Controversies in Choledochal Malformation in Children: An International Survey among Pediatric Hepatobiliary Surgeons and Gastroenterologists
Abstract
:1. Introduction
2. Materials and Methods
Statistics
3. Results
3.1. Organization of Care
3.2. Diagnostics
3.3. Indications for Surgery
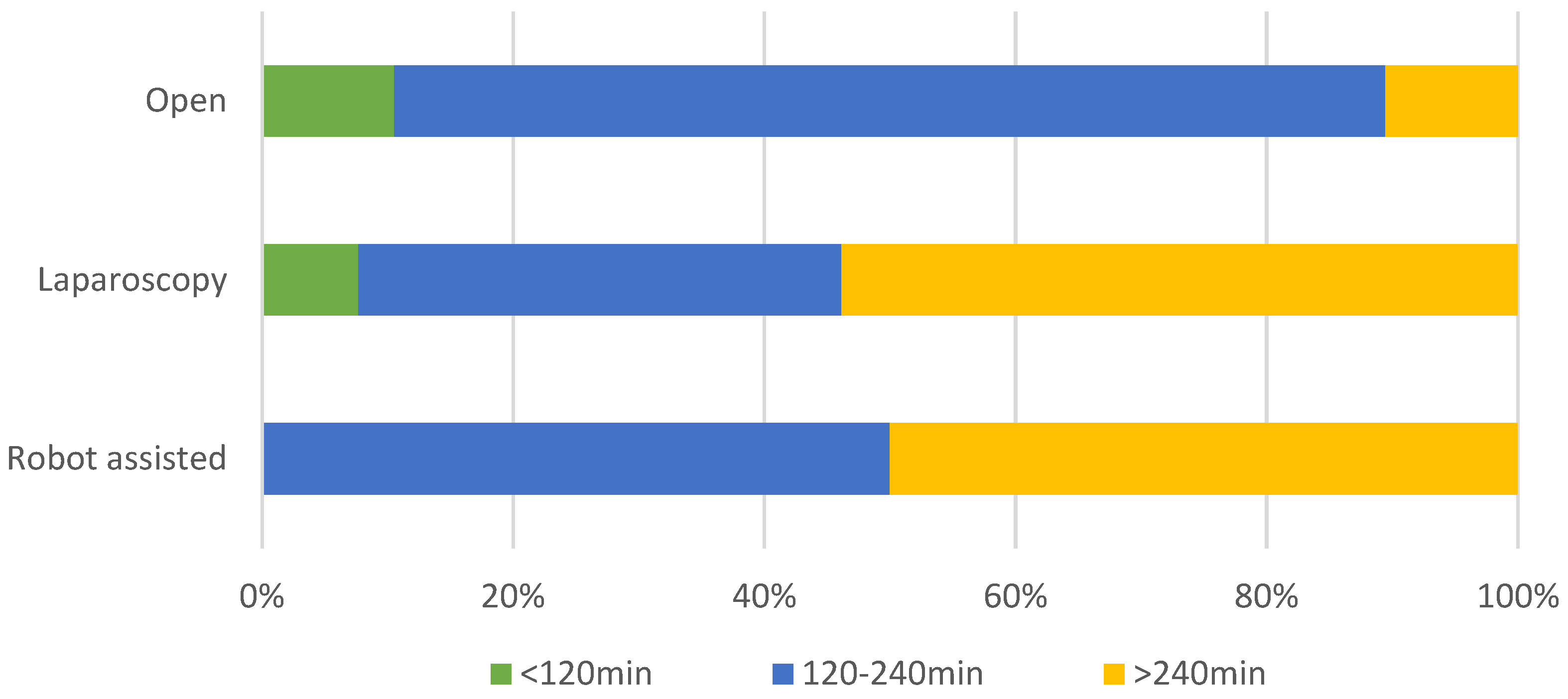
3.4. Medical and Surgical Treatment
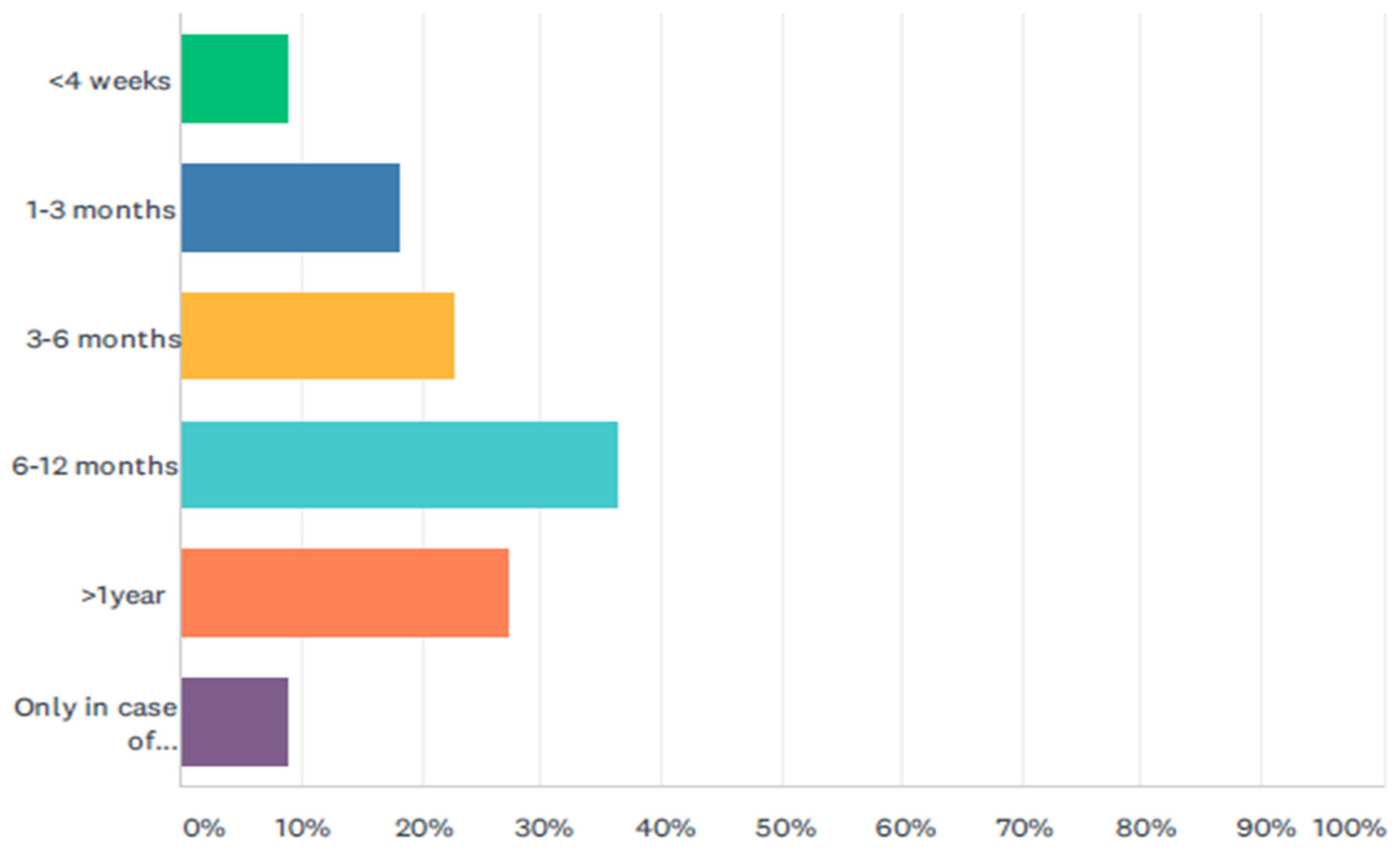
3.5. Postoperative Follow-Up and Transition of Care
3.6. Importance of the Several Items
4. Discussion
4.1. Organization of Care
4.2. Diagnostics
4.3. Medical and Surgical Treatment
4.4. Follow-Up
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Todani, T.; Watanabe, Y.; Toki, A.; Morotomi, Y. Classification of congenital biliary cystic disease: Special reference to type Ic and IVA cysts with primary ductal stricture. J. Hepato-Biliary-Pancreat. Surg. 2003, 10, 340–344. [Google Scholar] [CrossRef] [PubMed]
- Kronfli, R.; Davenport, M. Insights into the pathophysiology and classification of type 4 choledochal malfor-mation. J. Pediatr. Surg. 2020, 55, 2642–2646. [Google Scholar] [CrossRef] [PubMed]
- Ten Hove, A.; De Meijer, V.E.; Hulscher, J.B.F.; De Kleine, R.H.J. Meta-analysis of risk of developing malignancy in congenital choledochal malformation. Br. J. Surg. 2018, 105, 482–490. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wirth, T.C.; Kuebler, J.F.; Petersen, C.; Ure, B.M.; Madadi-Sanjani, O. Choledochal Cyst and Malignancy: A Plea for Lifelong Follow-Up. Eur. J. Pediatr. Surg. 2017, 29, 143–149. [Google Scholar] [CrossRef]
- Durkin, N.; Davenport, M. Centralization of Pediatric Surgical Procedures in the United Kingdom. Eur. J. Pediatr. Surg. 2017, 27, 416–421. [Google Scholar] [CrossRef]
- Wen, Z.; Liang, H.; Liang, J.; Liang, Q.; Xia, H. Evaluation of the learning curve of laparoscopic choledochal cyst ex-cision and Roux-en Y hepaticojejunostomy in children: CUSUM analysis of a single surgeon’s experience. Surg. Endosc. 2017, 31, 778–787. [Google Scholar] [CrossRef] [Green Version]
- Davenport, M.; Goyet, J.D.V.D.; Stringer, M.; Mieli-Vergani, G.; Kelly, D.; McClean, P.; Spitz, L. Seamless management of biliary atresia in England and Wales (1999–2002). Lancet 2004, 363, 1354–1357. [Google Scholar] [CrossRef]
