Time Trends (2012–2020), Sex Differences and Predictors for Influenza Vaccination Uptake among Individuals with Chronic Obstructive Pulmonary Disease in Spain
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Study Population
2.2. Study Variables
2.3. Statistical Analysis
2.4. Ethical Aspects
3. Results
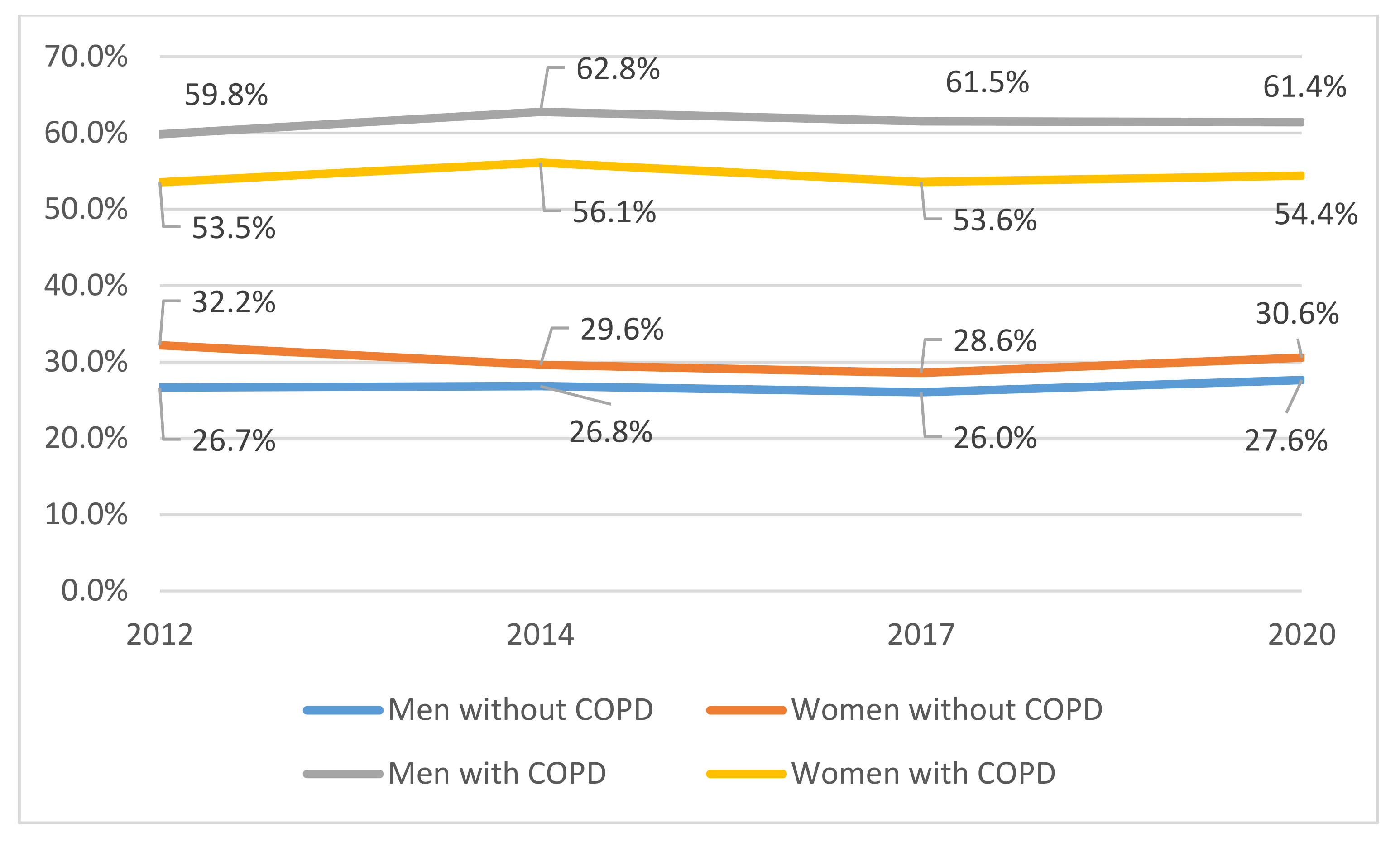
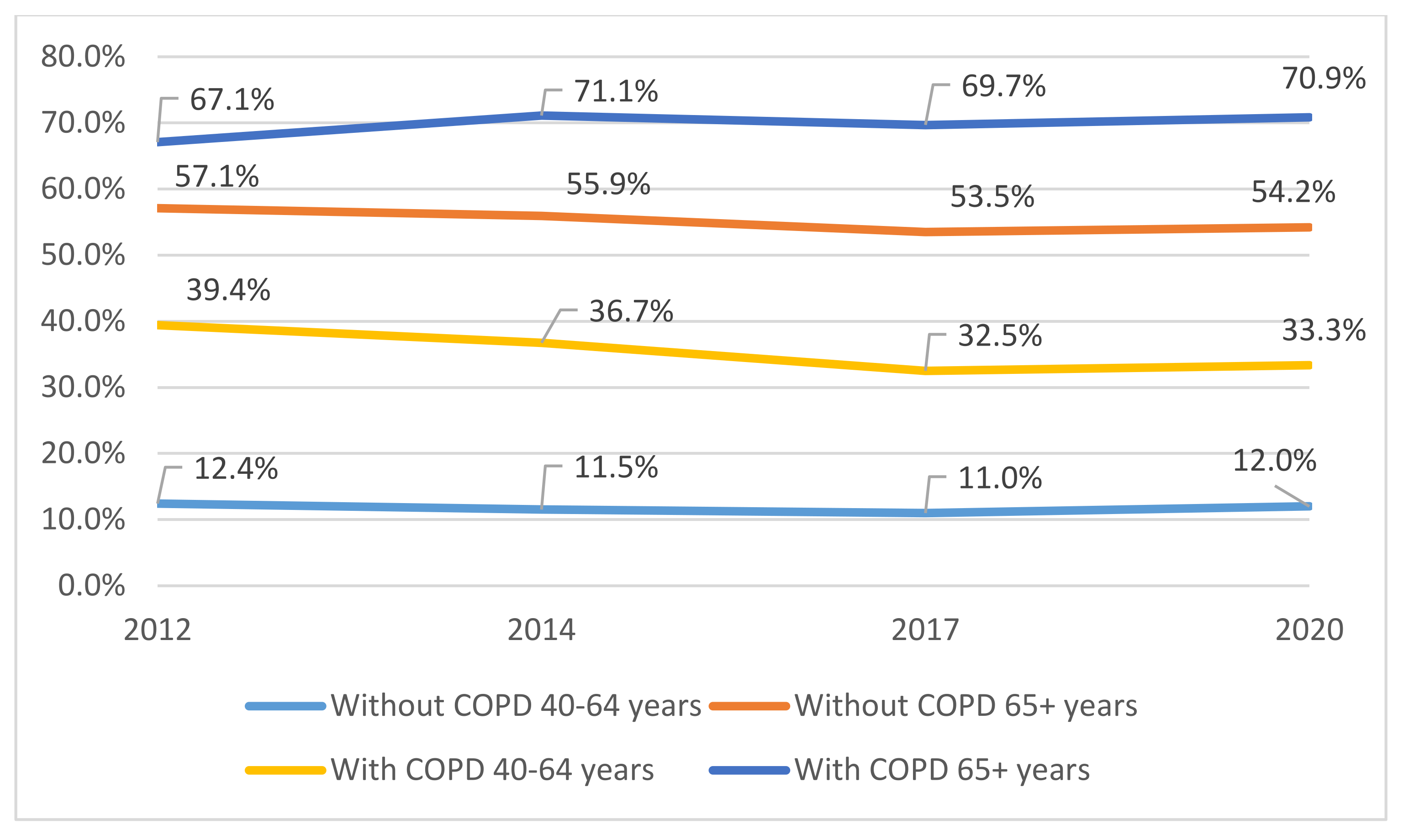
3.1. Influenza Vaccination Uptake in the COPD Population from 2012 to 2020
3.2. Influenza Vaccine Uptake among COPD Participants in the EHSS2020 According to Study Variables
3.3. Multivariable Analysis to Identify Variables Independently Associated with Influenza Vaccine Uptake among COPD Participants in the EHSS2020
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Viegi, G.; Pistelli, F.; Sherrill, D.L.; Maio, S.; Baldacci, S.; Carrozzi, L. Definition, epidemiology and natural history of COPD. Eur. Respir. J. 2007, 30, 993–1013. [Google Scholar] [CrossRef]
- Rabe, K.F.; Hurd, S.; Anzueto, A.; Barnes, P.J.; Buist, S.A.; Calverley, P.; Fukuchi, Y.; Jenkins, C.; Rodriguez-Roisin, R.; van Weel, C.; et al. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am. J. Respir. Crit. Care Med. 2007, 176, 532–555. [Google Scholar] [CrossRef]
- Adeloye, D.; Chua, S.; Lee, C.; Basquill, C.; Papana, A.; Theodoratou, E.; Nair, H.; Gasevic, D.; Sridhar, D.; Campbell, H.; et al. Global Health Epidemiology Reference Group (GHERG). Global and regional estimates of COPD prevalence: Systematic review and meta-analysis. J. Glob. Health 2015, 5, 020415. [Google Scholar] [CrossRef] [PubMed]
- Hilleman, D.E.; Dewan, N.; Malesker, M.; Friedman, M. Pharmacoeconomic evaluation of COPD. Chest 2000, 118, 1278–1285. [Google Scholar] [CrossRef] [PubMed]
- Seemungal, T.A.R.; Donaldson, G.C.; Paul, E.A.; Bestall, J.C.; Jeffries, D.J.; Wedzicha, J.A. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 1998, 157, 141822. [Google Scholar] [CrossRef]
- Soler Cataluña, J.J.; Martínez García, M.A.; Román Sánchez, P.; Salcedo, E.; Navarro, M.; Ochando, R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax 2005, 60, 925–931. [Google Scholar] [CrossRef]
