Cancer Impacts Prognosis on Mortality in Patients with Acute Heart Failure: Analysis of the EPICTER Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Population
2.2. Study Variables
2.3. Follow Up
2.4. Statistical Analysis
2.5. Ethical Aspects
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ameri, P.; Canepa, M.; Anker, M.S.; Belenkov, Y.; Bergler-Klein, J.; Cohen-Solal, A.; Farmakis, D.; López-Fernández, T.; Lainscak, M.; Pudil, R.; et al. Heart Failure Association Cardio-Oncology Study Group of the European Society of Cardiology Cancer diagnosis in patients with heart failure: Epidemiology, clinical implications and gaps in knowledge. Eur. J. Heart Fail. 2018, 20, 879–887. [Google Scholar] [CrossRef]
- Cuomo, A.; Paudice, F.; D’Angelo, G.; Perrotta, G.; Carannante, A.; Attanasio, U.; Iengo, M.; Fiore, F.; Tocchetti, C.G.; Mercurio, V.; et al. New-Onset Cancer in the HF Population: Epidemiology, Pathophysiology, and Clinical Management. Curr. Heart Fail. Rep. 2021, 18, 191–199. [Google Scholar] [CrossRef]
- Mehta, L.S.; Watson, K.E.; Barac, A.; Beckie, T.M.; Bittner, V.; Cruz-Flores, S.; Dent, S.; Kondapalli, L.; Ky, B.; Okwuosa, T.; et al. Cardiovascular disease and breast cancer: Where these entities intersect: A scientific statement from the American Heart Association. Circulation 2018, 137, e30–e66. [Google Scholar] [CrossRef] [PubMed]
- Bertero, E.; Canepa, M.; Maack, C.; Ameri, P. Linking Heart Failure to Cancer: Background Evidence and Research Perspectives. Circulation 2018, 138, 735–742. [Google Scholar] [CrossRef] [PubMed]
- Hara, M.R.; Kovacs, J.J.; Whalen, E.J.; Rajagopal, S.; Strachan, R.T.; Grant, W.; Towers, A.J.; Williams, B.; Lam, C.M.; Xiao, K.; et al. A stress response pathway regulates DNA damage through β2-adrenoreceptors and β-arrestin-1. Nature 2011, 477, 349–353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- George, A.J.; Thomas, W.G.; Hannan, R.D. The renin–angiotensin system and cancer: Old dog, new tricks. Nat. Rev. Cancer 2010, 10, 745–759. [Google Scholar] [CrossRef] [PubMed]
