Alexithymia in Adolescents with Acne: Association with Quality of Life Impairment and Stigmatization
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Questionnaires Used
2.2.1. Alexithymia Assessment
2.2.2. Quality of Life Assessment
2.2.3. Stigmatization Assessment
2.3. Statistical Analysis
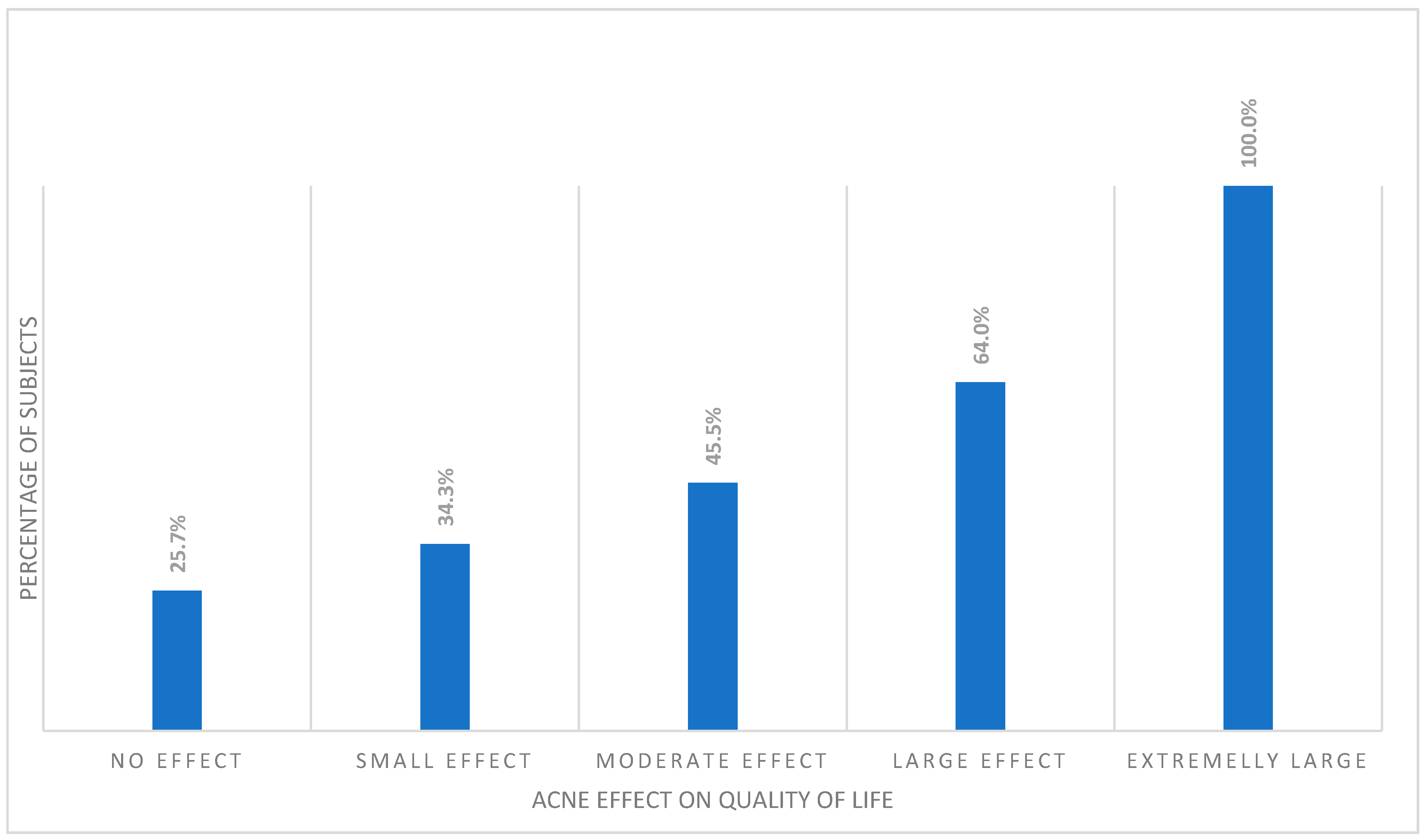
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wolkenstein, P.; Machovcová, A.; Szepietowski, J.C.; Tennstedt, D.; Veraldi, S.; Delarue, A. Acne prevalence and associations with lifestyle: A cross-sectional online survey of adolescents/young adults in 7 European countries. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Dreno, B.; Poli, F. Epidemiology of acne. Dermatology 2003, 206, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Smithard, A.; Glazebrook, C.; Williams, H.C. Acne prevalence, knowledge about acne and psychological morbidity in mid-adolescence: A community-based study. Br. J. Dermatol. 2001, 145, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Molla, A.; Alrizqi, H.; Alharbi, E.; Alsubhi, A.; Alrizqi, S.; Shahada, O. Assessment of Anxiety and Depression in Patients with Acne Vulgaris in Medina: A Case-Control Study. Clin. Cosmet. Investig. Dermatol. 2021, 14, 999–1007. [Google Scholar] [CrossRef]
- Cengiz, G.F.; Gürel, G. Difficulties in emotion regulation and quality of life in patients with acne. Qual. Life Res. 2020, 29, 431–438. [Google Scholar] [CrossRef]
- Tan, J.; Beissert, S.; Cook-Bolden, F.; Chavda, R.; Harper, J.; Hebert, A.; Lain, E.; Layton, A.; Rocha, M.; Weiss, J.; et al. Impact of facial and truncal acne on quality of life: A multi-country population-based survey. JAAD Int. 2021, 3, 102–110. [Google Scholar] [CrossRef]
- Naveed, S.; Masood, S.; Rahman, A.; Awan, S.; Tabassum, S. Impact of acne on quality of life in young Pakistani adults and its relationship with severity: A multicenter study. Pak. J. Med. Sci. 2021, 37, 727–732. [Google Scholar] [CrossRef]
- Đurović, M.R.; Đurović, M.; Janković, J.; Janković, S. Quality of life in Montenegrin pupils with acne. PLoS ONE 2021, 16, e0250155. [Google Scholar] [CrossRef]
