A Comparison of the Anesthetic Methods for Recurrence Rates of Bladder Cancer after Transurethral Resection of Bladder Tumors Using National Health Insurance Claims Data of South Korea
Abstract
1. Introduction
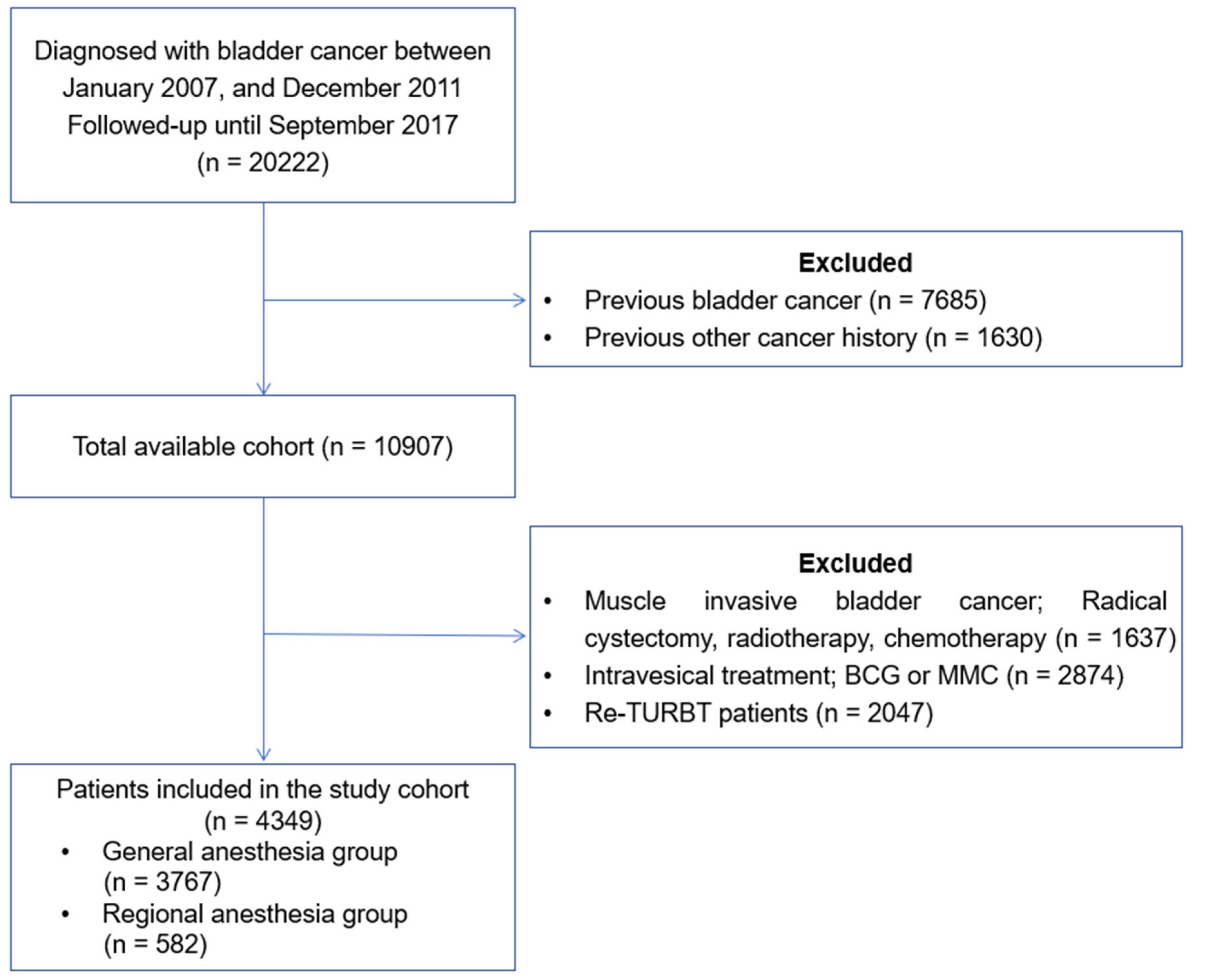
2. Method
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- DeGeorge, K.C.; Holt, H.R.; Hodges, S.C. Bladder Cancer: Diagnosis and Treatment. Am. Fam. Physician 2017, 96, 507–514. [Google Scholar] [PubMed]
- Sylvester, R.J.; van der Meijden, A.P.; Oosterlinck, W.; Witjes, J.A.; Bouffioux, C.; Denis, L.; Newling, D.W.; Kurth, K. Predicting Recurrence and Progression in Individual Patients with Stage Ta T1 Bladder Cancer Using EORTC Risk Tables: A Combined Analysis of 2596 Patients from Seven EORTC Trials. Eur. Urol. 2006, 49, 466–477. [Google Scholar] [CrossRef]
- Babjuk, M.; Oosterlinck, W.; Sylvester, R.; Kaasinen, E.; Böhle, A.; Palou-Redorta, J. EAU Guidelines on Non-Muscle-Invasive Urothelial Carcinoma of the Bladder. Eur. Urol. 2008, 54, 303–314. [Google Scholar] [CrossRef]
- Kim, H.S.; Jeong, C.W.; Kwak, C.; Kim, H.H.; Ku, J.H. Novel nomograms to predict recurrence and progression in primary non-muscle-invasive bladder cancer: Validation of predictive efficacy in comparison with European Organization of Research and Treatment of Cancer scoring system. World J. Urol. 2018, 37, 1867–1877. [Google Scholar] [CrossRef] [PubMed]
- Luján, S.; Santamaría, C.; Pontones, J.; Ruiz-Cerdá, J.; Trassierra, M.; Vera-Donoso, C.; Solsona, E.; Jiménez-Cruz, F. Risk estimation of multiple recurrence and progression of non-muscle invasive bladder carcinoma using new mathematical models. Actas Urol. Esp. 2014, 38, 647–654. [Google Scholar] [CrossRef]
- Choi, W.-J.; Baek, S.; Joo, E.-Y.; Yoon, S.-H.; Kim, E.; Hong, B.; Hwang, J.-H.; Kim, Y.-K. Comparison of the effect of spinal anesthesia and general anesthesia on 5-year tumor recurrence rates after transurethral resection of bladder tumors. Oncotarget 2017, 8, 87667–87674. [Google Scholar] [CrossRef]
- Kurosawa, S.; Kato, M. Anesthetics, immune cells, and immune responses. J. Anesthesia 2008, 22, 263–277. [Google Scholar] [CrossRef]
- Brausi, M.A.; Verrini, G.; De Luca, G.; Viola, M.; Simonini, G.L.; Peracchia, G.; Gavioli, M. The Use of Local Anesthesia with N-DO Injector (Physion) for Transurethral Resection (TUR) of Bladder Tumors and Bladder Mapping: Preliminary Results and Cost-Effectiveness Analysis. Eur. Urol. 2007, 52, 1407–1413. [Google Scholar] [CrossRef]