- Paulus, W.J.; Tschöpe, C. A novel paradigm for heart failure with preserved ejection fraction: Comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J. Am. Coll. Cardiol. 2013, 62, 263–271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Banke, A.; Schou, M.; Videbaek, L.; Møller, J.E.; Torp-Pedersen, C.; Gustafsson, F.; Dahl, J.S.; Køber, L.; Hildebrandt, P.R.; Gislason, G.H. Incidence of cancer in patients with chronic heart failure: A long-term follow-up study. Eur. J. Heart Fail. 2016, 18, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Hasin, T.; Gerber, Y.; McNallan, S.M.; Weston, S.A.; Kushwaha, S.S.; Nelson, T.J.; Cerhan, J.R.; Roger, V.L. Patients with heart failure have an increased risk of incident cancer. J. Am. Coll. Cardiol. 2013, 62, 881–886. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sicras-Mainar, A.; Sicras-Navarro, A.; Palacios, B.; Varela, L.; Delgado, J.F. Epidemiology and treatment of heart failure in Spain: The HF-PATHWAYS study. Rev. Esp. Cardiol. 2020, 27, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Meijers, W.C.; de Boer, R.A. Common risk factors for heart failure and cancer. Cardiovasc. Res. 2019, 115, 844–853. [Google Scholar] [CrossRef] [PubMed]
- Santos, N.F.D.; Pinho, C.P.S.; Cardoso, A.J.P.F.; Mendes, R.M.L. Cachexia in hospitalized patients with heart failure. Nutr. Hosp. 2018, 35, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Witte, K.K.A.; Clark, A.L. Nutritional abnormalities contributing to cachexia in chronic illness. Int. J. Cardiol. 2002, 85, 23–31. [Google Scholar] [CrossRef]
- Florea, V.G.; Henein, M.Y.; Rauchhaus, M.; Koloczek, V.; Sharma, R.; Doehner, W.; Poole-Wilson, P.A.; Coats, A.J.; Anker, S.D. The cardiac component of cardiac cachexia. Am. Heart J. 2002, 144, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Argilés, J.M.; Busquets, S.; López-Soriano, F.J.; Figueras, M. Fisiopatología de la caquexia neoplásica Pathophysiology of neoplasic cachexia. Nutr. Hosp. 2006, 21, 4–9. [Google Scholar] [PubMed]
- Patel, R.B.; Warraich, H.J.; Butler, J.; Vaduganathan, M. Surprise, surprise: Improving the referral pathway to palliative care interventions in advanced heart failure. Eur. J. Heart Fail. 2019, 21, 235–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Díez-Manglano, J.; Sánchez Muñoz, L.Á.; García Fenoll, R.; Freire, E.; Isasi de Isasmendi Pérez, S.; Carneiro, A.H.; Torres Bonafonte, O. Spanish and Portuguese Societies of Internal Medicine consensus guideline about best practice in end-of-life care. Rev. Clin. Esp. 2020, 221, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Egídio de Sousa, I.; Pedroso, A.; Chambino, B.; Roldão, M.; Pinto, F.; Guerreiro, R.; Araújo, I.; Henriques, C.; Fonseca, C. Palliative Care in Heart Failure: Challenging Prognostication. Cureus 2021, 13, e18301. [Google Scholar] [CrossRef] [PubMed]
