Human Amniotic Membrane for the Treatment of Cryptoglandular Anal Fistulas
Abstract
:1. Introduction
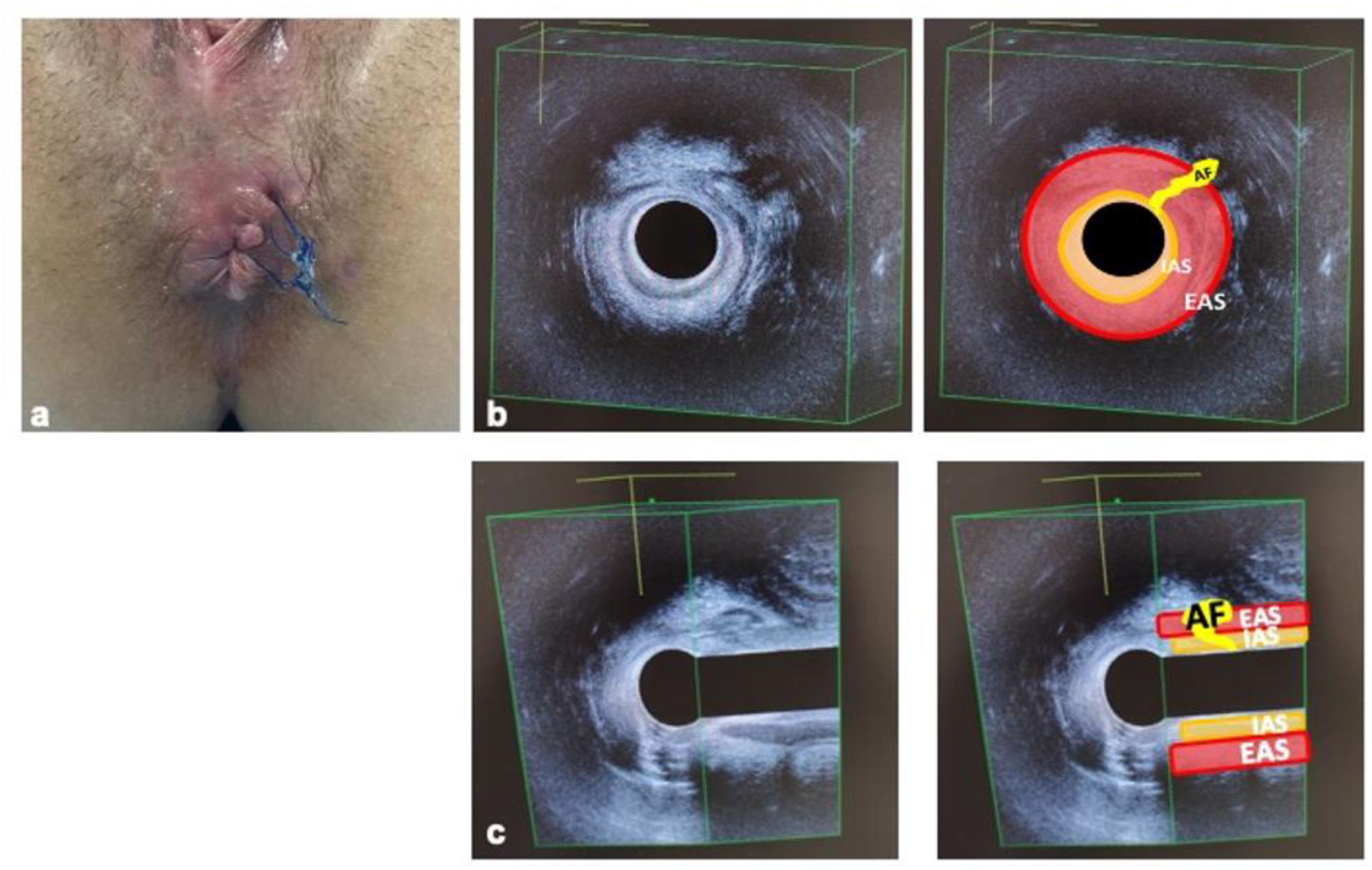
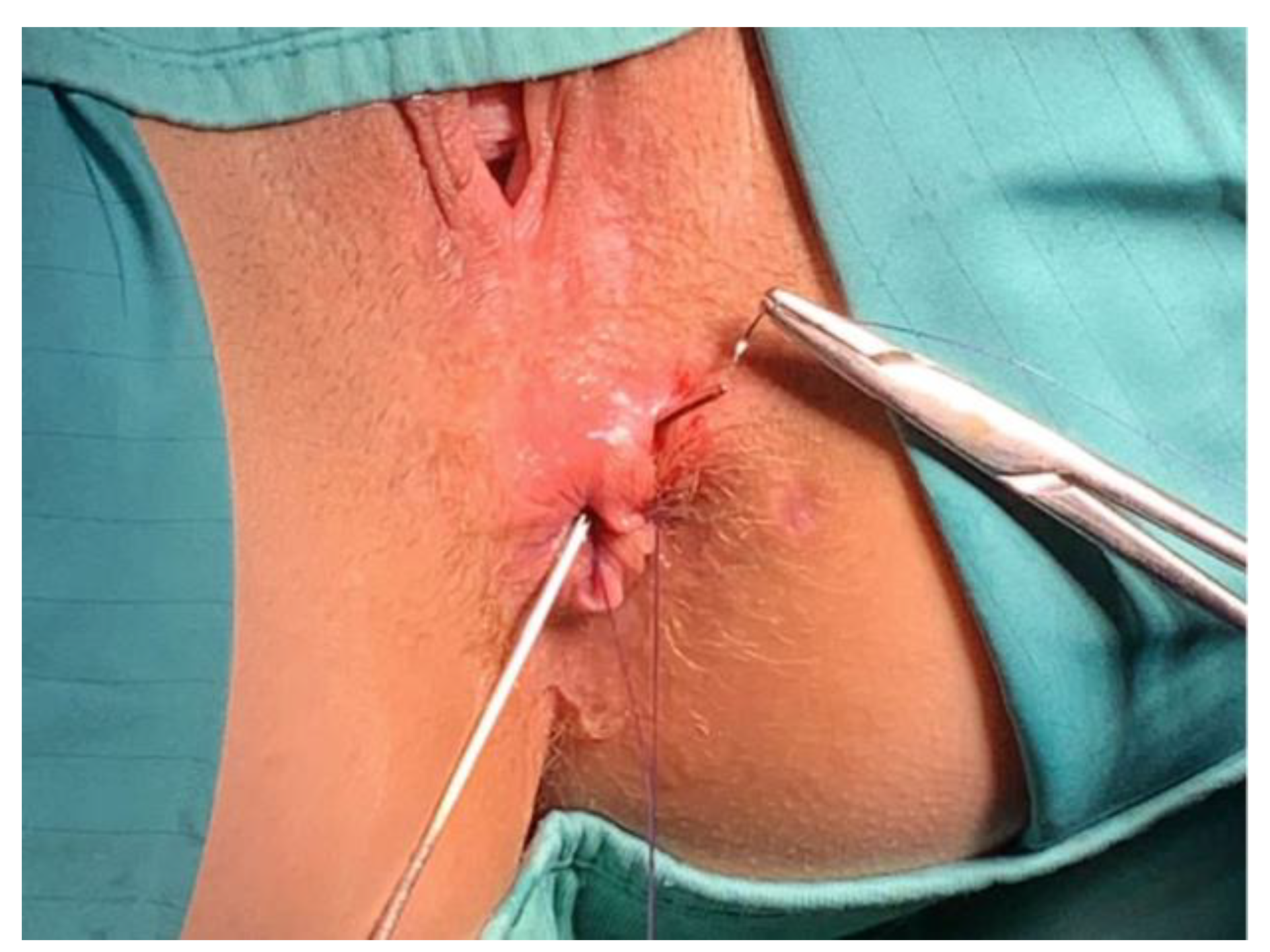
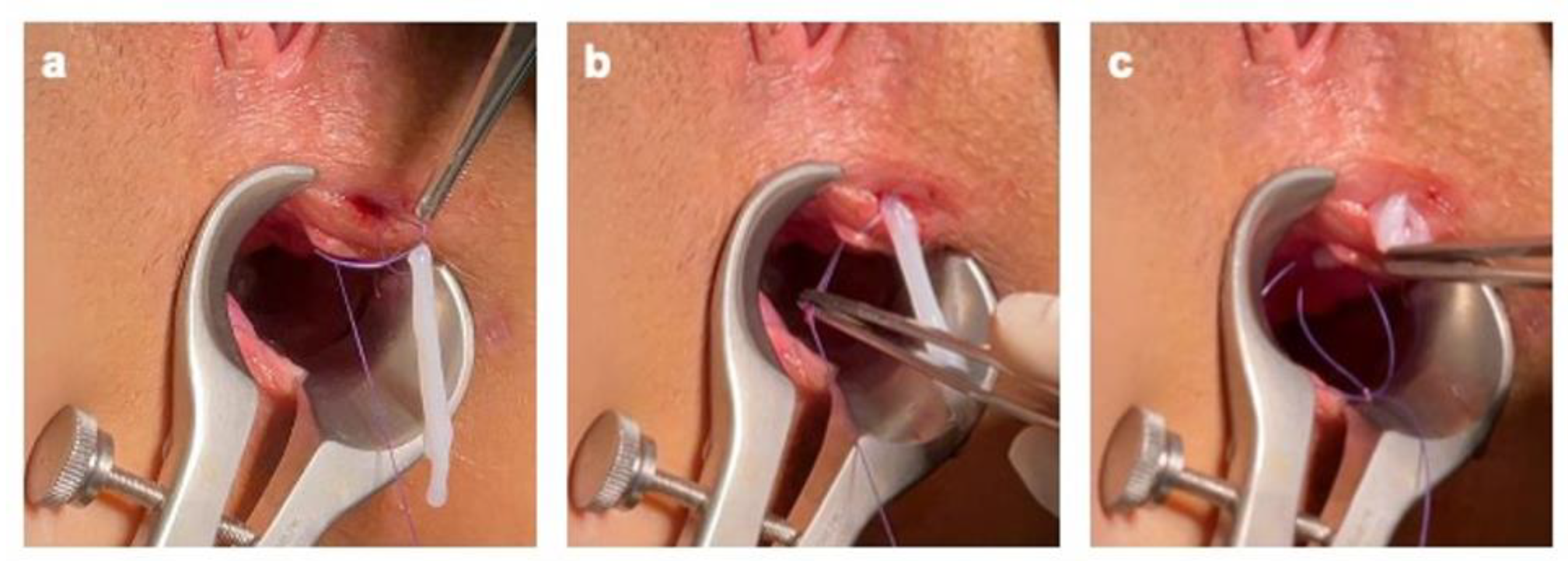
2. Materials and Methods
Surgical Procedure
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cadeddu, F.; Salis, F.; Lisi, G.; Ciangola, I.; Milito, G. Complex anal fistula remains a challenge for colorectal surgeon. Int. J. Colorectal Dis. 2015, 30, 595–603. [Google Scholar] [CrossRef]
- Parés, D. Pathogenesis and treatment of fistula in ano. Br. J. Surg. 2011, 98, 2–3. [Google Scholar] [CrossRef]
- van Koperen, P.J.; ten Kate, F.J.; Bemelman, W.A.; Slors, J.F. Histological identification of epithelium in perianal fistulae: A prospective study. Colorectal Dis. 2010, 12, 891–895. [Google Scholar] [CrossRef]
- Lunniss, P.J.; Sheffield, J.P.; Talbot, I.C.; Thomson, J.P.; Phillips, R.K. Persistence of idiopathic anal fistula may be related to epithelialization. Br. J. Surg. 1995, 82, 32–33. [Google Scholar] [CrossRef]
- Mitalas, L.E.; van Onkelen, R.S.; Monkhorst, K.; Zimmerman, D.D.; Gosselink, M.P.; Schouten, W.R. Identification of epithelialization in high transsphincteric fistulas. Tech. Coloproctol. 2012, 16, 113–117. [Google Scholar] [CrossRef] [Green Version]
- Toyonaga, T.; Matsushima, M.; Tanaka, Y.; Shimojima, Y.; Matsumura, N.; Kannyama, H.; Nozawa, M.; Hatakeyama, T.; Suzuki, K.; Yanagita, K.; et al. Microbiological analysis and endoanal ultrasonography for diagnosis of anal fistula in acute anorectal sepsis. Int. J. Colorectal Dis. 2007, 22, 209–213. [Google Scholar] [CrossRef]