- Jang, D.; Lim, C.S.; Shin, Y.S.; Ko, Y.K.; Park, S.I.; Song, S.H.; Kim, B.J. A comparison of regional and general anesthesia effects on 5 year survival and cancer recurrence after transurethral resection of the bladder tumor: A retrospective analysis. BMC Anesthesiol. 2015, 16, 16. [Google Scholar] [CrossRef]
- Koumpan, Y.; Jaeger, M.; Mizubuti, G.B.; Tanzola, R.; Jain, K.; Hosier, G.; Hopman, W.; Siemens, D.R. Spinal Anesthesia is Associated with Lower Recurrence Rates after Resection of Nonmuscle Invasive Bladder Cancer. J. Urol. 2018, 199, 940–946. [Google Scholar] [CrossRef] [PubMed]
- Zeegers, M.P.; E Tan, F.; Dorant, E.; Brandt, P.A.V.D. The impact of characteristics of cigarette smoking on urinary tract cancer risk: A meta-analysis of epidemiologic studies. Cancer 2000, 89, 630–639. [Google Scholar] [CrossRef]
- Divrik, R.T.; Şahin, A.; Altok, M.; Ünlü, N.; Zorlu, F. The Frequency of Hydronephrosis at Initial Diagnosis and its Effect on Recurrence and Progression in Patients With Superficial Bladder Cancer. J. Urol. 2007, 178, 802–806. [Google Scholar] [CrossRef] [PubMed]
- Gomez, J.M.F.; Madero, R.; Solsona, E.; Unda, M.; Martinez-Piñeiro, L.; Gonzalez, M.; Portillo, J.A.; Ojea, A.; Pertusa, C.; Rodriguez-Molina, J.; et al. Predicting Nonmuscle Invasive Bladder Cancer Recurrence and Progression in Patients Treated With Bacillus Calmette-Guerin: The CUETO Scoring Model. J. Urol. 2009, 182, 2195–2203. [Google Scholar] [CrossRef] [PubMed]
- Teleka, S.; Jochems, S.H.J.; Häggström, C.; Wood, A.M.; Järvholm, B.; Orho-Melander, M.; Liedberg, F.; Stocks, T. Association between blood pressure and BMI with bladder cancer risk and mortality in 340,000 men in three Swedish cohorts. Cancer Med. 2021, 10, 1431–1438. [Google Scholar] [CrossRef]
- Kok, V.C.; Zhang, H.-W.; Lin, C.-T.; Huang, S.-C.; Wu, M.-F. Positive association between hypertension and urinary bladder cancer: Epidemiologic evidence involving 79,236 propensity score-matched individuals. Upsala J. Med. Sci. 2018, 123, 109–115. [Google Scholar] [CrossRef]
- Hwang, E.C.; Kim, Y.J.; Hwang, I.S.; Hwang, J.E.; Jung, S.I.; Kwon, D.D.; Park, K.; Ryu, S.B. Impact of diabetes mellitus on recurrence and progression in patients with non-muscle invasive bladder carcinoma: A retrospective cohort study. Int. J. Urol. 2011, 18, 769–776. [Google Scholar] [CrossRef]
- Rieken, M.; Xylinas, E.; Kluth, L.; Crivelli, J.J.; Chrystal, J.; Faison, T.; Lotan, Y.; Karakiewicz, P.I.; Fajkovic, H.; Babjuk, M.; et al. Association of diabetes mellitus and metformin use with oncological outcomes of patients with non-muscle-invasive bladder cancer. Br. J. Urol. 2013, 112, 1105–1112. [Google Scholar] [CrossRef]