- Aaronson, E.L.; George, N.; Ouchi, K.; Zheng, H.; Bowman, J.; Monette, D.; Jacobsen, J.; Jackson, V. The surprise question can be used to identify heart failure patients in the emergency department who would benefit from palliative care. J. Pain Symptom Manag. 2019, 57, 944–951. [Google Scholar] [CrossRef] [PubMed]
| Variable | Acute HF with Cancer (n = 394) | Acute HF without Cancer (n = 2733) | p |
|---|---|---|---|
| Age | 79.29 +/− 10.2 | 78.83 +/− 11.05 | p = 0.439 |
| Sex (male) | 247 (63%) | 1295 (47%) | p < 0.001 |
| NYHA III-IV | 82/383 (21%) | 639/2683 (24%) | p = 0.334 |
| LVEF | 53.28% +/− 15.78 | 50.63% +/− 16.14 | p = 0.018 |
| NTpro-BNP | 8933 pg/mL +/− 1247 | 8334 pg/mL +/− 349 | p = 0.561 |
| Charlson score | 4.42 +/− 1.7 | 3.44 +/− 1.86 | p < 0.001 |
| Comorbid conditions | |||
| Hypertension | 332/393 (85%) | 2322/2726 (85%) | p = 0.705 |
| Diabetes | 168/392 (43%) | 1257/2724 (46%) | p = 0.23 |
| Ischemic cardiopathy | 113/390 (29%) | 885/2698 (33%) | p = 0.13 |
| Atrial fibrillation | 219/393 (56%) | 1556/2723 (57%) | p = 0.624 |
| Valvulopathy | 176/377 (47%) | 1141/2621 (44%) | p = 0.267 |
| COPD | 104/386 (27%) | 704/2699 (26%) | p = 0.711 |
| Chronic renal failure | 210/393 (53%) | 1254/2708 (46%) | p = 0.009 |
| Previous cerebrovascular disease | 75/392 (19%) | 592/2700 (22%) | p = 0.237 |
| Anaemia | 211/394 (54%) | 1302/2713 (48%) | p = 0.040 |
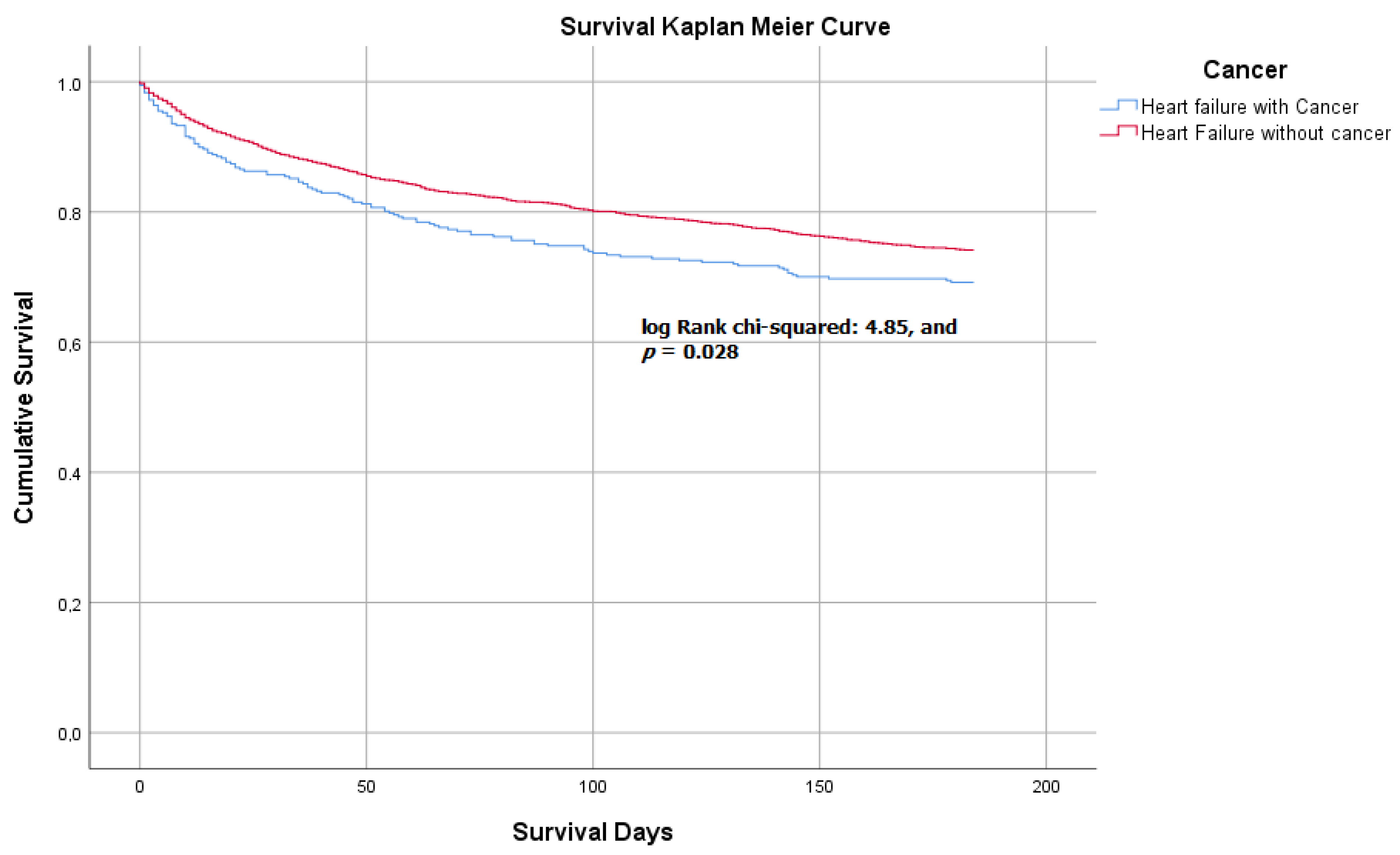
| In-hospital and 6-month follow-up mortality | 110/3573 (31%) | 637/2466 (26%) | p = 0.046 |
| Variable | Acute HF with Solid Tumor | Acute HF without Solid Tumor | p |
|---|---|---|---|
| Weight loss | 29/161 (18%) | 143/1227 (12%) | p = 0.03 |
| Functional decline | 78/181 (43%) | 461/1313 (35%) | p = 0.039 |
| Dyspnea | 208/261 (80%) | 1375/1767 (78%) | p = 0.52 |
| Anxiety | 87/621 (33%) | 572/1767 (32%) | p = 0.77 |
| Nausea | 36/261 (14%) | 197/1767 (11%) | p = 0.021 |
| Chest pain | 49/261 (19%) | 333/1764 (19%) | p = 1.00 |
| Generalized pain | 75/261 (29%) | 478/1285 (27%) | p = 0.603 |
| Delirium | 40/261 (15%) | 262/1767 (15%) | p = 0.85 |
| Insomnia | 97/261 (37%) | 613/1765 (35%) | p = 0.445 |
