Reflex Locomotion Therapy for Balance, Gait, and Fatigue Rehabilitation in Subjects with Multiple Sclerosis
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Sample Size Calculation
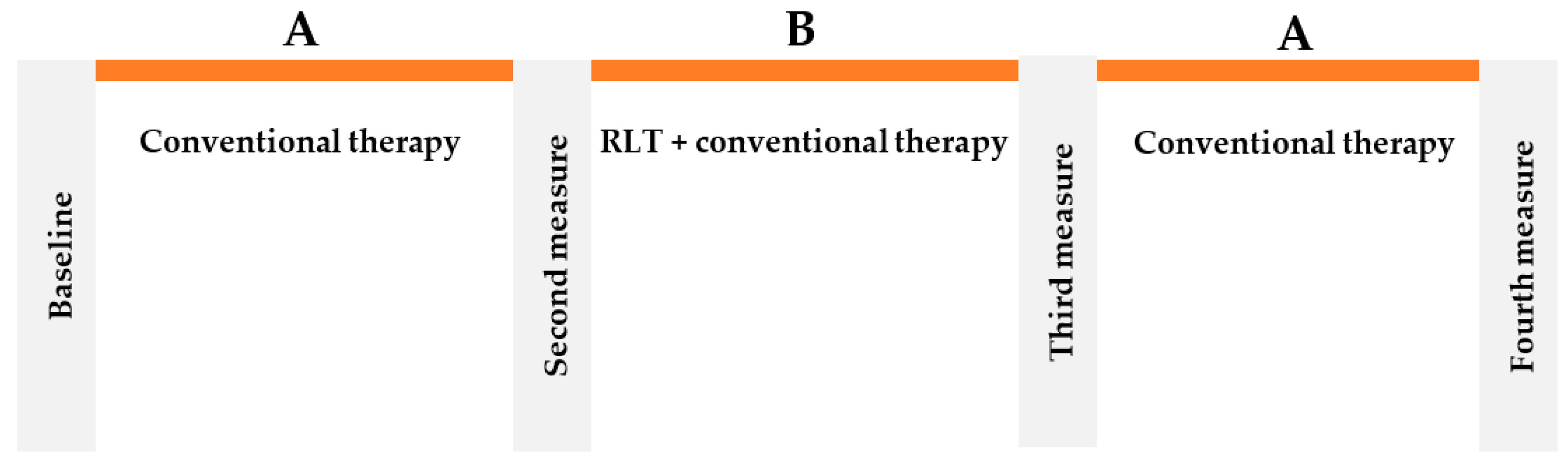
2.3. Study Procedure
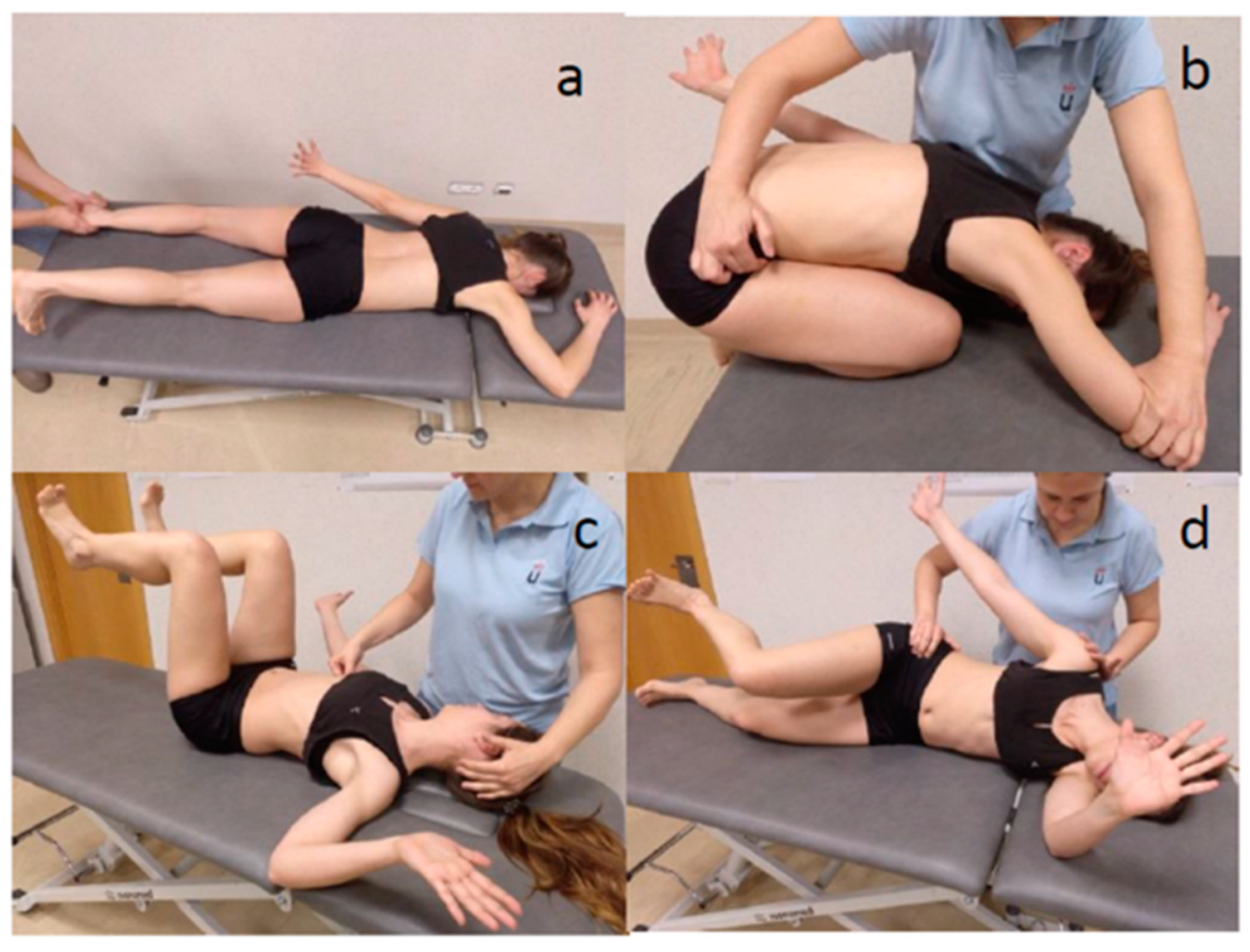
2.4. Intervention
2.5. Outcome Measures
2.5.1. Berg Balance Scale
2.5.2. Performance Oriented Mobility Assessment
2.5.3. Biomechanical Parameters
2.5.4. Assessment of Fatigue
2.5.5. Assessment of Satisfaction
2.5.6. Data Analysis
2.5.7. Statistical Analysis
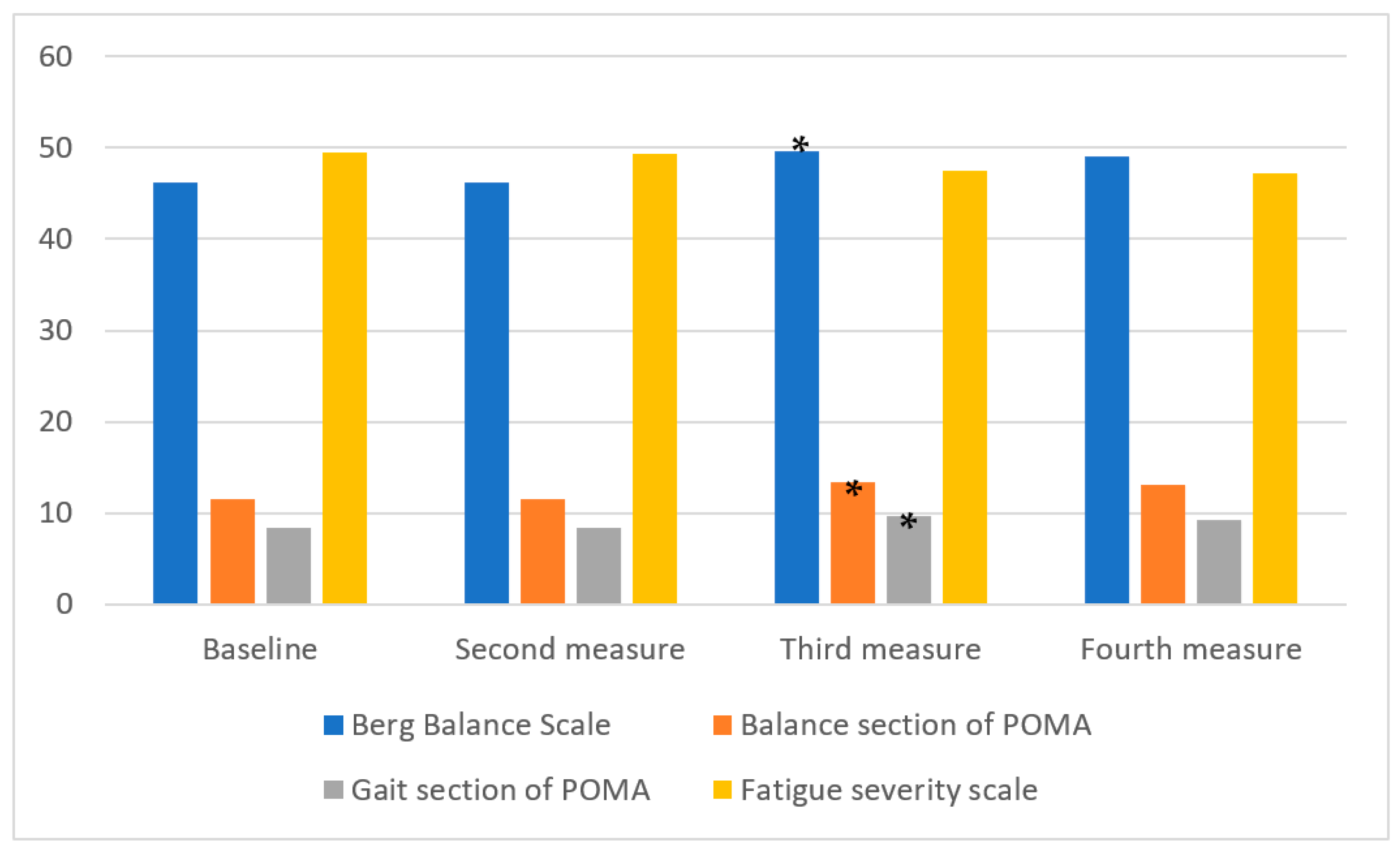
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fitzner, D.; Simons, M. Chronic Progressive Multiple Sclerosis—Pathogenesis of Neurodegeneration and Therapeutic Strategies. Curr. Neuropharmacol. 2010, 8, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Coca-Tapia, M.; Cuesta-Gómez, A.; Molina-Rueda, F.; Carratalá-Tejada, M. Gait Pattern in People with Multiple Sclerosis: A Systematic Review. Diagnostics 2021, 11, 584. [Google Scholar] [CrossRef] [PubMed]
- White, C.P.; White, M.B.; Russell, C.S. Invisible and visible symptoms of multiple sclerosis: Which are more predictive of health distress? J. Neurosci. Nurs. 2008, 40, 85–95, 102. [Google Scholar] [CrossRef] [PubMed]
- Zanghì, A.; Cimino, S.; Urzì, D.; Privitera, S.; Zagari, F.; Lanza, G.; Patti, F.; D’Amico, E. Pharmacotherapeutic management of lower urinary tract symptoms in Multiple Sclerosis patients. Expert Opin. Pharmacother. 2020, 21, 1449–1454. [Google Scholar] [CrossRef] [PubMed]