- Hu, J.; Chen, J.-B.; Cui, Y.; Zhu, Y.-W.; Ren, W.-B.; Zhou, X.; Liu, L.-F.; Chen, H.-Q.; Zu, X.-B. Association of metformin intake with bladder cancer risk and oncologic outcomes in type 2 diabetes mellitus patients. Medicine 2018, 97, e11596. [Google Scholar] [CrossRef]
- Huang, W.-L.; Huang, K.-H.; Huang, C.-Y.; Pu, Y.-S.; Chang, H.-C.; Chow, P.-M. Effect of diabetes mellitus and glycemic control on the prognosis of non-muscle invasive bladder cancer: A retrospective study. BMC Urol. 2020, 20, 117. [Google Scholar] [CrossRef]
- Richardson, L.C.; A Pollack, L. Therapy Insight: Influence of type 2 diabetes on the development, treatment and outcomes of cancer. Nat. Clin. Pract. Oncol. 2005, 2, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Attia, N.; Caprio, S.; Jones, T.W.; Heptulla, R.; Holcombe, J.; Silver, D.; Sherwin, R.S.; Tamborlane, W.V. Changes in Free Insulin-Like Growth Factor-1 and Leptin Concentrations during Acute Metabolic Decompensation in Insulin Withdrawn Patients with Type 1 Diabetes1. J. Clin. Endocrinol. Metab. 1999, 84, 2324–2328. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fujita, N.; Hatakeyama, S.; Momota, M.; Tobisawa, Y.; Yoneyama, T.; Yamamoto, H.; Imai, A.; Ito, H.; Yoneyama, T.; Hashimoto, Y.; et al. Preoperative chronic kidney disease predicts poor prognosis in patients with primary non–muscle-invasive bladder cancer who underwent transurethral resection of bladder tumor. Urol. Oncol. Semin. Orig. Investig. 2020, 38, 684.e1–684.e8. [Google Scholar] [CrossRef] [PubMed]
- Li, C.-E.; Chien, C.-S.; Chuang, Y.-C.; Chang, Y.-I.; Tang, H.-P.; Kang, C.-H. Chronic kidney disease as an important risk factor for tumor recurrences, progression and overall survival in primary non-muscle-invasive bladder cancer. Int. Urol. Nephrol. 2016, 48, 993–999. [Google Scholar] [CrossRef] [PubMed]
- Kobatake, K.; Hayashi, T.; Black, P.C.; Goto, K.; Sentani, K.; Kaneko, M.; Yasui, W.; Mita, K.; Teishima, J.; Matsubara, A. Chronic kidney disease as a risk factor for recurrence and progression in patients with primary non-muscle-invasive bladder cancer. Int. J. Urol. 2017, 24, 594–600. [Google Scholar] [CrossRef]