- Miratvilles, M.; Anzueto, A. Role of infection in exacerbations of chronic obstructive pulmonary disease. Curr. Opin. Pulm. Med. 2015, 21, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Mohan, A.; Chandra, S.; Agarwal, D.; Guleria, R.; Broor, S.; Gaur, B.; Pandey, R.M. Prevalence of viral infection detected by PCR and RT-PCR in patients with acute exacerbation of COPD: A systematic review. Respirology 2010, 15, 536–542. [Google Scholar] [CrossRef] [PubMed]
- Montufar Andrade, F.; Díaz Santos, G.A.; Matiz, C.; Munive, A.A.; Pacheco, M. Exacerbación aguda de EPOC en la época de COVID-19. Rev. Colomb. De Neumol. 2020, 32, 47–57. [Google Scholar] [CrossRef]
- O’Donnell, D.E.; Aaron, S.; Bourbeau, J.; Hernandez, P.; Marciniuk, D.D.; Balter, M.; Ford, G.; Gervais, A.; Goldstein, R.; Hodder, R.; et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease-2007 update. Can. Respir. J. 2007, 14, 5B–32B. [Google Scholar] [CrossRef] [PubMed]
- Miravitlles, M.; Calle, M.; Molina, J.; Almagro, P.; Gómez, J.T.; Trigueros, J.A.; Cosío, B.G.; Casanova, C.; López-Campos, J.L.; Riesco, J.A.; et al. Spanish COPD Guidelines (GesEPOC) 2021, Updated Pharmacological treatment of stable COPD. Arch. Bronconeumol. 2021, 58, T69–T81. [Google Scholar] [CrossRef]
- Mereckiene, J.; Cotter, S.; Nicoll, A.; Lopalco, P.; Noori, T.; Weber, J.; D’Ancona, F.; Levy-Bruhl, D.; Dematte, L.; Giambi, C.; et al. VENICE project gatekeepers group. Seasonal influenza immunisation in Europe. Overview of recommendations and vaccination coverage for three seasons: Pre-pandemic (2008/09), pandemic (2009/10) and post-pandemic (2010/11). Eurosurveillance 2014, 19, 20780. [Google Scholar] [CrossRef] [PubMed]
- Prins, W.; Butcher, E.; Hall, L.L.; Puckrein, G.; Rosof, B. Improving adult inmunization equity: Where do the published research literature and existing resources lead? Vaccine 2017, 35, 3020–3025. [Google Scholar] [CrossRef]
- Tan, L.L.J. A review of the key factors to improve adult immunization coverage rates: What can the clinician do? Vaccine 2018, 36, 5373–5378. [Google Scholar] [CrossRef] [PubMed]
- Coupland, C.; Harcourt, S.; Vinogradova, Y.; Smith, G.; Joseph, C.; Pringle, M.; Hippisley-Cox, J. Inequalities in uptake of influenza vaccine by deprivation and risk group: Time trends analysis. Vaccine 2007, 25, 7363–7371. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.R.; Mason, B.W.; Beer, L.; Scourfield, S.; James-Hatherill, H.; Hayes, S. Surveillance of influenza immunisation uptake in people aged under 65 years with chronic disease. Vaccine 2006, 24, 7027–7029. [Google Scholar] [CrossRef] [PubMed]