- Finlayson, M.L.; Peterson, E.W.; Cho, C. Risk factors for falling among people aged 45 to 90 with MS. Arch. Phys. Med. Rehabil. 2006, 87, 1274–1279. [Google Scholar] [CrossRef] [PubMed]
- Kesselring, J.; Beer, S. Symptomatic therapy and neurorehabilitation in multiple sclerosis. Lancet Neurol. 2005, 4, 643–652. [Google Scholar] [CrossRef]
- Rasova, K.; Feys, P.; Henze, T. Emerging evidence-based physical rehabilitation for multiple sclerosis—Towards an inventory of current content across Europe. Health Qual. Life Outcomes 2010, 8, 76. [Google Scholar] [CrossRef]
- Lord, S.E.; Wade, D.T.; Halligan, P.W. A comparison of two physiotherapy treatment approaches to improve walking in multiple sclerosis: A pilot randomized controlled study. Clin. Rehabil. 1998, 12, 477–486. [Google Scholar] [CrossRef]
- Pavlikova, M.; Cattaneo, D.; Jonsdottir, J.; Gervasoni, E.; Stetkarova, I.; Angelova, G.; Markova, M.; Prochazkova, M.; Prokopiusova, T.; Hruskova, N.; et al. The impact of balance specific physiotherapy, intensity of therapy and disability on static and dynamic balance in people with multiple sclerosis: A multi-center prospective study. Mult. Scler. Relat. Disord. 2020, 40, 101974. [Google Scholar] [CrossRef]
- Hok, P.; Opavský, J.; Kutín, M.; Tüdös, Z.; Kaňovský, P.; Hluštík, P. Modulation of the sensorimotor system by sustained manual pressure stimulation. Neuroscience 2017, 348, 11–22. [Google Scholar] [CrossRef]
