Trends in the Management of Headache Disorders in US Emergency Departments: Analysis of 2007–2018 National Hospital Ambulatory Medical Care Survey Data
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Sources
2.2. Study Cohort
2.3. Main Outcomes Measures
2.4. Patient and Hospital Characteristics
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics between 2015 and 2018
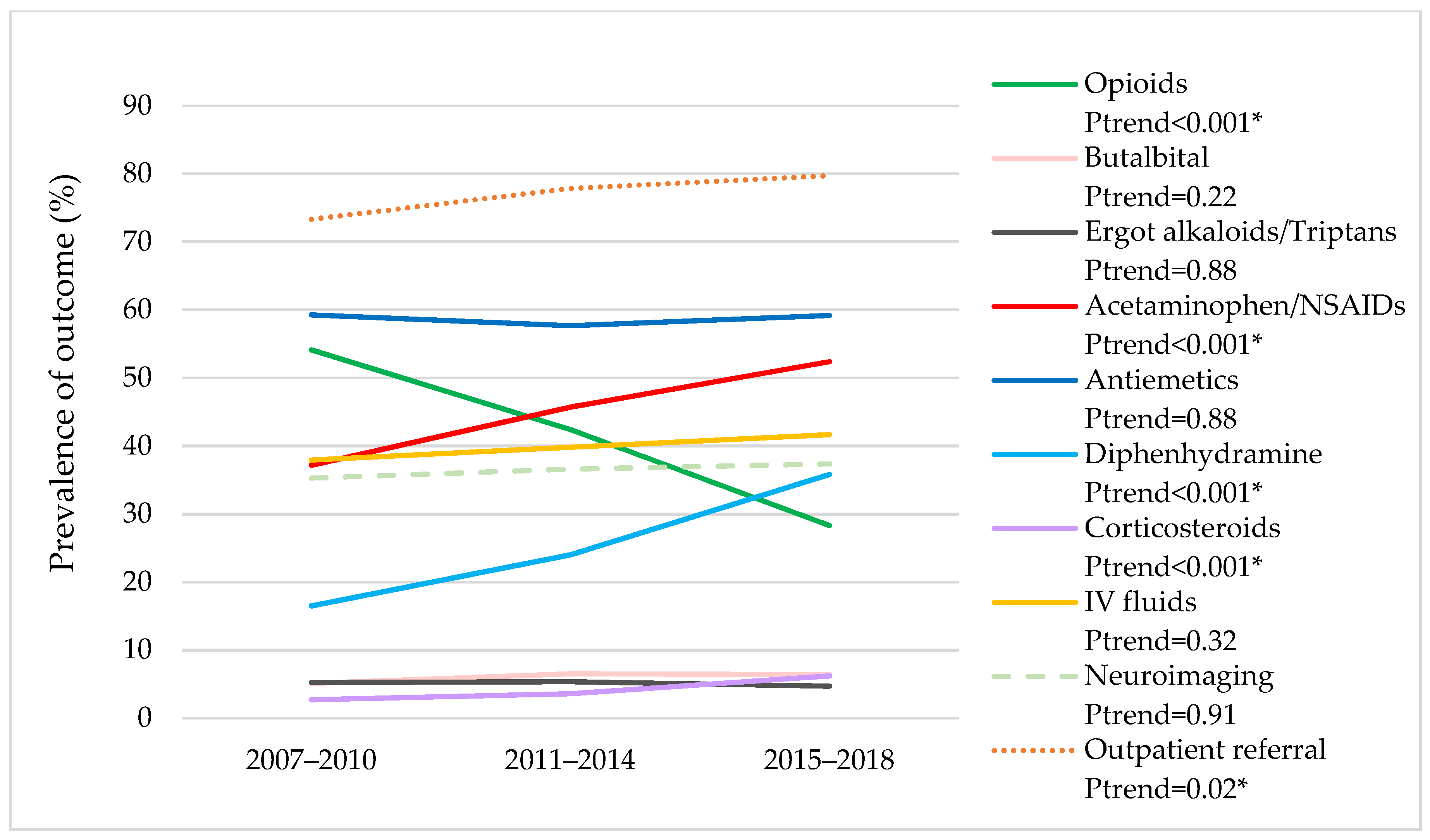
3.2. Trends in Medication Use, Neuroimaging Use, and Outpatient Referral for Follow-Up between 2007 and 2018
3.3. Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stovner, L.; Hagen, K.; Jensen, R.; Katsarava, Z.; Lipton, R.; Scher, A.; Steiner, T.; Zwart, J.A. The global burden of headache: A documentation of headache prevalence and disability worldwide. Cephalalgia 2007, 27, 193–210. [Google Scholar] [CrossRef] [PubMed]
- National Hospital Ambulatory Medical Care Survey: 2017 Emergency Department Summary Tables. NCHS. Published January 2020. Available online: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2017_ed_web_tables-508.pdf (accessed on 30 November 2021).