- Tozer, P.J.; Rayment, N.; Hart, A.L.; Daulatzai, N.; Murugananthan, A.U.; Whelan, K.; Phillips, R.K.S. What role do bacteria play in persisting fistula formation in idiopathic and Crohn’s anal fistula? Colorectal Dis. 2015, 17, 235–241. [Google Scholar] [CrossRef]
- Ratto, C.; Litta, F.; Lucchetti, D.; Parello, A.; Boninsegna, A.; Arena, V.; Donisi, L.; Calapà, F.; Sgambato, A. Immunopathological characterization of cryptoglandular anal fistula: A pilot study investigating its pathogenesis. Colorectal Dis. 2016, 18, O436–O444. [Google Scholar] [CrossRef]
- Silini, A.R.; Magatti, M.; Cargnoni, A.; Parolini, O. Is Immune Modulation the Mechanism Underlying the Beneficial Effects of Amniotic Cells and Their Derivatives in Regenerative Medicine? Cell Transplant. 2017, 26, 531–539. [Google Scholar] [CrossRef] [Green Version]
- Silini, A.R.; Cargnoni, A.; Magatti, M.; Pianta, S.; Parolini, O. The Long Path of Human Placenta, and Its Derivatives, in Regenerative Medicine. Front. Bioeng. Biotechnol. 2015, 3, 162. [Google Scholar] [CrossRef]
- Davis, S. Skin Transplantation: With a Review of 550 Cases at the Johns Hopkins Hospital. Johns Hopkins Hosp. Rep. Ba/t 1910, 15, 307–396. [Google Scholar]
- Liu, J.; Sheha, H.; Fu, Y.; Liang, L.; Tseng, S.C. Update on amniotic membrane transplantation. Expert Rev. Ophthalmol. 2010, 5, 645–661. [Google Scholar] [CrossRef] [Green Version]
- Riau, A.K.; Beuerman, R.W.; Lim, L.S.; Mehta, J.S. Preservation, sterilization and de-epithelialization of human amniotic membrane for use in ocular surface reconstruction. Biomaterials 2010, 31, 216–225. [Google Scholar] [CrossRef]
- Dua, H.S.; Gomes, J.A.; King, A.J.; Maharajan, V.S. The amniotic membrane in ophthalmology. Surv. Ophthalmol. 2004, 49, 51–77. [Google Scholar] [CrossRef]
- Kesting, M.R.; Wolff, K.D.; Nobis, C.P.; Rohleder, N. H Amniotic membrane in oral and maxillofacial surgery. Oral Maxillofac. Surg. 2014, 18, 153–164. [Google Scholar] [CrossRef]