- Sanz-Esteban, I.; Cano-de-la-Cuerda, R.; San-Martín-Gómez, A.; Jiménez-Antona, C.; Monge-Pereira, E.; Estrada-Barranco, C.; Serrano, J.I. Cortical activity during sensorial tactile stimulation in healthy adults through Vojta therapy. A randomized pilot controlled trial. J. Neuroeng. Rehabil. 2021, 18, 13. [Google Scholar] [CrossRef] [PubMed]
- Sanz-Esteban, I.; Cano-de-la-Cuerda, R.; San-Martin-Gomez, A.; Jimenez-Antona, C.; Monge-Pereira, E.; Estrada-Barranco, C.; Garcia-Sanchez, P.C.; Serrano, J.I. Innate Muscle Patterns Reproduction During Afferent Somatosensory Input With Vojta Therapy in Healthy Adults. A Randomized Controlled Trial. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 2232–2241. [Google Scholar] [CrossRef] [PubMed]
- Laufens, G.; Poltz, E.; Reimann, G.; Schmiegelt, F. Treadmill training and immediate effects. Phys. Med. Rehab. Kuror. 1998, 6, 174–177. [Google Scholar] [CrossRef]
- Laufens, G.; Poltz, W.; Prinz, E.; Reimann, G.; Schmiegelt, F. Alternating treadmill-Vojta-Treadmill-therapy in patients with multiple sclerosis with severely affected gait. Phys. Med. Rehab. Kuror. 2004, 31, 151–156. [Google Scholar]
- Perales Lopez, L.; Valdez Palmero, N.; Garcia Ruano, L.; San Leon Pascual, C.; White Orile, P.; Vegue Down, A.; Gor Garcia-Fogeda, M.D.; Toré, S. The implementation of a reflex locomotion program according to Vojta produces short-term automatic postural control changes in patients with multiple sclerosis. J. Bodyw. Mov. Ther. 2021, 26, 401–405. [Google Scholar] [CrossRef] [PubMed]