- Friedman, B.W. Migraine in the emergency department. Neurol. Clin. 2019, 37, 743–752. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M. Headache Classification Committee of the International Headache Society (IHS) The International classification of headache disorders. Cephalalgia 2018, 38, 1–211. [Google Scholar] [CrossRef]
- Friedman, B.W.; Grosberg, B.M. Diagnosis and management of the primary headache disorders in the emergency department setting. Emerg. Med. Clin. N. Am. 2009, 27, 71–87. [Google Scholar] [CrossRef] [Green Version]
- Hainer, B.L.; Matheson, E.M. Approach to acute headache in adults. Am. Fam. Physician 2013, 87, 682–687. [Google Scholar]
- Do, T.P.; Remmers, A.; Schytz, H.W.; Schankin, C.; Nelson, S.E.; Obermann, M.; Hansen, J.M.; Sinclair, A.J.; Gantenbein, A.R.; Schoonman, G.G. Red and orange flags for secondary headaches in clinical practice: SNNOOP10 list. Neurology 2019, 92, 134–144. [Google Scholar] [CrossRef]
- Kanzaria, H.K.; Hoffman, J.R.; Probst, M.A.; Caloyeras, J.P.; Berry, S.H.; Brook, R.H. Emergency physician perceptions of medically unnecessary advanced diagnostic imaging. Acad. Emerg. Med. 2015, 22, 390–398. [Google Scholar] [CrossRef]
- Silberstein, S.D. Practice parameter: Evidence-based guidelines for migraine headache (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2000, 55, 754–762. [Google Scholar] [CrossRef] [Green Version]
- Loder, E.; Weizenbaum, E.; Frishberg, B.; Silberstein, S. Choosing wisely in headache medicine: The American Headache Society’s list of five things physicians and patients should question. Headache 2013, 53, 1651–1659. [Google Scholar] [CrossRef]
- Expert Panel on Neurologic Imaging; Whitehead, M.T.; Cardenas, A.M.; Corey, A.S.; Policeni, B.; Burns, J.; Chakraborty, S.; Crowley, R.W.; Jabbour, P.; Ledbetter, L.N.; et al. ACR appropriateness criteria(R) headache. J. Am. Coll. Radiol. 2019, 16, S364–S377. [Google Scholar] [CrossRef] [Green Version]
- Evans, R.W.; Burch, R.C.; Frishberg, B.M.; Marmura, M.J.; Mechtler, L.L.; Silberstein, S.D.; Turner, D.P. Neuroimaging for migraine: The american headache society systematic review and evidence-based guideline. Headache 2020, 60, 318–336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cote, D.J.; Laws, E.R., Jr. The ethics of “choosing wisely”: The use of neuroimaging for uncomplicated headache. Neurosurgery 2017, 80, 816–819. [Google Scholar] [CrossRef] [PubMed]
- Orr, S.L.; Friedman, B.W.; Christie, S.; Minen, M.T.; Bamford, C.; Kelley, N.E.; Tepper, D. Management of adults with acute migraine in the emergency department: The American headache society evidence assessment of parenteral pharmacotherapies. Headache 2016, 56, 911–940. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weinman, D.; Nicastro, O.; Akala, O.; Friedman, B.W. Parenteral treatment of episodic tension-type headache: A systematic review. Headache 2014, 54, 260–268. [Google Scholar] [CrossRef]
- Robbins, M.S.; Starling, A.J.; Pringsheim, T.M.; Becker, W.J.; Schwedt, T.J. Treatment of cluster headache: The American headache society evidence-based guidelines. Headache 2016, 56, 1093–1106. [Google Scholar] [CrossRef] [Green Version]
- Griffith, J.D.; Mycyk, M.B.; Kyriacou, D.N. Metoclopramide versus hydromorphone for the emergency department treatment of migraine headache. J. Pain. 2008, 9, 88–94. [Google Scholar] [CrossRef]
- Friedman, B.W.; Irizarry, E.; Solorzano, C.; Latev, A.; Rosa, K.; Zias, E.; Vinson, D.R.; Bijur, P.E.; Gallagher, E.J. Randomized study of IV prochlorperazine plus diphenhydramine vs. IV hydromorphone for migraine. Neurology 2017, 89, 2075–2082. [Google Scholar] [CrossRef]
- Tepper, S.J. Opioids should not be used in migraine. Headache 2012, 52, 30–34. [Google Scholar] [CrossRef]