- Sifneos, P.E. The prevalence of ‘alexithymic’ characteristics in psychosomatic patients. Psychother. Psychosom. 1973, 22, 255–262. [Google Scholar] [CrossRef]
- Carpenter, K.M.; Addis, M.E. Alexithymia, Gender, and Responses to Depressive Symptoms. Sex Roles 2000, 43, 629–644. [Google Scholar] [CrossRef]
- Rzepka, M.; Toś, M.; Bratek, A.; Rybak, E.; Drzyzga, K.; Kucia, K. Family and demographic factors related to alexithymia in Polish students. Arch. Psychiatry Psychother. 2019, 21, 22–27. [Google Scholar]
- Taylor, G.J. The alexithymia construct: Conceptualization, validation, and relationship with basic dimensions of personality. New Trends Exp. Clin. Psychiatry 1994, 10, 61–74. [Google Scholar]
- Panasiti, M.S.; Ponsi, G.; Violani, C. Emotions, Alexithymia, and Emotion Regulation in Patients with Psoriasis. Front. Psychol. 2020, 11, 836. [Google Scholar] [CrossRef] [PubMed]
- Mattila, A.K.; Salminen, J.K.; Nummi, T.; Joukamaa, M. Age is strongly associated with alexithymia in the general population. J. Psychosom. Res. 2006, 61, 629–635. [Google Scholar] [CrossRef] [PubMed]
- Dehghani, F.; Dehghani, F.; Kafaie, P.; Taghizadeh, M.R. Alexithymia in different dermatologic patients. Asian J. Psychiatry 2017, 25, 42–45. [Google Scholar] [CrossRef]
- Willemsen, R.; Roseeuw, D.; Vanderlinden, J. Alexithymia and dermatology: The state of the art. Int. J. Dermatol. 2008, 47, 903–910. [Google Scholar] [CrossRef]
- Assogna, F.; Cravello, L.; Orfei, M.D.; Cellupica, N.; Caltagirone, C.; Spalletta, G. Alexithymia in Parkinson’s disease: A systematic review of the literature. Parkinsonism Relat. Disord. 2016, 28, 1–11. [Google Scholar] [CrossRef]
- Ossola, P.; Gerra, M.L.; Beltrani, M.; Marchesi, C. Alexithymia and Cardiac Outcome in Patients at First Acute Coronary Syndrome. Int. J. Behav. Med. 2019, 26, 673–679. [Google Scholar] [CrossRef]