- Laufens, G.; Poltz, W.; Prinz, E.; Reimann, G.; Schmiegelt, F. Improvement in locomotion by combined treadmill/Vojta physiotherapy applied to selected MS patients. Phys. Med. Rehab. Kuror. 1999, 9, 187–189. [Google Scholar] [CrossRef]
- Polman, C.H.; Reingold, S.C.; Banwell, B.; Clanet, M.; Cohen, J.A.; Filippi, M.; Fujihara, K.; Havrdova, E.; Hutchinson, M.; Kappos, L.; et al. Diagnostic criteria for multiple sclerosis: 2010 Revisions to the McDonald criteria. Ann. Neurol 2011, 69, 292–302. [Google Scholar] [CrossRef]
- Davis, R.B.; Ounpuu, S.; Tyburski, D.; Gage, J.R. A gait analysis data collection and reduction technique. Hum. Mot. Sci. 1991, 10, 575–587. [Google Scholar] [CrossRef]
- Kadaba, M.P.; Ramakrishnan, H.K.; Wootten, M.E. Measurement of lower extremity kinematics during level walking. J. Orthop. Res. 1990, 8, 383–392. [Google Scholar] [CrossRef]
- Vojta, V. El Principio Vojta; Spriger: Barcelona, Spain, 1995. [Google Scholar]
- Berg, K.; Wood-Dauphine, S.; Williams, J.I.; Gayton, D. Measuring balance in the elderly: Preliminary development of an instrument. Physiother. Can. 1989, 41, 304–311. [Google Scholar] [CrossRef]
- Cattaneo, D.; Regola, A.; Meotti, M. Validity of six balance disorders scales in persons with multiple sclerosis. Disabil. Rehabil. 2006, 28, 789–795. [Google Scholar] [CrossRef] [PubMed]