- Chiatti, C.; Barbadoro, P.; Marigliano, A.; Ricciardi, A.; Di Stanislao, F.; Prospero, E. Determinants of influenza vaccination among the adult and older Italian population with chronic obstructive pulmonary disease: A secondary analysis of the multipurpose ISTAT survey on health and health care use. Hum. Vaccines 2011, 7, 1021–1025. [Google Scholar] [CrossRef] [PubMed]
- Santos-Sancho, J.M.; Jimenez-Trujillo, I.; Hernández-Barrera, V.; López-de Andrés, A.; Carrasco-Garrido, P.; Ortega-Molina, P.; Jiménez-García, R. Influenza vaccination coverage and uptake predictors among Spanish adults suffering COPD. Hum. Vaccines Immunother. 2012, 8, 938–945. [Google Scholar] [CrossRef] [PubMed]
- Ariñez Fernández, M.C.; Hernández Barrera, V.; García Carballo, M.M.; Gil de Miguel, A.; Carrasco Garrido, P.; Jiménez García, R. Cumplimiento de vacunación frente a la gripe y el neumococo en pacientes con enfermedad obstructiva crónica atendidos en atención primaria en Galicia. Vacunas 2006, 2, 57–63. [Google Scholar] [CrossRef]
- Garrastazu, R.; García-Rivero, J.L.; Ruiz, M.; Helguera, J.M.; Arenal, S.; Bonnardeux, C.; León, C.; Llorca, J.; Santibañez, M. Prevalence of Influenza Vaccination in Chronic Obstructive Pulmonary Disease Patients and Impact on the Risk of Severe Exacerbations. Arch. Bronconeumol. 2016, 52, 88–95. [Google Scholar] [CrossRef]
- Jiménez García, R.; Ariñez Fernandez, M.C.; Garcia Carballo, M.; Hernández Barrera, V.; de Miguel, A.G.; Carrasco Garrido, P. Influenza vaccination coverage and related factors among Spanish patients with chronic obstructive pulmonary disease. Vaccine 2005, 23, 3679–3686. [Google Scholar] [CrossRef] [PubMed]
- López de Andrés, A.; Carrasco Garrido, P.; Hernández Barrera, V.; de Miguel, A.G.; Jiménez García, R. Coverages and factors associated with influenza vaccination among subjects with chronic respiratory diseases in Spain. Eur. J. Public Health 2008, 18, 173–177. [Google Scholar] [CrossRef]