- Rausch, S.; Hennenlotter, J.; Todenhöfer, T.; Aufderklamm, S.; Schwentner, C.; Sievert, K.-D.; Stenzl, A.; Gakis, G. Impaired estimated glomerular filtration rate is a significant predictor for non–muscle-invasive bladder cancer recurrence and progression—Introducing a novel prognostic model for bladder cancer recurrence. Urol. Oncol. Semin. Orig. Investig. 2014, 32, 1178–1183. [Google Scholar] [CrossRef]
- Kato, S.; Chmielewski, M.; Honda, H.; Pecoits-Filho, R.; Matsuo, S.; Yuzawa, Y.; Tranaeus, A.; Stenvinkel, P.; Lindholm, B. Aspects of Immune Dysfunction in End-stage Renal Disease. Clin. J. Am. Soc. Nephrol. 2008, 3, 1526–1533. [Google Scholar] [CrossRef]
- Mbeutcha, A.; Shariat, S.F.; Rieken, M.; Rink, M.; Xylinas, E.; Seitz, C.; Lucca, I.; Mathieu, R.; Rouprêt, M.; Briganti, A.; et al. Prognostic significance of markers of systemic inflammatory response in patients with non–muscle-invasive bladder cancer. Urol. Oncol. Semin. Orig. Investig. 2016, 34, 483.e17–483.e24. [Google Scholar] [CrossRef]
- Schupp, N.; Stopper, H.; Heidland, A. DNA Damage in Chronic Kidney Disease: Evaluation of Clinical Biomarkers. Oxidative Med. Cell. Longev. 2016, 2016, 3592042. [Google Scholar] [CrossRef]
- Reuter, S.; Gupta, S.C.; Chaturvedi, M.M.; Aggarwal, B.B. Oxidative stress, inflammation, and cancer: How are they linked? Free Radic. Biol. Med. 2010, 49, 1603–1616. [Google Scholar] [CrossRef]
- Byrne, K.; Levins, K.J.; Buggy, D.J. Can anesthetic-analgesic technique during primary cancer surgery affect recurrence or metastasis? Can. J. Anaesth. 2015, 63, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Tavare, A.N.; Perry, N.J.; Benzonana, L.L.; Takata, M.; Ma, D. Cancer recurrence after surgery: Direct and indirect effects of anesthetic agents*. Int. J. Cancer 2011, 130, 1237–1250. [Google Scholar] [CrossRef] [PubMed]
- Kim, R. Effects of surgery and anesthetic choice on immunosuppression and cancer recurrence. J. Transl. Med. 2018, 16, 8. [Google Scholar] [CrossRef] [PubMed]
- Sessler, D.I. Does regional analgesia reduce the risk of cancer recurrence? A hypothesis. Eur. J. Cancer Prev. 2008, 17, 269–272. [Google Scholar] [CrossRef]
- Ahlers, O.; Nachtigall, I.; Lenze, J.; Goldmann, A.; Schulte, E.; Höhne, C.; Fritz, G.; Keh, D. Intraoperative thoracic epidural anaesthesia attenuates stress-induced immunosuppression in patients undergoing major abdominal surgery. Br. J. Anaesth. 2008, 101, 781–787. [Google Scholar] [CrossRef]
- Piegeler, M.T.; Votta-Velis, M.E.G.; Liu, P.G.; Place, P.A.T.; Schwartz, M.D.E.; Beck-Schimmer, M.B.; Minshall, P.R.D.; Borgeat, M.A. Antimetastatic Potential of Amide-linked Local Anesthetics. Anesthesiology 2012, 117, 548–559. [Google Scholar] [CrossRef]
