systematic Review. Scand. J. Trauma Resusc. Emerg. Med. 2012, 20, 39. [Google Scholar] [CrossRef]
- Wang, P.L.; Brooks, S.C. Mechanical Versus Manual Chest Compressions for Cardiac Arrest. Cochrane Database Syst. Rev. 2018. [Google Scholar] [CrossRef]
- Lyon, R.M.; Crawford, A.; Crookston, C.; Short, S.; Clegg, G.R. The Combined Use of Mechanical CPR and a Carry Sheet to Maintain Quality Resuscitation in Out-of-Hospital Cardiac Arrest Patients During Extrication and Transport. Resuscitation 2015, 93, 102–106. [Google Scholar] [CrossRef]
- Becker, L.R.; Zaloshnja, E.; Levick, N.; Li, G.; Miller, T.R. Relative Risk of Injury and Death in Ambulances and Other Emergency Vehicles. Accid. Anal. Prev. 2003, 35, 941–948. [Google Scholar] [CrossRef]
- Kahn, C.A.; Pirrallo, R.G.; Kuhn, E.M. Characteristics of Fatal Ambulance Crashes in the United States: An 11-Year Retrospective Analysis. Prehosp. Emerg. Care 2001, 5, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Kurz, M.C.; Dante, S.A.; Puckett, B.J. Estimating the Impact of Off-Balancing Forces Upon Cardiopulmonary Resuscitation During Ambulance Transport. Resuscitation 2012, 83, 1085–1089. [Google Scholar] [CrossRef] [PubMed]
- Hassager, C.; Nagao, K.; Hildick-Smith, D. Out-of-Hospital Cardiac Arrest: In-Hospital Intervention Strategies. Lancet 2018, 391, 989–998. [Google Scholar] [CrossRef]
- Schünemann, H.J.; Cuello, C.; Akl, E.A.; Mustafa, R.A.; Meerpohl, J.J.; Thayer, K.; Morgan, R.L.; Gartlehner, G.; Kunz, R.; Katikireddi, S.V.; et al. [GRADE guidelines, 105–114] [GRADE guidelines, 105–114]. GRADE Guidelines: 18. How Robins-I and Other Tools to Assess Risk of Bias in Nonrandomized Studies Should Be Used to Rate the Certainty of a Body of Evidence. J. Clin. Epidemiol. 2019, 111, 105–114. [Google Scholar] [CrossRef]
- Chang, H.C.; Tsai, M.S.; Kuo, L.K.; Hsu, H.H.; Huang, W.C.; Lai, C.H.; Shih, M.C.; Huang, C.H. Factors Affecting Outcomes in Patients With Cardiac Arrest Who Receive Target Temperature Management: The Multi-Center TIMECARD Registry. J. Formos. Med. Assoc. 2022, 121, 294–303. [Google Scholar] [CrossRef]
- Soar, J.; Böttiger, B.W.; Carli, P.; Couper, K.; Deakin, C.D.; Djärv, T.; Lott, C.; Olasveengen, T.; Paal, P.; Pellis, T.; et al. European Resuscitation Council Guidelines 2021: Adult Advanced Life Support. Resuscitation 2021, 161, 115–151. [Google Scholar] [CrossRef]

| Author | Year of Publication | Country | N | Study Period | Definite Study Design | Nationwide Study | Type of Mechanical Device | CPR Guideline | Witnessed Arrest | Shockable Rhythm |
|---|---|---|---|---|---|---|---|---|---|---|
| Randomized studies | ||||||||||
| Anantharaman | 2017 | Singapore | 1191 | 2011–2012 | Cluster RCT | No | LUCAS | 2010 ILCOR | 52% man, 62% mech | 17% man, 23% mech |
| Gao | 2016 | China | 133 | 2011–2012 | Cluster RCT | No | Autopulse | 2010 AHA | 59% man, 67% mech | 13% man, 13% mech |
| Hallstrom | 2006 | USA and Canada | 767 | 2004–2005 | Cluster RCT | No | Autopulse | 2000 AHA | 49% man, 44% mech | 32% man, 31% mech |
| Perkins | 2015 | UK | 4471 | 2010–2013 | Cluster RCT | No | LUCAS | 2005/2010 ERC | 62% man, 61% mech | 22% man, 23% mech |
| Rubertsson | 2014 | Sweden, UK, The Netherlands | 2589 | 2008–2013 | Individually RCT | No | LUCAS | 2005 ERC | 72% man, 73% mech | 30% man, 29% mech |