- Lo, V.; Pope, E. Amniotic membrane use in dermatology. Int. J. Dermatol. 2009, 48, 935–940. [Google Scholar] [CrossRef]
- European Directorate for the Quality of Medicines & HealthCare of the Council of Europe. Guide to The Quality and Safety of Tissues and Cells for Human Application, 4th ed.; European Directorate for the Quality of Medicines & HealthCare of the Council of Europe: Strasbourg, France, 2019; Available online: https://www.edqm.eu (accessed on 24 February 2022).
- Bleier, J.I.; Moloo, H. Current management of cryptoglandular fistula-in-ano. World J. Gastroenterol. 2011, 17, 3286–3291. [Google Scholar] [CrossRef]
- Parks, A.G. Pathogenesis and treatment of fistuila-in-ano. Br. Med. J. 1961, 1, 463–469. [Google Scholar] [CrossRef] [Green Version]
- van Onkelen, R.S.; Mitalas, L.E.; Gosselink, M.P.; van Belkum, A.; Laman, J.D.; Schouten, W.R. Assessment of microbiota and peptidoglycan in perianal fistulas. Diagn. Microbiol. Infect. Dis. 2013, 75, 50–54. [Google Scholar] [CrossRef]
- Tan, J.L.; Chan, S.T.; Wallace, E.M.; Lim, R. Human amnion epithelial cells mediate lung repair by directly modulating macrophage recruitment and polarization. Cell Transplant. 2014, 23, 319–328. [Google Scholar] [CrossRef] [Green Version]
- Magatti, M.; Vertua, E.; De Munari, S.; Caro, M.; Caruso, M.; Silini, A.; Delgado, M.; Parolini, O. Human amnion favours tissue repair by inducing the M1-to-M2 switch and enhancing M2 macrophage features. J. Tissue Eng. Regen. Med. 2017, 11, 2895–2911. [Google Scholar] [CrossRef] [PubMed]
- Taghiabadi, E.; Nasri, S.; Shafieyan, S.; Jalili Firoozinezhad, S.; Aghdami, N. Fabrication and characterization of spongy denuded amniotic membrane based scaffold for tissue engineering. Cell J. 2015, 16, 476–487. [Google Scholar] [CrossRef]