- Bigal, M.E.; Serrano, D.; Buse, D.; Scher, A.; Stewart, W.F.; Lipton, R.B. Acute migraine medications and evolution from episodic to chronic migraine: A longitudinal population-based study. Headache 2008, 48, 1157–1168. [Google Scholar] [CrossRef]
- Bigal, M.E.; Lipton, R.B. Excessive opioid use and the development of chronic migraine. Pain 2009, 142, 179–182. [Google Scholar] [CrossRef]
- Scher, A.I.; Stewart, W.F.; Ricci, J.A.; Lipton, R.B. Factors associated with the onset and remission of chronic daily headache in a population-based study. Pain 2003, 106, 81–89. [Google Scholar] [CrossRef] [Green Version]
- Katsarava, Z.; Schneeweiss, S.; Kurth, T.; Kroener, U.; Fritsche, G.; Eikermann, A.; Diener, H.C.; Limmroth, V. Incidence and predictors for chronicity of headache in patients with episodic migraine. Neurology 2004, 62, 788–790. [Google Scholar] [CrossRef] [PubMed]
- Jakubowski, M.; Levy, D.; Goor-Aryeh, I.; Collins, B.; Bajwa, Z.; Burstein, R. Terminating migraine with allodynia and ongoing central sensitization using parenteral administration of COX1/COX2 inhibitors. Headache 2005, 45, 850–861. [Google Scholar] [CrossRef]
- Ho, T.W.; Rodgers, A.; Bigal, M.E. Impact of recent prior opioid use on rizatriptan efficacy. A post hoc pooled analysis. Headache 2009, 49, 395–403. [Google Scholar] [CrossRef]
- Office of the Assistant Secretary for Planning and Evaluation Opioid Abuse in the U.S. and HHS Actions to Address Opioid-Drug Related Overdoses and Deaths. Published 26 March 2015. Available online: https://aspe.hhs.gov/basic-report/opioid-abuse-us-and-hhs-actions-address-opioid-drug-related-overdoses-and-deaths (accessed on 4 May 2017).
- Young, N.; Silverman, D.; Bradford, H.; Finkelstein, J. Multicenter prevalence of opioid medication use as abortive therapy in the ED treatment of migraine headaches. Am. J. Emerg. Med. 2017, 35, 1845–1849. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, L.H.; Cowan, R.P. Comparison of parenteral treatments of acute primary headache in a large academic emergency department cohort. Cephalalgia 2015, 35, 807–815. [Google Scholar] [CrossRef] [Green Version]
- Tornabene, S.V.; Deutsch, R.; Davis, D.P.; Chan, T.C.; Vilke, G.M. Evaluating the use and timing of opioids for the treatment of migraine headaches in the emergency department. J. Emerg. Med. 2009, 36, 333–337. [Google Scholar] [CrossRef]
- Center for Disease Control and Prevention. National Center for Health Statistics. About the Ambulatory Health Care Surveys. 6 September 2019. Available online: https://www.cdc.gov/nchs/ahcd/about_ahcd.htm#NHAMCS (accessed on 18 October 2021).
- Center for Disease Control and Prevention. National Center for Health Statistics. Scope and Sample Design. 6 November 2015. Available online: https://www.cdc.gov/nchs/ahcd/ahcd_scope.htm (accessed on 18 October 2021).
- Zhou, L.; Bhattacharjee, S.; Kwoh, C.K.; Tighe, P.J.; Malone, D.C.; Slack, M.; Wilson, D.L.; Brown, J.D.; Lo-Ciganic, W.H. Trends, patient and prescriber characteristics in gabapentinoid use in a sample of United States ambulatory care visits from 2003 to 2016. J. Clin. Med. 2019, 9, 83. [Google Scholar] [CrossRef] [Green Version]
- Jensen, M.P.; Smith, D.G.; Ehde, D.M.; Robinsin, L.R. Pain site and the effects of amputation pain: Further clarification of the meaning of mild, moderate, and severe pain. Pain 2001, 91, 317–322. [Google Scholar] [CrossRef]
- Center for Disease Control and Prevention. National Center for Health Statistics. Survey Methods and Analytic Guidelines. 6 February 2019. Available online: https://www.cdc.gov/nchs/ahcd/survey_methods.htm (accessed on 18 October 2021).
- Center for Disease Control and Prevention. National Center for Health Statistics. Reliability of Estimates. 6 November 2015. Available online: https://www.cdc.gov/nchs/ahcd/ahcd_estimation_reliability.htm (accessed on 18 October 2021).