- Martin-Kleiner, I.; Balog, T.; Gabrilovac, J. Signal Transduction Induced by Opioids in Immune Cells: A Review. Neuroimmunomodulation 2006, 13, 1–7. [Google Scholar] [CrossRef]
- McCarthy, L.; Wetzel, M.; Sliker, J.K.; Eisenstein, T.K.; Rogers, T.J. Opioids, opioid receptors, and the immune response. Drug Alcohol Depend. 2001, 62, 111–123. [Google Scholar] [CrossRef]
- Kim, H.S.; Ku, J.H.; Kim, S.J.; Hong, S.J.; Kim, H.S.; Kwon, T.G.; Cho, J.S.; Jeon, S.S.; Joo, K.J.; Ahn, H.J.; et al. Prognostic Factors for Recurrence and Progression in Korean Non-Muscle-Invasive Bladder Cancer Patients: A Retrospective, Multi-Institutional Study. Yonsei Med. J. 2016, 57, 855–864. [Google Scholar] [CrossRef]
- Falke, J.; Witjes, J.A. Contemporary management of low-risk bladder cancer. Nat. Rev. Urol. 2011, 8, 42–49. [Google Scholar] [CrossRef]
- Kim, J.-A.; Yoon, S.; Kim, L.-Y.; Kim, D.-S. Towards Actualizing the Value Potential of Korea Health Insurance Review and Assessment (HIRA) Data as a Resource for Health Research: Strengths, Limitations, Applications, and Strategies for Optimal Use of HIRA Data. J. Korean Med. Sci. 2017, 32, 718–728. [Google Scholar] [CrossRef] [PubMed]

| Variable | Full Cohort (n = 4349) | Propensity Score-Matched Full Cohort (n = 1164) | ||||
|---|---|---|---|---|---|---|
| Regional (n = 582) | General (n = 3767) | p-Value | Regional (n = 582) | General (n = 582) | p-Value | |
| Age | 66.75 ± 6.09 | 65.50 ± 6.29 | <0.001 | 66.75 ± 6.09 | 66.50 ± 6.06 | 0.094 |
| Gender | <0.001 | 0.999 | ||||
| Male | 460 (79.04%) | 3131 (71.99%) | 460 (79.04%) | 460 (79.04%) | ||
| Female | 122 (20.96%) | 1218 (28.01%) | 122 (20.96%) | 122 (20.96%) | ||
| Medical history | ||||||
| Hypertension | 212 (36.45%) | 1476 (39.19%) | 0.001 | 212 (36.45%) | 212 (36.45%) | 0.999 |
| Diabetes mellitus | 82 (14.01%) | 557 (14.78%) | 0.180 | 82 (14.01%) | 82 (14.01%) | 0.999 |
| Myocardial infarction | 10 (1.65%) | 67 (1.78%) | 0.519 | 10 (1.65%) | 10 (1.65%) | 0.999 |
| Cerebral vascular disease | 55 (9.49%) | 377 (10.02%) | 0.281 | 55 (9.49%) | 55 (9.49%) | 0.999 |
| Congestive heart failure | 15 (2.52%) | 90 (2.40%) | 0.660 | 15 (2.52%) | 15 (2.52%) | 0.999 |
| Renal disease | 30 (5.20%) | 311 (8.25%) | <0.001 | 30 (5.20%) | 32 (5.50%) | 0.453 |
| Dementia | 26 (4.42%) | 1772 (4.57%) | 0.668 | 26 (4.42%) | 26 (4.42%) | 0.999 |
| Liver disease | 15 (2.52%) | 90 (2.40%) | 0.642 | 15 (2.52%) | 15 (2.52%) | 0.999 |
| COPD | 79 (13.62%) | 520 (13.80) | 0.766 | 79 (13.62%) | 79 (13.62%) | 0.999 |