| Smekal | 2011 | Sweden | 148 | 2005–2007 | Individually RCT | No | LUCAS | 2000 ERC | 74% man, 68% mech | 27% man, 27% mech |
| Wik | 2014 | Norway | 4231 | 2009–2011 | Individually RCT | No | Autopulse | 2005 ERC/AHA | 48% man, 47% mech | 24% man, 21% mech |
| Non-randomized studies | ||||||||||
| Axelsson | 2006 | Sweden | 210 | 2003–2005 | Prospective cohort | No | LUCAS | 2000 AHA | 100% man, 100% mech | 32% man, 30% mech |
| Axelsson | 2013 | Sweden | 1165 | 2007–2011 | Retrospective cohort | No | LUCAS | Not reported | 72%man, 73% mech | 25% man, 26% mech |
| Casner | 2005 | USA | 162 | 2003 | Retrospective cohort | No | Autopulse | Not reported | Not reported | 28% man, 33% mech |
| Chen | 2021 | Taiwan | 552 | 2018–2020 | Retrospective cohort | No | LUCAS | 2015 AHA | 53% man, 48% mech | 21% man, 26% mech |
| Jennings | 2012 | Australia | 286 | 2006–2010 | Retrospective cohort | No | Autopulse | Not reported | 72% man, 71% mech | 36% man, 30% mech |
| Jung | 2019 | Korea | 30,921 | 2016–2017 | Prospective cohort | Yes | LUCAS/Autopulse | Not reported | 47% man, 47% mech | 14% man, 14% mech |
| Maule | 2007 | België | 290 | 2004–2006 | Retrospective cohort | No | LUCAS | Not reported | Not reported | Not reported |
| Newberry | 2018 | USA | 2999 | 2013–2015 | Retrospective cohort | No | LUCAS | Not reported | 43% man, 37% mech | 14% man, 12% mech |
| Ong | 2006 | USA | 783 | 2001–2005 | Prospective cohort | No | Autopulse | Not reported | 47% man, 52% mech | 20% man, 23% mech |
| Satterlee | 2013 | USA | 572 | 2008–2010 | Retrospective cohort | No | LUCAS | Not reported | 61% man, 53% mech | 18% man, 21% mech |
| Savastano | 2019 | Italy | 1401 | 2015–2017 | Prospective cohort | No | Autopulse | Not reported | 70% man, 86% mech | 14% man, 43% mech |
| Schmidbauer | 2017 | Sweden | 13,922 | 2011–2015 | Prospective cohort | Yes | LUCAS | 2010 ERC | 66% man, 67% mech | 22% man, 23% mech |
| Seewald | 2019 | Germany | 17,957 | 2007–2014 | Retrospective cohort | Yes | LUCAS/Autopulse | Not reported | 56% man, 62% mech | 25% man, 33% mech |
| Ujvárosy | 2018 | Hungary | 287 | 2010–2013 | Retrospective cohort | No | LUCAS | Not reported | Not reported | Not reported |
| Zeiner | 2015 | Austria | 938 | 2013–2014 | Prospective cohort | No | LUCAS/Autopulse | Not reported | 54% man, 56% mech | 22% man, 34% mech |
| ROSC | Survival to Hospital Admission | Survival to Discharge | Survival to Discharge with Favorable Neurologic Status | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Subgroups | No. of Studies | Pooled OR (95% CI) | p | I2 (%) | No. of Studies | Pooled OR (95% CI) | p | I2 (%) | No. of Studies | Pooled OR (95% CI) | p | I2 (%) | No. of Studies | Pooled OR (95% CI) | p | I2 (%) |
| Type of mechanical CPR device | ||||||||||||||||
| LUCAS | 10 | 1.19 (0.99–1.43) | 0.06 | 74% | 9 | 1.00 (0.88–1.13) | 0.94 | 43% | 8 | 0.74 (0.57–0.97) | 0.03 | 78% | 4 | 0.86 (0.67–1.12) | 0.27 | 48% |
| Autopulse | 6 | 1.65 (0.97–2.79) | 0.06 | 94% | 6 | 1.67 (0.97–2.84) | 0.06 | 91% | 6 | 1.24 (0.71–2.18) | 0.45 | 83% | 4 | 1.13 (0.47–2.73) | 0.79 | 83% |
| LUCAS + Autopulse | 2 | 1.15 (0.64–2.04) | 0.65 | 92% | 1 | 1.43 (1.25–1.64) | <0.001 | NA | 2 | 0.83 (0.60–1.15) | 0.26 | 52% | 2 | 0.61 (0.42–0.88) | 0.009 | 27% |
| Geographic location | ||||||||||||||||