- Austin, P.C. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar. Behav. Res. 2011, 46, 399–424. [Google Scholar] [CrossRef] [Green Version]
- Blumenthal, H.J.; Weisz, M.A.; Kelly, K.M.; Mayer, R.L.; Blonsky, J. Treatment of primary headache in the emergency department. Headache 2003, 43, 1026–1031. [Google Scholar] [CrossRef] [PubMed]
- Granato, A.; D’Acunto, L.; Morelli, M.E.; Bellavita, G.; Cominotto, F.; Manganotti, P. Lost diagnoses in not otherwise specified headache in Emergency Department. Acta Neurol. Belg. 2021, 121, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Vigano, A.; Savastano, E.; Petolicchio, B.; Toscano, M.; De Sanctis, R.; Maestrini, I.; Di Piero, V. A Study of clinical features and risk factors of self-referring emergency department headache patients: A comparison with headache center outpatients. Eur. Neurol. 2020, 83, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Friedman, B.W.; Hochberg, M.L.; Esses, D.; Grosberg, B.; Corbo, J.; Toosi, B.; Meyer, R.H.; Bijur, P.E.; Lipton, R.B.; Gallagher, E.J. Applying the international classification of headache disorders to the emergency department: An assessment of reproducibility and the frequency with which a unique diagnosis can be assigned to every acute headache presentation. Ann. Emerg. Med. 2007, 49, 409–419. [Google Scholar] [CrossRef]
- Munoz-Ceron, J.; Marin-Careaga, V.; Peña, L.; Mutis, J.; Ortiz, G. Headache at the emergency room: Etiologies, diagnostic usefulness of the ICHD 3 criteria, red and green flags. PLoS ONE 2019, 14, e0208728. [Google Scholar] [CrossRef]
- American College of Emergency Physicians Clinical Policies Subcommittee on Acute Headache; Godwin, S.A.; Cherkas, D.S.; Panagos, P.D.; Shih, R.D.; Byyny, R.; Wolf, S.J. Clinical policy: Critical issues in the evaluation and management of adult patients presenting to the emergency department with acute headache. Ann. Emerg. Med. 2019, 74, e41–e74. [Google Scholar] [CrossRef] [Green Version]
- Gleber, R.; Vilke, G.M.; Castillo, E.M.; Brennan, J.; Oyama, L.; Coyne, C.J. Trends in emergency physician opioid prescribing practices during the United States opioid crisis. Am. J. Emerg. Med. 2020, 38, 735–740. [Google Scholar] [CrossRef]
- Rui, P.; Santo, L.; Ashman, J.J. Trends in opioids prescribed at discharge from emergency departments among adults: United States, 2006–2017. Natl. Health Stat. Rep. 2020, 135, 1–12. [Google Scholar]
- Ruzek, M.; Richman, P.; Eskin, B.; Allegra, J.R. ED treatment of migraine patients has changed. Am. J. Emerg. Med. 2019, 37, 1069–1072. [Google Scholar] [CrossRef]
- Rosenberg, J.M.; Bilka, B.M.; Wilson, S.M.; Spevak, C. Opioid therapy for chronic pain: Overview of the 2017 US Department of Veterans Affairs and US Department of Defense Clinical practice guideline. Pain. Med. 2018, 19, 928–941. [Google Scholar] [CrossRef]
- Manchikanti, L.; Kaye, A.M.; Knezevic, N.N.; McAnally, H.; Slavin, K.; Trescot, A.M.; Blank, S.; Pampati, V.; Abdi, S.; Grider, J.S.; et al. Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of interventional pain physicians (ASIPP) guidelines. Pain Physician 2017, 20, S3–S92. [Google Scholar] [CrossRef] [PubMed]
- Dowell, D.; Haegerich, T.M.; Chou, R. CDC Guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm. Rep. 2016, 65, 1–49. [Google Scholar] [CrossRef] [PubMed]