| Follow-up (day) | 1607.05 ± 651.74 | 1598.93 ± 655.66 | 1607.05 ± 651.74 | 1606.19 ± 652.64 | ||
| Recurrence | 107 (18.38%) | 710 (18.85%) | 0.451 | 107 (18.38%) | 108 (18.56%) | 0.613 |
| Variable | Propensity Score-Matched Full Cohort | |
|---|---|---|
| HR (95% CI) | p-Value | |
| Age (≥65) | 1.65 (1.47–1.85) | <0.001 |
| Male | 1.73 (1.52–1.97) | <0.001 |
| Medical history | ||
| Hypertension | 1.24 (1.08–1.42) | 0.003 |
| Diabetes mellitus | 1.30 (1.13–1.50) | 0.001 |
| Myocardial infarction | 1.36 (0.89–2.08) | 0.161 |
| Cerebral vascular disease | 0.65 (0.24–1.75) | 0.399 |
| Congestive heart failure | 1.04 (0.86–1.27) | 0.669 |
| Renal disease | 1.74 (1.33–2.28) | <0.001 |
| Dementia | 0.95 (0.79–1.13) | 0.553 |
| Liver disease | 1.01 (0.86–1.19) | 0.863 |
| COPD | 1.02 (0.91–1.15) | 0.725 |
| Anesthetic method | ||
| Regional | 1.11 (0.97–1.28) | 0.131 |
| General | 0.97 (0.79–1.19) | 0.743 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.W.; Tae, B.S.; Choi, Y.J.; Yoon, S.M.; Lee, Y.S.; Kim, J.H.; Shin, H.W.; Park, J.Y.; Bae, J.H. A Comparison of the Anesthetic Methods for Recurrence Rates of Bladder Cancer after Transurethral Resection of Bladder Tumors Using National Health Insurance Claims Data of South Korea. J. Clin. Med. 2022, 11, 1143. https://doi.org/10.3390/jcm11041143
Lee SW, Tae BS, Choi YJ, Yoon SM, Lee YS, Kim JH, Shin HW, Park JY, Bae JH. A Comparison of the Anesthetic Methods for Recurrence Rates of Bladder Cancer after Transurethral Resection of Bladder Tumors Using National Health Insurance Claims Data of South Korea. Journal of Clinical Medicine. 2022; 11(4):1143. https://doi.org/10.3390/jcm11041143
Chicago/Turabian StyleLee, Sang Won, Bum Sik Tae, Yoon Ji Choi, Sang Min Yoon, Yoon Sook Lee, Jae Hwan Kim, Hye Won Shin, Jae Young Park, and Jae Hyun Bae. 2022. "A Comparison of the Anesthetic Methods for Recurrence Rates of Bladder Cancer after Transurethral Resection of Bladder Tumors Using National Health Insurance Claims Data of South Korea" Journal of Clinical Medicine 11, no. 4: 1143. https://doi.org/10.3390/jcm11041143
APA StyleLee, S. W., Tae, B. S., Choi, Y. J., Yoon, S. M., Lee, Y. S., Kim, J. H., Shin, H. W., Park, J. Y., & Bae, J. H. (2022). A Comparison of the Anesthetic Methods for Recurrence Rates of Bladder Cancer after Transurethral Resection of Bladder Tumors Using National Health Insurance Claims Data of South Korea. Journal of Clinical Medicine, 11(4), 1143. https://doi.org/10.3390/jcm11041143