- Calia, R.; Lai, C.; Aceto, P.; Luciani, M.; Camardese, G.; Lai, S.; Fantozzi, C.; Pietroni, V.; Salerno, M.P.; Spagnoletti, G.; et al. Emotional self-efficacy and alexithymia may affect compliance, renal function and quality of life in kidney transplant recipients: Results from a preliminary cross-sectional study. Physiol. Behav. 2015, 142, 152–154. [Google Scholar] [CrossRef]
- Talamonti, M.; Galluzzo, M.; Silvaggio, D.; Lombardo, P.; Tartaglia, C.; Bianchi, L. Quality of Life and Psychological Impact in Patients with Atopic Dermatitis. J. Clin. Med. 2021, 10, 1298. [Google Scholar] [CrossRef]
- Heisig, M.; Reich, A.; Szepietowski, J.C. Alexithymia in Uraemic Pruritus. Acta Derm.-Venereol. 2016, 96, 699–700. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glowaczewska, A.; Szepietowski, J.C.; Matusiak, L. Prevalence and Associated Factors of Alexithymia in Patients with Hidradenitis Suppurativa: A Cross-sectional Study. Acta Derm.-Venereol. 2021, 101, adv00598. [Google Scholar] [CrossRef] [PubMed]
- Misery, L. Alexithymia and psoriasis: What is the link? Br. J. Dermatol. 2019, 180, 261. [Google Scholar] [CrossRef] [PubMed]
- Sunay, D.; Baykir, M.; Ateş, G.; Ekşioğlu, M. Alexithymia and Acne Vulgaris: A Case Control Study. Psychiatry Investig. 2011, 8, 327–333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feki, R.; Sellami, R.; Feki, I.; Trigui, D.; Turki, H.; Masmoudi, J. Association between depression and alexithymia in adolescents with Acne vulgaris. Eur. Psychiatry 2017, 41, S437. [Google Scholar] [CrossRef]
- Eusebio-Alpapara, K. Acne Severity Scale: How Bad Is Your Acne? 2021. Available online: www.thankyourskin.com/acne-severity-scale/ (accessed on 28 December 2021).
- Alsulaimani, H.; Kokandi, A.; Khawandanh, S.; Hamad, R. Severity of Acne Vulgaris: Comparison of Two Assessment Methods. Clin. Cosmet. Investig. Dermatol. 2020, 13, 711–716. [Google Scholar] [CrossRef]
- Bagby, R.M.; Parker, J.D.A.; Taylor, G.J. The twenty-item Toronto Alexithymia scale—I. Item selection and cross-validation of the factor structure. J. Psychosom. Res. 1994, 38, 23–32. [Google Scholar] [CrossRef]