- Cattaneo, D.; Jonsdottir, J.; Repetti, S. Reliability of four scales on balance disorders in persons with multiple sclerosis. Disabil. Rehabil. 2007, 29, 1920–1925. [Google Scholar] [CrossRef] [PubMed]
- Nilsagård, Y.; Lundholm, C.; Denison, E.; Gunnarsson, L.G. Predicting accidental falls in people with multiple sclerosis—a longitudinal study. Clin. Rehabil. 2009, 23, 259–269. [Google Scholar] [CrossRef]
- Tinetti, M.E. Performance-oriented assessment of mobility problems in elderly patients. J. Am. Geriatr. Soc. 1986, 34, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Soyuer, F.; Mirza, M.; Erkorkmaz, Ü. Balance performance in three forms of multiple sclerosis. Neurol. Res. 2006, 28, 555–562. [Google Scholar] [CrossRef]
- Tesio, L.; Perucca, L.; Franchignoni, F.P.; Battaglia, M.A. A short measure of balance in multiple sclerosis: Validation through Rasch analysis. Funct. Neurol. 1997, 12, 255–268. [Google Scholar]
- Mills, R.J.; Young, C.A.; Nicholas, R.S.; Pallant, J.F.; Tennant, A. Rasch analysis of the Fatigue Severity Scale in multiple sclerosis. Mult. Scler. 2009, 15, 81–87. [Google Scholar] [CrossRef]
- Roberts, R.E.; Atrkisson, C.C.; Mendias, R.M. Assessing the client satisfaction questionnaire in English and Spanish. Hisp. J. Behav. Sci. 1984, 6, 385–396. [Google Scholar] [CrossRef]
- Vicon Plug-in Gait Product Guide-Foundation Notes Revision 2.0. March 2010.