- Friedman, B.W.; Garber, L.; Yoon, A.; Solorzano, C.; Wollowitz, A.; Esses, D.; Bijur, P.E.; Gallagher, E.J. Randomized trial of IV valproate vs. metoclopramide vs. ketorolac for acute migraine. Neurology 2014, 82, 976–983. [Google Scholar] [CrossRef]
- Friedman, B.W.; Corbo, J.; Lipton, R.B.; Bijur, P.E.; Esses, D.; Solorzano, C.; Gallagher, E.J. A trial of metoclopramide vs. sumatriptan for the emergency department treatment of migraines. Neurology 2005, 64, 463–468. [Google Scholar] [CrossRef]
- Talabi, S.; Masoumi, B.; Azizkhani, R.; Esmailian, M. Metoclopramide versus sumatriptan for treatment of migraine headache: A randomized clinical trial. J. Res. Med. Sci. 2013, 18, 695–698. [Google Scholar] [PubMed]
- Miller, M.A.; Levsky, M.E.; Enslow, W.; Rosin, A. Randomized evaluation of octreotide vs prochlorperazine for ED treatment of migraine headache. Am. J. Emerg. Med. 2009, 27, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Kostic, M.A.; Gutierrez, F.J.; Rieg, T.S.; Moore, T.S.; Gendron, R.T. A prospective, randomized trial of intravenous prochlorperazine versus subcutaneous sumatriptan in acute migraine therapy in the emergency department. Ann. Emerg. Med. 2010, 56, 1–6. [Google Scholar] [CrossRef]
- Tanen, D.A.; Miller, S.; French, T.; Riffenburgh, R.H. Intravenous sodium valproate versus prochlorperazine for the emergency department treatment of acute migraine headaches: A prospective, randomized, double-blind trial. Ann. Emerg. Med. 2003, 41, 847–853. [Google Scholar] [CrossRef]
- Mazer-Amirshahi, M.; Dewey, K.; Mullins, P.M.; van den Anker, J.; Pines, J.M.; Perrone, J.; Nelson, L. Trends in opioid analgesic use for headaches in US emergency departments. Am. J. Emerg. Med. 2014, 32, 1068–1073. [Google Scholar] [CrossRef]
- Grissinger, M. Preventing serious tissue injury with intravenous promethazine (phenergan). Pharm. Ther. 2009, 34, 175–176. [Google Scholar]
- Friedman, B.W.; Cabral, L.; Adewunmi, V.; Solorzano, C.; Esses, D.; Bijur, P.E.; Gallagher, E.J. Diphenhydramine as adjuvant therapy for acute migraine: An emergency department-based randomized clinical trial. Ann. Emerg. Med. 2016, 67, 32–39.e33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Erdur, B.; Tura, P.; Aydin, B.; Ozen, M.; Ergin, A.; Parlak, I.; Kabay, B. A trial of midazolam vs diphenhydramine in prophylaxis of metoclopramide-induced akathisia. Am. J. Emerg. Med. 2012, 30, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Friedman, B.W.; Bender, B.; Davitt, M.; Solorzano, C.; Paternoster, J.; Esses, D.; Bijur, P.; Gallagher, E.J. A randomized trial of diphenhydramine as prophylaxis against metoclopramide-induced akathisia in nauseated emergency department patients. Ann. Emerg. Med. 2009, 53, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Vinson, D.R.; Drotts, D.L. Diphenhydramine for the prevention of akathisia induced by prochlorperazine: A randomized, controlled trial. Ann. Emerg. Med. 2001, 37, 125–131. [Google Scholar] [CrossRef]
- Vinson, D.R. Diphenhydramine in the treatment of akathisia induced by prochlorperazine. J. Emerg. Med. 2004, 26, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Regan, L.A.; Hoffman, R.S.; Nelson, L.S. Slower infusion of metoclopramide decreases the rate of akathisia. Am. J. Emerg. Med. 2009, 27, 475–480. [Google Scholar] [CrossRef]