- Ścigała, D.; Zdankiewicz-Ścigała, E.; Bedyńska, S.; Kokoszka, A. Psychometric Properties and Configural Invariance of the Polish—Language Version of the 20-Item Toronto Alexithymia Scale in Non-clinical and Alcohol Addict Persons. Front. Psychol. 2020, 11, 1241. [Google Scholar] [CrossRef]
- Finlay, A.Y.; Khan, G.K. Dermatology Life Quality Index (DLQI)—A simple practical measure for routine clinical use. Clin. Exp. Dermatol. 1994, 19, 210–216. [Google Scholar] [CrossRef]
- Szepietowski, J.; Salomon, J.; Finlay, A.Y.; Klepacki, A.; Chodynicka, B.; Marionneau, N.; TaYeb, C.; Myon, E. Wskaznik wplywu dolegliwosci skornych na jakosc zycia-Dermatology Life Quality Index (DLQI): Polska wersja jezykowa. Dermatol. Klin. 2004, 6, 63–70. [Google Scholar]
- Hongbo, Y.; Thomas, C.L.; Harrison, M.A.; Salek, M.S.; Finlay, A.Y. Translating the science of quality of life into practice: What do dermatology life quality index scores mean? J. Invest. Dermatol. 2005, 125, 659–664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hrehorów, E.; Szepietowski, J.; Reich, A.; Evers, A.; Ginsburg, I. Instruments for stigmatization evaluation in patients suffering from psoriasis: Polish language versions. Dermatol. Klin. 2006, 8, 253–258. [Google Scholar]
- Lu, Y.; Duller, P.; van der Valk, P.G.M.; Evers, A.W.M. Helplessness as Predictor of Perceived Stigmatization in Patients with Psoriasis and Atopic Dermatitis. Dermatol. Psychosom. 2003, 4, 146–150. [Google Scholar] [CrossRef]
- Ayer, J.; Burrows, N. Acne: More than skin deep. Postgrad. Med. J. 2006, 82, 500–506. [Google Scholar] [CrossRef] [PubMed]
- Altunay, I.K.; Ozkur, E.; Dalgard, F.J.; Gieler, U.; Tomas Aragones, L.; Lien, L.; Poot, F.; Jemec, G.B.; Misery, L.; Szabó, C.; et al. Psychosocial Aspects of Adult Acne: Data from 13 European Countries. Acta Derm.-Venereol. 2020, 100, adv00051. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Samuels, D.V.; Rosenthal, R.; Lin, R.; Chaudhari, S.; Natsuaki, M.N. Acne vulgaris and risk of depression and anxiety: A meta-analytic review. J. Am. Acad. Dermatol. 2020, 83, 532–541. [Google Scholar] [CrossRef] [PubMed]