- Becker, M.; Maring, J.A.; Schneider, M.; Herrera Martin, A.X.; Seifert, M.; Klein, O.; Braun, T.; Falk, V.; Stamm, C. Towards a Novel Patch Material for Cardiac Applications: Tissue-Specific Extracellular Matrix Introduces Essential Key Features to Decellularized Amniotic Membrane. Int. J. Mol. Sci. 2018, 19, 1032. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murphy, S.V.; Skardal, A.; Nelson, R.A., Jr.; Sunnon, K.; Reid, T.; Clouse, C.; Kock, N.D.; Jackson, J.; Soker, S.; Atala, A. Amnion membrane hydrogel and amnion membrane powder accelerate wound healing in a full thickness porcine skin wound model. Stem Cells Transl. Med. 2020, 9, 80–92. [Google Scholar] [CrossRef] [Green Version]
- Shimmura, S.; Shimazaki, J.; Ohashi, Y.; Tsubota, K. Antiinflammatory effects of amniotic membrane transplantation in ocular surface disorders. Cornea 2001, 20, 408–413. [Google Scholar] [CrossRef] [PubMed]
- Kogan, S.; Sood, A.; Granick, M.S. Amniotic Membrane Adjuncts and Clinical Applications in Wound Healing: A Review of the Literature. Wounds 2018, 30, 168–173. [Google Scholar]
- Rafati, M.; Hosseini, S.V.; Moradian, F.; Zamani, M.; Khazraei, H.; Mokhtari, M. Human Amniotic Membrane Effect on Perianal Fistula Healing in Rabbits: An Experimental Study. Iran. J. Med. Sci. 2018, 43, 473–478. [Google Scholar]
- Roshanravan, R.; Ghahramani, L.; Hosseinzadeh, M.; Mohammadipour, M.; Moslemi, S.; Rezaianzadeh, A.; Safarpour, A.R.; Rahimikazerooni, S.; Hosseini, S.V. A new method to repair recto-vaginal fistula: Use of human amniotic membrane in an animal model. Adv. Biomed. Res. 2014, 3, 114. [Google Scholar] [CrossRef]