- Cavero-Redondo, I.; Alvarez-Bueno, C.; Pozuelo-Carrascosa, D.P.; Diez-Fernandez, A.; Notario-Pacheco, B. Risk of extrapyramidal side effects comparing continuous vs. bolus intravenous metoclopramide administration: A systematic review and meta-analysis of randomised controlled trials. J. Clin. Nurs. 2015, 24, 3638–3646. [Google Scholar] [CrossRef]
- Gray, S.L.; Anderson, M.L.; Dublin, S.; Hanlon, J.T.; Hubbard, R.; Walker, R.; Yu, O.; Crane, P.K.; Larson, E.B. Cumulative use of strong anticholinergics and incident dementia: A prospective cohort study. JAMA. Intern. Med. 2015, 175, 401–407. [Google Scholar] [CrossRef]
- Saran, J.S.; Barbano, R.L.; Schult, R.; Wiegand, T.J.; Selioutski, O. Chronic diphenhydramine abuse and withdrawal: A diagnostic challenge. Neurol. Clin. Pr. 2017, 7, 439–441. [Google Scholar] [CrossRef]
- Minen, M.T.; Tanev, K.; Friedman, B.W. Evaluation and treatment of migraine in the emergency department: A review. Headache 2014, 54, 1131–1145. [Google Scholar] [CrossRef]
- Nijjar, S.S.; Pink, L.; Gordon, A.S. Examination of migraine management in emergency departments. Pain Res. Manag. 2011, 16, 183–186. [Google Scholar] [CrossRef]
- Shao, Q.; Rascati, K.L.; Lawson, K.A.; Wilson, J.P. Patterns and predictors of opioid use among migraine patients at emergency departments: A retrospective database analysis. Cephalalgia 2020, 40, 1489–1501. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Alter, H.J.; Zaia, B. Does the addition of dexamethasone to standard therapy for acute migraine headache decrease the incidence of recurrent headache for patients treated in the emergency department? A meta-analysis and systematic review of the literature. Acad. Emerg. Med. 2008, 15, 1223–1233. [Google Scholar] [CrossRef] [PubMed]
- Friedman, B.W.; Hochberg, M.L.; Esses, D.; Grosberg, B.M.; Rothberg, D.; Bernstein, B.; Bijur, P.E.; Lipton, R.B.; Gallagher, E.J. Recurrence of primary headache disorders after emergency department discharge: Frequency and predictors of poor pain and functional outcomes. Ann. Emerg. Med. 2008, 52, 696–704. [Google Scholar] [CrossRef]
- Silberstein, S.D.; McCrory, D.C. Butalbital in the treatment of headache: History, pharmacology, and efficacy. Headache 2001, 41, 953–967. [Google Scholar] [CrossRef]
- Prabhakar, A.M.; Gottumukkala, R.V.; Hemingway, J.; Hughes, D.R.; Patel, S.S.; Duszak, R., Jr. Increasing utilization of emergency department neuroimaging in Medicare beneficiaries from 1994 to 2015. Am. J. Emerg. Med. 2018, 36, 680–683. [Google Scholar] [CrossRef] [PubMed]
- Kocher, K.E.; Meurer, W.J.; Fazel, R.; Scott, P.A.; Krumholz, H.M.; Nallamothu, B.K. National trends in use of computed tomography in the emergency department. Ann. Emerg. Med. 2011, 58, 452–462.e453. [Google Scholar] [CrossRef]
- Levin, D.C.; Rao, V.M.; Parker, L.; Frangos, A.J. Continued growth in emergency department imaging is bucking the overall trends. J. Am. Coll Radiol. 2014, 11, 1044–1047. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, J.N.; Camargo, C.A., Jr.; Pelletier, A.J.; Edlow, J.A. Headache in United States emergency departments: Demographics, work-up and frequency of pathological diagnoses. Cephalalgia 2006, 26, 684–690. [Google Scholar] [CrossRef]
- Gilbert, J.W.; Johnson, K.M.; Larkin, G.L.; Moore, C.L. Atraumatic headache in US emergency departments: Recent trends in CT/MRI utilisation and factors associated with severe intracranial pathology. Emerg. Med. J. 2012, 29, 576–581. [Google Scholar] [CrossRef]