- Beisert, M.; Pilarczyk, K.; Zakrzewska, M.; Pawlaczyk, M. Sexual satisfaction and self-esteem in women with acne. J. Cosmet. Dermatol. 2020, 19, 1768–1773. [Google Scholar] [CrossRef] [PubMed]
- Baldwin, H.E. The interaction between acne vulgaris and the psyche. Cutis 2002, 70, 133–139. [Google Scholar]
- Montreuil, M.; Pedinielli, J.L. Parallel visual processing characteristics in healthy alexithymic subjects. Administration of the Toronto Alexithymia Scale and the parallel visual information test. Encephale 1995, 21, 589–595. [Google Scholar]
- Benjamin, A.; Kuperman, Y.; Eren, N.; Rotkopf, R.; Amitai, M.; Rossman, H.; Shilo, S.; Meir, T.; Keshet, A.; Nuttman-Shwartzet, O.; et al. Stress-related emotional and behavioural impact following the first COVID-19 outbreak peak. Mol. Psychiatry 2021, 26, 6149–6158. [Google Scholar] [CrossRef]
- Veronese, G.; Mahamid, F.; Bdier, D.; Pancake, R. Stress of COVID-19 and mental health outcomes in Palestine: The mediating role of well-being and resilience. Health Psychol. Rep. 2021, 9, 398–410. [Google Scholar] [CrossRef]
- Kim, H.W.; Rim, H.D.; Kim, J.H.; Lee, S.J. Alexithymia and Stress Response Patterns among Patients with Depressive Disorders in Korea. Psychiatry Investig. 2009, 6, 13–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, C.S.; Sinha, R. Alexithymia and stress-induced brain activation in cocaine-dependent men and women. J. Psychiatry Neurosci. 2006, 31, 115–121. [Google Scholar] [PubMed]
- Ravens-Sieberer, U.; Kaman, A.; Erhart, M.; Devine, J.; Schlack, R.; Otto, C. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur. Child Adolesc. Psychiatry 2021. [Google Scholar] [CrossRef] [PubMed]
- Richards, H.L.; Fortune, D.G.; Griffiths, C.E.M.; Main, C.J. Alexithymia in patients with psoriasis: Clinical correlates and psychometric properties of the Toronto Alexithymia Scale-20. J. Psychosom. Res. 2005, 58, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Consoli, S.M.; Rolhion, S.; Martin, C.; Ruel, K.; Cambazard, F.; Pellet, J.; Misery, L. Low levels of emotional awareness predict a better response to dermatological treatment in patients with psoriasis. Dermatology 2006, 212, 128–136. [Google Scholar] [CrossRef] [PubMed]