- Mayo Montero, E.; Hernández Barrera, V.; Carrasco Garrido, P.; Gil de Miguel, A.; Jiménez García, R. Influenza vaccination among persons with chronic respiratory diseases: Coverage, related factors and timetrend,1993–2001. Public Health 2007, 121, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Vozoris, N.T.; Lougheed, M.D. Influenza vaccination among Canadians with chronic respiratory disease. Respir. Med. 2009, 103, 50–58. [Google Scholar] [CrossRef][Green Version]
- Montserrat-Capdevila, J.; Godoy, P.; Marsal, J.R.; Cruz, I.; Solanes, M. Efectividad de la vacunación antigripal para evitar el ingreso hospitalario por agudización de la enfermedad pulmonar obstructiva crónica. Effectiveness of influenza vaccination in preventing hospital admission due to exacerbations of chronic obstructive pulmonary disease. Enferm. Infecc. Microbiol. Clin. 2014, 32, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Nichol, K.L.; Baken, L.; Nelson, A. Relation between influenza vaccination and outpatient visits, hospitalization, and mortality in elderly persons with chronic lung disease. Ann. Int. Med. 1999, 130, 397–403. [Google Scholar] [CrossRef]
- Poole, P.J.; Chacko, E.; Wood-Baker, R.W.B.; Cates, C.J. Influenzae vaccine for patients with chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2006, 25, CD002733. [Google Scholar] [CrossRef]
- Menon, B.; Gurnani, M.; Aggarwal, B. Comparison of outpatient visits and hospitalisations, in patients with chronic obstructive pulmonary disease, before and after influenza vaccination. Int. J. Clin. Pract. 2008, 62, 593–598. [Google Scholar] [CrossRef] [PubMed]
- Guerin, N. Assessing immunization coverage: How and why? Vaccine 1998, 16, S81–S83. [Google Scholar] [CrossRef]
- Kamal, K.M.; Madhavan, S.S.; Amonkar, M.M. Determinants of adult influenza and pneumonia immunization rates. J. Am. Pharm. Assoc. 2003, 43, 403–411. [Google Scholar] [CrossRef]
- Kroneman, M.; Paget, W.J.; Van Essen, G.A. Influenza vaccination in Europe: An inventory of strategies to reach target populations and optimise vaccination uptake. Eurosurveillance 2003, 8, 130–138. [Google Scholar] [CrossRef]
- Ministerio de Sanidad. European Health Survey in Spain 2020 [Encuesta Europea de Salud en España 2020]. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/EncuestaEuropea/Enc_Eur_Salud_en_Esp_2020.htm (accessed on 22 October 2021).