- Sahai-Srivastava, S.; Desai, P.; Zheng, L. Analysis of headache management in a busy emergency room in the United States. Headache 2008, 48, 931–938. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.X.; Silberstein, S.D.; Young, W.B.; Hopkins, M.; Lopez, B.L.; Samsa, G.P. Less is not more: Underutilization of headache medications in a university hospital emergency department. Headache 2007, 47, 1125–1133. [Google Scholar] [CrossRef] [PubMed]
- Friedman, D.; Feldon, S.; Holloway, R.; Fisher, S. Utilization, diagnosis, treatment and cost of migraine treatment in the emergency department. Headache 2009, 49, 1163–1173. [Google Scholar] [CrossRef]
- Ducharme, J.; Beveridge, R.C.; Lee, J.S.; Beaulieu, S. Emergency management of migraine: Is the headache really over? Acad. Emerg. Med. 1998, 5, 899–905. [Google Scholar] [CrossRef] [PubMed]
| Weighted Visits | All Headaches | Migraine | NOS Headaches | |
|---|---|---|---|---|
| 10.2 Million (100.0%) | 3.4 Million (32.9%) | 6.6 Million (63.9%) | ||
| Characteristics | Weighted % | Weighted % | Weighted % | SMD a |
| Age | 0.32 | |||
| 18–34 | 39.4 | 40.9 | 38.4 | |
| 35–49 | 31.3 | 37.2 | 28.1 | |
| 50–64 | 20.3 | 16.6 | 22.4 | |
| ≥65 | 9.0 | 5.3 | 11.1 | |
| Sex | 0.33 | |||
| Female | 72.9 | 82.0 | 68.0 | |
| Male | 27.1 | 18.0 | 32.0 | |
| Race | 0.41 | |||
| White | 70.3 | 82.2 | 64.7 | |
| Non-White | 29.7 | 17.8 | 35.3 | |
| No. of chronic conditions | 0.08 | |||
| 0 | 46.3 | 49.5 | 43.8 | |
| 1 | 26.3 | 24.6 | 27.0 | |
| ≥2 | 26.1 | 23.7 | 28.3 | |
| Cardiovascular diseases b | 32.2 | 25.5 | 36.0 | 0.16 |
| Depression | 13.5 | 17.5 | 12.1 | 0.16 |
| Pain scale | 0.37 | |||
| None (0) | 5.0 | 3.0 * | 6.1 | |
| Mild (1–3) | 4.9 | 2.7 * | 6.2 | |
| Moderate (4–6) | 13.7 | 9.6 | 15.2 | |
| Severe (7–10) | 53.0 | 65.0 | 47.3 | |
| Payment source | 0.37 | |||
| Commercial | 31.3 | 35.7 | 29.2 | |
| Medicare | 16.3 | 13.7 | 17.2 | |
| Medicaid | 29.5 | 30.6 | 29.4 | |
| Others | 10.2 | 7.5 | 11.1 | |
| No. of medications administered in ED | 0.50 | |||
| 0 | 21.3 | 12.3 | 26.4 | |
| 1 | 10.5 | 5.2 | 13.3 | |
| 2 | 14.8 | 14.9 | 14.2 | |
| ≥3 | 53.5 | 67.6 | 46.1 | |
| No. of medications prescribed at discharge | 0.16 | |||
| 0 | 54.1 | 60.7 | 50.4 | |
| 1 | 21.1 | 17.2 | 22.7 | |
| 2 | 15.3 | 15.4 | 15.6 | |
| ≥3 | 9.5 | 6.6 | 11.3 | |
| Provider type c | ||||
| ED physician | 85.7 | 86.6 | 85.5 | 0.02 |
| Consulting physician | 5.6 | 6.7 | 5.0 | 0.00 |
| ED resident/intern | 9.3 | 9.4 | 9.5 | 0.07 |
| Nurse practitioner | 10.3 | 8.9 | 10.9 | 0.00 |
| Physician assistant | 14.9 | 14.0 | 15.4 | 0.07 |
| Geographic regions | 0.09 | |||
| South | 38.3 | 33.7 | 40.2 | |
| Northeast | 14.4 | 14.5 | 14.3 | |
| Midwest | 24.1 | 27.7 | 22.4 | |
| West | 23.3 | 24.1 | 23.1 | |
| Metropolitan area | 86.2 | 81.2 | 88.5 | 0.23 |
| Medication a | 2007–2010 (%) | 2011–2014 (%) | 2015–2018 (%) | Ptrend b |
|---|---|---|---|---|
| Opioids | 54.1 | 42.4 | 28.3 | <0.001 |
| Codeine | 1.0 | 0.8 * | 3.6 | <0.001 |
| Hydrocodone | 16.0 | 12.4 | 6.6 | <0.001 |
| Hydromorphone | 17.3 | 14.9 | 8.8 | <0.001 |
| Meperidine | 6.6 | 2.2 | 0.9 * | <0.001 |
| Morphine | 9.3 | 9.8 | 5.1 | <0.001 |
| Nalbuphine | 4.2 | 1.1 | 1.2 * | <0.001 |
| Oxycodone | 6.7 | 7.1 | 3.0 | <0.001 |
| Butalbital | 5.1 | 6.5 | 6.4 | 0.22 |
| Ergot alkaloids/Triptans | 5.2 | 5.3 | 4.7 | 0.88 |
| Sumatriptan | 4.3 | 4.8 | 3.8 | 0.52 |