- Molina-Rueda, F.; Alguacil-Diego, I.M.; Cuesta-Gómez, A.; Iglesias-Giménez, J.; Martín-Vivaldi, A.; Miangolarra-Page, J.C. Thorax, pelvis and hip pattern in the frontal plane during walking in unilateral transtibial amputees: Biomechanical analysis. Braz. J. Phys. Ther. 2014, 18, 252–258. [Google Scholar] [CrossRef][Green Version]
- Belda-Lois, J.M.; Mena-del Horno, S.; Bermejo-Bosch, I.; Moreno, J.C.; Pons, J.L.; Farina, D.; Iosa, M.; Molinari, M.; Tamburella, F.; Ramos-Murguialday, A.; et al. Rehabilitation of gait after stroke: A review towards a top-down approach. J. Neuroeng. Rehabil. 2011, 8, 66. [Google Scholar] [CrossRef] [PubMed]
- Cameron, M.H.; Nilsagard, Y. Balance, gait, and falls in multiple sclerosis. Handb. Clin. Neurol. 2018, 159, 237–250. [Google Scholar] [PubMed]
- Guner, S.; Inanici, F. Yoga therapy and ambulatory multiple sclerosis Assessment of gait analysis parameters, fatigue and balance. J. Bodyw. Mov. Ther. 2015, 19, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Benedetti, M.G.; Riperno, R.; Simoncini, L.; Bonato, P.; Tonini, A.; Giannini, S. Gait abnormalities in minimally impaired multiple sclerosis patients. Mult. Scler. 1999, 5, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Preiningerova, J.L.; Novotna, K.; Rusz, J.; Sucha, L.; Ruzicka, E.; Havrdova, E. Spatial and temporal characteristics of gait as outcome measures in multiple sclerosis (EDSS 0 to 6.5). J. Neuroeng. Rehabil. 2015, 12, 14. [Google Scholar] [CrossRef]
- McGinley, J.L.; Baker, R.; Wolfe, R.; Morris, M.E. The reliability of three-dimensional kinematic gait measurements: A systematic review. Gait Posture 2009, 29, 360–369. [Google Scholar] [CrossRef]
- Filli, L.; Sutter, T.; Easthope, C.S.; Killeen, T.; Meyer, C.; Reuter, K.; Lörincz, L.; Bolliger, M.; Weller, M.; Curt, A.; et al. Profiling walking dysfunction in multiple sclerosis: Characterisation, classification and progression over time. Sci. Rep. 2018, 8, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Pavlu, D.; Véle, F.; Havlickova, L. Electromyography and kinesiological analysis of Vojta’s therapeutical princip. Rehab. Fyzil. 2000, 7, 34–39. [Google Scholar]
- Sung, H. Effects of Vojta method on trunk stability in healthy individuals. J. Exerc. Rehabil. 2016, 12, 542–547. [Google Scholar]
- Husárová, R. The vojta approach in adult patients. Rehabilitacia 2005, 42, 38–43. [Google Scholar]
- Perales, L.; Pérez, A.M.; Atín, M.A.; Varela, E. Efecto de la terapia Vojta en la rehabilitación de la marcha en dos pacientes adultos con daño cerebral adquirido en fase tardía. Fisioterapia 2009, 31, 151–162. [Google Scholar] [CrossRef]
- Epple, C.; Maurer-Burkhard, B.; Lichti, M.-C.; Steiner, T. Vojta therapy improves postural control in very early stroke rehabilitation: A randomised controlled pilot trial. Neurol. Res. Pract. 2020, 2, 4. [Google Scholar] [CrossRef] [PubMed]