- Uludag, M.; Citgez, B.; Ozkaya, O.; Yetkin, G.; Ozcan, O.; Polat, N.; Isgor, A. Effects of amniotic membrane on the healing of primary colonic anastomoses in the cecal ligation and puncture model of secondary peritonitis in rats. Int. J. Colorectal Dis. 2009, 24, 559–567. [Google Scholar] [CrossRef]
- Razzaghi, M.; Rahavian, A.; Fallah Karkan, M.; Allameh, F.; Ghiasy, S.; Javanmard, B. Use of human amniotic membrane repair of anterior urethral defect: First clinical report. Int. J. Urol. 2020, 27, 605–609. [Google Scholar] [CrossRef]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ratto, C.; Parolini, O.; Marra, A.A.; Orticelli, V.; Parello, A.; Campennì, P.; De Simone, V.; Trojan, D.; Litta, F. Human Amniotic Membrane for the Treatment of Cryptoglandular Anal Fistulas. J. Clin. Med. 2022, 11, 1350. https://doi.org/10.3390/jcm11051350
Ratto C, Parolini O, Marra AA, Orticelli V, Parello A, Campennì P, De Simone V, Trojan D, Litta F. Human Amniotic Membrane for the Treatment of Cryptoglandular Anal Fistulas. Journal of Clinical Medicine. 2022; 11(5):1350. https://doi.org/10.3390/jcm11051350
Chicago/Turabian StyleRatto, Carlo, Ornella Parolini, Angelo Alessandro Marra, Valentina Orticelli, Angelo Parello, Paola Campennì, Veronica De Simone, Diletta Trojan, and Francesco Litta. 2022. "Human Amniotic Membrane for the Treatment of Cryptoglandular Anal Fistulas" Journal of Clinical Medicine 11, no. 5: 1350. https://doi.org/10.3390/jcm11051350
APA StyleRatto, C., Parolini, O., Marra, A. A., Orticelli, V., Parello, A., Campennì, P., De Simone, V., Trojan, D., & Litta, F. (2022). Human Amniotic Membrane for the Treatment of Cryptoglandular Anal Fistulas. Journal of Clinical Medicine, 11(5), 1350. https://doi.org/10.3390/jcm11051350