- Ministerio de Sanidad. European Health Survey in Spain 2014 [Encuesta Europea de Salud en España 2014]. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/EncuestaEuropea/Enc_Eur_Salud_en_Esp_2014.htm (accessed on 22 October 2021).
- Ministerio de Sanidad. National Health Survey 2017 [Encuesta Nacional de Salud 2017]. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/encuestaNacional/encuesta2017.htm (accessed on 6 June 2021).
- Ministerio de Sanidad. National Health Survey 2011 [Encuesta Nacional de Salud 2011]. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/encuestaNacional/encuesta2011.htm (accessed on 22 October 2021).
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2021 Report). Available online: https://www.mscbs.gob.es/organizacion/sns/planCalidadSNS/pdf/GOLD_Report_2015_Apr2.pdf (accessed on 30 November 2021).
- Cimen, P.; Unlu, M.; Kirakli, C.; Katgi, N.; Ucsular, F.D.; Ayranci, A.; Guclu, S.Z. Should Patients with COPD Be Vaccinated? Respir. Care 2015, 60, 239–243. [Google Scholar] [CrossRef]
- Eagan, T.M.; Hardie, J.A.; Jul-Larsen, A.; Grydeland, T.B.; Bakke, P.S.; Cox, R.J. Self-reported influenza vaccination and protective serum antibody titers in a cohort of COPD patients. Respir. Med. 2016, 115, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Plans Rubió, P. Prevention and control of influenza in persons with chronic obstructive pulmonary disease. Int. J. Chronic Obstr. Pulm. Dis. 2007, 2, 41–53. [Google Scholar] [CrossRef] [PubMed]
- Harper, S.A.; Fukuda, K.; Uyeki, T.M.; Cox, N.J.; Bridges, C.B. Advisory Committee on Immunization Practices (ACIP) Centers for Disease Control and Prevention. Prevention and control of influenza: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. 2005, 54, 1–40. [Google Scholar] [PubMed]
- Ruiz Azcona, L.; Román-Rodriguez, M.; Llort Bove, M.; Van Boven, J.F.M.; Santibáñez Marguello, M. Prevalence of seasonal influenza vaccination in chronic obstructive pulmonary disease (COPD) patients in the Balearic Islands (Spain) and its effect on COPD exacerbations: A population-based retrospective cohort study. Int. J. Environ. Res. Public Health 2020, 17, 4027. [Google Scholar] [CrossRef] [PubMed]
- Astray-Mochales, J.; López de Andrés, A.; Hernández-Barrera, V.; Rodríguez-Rieiro, C.; Carrasco Garrido, P.; Esteban-Vasallo, M.D.; Domínguez-Berjón, M.F.; Jimenez-Trujillo, I.; Jiménez-García, R. Influenza vaccination coverages among high risk subjects and health care workers in Spain. Results of two consecutive National Health Surveys (2011–2014). Vaccine 2016, 34, 4898–4904. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Huedo, M.A.; Lopez-De-Andrés, A.; Mora-Zamorano, E.; Hernández-Barrera, V.; Jiménez-Trujillo, I.; Zamo-rano-Leon, J.J.; Jiménez-García, R. Decreasing influenza vaccine coverage among adults with high-risk chronic diseases in Spain from 2014 to 2017. Hum. Vaccines Immunother. 2020, 16, 95–99. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Sanidad. Vaccination Coverage. Statistical Data [Coberturas de Vacunación. Datos Estadísticos]. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/vacunaciones/calendario-y-coberturas/coberturas/ (accessed on 4 January 2022).
- Info BDCAP. Num 4. Flu Vaccination Coverage in Risk Groups [Cobertura de Vacunación Antigripal en los Grupos de Riesgo]. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SIAP/4Cob_vac_antigripal.pdf (accessed on 4 January 2022).