| Variable | Subjects | ||
|---|---|---|---|
| Age (years) * | 44.39 (7.37) | ||
| Sex | ♀ 73.91% (n = 17) | ♂ 26.08% (n = 6) | |
| Most affected side | Right 43.48% (n = 10) | Left 56.56% (n = 13) | |
| Years since diagnosis * | 14.39 (5.85) | ||
| Type of MS | RRMS 56.52% (n = 13) | SPMS 21.73% (n = 5) | PPMS 21.73% (n = 5) |
| Mean (SD) | Second vs. Baseline Measurement | Third vs. Second Measurement | Fourth vs. Third Measurement | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Second Measure | Third Measure | Fourth Measure | DM | p | CI 95% | DM | p | CI 95% | DM | p | CI 95% | |
| Berg Balance Scale | 46.21 ± 7.24 | 46.13 ± 7.17 | 49.65 ± 5.56 | 49.08 ± 6.26 | −0.09 | 1.000 | −1.94 to 1.76 | 3.52 | <0.001 * | 1.67 to 5.37 | −0.57 | 1.000 | −2.41 to 1.28 |
| Balance section of POMA | 11.56 ± 2.51 | 11.47 ± 2.71 | 13.34 ± 2.08 | 13.13 ± 1.79 | −0.09 | 1.000 | −0.97 to 0.79 | 1.87 | <0.001 * | 0.99 to 2.75 | −0.22 | 1.000 | −1.10 to 0.66 |
| Gait section of POMA | 8.43 ± 2.33 | 8.39 ± 2.38 | 9.73 ± 1.98 | 9.30 ± 2.22 | −0.04 | 1.000 | −0.58 to 0.50 | 1.35 | <0.001 * | 0.81 to 1.89 | −0.43 | 0.190 | −0.97 to 0.10 |
| Fatigue severity scale | 49.52 ± 10.99 | 49.39 ± 11.69 | 47.47 ± 10.08 | 47.26 ± 11.33 | −0.13 | 1.000 | −3.92 to 3.66 | −1.91 | 1.000 | −5.70 to 1.88 | −0.22 | 1.000 | −4.01 to 3.57 |
| Mean (SD) | Second vs. Baseline Measurement | Third vs. Second Measurement | Fourth vs. Third Measurement | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Second Measure | Third Measure | Fourth Measure | DM | p | CI 95% | DM | p | CI 95% | DM | p | CI 95% | |
| Stride length | 0.98 ± 0.23 | 0.98 ± 0.24 | 1.09 ± 0.23 | 1.08 ± 0.21 | −0.0012 | 1.000 | −0.07 to 0.06 | 0.113 | <0.01 * | 0.05 to 0.18 | −0.01 | 1.00 | −0.08 to 0.05 |
| Single support | 0.47 ± 0.08 | 0.47 ± 0.08 | 0.46 ± 0.10 | 0.48 ± 0.11 | −0.0002 | 1.000 | −0.03 to 0.03 | −0.004 | 1.00 | −0.03 to 0.02 | 0.02 | 0.70 | −0.01 to 0.04 |
| Double support | 0.43 ± 0.26 | 0.43 ± 0.26 | 0.37 ± 0.21 | 0.41 ± 0.32 | −0.0070 | 1.000 | −0.07 to 0.05 | −0.059 | 0.047 * | −0.12 to −0.0004 | 0.04 | 0.30 | −0.02 to 0.10 |
| Velocity | 0.77 ± 0.24 | 0.76 ± 0.26 | 0.88 ± 0.29 | 0.86 ± 0.28 | −0.0049 | 1.000 | −0.08 to 0.07 | 0.114 | 0.001 * | 0.04 to 0.19 | −0.02 | 1.00 | −0.09 to 0.06 |
| Kinematic (Degrees) | Mean (SD) | Second vs. Baseline Measurement | Third vs. Second Measurement | Fourth vs. Third Measurement | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Second Measure | Third Measure | Fourth Measure | DM | p | CI 95% | DM | p | CI 95% | DM | p | CI 95% | |
| Hip ROM | 40.18 ± 8.21 | 40.25 ± 8.28 | 42.92 ± 6.69 | 43.20 ± 7.28 | 0.07 | 1.00 | −2.03 to 2.18 | 2.66 | 0.006 * | 0.56 to 4.77 | 0.28 | 1.00 | −1.82 to 2.39 |
| Hip angle at IC | 30.75 ± 8.93 | 30.55 ± 8.89 | 32.07 ± 8.10 | 31.98 ± 8.38 | −0.20 | 1.00 | −2.54 to 2.14 | 1.52 | 0.47 | −0.83 to 3.86 | −0.24 | 1.00 | −2.601 to 2.13 |