| Europe | 10 | 1.37 (1.06–1.78) | 0.02 | 92% | 8 | 1.12 (0.88–1.42) | 0.36 | 90% | 9 | 0.77 (0.61–0.97) | 0.02 | 79% | 4 | 0.79 (0.61–1.02) | 0.07 | 62% |
| North America | 5 | 1.16 (0.85–1.60) | 0.34 | 76% | 4 | 1.33 (0.84–2.11) | 0.22 | 79% | 3 | 1.13 (0.45–2.84) | 0.79 | 90% | 3 | 0.93 (0.32–2.73) | 0.89 | 88% |
| Asia | 3 | 1.46 (0.97–2.20) | 0.07 | 63% | 3 | 1.51 (1.10–2.09) | 0.01 | 23% | 3 | 1.26 (0.72–2.18) | 0.42 | 59% | 3 | 0.95 (0.55–1.64) | 0.86 | 35% |
| Oceania | 0 | NA | NA | NA | 1 | 1.43 (0.75–2.72) | 0.28 | NA | 1 | 0.43 (0.10–1.92) | 0.27 | NA | 0 | NA | NA | NA |
| Mechanical CPR Compared to Manual CPR for Out-of-Hospital Cardiac Arrest | |||||||
|---|---|---|---|---|---|---|---|
| Certainty Assessment | Summary of Findings | ||||||
| No. of Participants (Studies) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Overall Certainty of Evidence | Anticipated Absolute Effects Risk Difference |
| ROSC | |||||||
| 39,675 | very serious a | serious b | not serious | not serious | none | ⨁◯◯◯ | 67 more per 1000 |
| (7 RCTs, 11 non-RCTs) | Very Low | (from 25 more to 112 more) | |||||
| Survival to hospital admission | |||||||
| 38,829 | very serious a | serious b | not serious | not serious | none | ⨁◯◯◯ | 47 more per 1000 |
| (6 RCTs, 10 non-RCTs) | Very Low | (from 9 fewer to 90 more) | |||||
| Survival to discharge | |||||||
| 66,133 | very serious a | serious b | not serious | serious c | none | ⨁◯◯◯ | 7 fewer per 1000 |
| (7 RCTs, 9 non-RCTs) | Very Low | (from 15 fewer to 3 more) | |||||
| Survival to discharge with favorable neurologic status | |||||||
| 48,384 | very serious a | serious b | not serious | serious c | none | ⨁◯◯◯ | 5 fewer per 1000 |
| (5 RCTs, 5 non-RCTs) | Very Low | (from 10 fewer to 2 more) | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiang, C.-Y.; Lim, K.-C.; Lai, P.C.; Tsai, T.-Y.; Huang, Y.T.; Tsai, M.-J. Comparison between Prehospital Mechanical Cardiopulmonary Resuscitation (CPR) Devices and Manual CPR for Out-of-Hospital Cardiac Arrest: A Systematic Review, Meta-Analysis, and Trial Sequential Analysis. J. Clin. Med. 2022, 11, 1448. https://doi.org/10.3390/jcm11051448
Chiang C-Y, Lim K-C, Lai PC, Tsai T-Y, Huang YT, Tsai M-J. Comparison between Prehospital Mechanical Cardiopulmonary Resuscitation (CPR) Devices and Manual CPR for Out-of-Hospital Cardiac Arrest: A Systematic Review, Meta-Analysis, and Trial Sequential Analysis. Journal of Clinical Medicine. 2022; 11(5):1448. https://doi.org/10.3390/jcm11051448
Chicago/Turabian StyleChiang, Cheng-Ying, Ket-Cheong Lim, Pei Chun Lai, Tou-Yuan Tsai, Yen Ta Huang, and Ming-Jen Tsai. 2022. "Comparison between Prehospital Mechanical Cardiopulmonary Resuscitation (CPR) Devices and Manual CPR for Out-of-Hospital Cardiac Arrest: A Systematic Review, Meta-Analysis, and Trial Sequential Analysis" Journal of Clinical Medicine 11, no. 5: 1448. https://doi.org/10.3390/jcm11051448
APA StyleChiang, C.-Y., Lim, K.-C., Lai, P. C., Tsai, T.-Y., Huang, Y. T., & Tsai, M.-J. (2022). Comparison between Prehospital Mechanical Cardiopulmonary Resuscitation (CPR) Devices and Manual CPR for Out-of-Hospital Cardiac Arrest: A Systematic Review, Meta-Analysis, and Trial Sequential Analysis. Journal of Clinical Medicine, 11(5), 1448. https://doi.org/10.3390/jcm11051448