- Lampela, H.; Ritvanen, A.; Kosola, S.; Koivusalo, A.; Rintala, R.; Jalanko, H.; Pakarinen, M. National centralization of biliary atresia care to an assigned multidisciplinary team provides high-quality outcomes. Scand. J. Gastroenterol. 2012, 47, 99–107. [Google Scholar] [CrossRef]
- Madadi-Sanjani, O.; Fortmann, D.; Rolle, U.; Rodeck, B.; Sturm, E.; Pfister, E.-D.; Kuebler, J.F.; Baumann, U.; Schmittenbecher, P.; Petersen, C. Centralization of Biliary Atresia: Has Germany Learned Its Lessons? Eur. J. Pediatr. Surg. 2021. [Google Scholar] [CrossRef]
- Casimir, G. Why Children’s Hospitals are Unique and so Essential. Front. Pediatr. 2019, 7, 305. [Google Scholar] [CrossRef] [Green Version]
- De Groot, S.; van der Linden, N.; Franken, M.G.; Blommestein, H.M.; Leeneman, B.; van Rooijen, E.; van der Hoeven, J.J.M.; Wouters, M.W.; Westgeest, H.M.; Uyl-de Groot, C.A. Balancing the Optimal and the Feasible: A Practical Guide for Setting Up Patient Registries for the Collection of Real-World Data for Health Care Decision Making Based on Dutch Experiences. Value Health 2017, 20, 627–636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saito, T.; Terui, K.; Mitsunaga, T.; Nakata, M.; Yoshida, H. Significance of imaging modalities for preoperative evaluation of the pancreaticobiliary system in surgery for pediatric choledochal cyst. J. Hepato-Biliary-Pancreat. Sci. 2016, 23, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, K.M.; Pitt, H.A.; Zyromski, N.J.; Chauhan, A.; Sherman, S.; Moffatt, D.; Lehman, G.A.; Lillemoe, K.D.; Rescorla, F.J.; West, K.W.; et al. Choledochoceles: Are they choledochal cysts? Ann. Surg. 2010, 252, 683–690. [Google Scholar] [CrossRef] [PubMed]
- Hukkinen, M.; Björnland, K.; Gatzinsky, V.; Iber, T.; Johansen, L.S.; Qvist, N.; Stenström, P.; Svensson, J.F.; Pakarinen, M.P. Management strategies and treatment results of pediatric choledochal malformations in the Nordic countries. HPB 2020, 22, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Zheng, W.; Xia, Z.; Long, L.; Lishuang, M.; Pu, Y.; Wenjuan, Z.; Xiaofan, L. Laparoscopic Excision Versus Open Excision for the Treatment of Choledochal Cysts: A Systematic Review and Meta-Analysis. Int. Surg. 2015, 100, 115–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, R.; Zhao, N.; Zhao, K.; Su, Z.; Zhang, Y.; Diao, M.; Li, L. Comparison of efficacy and safety of laparoscopic excision and open operation in children with choledochal cysts: A systematic review and update meta-analysis. PLoS ONE 2020, 15, e0239857. [Google Scholar] [CrossRef]