- Picardi, A.; Mazzotti, E.; Gaetano, P.; Cattaruzza, M.S.; Baliva, G.; Melchi, C.F.; Biondi, M.; Pasquini, P. Stress, social support, emotional regulation, and exacerbation of diffuse plaque psoriasis. Psychosomatics 2005, 46, 556–564. [Google Scholar] [CrossRef]
- Chiricozzi, A.; Esposito, M.; Gisondi, P.; Valenti, M.; Gori, N.; Giovanardi, G.; Bellinato, F.; De Simone, C.; Costanzo, A.; Fargnoli, M.C.; et al. Disease Severity Is Associated with Alexithymia in Patients with Atopic Dermatitis. Dermatology 2020, 236, 329–335. [Google Scholar] [CrossRef]
- Picardi, A.; Pasquini, P.; Cattaruzza, M.S.; Gaetano, P.; Melchi, C.F.; Baliva, G.; Camaioni, D.; Tiago, A.; Abeni, D.; Biondi, M. Stressful life events, social support, attachment security and alexithymia in vitiligo. A case-control study. Psychother. Psychosom. 2003, 72, 150–158. [Google Scholar] [CrossRef]
- Chiricozzi, A.; Giovanardi, G.; Caro, D.R.C.; Iannone, M.; Garcovich, S.; Dini, V.; De Simone, C.; Franceschini, C.; Oranges, T.; Mingrone, G.; et al. Alexithymia affects patients with hidradenitis suppurativa. Eur. J. Dermatol. 2018, 28, 482–487. [Google Scholar] [CrossRef]
- Willemsen, R.; Haentjens, P.; Roseeuw, D.; Vanderlinden, J. Alexithymia in patients with alopecia areata: Educational background much more important than traumatic events. J. Eur. Acad. Dermatol. Venereol. 2009, 23, 1141–1146. [Google Scholar] [CrossRef] [PubMed]
- Rubino, I.A.; Sonnino, A.; Stefanato, C.M.; Pezzarossa, B.; Ciani, N. Separation-individuation, aggression and alexithymia in psoriasis. Acta Derm.-Venereol. Suppl. 1989, 146, 87–90. [Google Scholar]
- Fava, G.A.; Perini, G.I.; Santonastaso, P.; Fornasa, C.V. Life events and psychological distress in dermatologic disorders: Psoriasis, chronic urticaria and fungal infections. Br. J. Med. Psychol. 1980, 53, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Talamonti, M.; Galluzzo, M.; Servoli, S.; D’Adamio, S.; Bianchi, L. Alexithymia and Plaque Psoriasis: Preliminary Investigation in a Clinical Sample of 250 Patients. Dermatology 2016, 232, 648–654. [Google Scholar] [CrossRef] [PubMed]