| Acetaminophen/NSAIDs | 37.2 | 45.7 | 52.4 | <0.001 |
| Acetaminophen | 6.7 | 12.2 | 12.2 | <0.001 |
| Ibuprofen | 9.2 | 10.3 | 10.3 | 0.68 |
| Ketorolac | 25.5 | 36.9 | 36.9 | <0.001 |
| Naproxen | 1.8 | 2.4 | 2.3 | 0.51 |
| Antiemetics | 59.3 | 57.7 | 59.2 | 0.88 |
| Dopamine receptor antagonists | 27.5 | 28.8 | 38.0 | <0.001 |
| Metoclopramide | 13.9 | 19.8 | 25.2 | <0.001 |
| Prochlorperazine | 13.4 | 7.6 | 12.2 | <0.001 |
| Promethazine | 25.0 | 15.4 | 11.8 | <0.001 |
| 5-HT3 antagonists | 14.0 | 24.1 | 18.6 | <0.001 |
| Ondansetron | 14.0 | 24.1 | 18.6 | <0.001 |
| Diphenhydramine | 16.5 | 24.0 | 35.8 | <0.001 |
| Corticosteroids | 2.7 | 3.6 | 6.2 | <0.001 |
| Dexamethasone | 0.7 * | 1.6 | 3.5 | <0.001 |
| Methylprednisolone | 1.4 | 1.3 | 1.8 * | 0.60 |
| Most Common Therapies | 2007–2010 (%) | 2011–2014 (%) | 2015–2018 (%) |
|---|---|---|---|
| Acetaminophen/NSAIDs | 8.9 | 8.8 | 10.6 |
| Acetaminophen/NSAIDs + Antiemetic | 7.4 | 8.8 | 7.6 |
| Acetaminophen/NSAIDs + Antiemetic + Diphenhydramine | 3.9 | 7.0 | 15.7 |
| Antiemetic | 4.8 | 4.2 | 3.2 |
| Antiemetic + Diphenhydramine | 4.9 | 4.9 | 7.4 |
| Opioid | 8.8 | 5.0 | 1.9 |
| Opioid + Acetaminophen/NSAIDs + Antiemetic | 5.1 | 4.5 | 3.8 |
| Opioid + Antiemetic | 21.0 | 13.7 | 6.6 |
| Opioid + Antiemetic + Diphenhydramine | 2.9 | 3.4 | 2.1 |
| Medications | 2007–2010 | 2015–2018 | ||
|---|---|---|---|---|
| Administered in ED (%) | Prescribed at Discharge (%) | Administered in ED (%) | Prescribed at Discharge (%) | |
| Opioids | 44.0 | 23.2 | 21.7 | 11.5 |
| Butalbital | 1.1 * | 4.0 | 2.0 | 5.3 |
| Acetaminophen/NSAIDs | 30.1 | 11.9 | 47.9 | 12.8 |
| Ergot alkaloids/Triptans | 3.1 * | 3.6 * | 2.8 | 2.4 |
| Antiemetics | 55.5 | 11.6 | 56.2 | 12.2 |
| Diphenhydramine | 15.7 | 1.2 | 35.0 | 2.2 |
| Corticosteroids | 2.3 | 0.3 * | 5.0 | 1.5 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, S.; Orlova, Y.; Lipe, A.; Boren, M.; Hincapie-Castillo, J.M.; Park, H.; Chang, C.-Y.; Wilson, D.L.; Adkins, L.; Lo-Ciganic, W.-H. Trends in the Management of Headache Disorders in US Emergency Departments: Analysis of 2007–2018 National Hospital Ambulatory Medical Care Survey Data. J. Clin. Med. 2022, 11, 1401. https://doi.org/10.3390/jcm11051401
Yang S, Orlova Y, Lipe A, Boren M, Hincapie-Castillo JM, Park H, Chang C-Y, Wilson DL, Adkins L, Lo-Ciganic W-H. Trends in the Management of Headache Disorders in US Emergency Departments: Analysis of 2007–2018 National Hospital Ambulatory Medical Care Survey Data. Journal of Clinical Medicine. 2022; 11(5):1401. https://doi.org/10.3390/jcm11051401
Chicago/Turabian StyleYang, Seonkyeong, Yulia Orlova, Abigale Lipe, Macy Boren, Juan M. Hincapie-Castillo, Haesuk Park, Ching-Yuan Chang, Debbie L. Wilson, Lauren Adkins, and Wei-Hsuan Lo-Ciganic. 2022. "Trends in the Management of Headache Disorders in US Emergency Departments: Analysis of 2007–2018 National Hospital Ambulatory Medical Care Survey Data" Journal of Clinical Medicine 11, no. 5: 1401. https://doi.org/10.3390/jcm11051401
APA StyleYang, S., Orlova, Y., Lipe, A., Boren, M., Hincapie-Castillo, J. M., Park, H., Chang, C.-Y., Wilson, D. L., Adkins, L., & Lo-Ciganic, W.-H. (2022). Trends in the Management of Headache Disorders in US Emergency Departments: Analysis of 2007–2018 National Hospital Ambulatory Medical Care Survey Data. Journal of Clinical Medicine, 11(5), 1401. https://doi.org/10.3390/jcm11051401