- Xie, X.; Li, K.; Wang, J.; Wang, C.; Xiang, B. Comparison of pediatric choledochal cyst excisions with open procedures, laparoscopic procedures and robot-assisted procedures: A retrospective study. Surg. Endosc. 2020, 34, 3223–3231. [Google Scholar] [CrossRef]
- van den Eijnden, M.H.A.; de Kleine, R.H.J.; de Blaauw, I.; Peeters, P.G.J.M.; Koot, B.P.G.; Oomen, M.W.N.; Sloots, C.E.J.; van Gemert, W.G.; van der Zee, D.C.; van Heurn, L.W.E.; et al. Choledochal Malformation in Children: Lessons Learned from a Dutch National Study. World J. Surg. 2017, 41, 2631–2637. [Google Scholar] [CrossRef] [Green Version]
- Alizai, N.K.; Dawrant, M.J.; Najmaldin, A.S. Robot-assisted resection of choledochal cysts and hepaticojejunostomy in children. Pediatr. Surg. Int. 2014, 30, 291–294. [Google Scholar] [CrossRef]
- Narayanan, S.K.; Chen, Y.; Narasimhan, K.L.; Cohen, R.C. Hepaticoduodenostomy versus hepaticojejunostomy after resction of choledochal cyst: A systematic review and meta-analysis. J. Pediatr. Surg. 2013, 48, 2336–2342. [Google Scholar] [CrossRef]
- Mizuguchi, Y.; Nakamura, Y.; Uchida, E. Subsequent biliary cancer originating from remnant intrapancreatic bile ducts after cyst excision: A literature review. Surg. Today 2016, 47, 660–667. [Google Scholar] [CrossRef] [PubMed]
- La Pergola, E.; Zen, Y.; Davenport, M. Congenital choledochal malformation: Search for a marker of epithelial in-stability. J. Pediatr. Surg. 2016, 51, 1445–1449. [Google Scholar] [CrossRef] [PubMed]
- Ishibashi, H.; Shimada, M.; Kamisawa, T.; Fujii, H.; Hamada, Y.; Kubota, M.; Urushihara, N.; Endo, I.; Nio, M.; Taguchi, T.; et al. Japanese clinical practice guidelines for congenital biliary dilatation. J. Hepato-Biliary-Pancreat. Sci. 2017, 24, 1–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Median (Range) | |
|---|---|
| Dedicated team | 10.0 (9.4–10.0) |
| Imaging techniques | 10.0 (7.5–10.0) |
| Centralization | 9.9 (3.3–10.0) |
| Life-long follow-up | 9.7 (1.2–10.0) |
| Length of Roux loop | 9.5 (2.0–10.0) |
| Nationwide registry | 9.4 (5.0–10.0) |
| Intraoperative cholangiogram | 9.4 (1.0–10.0) |
| Features for diagnosis | 8.5 (2.0–9.9) |
| Postponing surgery i.c.o. pancreatitis | 8.3 (4.5–10.0) |