- Portero de la Cruz, S.; Cebrino, J. Trends, Coverage and Influencing Determinants of Influenza Vaccination in the Elderly: A Population-Based National Survey in Spain (2006-2017). Vaccines 2020, 8, 327. [Google Scholar] [CrossRef] [PubMed]
- Dios-Guerra, C.; Carmona-Torres, J.M.; López-Soto, P.J.; Morales-Cané, I.; Rodríguez-Borrego, M.A. Prevalence and factors associated with influenza vaccination of persons over 65 years old in Spain (2009–2014). Vaccine 2017, 35, 7095–7100. [Google Scholar] [CrossRef]
- Jenkins, C.R.; Chapman, K.R.; Donohue, J.F.; Roche, N.; Tsiligianni, I.; Han, M.K. Improving the management of COPD in women. Chest 2017, 15, 686–696. [Google Scholar] [CrossRef] [PubMed]
- Kini, A.; Morgan, R.; Kuo, H.; Shea, P.; Shapiro, J.; Leng, S.X.; Pekosz, A.; Klein, S.L. Differences and disparities in seasonal influenza vaccine, acceptance, adverse reactions, and coverage by age, sex, gender, and race. Vaccine 2021, 40, 1643–1654. [Google Scholar] [CrossRef] [PubMed]
- Jiménez, R.; Larrauri, A.; Carrasco, P.; Esteba, J.; Gómez López, L.I.; Gil, A. Influenza coverages in Spain and vaccination-related factors in the subgroup aged 50–64 years. Vaccine 2003, 21, 3550–3555. [Google Scholar] [CrossRef]
- Jiménez-García, R.; Mayo-Montero, E.; Hernández-Barrera, V.; Sierra-Moros, M.J.; Pachón del Amo, I.; Carrasco-Garrido, P.; Martinez-Hernandez, D.; de Miguel, A.G. Evolution of anti-influenza vaccination coverage in Spain from 1993 to 2001. Vaccine 2005, 23, 2844–2850. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S.; Williams, S.G.; Mannino, D.M.; Redd, S.C. Influenza vaccination coverage among adults with asthma: Findings from the 2000 Behavioral Risk Factor Surveillance System. Am. J. Med. 2004, 116, 555–558. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Saeed, G.J.; Valero-Elizondo, J.; Mszar, R.; Grandhi, G.R.; Cainzos-Achirica, M.; Omer, S.B.; Nasir, K. Prevalence and Disparities in Influenza Vaccination Among Patients with COPD in the United States. Chest 2021, 159, 1411–1414. [Google Scholar] [CrossRef]
- Honkanen, P.O.; Keistinen, T.; Kivela, S.L. The impact of vaccination strategy and methods of information on influenza and pneumococcal vaccination coverage in the elderly population. Vaccine 1997, 15, 317–320. [Google Scholar] [CrossRef]
- Jain, A.; van Hoek, A.J.; Boccia, D.; Thomas, S.L. Lower vaccine uptake amongst older individuals living alone: A systematic review and meta-analysis of social determinants of vaccine uptake. Vaccine 2017, 35, 2315–2328. [Google Scholar] [CrossRef] [PubMed]
- Lucyk, K.; Simmonds, K.A.; Lorenzetti, D.L.; Drews, S.J.; Svenson, L.W.; Russell, M.L. The association between influenza vaccination and socioeconomic status in high income countries varies by the measure used: A systematic review. BMC Med Res. Methodol. 2019, 19, 153. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Rieiro, C.; Domínguez-Berjón, M.F.; Esteban-Vasallodomínguez-Berjón, M.D.; Cuadrado, A.R.; Carrasco-Garrido, P.; Jiménez-García, R. Coverage and predictors of influenza vaccine uptake among adults aged 16 to 59 years suffering from a chronic condition in Madrid, Spain. Hum. Vaccines 2011, 7, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-García, R.; Hernández-Barrera, V.; de Andres, A.L.; Jimenez-Trujillo, I.; Esteban-Hernández, J.; Carrasco-Garrido, P. Gender influence in influenza vaccine uptake in Spain: Time trends analysis (1995-2006). Vaccine 2010, 28, 6169–6175. [Google Scholar] [CrossRef] [PubMed]