- Quinto, R.M.; Sampogna, F.; Fania, L.; Ciccone, D.; Fusari, R.; Mastroeni, S.; Iani, L.; Abeni, D. Alexithymia, Psychological Distress, and Social Impairment in Patients with Hidradenitis Suppurativa. Dermatology 2021, 237, 103–110. [Google Scholar] [CrossRef]
- Galluzzo, M.; D’Adamio, S.; Campione, E.; Mazzilli, S.; Bianchi, L.; Talamonti, M. A clinical case of severe disease burden: An erythrodermic psoriatic patient treated with secukinumab. J. Dermatol. Treat. 2018, 29 (Suppl. 1), 17–20. [Google Scholar] [CrossRef]
- Alvarado-Bolaños, A.; Cervantes-Arriaga, A.; Zuazua-Vidal, L.; Esquivel-Zapata, Ó.; Alcocer-Salas, Á.; Rodríguez-Violante, M. Determinants and impact of alexithymia on quality of life in Parkinson’s disease. Neurología, 2020; in press. [Google Scholar]
- Klietz, M.; Schnur, T.; Drexel, S.C.; Lange, F.; Paracka, L.; Huber, M.K.; Dressler, D.; Höglinger, G.U.; Wegner, F. Alexithymia Is Associated with Reduced Quality of Life and Increased Caregiver Burden in Parkinson’s Disease. Brain Sci. 2020, 10, 401. [Google Scholar] [CrossRef]
- Loas, G.; Braun, S.; Delhaye, M.; Linkowski, P. The measurement of alexithymia in children and adolescents: Psychometric properties of the Alexithymia Questionnaire for Children and the twenty-item Toronto Alexithymia Scale in different non-clinical and clinical samples of children and adolescents. PLoS ONE 2017, 12, e0177982. [Google Scholar] [CrossRef] [Green Version]
| Alexithymia, Number of Subject (%) | Whole Group (n = 730) | Acne Group (n = 476) | Non-Acne Group (n = 254) | p |
|---|---|---|---|---|
| Alexithymia | 226 (31.0) | 144 (30.3) | 82 (32.3) | NS |
| Intermediate alexithymia | 183 (25.1) | 116 (24.4) | 67 (26.4) | NS |
| No alexithymia | 321 (44.0) | 216 (45.4) | 105 (41.3) | NS |
| Toronto Alexithymia Scale (Points) | Acne Group (n = 476) | Non-Acne Group (n = 254) | p |
|---|---|---|---|
| Total score | 53.1 ± 12.8 | 53.5 ± 11.9 | NS |
| DIF subscale | 19.7 ± 7.1 | 19.7 ± 6.7 | NS |
| DDF subscale | 15.2 ± 5.1 | 15.4 ± 4.8 | NS |