| Importance of pancreaticobiliary maljunction for diagnosis | 8.3 (6.0–9.9) |
| Placement of a drain postoperative | 8.0 (0.0–9.9) |
| Obtaining a liver biopsy | 8.0 (1.4–9.6) |
| Delay of surgery until first birthday in asymptomatic patients | 7.5 (0.5–10.0) |
| Leave a cuff of proximal bile duct to suture on | 7.2 (1.9–10.0) |
| Running sutures | 4.6 (0.0–9.8) |
| Nasogastric tube | 4.3 (1.0–9.0) |
| Elevated pancreatic enzymes in bile (for diagnosis) | 4.2 (1.0–7.8) |
| Ursodeoxycholic acid postoperative | 4.0 (2.0–9.9) |
| Minimally invasive surgery (when possible) | 3.3 (3.0–10.0) |
| High pressure in main duct (for diagnosis) | 3.2 (1.0–5.0) |
| Postoperative antibiotic prophylaxis | 3.1 (0.1–10.0) |
| Hepaticoduodenostomy as valid option | 1.7 (0.0–10.0) |
| Running sutures for hepaticojejunostomy | 1.5 (0.0–7.7) |
| Avoiding surgery in asymptomatic patients | 0.9 (0.0–3.3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hulscher, J.B.F.; Kuebler, J.F.; Bruggink, J.M.; Davenport, M.; Scholz, S.; Petersen, C.; Madadi-Sanjani, O.; Schukfeh, N. Controversies in Choledochal Malformation in Children: An International Survey among Pediatric Hepatobiliary Surgeons and Gastroenterologists. J. Clin. Med. 2022, 11, 1148. https://doi.org/10.3390/jcm11041148
Hulscher JBF, Kuebler JF, Bruggink JM, Davenport M, Scholz S, Petersen C, Madadi-Sanjani O, Schukfeh N. Controversies in Choledochal Malformation in Children: An International Survey among Pediatric Hepatobiliary Surgeons and Gastroenterologists. Journal of Clinical Medicine. 2022; 11(4):1148. https://doi.org/10.3390/jcm11041148
Chicago/Turabian StyleHulscher, Jan B. F., Joachim F. Kuebler, Janneke M. Bruggink, Mark Davenport, Stefan Scholz, Claus Petersen, Omid Madadi-Sanjani, and Nagoud Schukfeh. 2022. "Controversies in Choledochal Malformation in Children: An International Survey among Pediatric Hepatobiliary Surgeons and Gastroenterologists" Journal of Clinical Medicine 11, no. 4: 1148. https://doi.org/10.3390/jcm11041148
APA StyleHulscher, J. B. F., Kuebler, J. F., Bruggink, J. M., Davenport, M., Scholz, S., Petersen, C., Madadi-Sanjani, O., & Schukfeh, N. (2022). Controversies in Choledochal Malformation in Children: An International Survey among Pediatric Hepatobiliary Surgeons and Gastroenterologists. Journal of Clinical Medicine, 11(4), 1148. https://doi.org/10.3390/jcm11041148