- Tuells, J.; Caballero, P.; Nolasco, A.; Montagud, E. Factores asociados a la predisposición a vacunarse contra la gripe pandémica A/H1N1 en población adulta del Departamento de Salud de Elche (España) [Factors associated with willingness to be vaccinated against pandemic flu A/H1N1 in the adult population of the Health Department of Elche (Spain)]. An. Del Sist. Sanit. Navar. 2012, 35, 251–260. [Google Scholar] [CrossRef][Green Version]
- Blanck, P.R.; Schwenkglenks, M.; Szucs, T.D. Influenza vaccination coverage rates in five European countries during season 2006/07 and trends over six consecutive seasons. BMC Public Health 2008, 8, 272. [Google Scholar] [CrossRef]
- Ompad, D.C.; Galea, S.; Vlahov, D. Distribution of influenza vaccine to high -risk groups. Epidemiol. Rev. 2006, 28, 54–70. [Google Scholar] [CrossRef] [PubMed]
- Muller, D.; Nguyen -Van-Tam, J.S.; Szucs, T.D. Influenza vaccination coverage rates in the UK: A comparison of two monitoring methods during the 2002-2003 and 2003-2004 seasons. Public Health 2006, 120, 1074–1080. [Google Scholar] [CrossRef]
- Donald, R.M.; Baken, L.; Nelson, A.; Nichol, K.L. Validation of self-report of influenza and pneumococcal vaccination status in elderly outpatients. Am. J. Prev. Med. 1999, 16, 173–177. [Google Scholar] [CrossRef]
- Skull, S.A.; Andrews, R.M.; Byrnes, G.B.; Kelly, H.A.; Nolan, T.M.; Brown, G.V.; Campbell, D.A. Validity of self-reported influenza and pneumococcal vaccination status among a cohort of hospitalized elderly inpatients. Vaccine 2007, 25, 4775–4783. [Google Scholar] [CrossRef] [PubMed]
- Irving, S.A.; Donahue, J.G.; Shay, D.K.; Ellis-Coyle, T.L.; Belongia, E.A. Evaluation of self-reported and registry-based influenza vaccination status in a Wisconsin cohort. Vaccine 2009, 27, 6546–6549. [Google Scholar] [CrossRef] [PubMed]
- Trigueros, J.A.; Riesco, J.A.; Alcázar-Navarrete, B.; Campuzano, A.; Pérez, J. Clinical Features of Women With COPD: Sex Differences in a Cross-Sectional Study in Spain (“The ESPIRAL-ES Study”). Int. J. Chronic Obstr. Pulm. Dis. 2019, 14, 2469–2478. [Google Scholar] [CrossRef] [PubMed]
- Perez, T.A.; Castillo, E.G.; Ancochea, J.; Pastor Sanz, M.T.; Almagro, P.; Martínez-Camblor, P.; Miravitlles, M.; Rodríguez-Carballeira, M.; Navarro, A.; Lamprecht, B.; et al. Sex differences between women and men with COPD: A new analysis of the 3CIA study. Respir. Med. 2020, 171, 106105. [Google Scholar] [CrossRef] [PubMed]
| COPD | Variable | Categories | Odds Ratio | 95% Confidence Interval | |
|---|---|---|---|---|---|
| Yes | Sex | Women | Ref | ||
| Men | 1.283 | 1.119 | 1.470 | ||
| Age groups | 40–64 years | Ref | - | - | |
| 65–74 years | 3.243 | 2.734 | 3.848 | ||
| 75 years and over | 4.968 | 4.232 | 5.831 | ||
| Year of survey | 2012 | Ref | - | - | |
| 2014 | 1.075 | 0.888 | 1.301 | ||
| 2017 | 0.973 | 0.808 | 1.173 | ||
| 2020 | 1.022 | 0.839 | 1.245 | ||
| No | Sex | Men | Ref | - | - |
| Women | 1.088 | 1.045 | 1.133 | ||
| Age groups | 40–64 years | Ref | - | - | |
| 65–74 years | 6.267 | 5.971 | 6.577 | ||
| 75 years and over | 13.733 | 13.079 | 14.420 | ||
| Year of survey | 2012 | Ref | - | - | |
| 2014 | 0.944 | 0.890 | 1.000 | ||
| 2017 | 0.863 | 0.815 | 0.915 | ||
| 2020 | 0.914 | 0.863 | 0.968 | ||
| Variable | Categories | % | 95% CI | p |
|---|---|---|---|---|
| Age groups | 40–64 years | 33.3 | 30.1–36.5 | <0.001 |
| 65–74 years | 65.8 | 59.6–71.9 | ||
| 75 years and over | 74.5 | 69.7–79.3 | ||
| Sex | Man | 61.4 | 56.6–66.2 | 0.040 |
| Women | 54.4 | 49.8–59.0 | ||
| Marital status | Married | 55.6 | 50.8–60.3 | 0.117 |