| Variable | Acute HF with Solid Tumor (n = 394) | Acute HF without Solid Tumor (n = 2733) | p |
|---|---|---|---|
| Intravenous furosemide | 98.5% | 97.4% | p = 0.394 |
| Noninvasive mechanical ventilation | 5% | 5% | p = 0.423 |
| Hypertonic saline + furosemide | 2% | 3% | p = 0.394 |
| Use of amines | 5% | 5% | p = 0.618 |
| Vasodilators | 9% | 11% | p = 0.892 |
| Dialysis | 1% | 1% | p = 0.987 |
| Oral morphine | 32% | 26% | p = 0.045 |
| Intravenous morphine | 12% | 11% | p = 0.823 |
| Benzodiazepines | 36% | 33% | p = 0.405 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Méndez-Bailón, M.; Lorenzo-Villalba, N.; Romero-Correa, M.; Guisado-Espartero, E.; González-Soler, J.; Rugeles-Niño, J.; Sebastián-Leza, A.; Ceresuela-Eito, L.; Romaní-Costa, V.; Quesada-Simón, A.; et al. Cancer Impacts Prognosis on Mortality in Patients with Acute Heart Failure: Analysis of the EPICTER Study. J. Clin. Med. 2022, 11, 571. https://doi.org/10.3390/jcm11030571
Méndez-Bailón M, Lorenzo-Villalba N, Romero-Correa M, Guisado-Espartero E, González-Soler J, Rugeles-Niño J, Sebastián-Leza A, Ceresuela-Eito L, Romaní-Costa V, Quesada-Simón A, et al. Cancer Impacts Prognosis on Mortality in Patients with Acute Heart Failure: Analysis of the EPICTER Study. Journal of Clinical Medicine. 2022; 11(3):571. https://doi.org/10.3390/jcm11030571
Chicago/Turabian StyleMéndez-Bailón, Manuel, Noel Lorenzo-Villalba, Miriam Romero-Correa, Esther Guisado-Espartero, Juan González-Soler, Jessica Rugeles-Niño, Angel Sebastián-Leza, Luis Ceresuela-Eito, Verónica Romaní-Costa, Angustias Quesada-Simón, and et al. 2022. "Cancer Impacts Prognosis on Mortality in Patients with Acute Heart Failure: Analysis of the EPICTER Study" Journal of Clinical Medicine 11, no. 3: 571. https://doi.org/10.3390/jcm11030571
APA StyleMéndez-Bailón, M., Lorenzo-Villalba, N., Romero-Correa, M., Guisado-Espartero, E., González-Soler, J., Rugeles-Niño, J., Sebastián-Leza, A., Ceresuela-Eito, L., Romaní-Costa, V., Quesada-Simón, A., Soler-Rangel, L., Herrero-Domingo, A., Díez-García, L., Alcalá-Pedrajas, J., Villalonga-Comas, M., Andrès, E., Gudiñ-Aguirre, D., Formiga, F., Aramburu-Bodas, O., ... on behalf of EPICTER Study Group. (2022). Cancer Impacts Prognosis on Mortality in Patients with Acute Heart Failure: Analysis of the EPICTER Study. Journal of Clinical Medicine, 11(3), 571. https://doi.org/10.3390/jcm11030571