| Peak hip extension stance period | −7.13 ± 9.69 | −7.48 ± 10.04 | −8.44 ± 8.97 | −8.75 ± 7.56 | −0.35 | 1.00 | −3.16 to 2.46 | −0.95 | 1.00 | −3.76 to 1.86 | 0.60 | 1.00 | −2.35 to 3.56 |
| Peak hip flexion swing period | 32.70 ± 9.12 | 32.42 ± 9.16 | 34.08 ± 8.45 | 34.18 ± 8.30 | −0.28 | 1.00 | −3.10 to 2.53 | 1.67 | 0.67 | −1.15 to 4.48 | −0.06 | 1.00 | −2.91 to 2.78 |
| Knee ROM | 49.80 ± 4.18 | 49.74 ± 14.08 | 52.75 ± 12.18 | 51.79 ± 11.50 | −0.06 | 1.00 | −3.47 to 3.36 | 3.01 | 0.045 * | −0.40 to 6.43 | −0.97 | 1.00 | −4.38 to 2.45 |
| Knee angle at IC | 6.53 ± 8.32 | 6.35 ± 8.43 | 3.94 ± 7.69 | 4.78 ± 7.09 | −0.19 | 1.00 | −2.65 to 2.28 | −2.23 | 0.097 | −4.70 to 0.23 | 0.67 | 1.00 | −1.80 to 3.14 |
| Peak knee flexion swing period | 50.04 ± 3.21 | 49.77 ± 13.08 | 49.66 ± 11.95 | 49.38 ± 11.32 | −0.27 | 1.00 | −4.20 to 3.65 | −0.11 | 1.00 | −4.03 to 3.82 | −0.28 | 1.00 | −4.20 to 3.65 |
| Ankle ROM | 26.94 ± 9.82 | 25.69 ± 7.11 | 26.00± 6.73 | 26.12 ± 5.19 | −1.25 | 1.00 | 4.38 to 1.89 | 0.31 | 1.00 | −2.83 to 3.44 | 0.12 | 1.00 | −3.02 to 3.25 |
| Ankle angle at IC | 2.31 ± 6.64 | 1.85 ± 6.81 | 2.55 ± 5.63 | 2.65 ± 7.34 | −0.46 | 1.00 | −1.91 to 0.98 | 0.70 | 1.00 | −0.74 to 2.15 | 0.10 | 1.00 | −1.35 to 1.54 |
| Peak ankle plantar flexion toe-off (º) | −3.14 ± 12.26 | −2.05 ± 9.84 | −3.03 ± 8.61 | −3.30 ± 9.61 | 1.10 | 1.00 | −1.41 to 3.60 | −0.98 | 1.00 | −3.49 to 1.52 | −0.27 | 1.00 | −2.77 to 2.23 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carratalá-Tejada, M.; Cuesta-Gómez, A.; Ortiz-Gutiérrez, R.; Molina-Rueda, F.; Luna-Oliva, L.; Miangolarra-Page, J.C. Reflex Locomotion Therapy for Balance, Gait, and Fatigue Rehabilitation in Subjects with Multiple Sclerosis. J. Clin. Med. 2022, 11, 567. https://doi.org/10.3390/jcm11030567
Carratalá-Tejada M, Cuesta-Gómez A, Ortiz-Gutiérrez R, Molina-Rueda F, Luna-Oliva L, Miangolarra-Page JC. Reflex Locomotion Therapy for Balance, Gait, and Fatigue Rehabilitation in Subjects with Multiple Sclerosis. Journal of Clinical Medicine. 2022; 11(3):567. https://doi.org/10.3390/jcm11030567
Chicago/Turabian StyleCarratalá-Tejada, María, Alicia Cuesta-Gómez, Rosa Ortiz-Gutiérrez, Francisco Molina-Rueda, Laura Luna-Oliva, and Juan Carlos Miangolarra-Page. 2022. "Reflex Locomotion Therapy for Balance, Gait, and Fatigue Rehabilitation in Subjects with Multiple Sclerosis" Journal of Clinical Medicine 11, no. 3: 567. https://doi.org/10.3390/jcm11030567
APA StyleCarratalá-Tejada, M., Cuesta-Gómez, A., Ortiz-Gutiérrez, R., Molina-Rueda, F., Luna-Oliva, L., & Miangolarra-Page, J. C. (2022). Reflex Locomotion Therapy for Balance, Gait, and Fatigue Rehabilitation in Subjects with Multiple Sclerosis. Journal of Clinical Medicine, 11(3), 567. https://doi.org/10.3390/jcm11030567