| Not married | 59.9 | 55.2–64.6 | ||
| Education level | Primary school or less | 66.3 | 61.9–70.7 | <0.001 |
| Secondary school or equivalent | 48.8 | 43.1–54.5 | ||
| Higher education | 46.0 | 36.2–55.8 | ||
| Social class | High | 50.6 | 40.0–61.2 | 0.205 |
| Medium | 59.8 | 53.9–65.8 | ||
| Low | 57.9 | 53.4–62.4 | ||
| Self-rated health | Very good/good | 53.1 | 46.8–59.5 | 0.089 |
| Fair/poor/very poor | 59.6 | 55.6–63.5 | ||
| Obesity | No | 57.4 | 53.3–61.5 | 0.581 |
| Yes | 56.8 | 50.3–63.4 | ||
| Current smoking | No | 63.8 | 60.1–67.6 | <0.001 |
| Yes | 39.0 | 32.3–45.7 | ||
| Alcohol consumption | No | 61.0 | 56.7–65.2 | 0.017 |
| Yes | 52.7 | 47.3–58.0 | ||
| Physical activity | No | 56.4 | 51.9–60.8 | 0.366 |
| Yes | 59.5 | 54.5–64.6 | ||
| Heart disease | No | 54.9 | 50.9–58.8 | 0.007 |
| Yes | 65.1 | 59.0–71.2 | ||
| Cancer | No | 56.0 | 52.5–59.6 | 0.008 |
| Yes | 69.9 | 61.0–78.8 | ||
| Cerebrovascular diseases | No | 57.8 | 54.3–61.2 | 0.896 |
| Yes | 56.9 | 43.3–70.5 | ||
| Diabetes | No | 56.3 | 52.5–60.1 | 0.114 |
| Yes | 62.8 | 55.8–69.8 | ||
| Renal disease | No | 57.8 | 54.3–61.4 | 0.899 |
| Yes | 57.1 | 47.3–66.9 | ||
| Mental disease | No | 59.5 | 55.3–63.7 | 0.173 |
| Yes | 54.7 | 49.3–60.2 | ||
| Any chronic condition | No | 53.0 | 47.0–59.0 | 0.059 |
| Yes | 59.9 | 55.9–63.9 |
| Variable | Categories | Odds Ratio | 95% Confidence Interval | |
|---|---|---|---|---|
| Sex | Women | Ref | ||
| Men | 1.336 | 1.022 | 2.199 | |
| Age groups | 40–64 years | Ref | - | - |
| 65–74 years | 3.844 | 2.667 | 5.541 | |
| 75 years and over | 5.855 | 4.126 | 8.309 | |
| Current smoking | Yes | Ref | - | - |
| No | 1.508 | 1.041 | 2.183 | |
| Heart disease | No | Ref | - | - |
| Yes | 1.352 | 1.039 | 1.994 | |
| Cancer | No | Ref | - | - |
| Yes | 1.273 | 1.006 | 1.768 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fuentes-Alonso, M.; Jimenez-Garcia, R.; Lopez-de-Andres, A.; Zamorano-Leon, J.J.; Carabantes-Alarcon, D.; Jimenez-Trujillo, I.; Sanz-Rojo, S.; de Miguel-Diez, J. Time Trends (2012–2020), Sex Differences and Predictors for Influenza Vaccination Uptake among Individuals with Chronic Obstructive Pulmonary Disease in Spain. J. Clin. Med. 2022, 11, 1423. https://doi.org/10.3390/jcm11051423
Fuentes-Alonso M, Jimenez-Garcia R, Lopez-de-Andres A, Zamorano-Leon JJ, Carabantes-Alarcon D, Jimenez-Trujillo I, Sanz-Rojo S, de Miguel-Diez J. Time Trends (2012–2020), Sex Differences and Predictors for Influenza Vaccination Uptake among Individuals with Chronic Obstructive Pulmonary Disease in Spain. Journal of Clinical Medicine. 2022; 11(5):1423. https://doi.org/10.3390/jcm11051423
Chicago/Turabian StyleFuentes-Alonso, Marta, Rodrigo Jimenez-Garcia, Ana Lopez-de-Andres, Jose J. Zamorano-Leon, David Carabantes-Alarcon, Isabel Jimenez-Trujillo, Sara Sanz-Rojo, and Javier de Miguel-Diez. 2022. "Time Trends (2012–2020), Sex Differences and Predictors for Influenza Vaccination Uptake among Individuals with Chronic Obstructive Pulmonary Disease in Spain" Journal of Clinical Medicine 11, no. 5: 1423. https://doi.org/10.3390/jcm11051423
APA StyleFuentes-Alonso, M., Jimenez-Garcia, R., Lopez-de-Andres, A., Zamorano-Leon, J. J., Carabantes-Alarcon, D., Jimenez-Trujillo, I., Sanz-Rojo, S., & de Miguel-Diez, J. (2022). Time Trends (2012–2020), Sex Differences and Predictors for Influenza Vaccination Uptake among Individuals with Chronic Obstructive Pulmonary Disease in Spain. Journal of Clinical Medicine, 11(5), 1423. https://doi.org/10.3390/jcm11051423