| EOT subscale | 19.1 ± 4.4 | 18.4 ± 4.4 | NS |
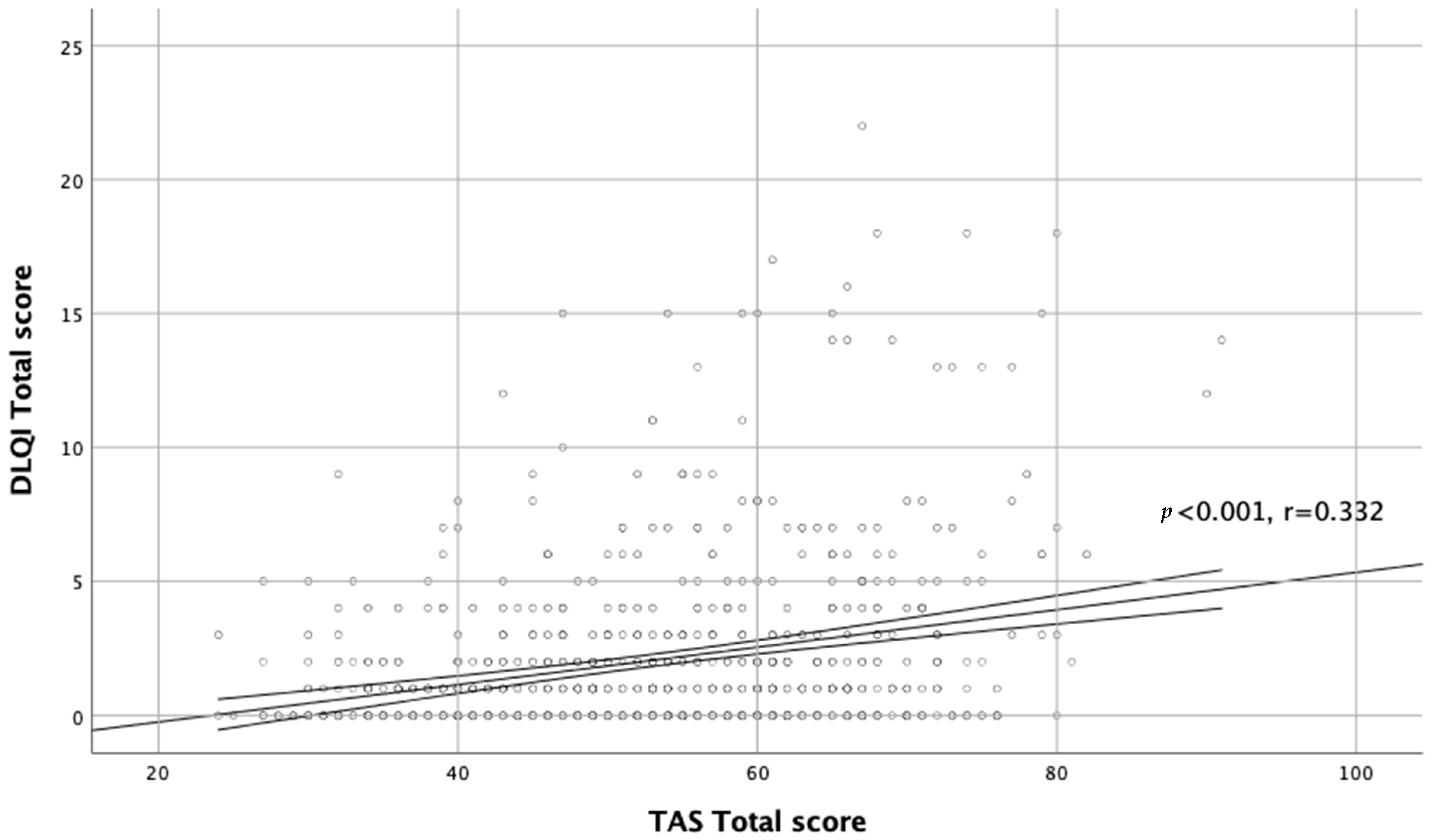
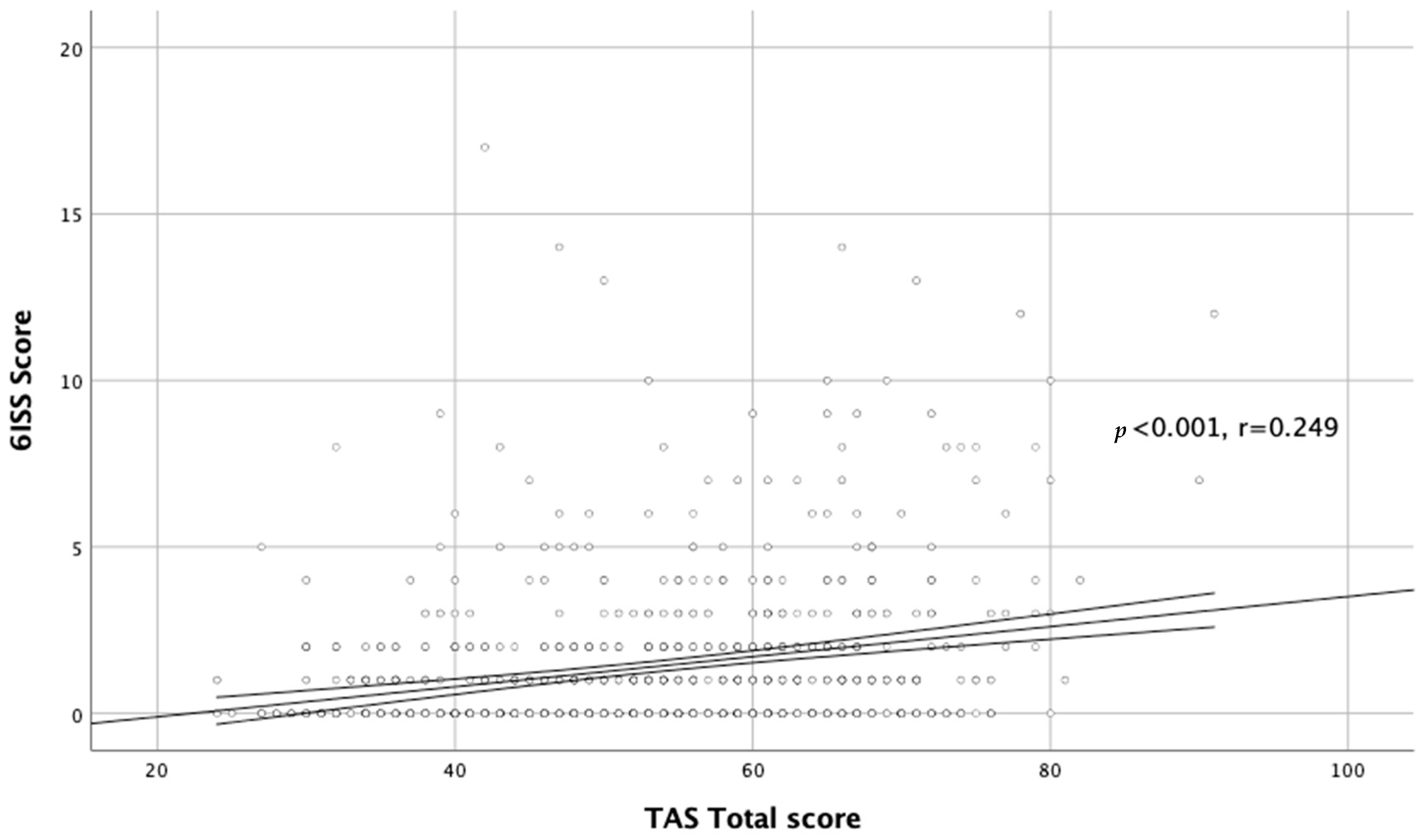
| Toronto Alexithymia Scale (TAS-20) | DLQI Total Score | DLQI Score Girls | DLQI Score Boys | 6ISS Total Score | 6ISS Girls | 6ISS Boys |
|---|---|---|---|---|---|---|
| Total score | p < 0.001 r = 0.332 | p < 0.001 r = 0.283 | p < 0.001 r = 0.332 | p < 0.001 r = 0.249 | p < 0.001 r = 0.286 | NS |
| DIF subscale | p < 0.001 r = 0.316 | p < 0.001 r = 0.346 | p < 0.001 r = 0.294 | p < 0.001 r = 0.314 | p < 0.001 r = 0.308 | p = 0.007 r = 0.186 |
| DDF subscale | p < 0.001 r = 0.207 | p < 0.001 r = 0.211 | p < 0.001 r = 0.267 | p < 0.001 r = 0.277 | p < 0.001 r = 0.288 | p = 0.003 r = 0.201 |
| EOT subscale | NS | NS | NS | NS | NS | NS |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szepietowska, M.; Dąbrowska, A.; Nowak, B.; Skinderowicz, K.; Wilczyński, B.; Krajewski, P.K.; Jankowska-Konsur, A. Alexithymia in Adolescents with Acne: Association with Quality of Life Impairment and Stigmatization. J. Clin. Med. 2022, 11, 732. https://doi.org/10.3390/jcm11030732
Szepietowska M, Dąbrowska A, Nowak B, Skinderowicz K, Wilczyński B, Krajewski PK, Jankowska-Konsur A. Alexithymia in Adolescents with Acne: Association with Quality of Life Impairment and Stigmatization. Journal of Clinical Medicine. 2022; 11(3):732. https://doi.org/10.3390/jcm11030732
Chicago/Turabian StyleSzepietowska, Marta, Alicja Dąbrowska, Bernadetta Nowak, Katarzyna Skinderowicz, Bartosz Wilczyński, Piotr K. Krajewski, and Alina Jankowska-Konsur. 2022. "Alexithymia in Adolescents with Acne: Association with Quality of Life Impairment and Stigmatization" Journal of Clinical Medicine 11, no. 3: 732. https://doi.org/10.3390/jcm11030732
APA StyleSzepietowska, M., Dąbrowska, A., Nowak, B., Skinderowicz, K., Wilczyński, B., Krajewski, P. K., & Jankowska-Konsur, A. (2022). Alexithymia in Adolescents with Acne: Association with Quality of Life Impairment and Stigmatization. Journal of Clinical Medicine, 11(3), 732. https://doi.org/10.3390/jcm11030732






