How Long to Continue Eyelid Hygiene to Treat Meibomian Gland Dysfunction
Abstract
:1. Introduction
2. Methods
2.1. Participants and Study Design
2.2. Meibomian Gland Dysfunction and Dry Eye Assessments
2.3. Therapeutic Interventions
2.4. Statistical Analysis
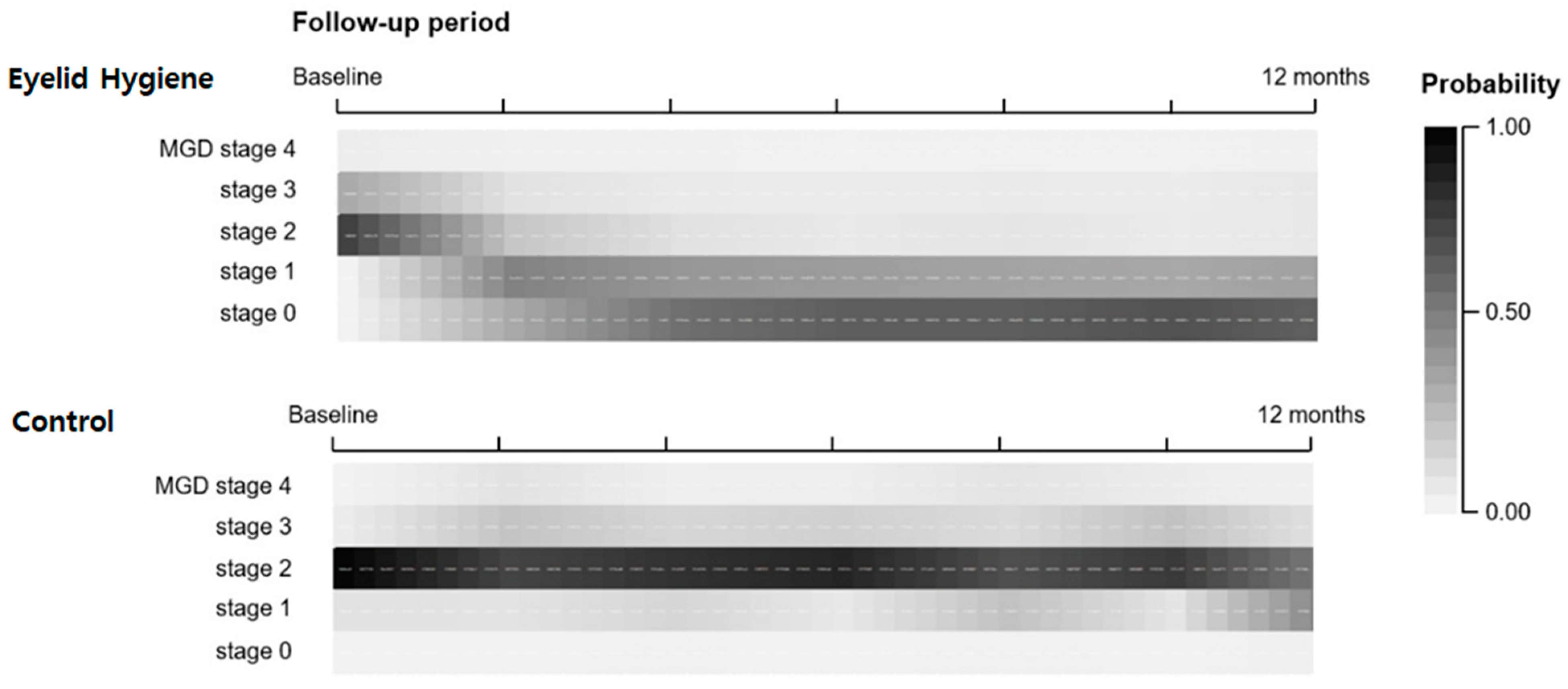
3. Results
Efficacy of Eyelid Hygiene and Factors Affecting the MGD Stage
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Tomlinson, A.; Bron, A.J.; Korb, D.R.; Amano, S.; Paugh, J.R.; Pearce, E.I.; Yee, R.; Yokoi, N.; Arita, R.; Dogru, M. The international workshop on meibomian gland dysfunction: Report of the diagnosis subcommittee. Investig. Ophthalmol. Vis. Sci. 2011, 52, 2006–2049. [Google Scholar] [CrossRef]
- Shimazaki, J.; Sakata, M.; Tsubota, K. Ocular surface changes and discomfort in patients with meibomian gland dysfunction. Arch. Ophthalmol. 1995, 113, 1266–1270. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Oh, D.H.; Jung, J.Y.; Kim, J.C.; Jeon, C.O. Comparative ocular microbial communities in humans with and without blepharitis. Investig. Ophthalmol. Vis. Sci. 2012, 53, 5585–5593. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mizoguchi, S.; Iwanishi, H.; Arita, R.; Shirai, K.; Sumioka, T.; Kokado, M.; Jester, J.V.; Saika, S. Ocular surface inflammation impairs structure and function of meibomian gland. Exp. Eye Res. 2017, 163, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Craig, J.P.; Nichols, K.K.; Akpek, E.K.; Caffery, B.; Dua, H.S.; Joo, C.-K.; Liu, Z.; Nelson, J.D.; Nichols, J.J.; Tsubota, K. TFOS DEWS II definition and classification report. Ocul. Surf. 2017, 15, 276–283. [Google Scholar] [CrossRef]
- Baudouin, C.; Messmer, E.M.; Aragona, P.; Geerling, G.; Akova, Y.A.; Benítez-del-Castillo, J.; Boboridis, K.G.; Merayo-Lloves, J.; Rolando, M.; Labetoulle, M. Revisiting the vicious circle of dry eye disease: A focus on the pathophysiology of meibomian gland dysfunction. Br. J. Ophthalmol. 2016, 100, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Nichols, K.K.; Foulks, G.N.; Bron, A.J.; Glasgow, B.J.; Dogru, M.; Tsubota, K.; Lemp, M.A.; Sullivan, D.A. The international workshop on meibomian gland dysfunction: Executive summary. Investig. Ophthalmol. Vis. Sci. 2011, 52, 1922–1929. [Google Scholar] [CrossRef] [Green Version]
- Jones, L.; Downie, L.E.; Korb, D.; Benitez-del-Castillo, J.M.; Dana, R.; Deng, S.X.; Dong, P.N.; Geerling, G.; Hida, R.Y.; Liu, Y. TFOS DEWS II management and therapy report. Ocul. Surf. 2017, 15, 575–628. [Google Scholar] [CrossRef]
- Benitez-del-Castillo, J.M. How to promote and preserve eyelid health. Clin. Ophthalmol. 2012, 6, 1689. [Google Scholar] [CrossRef] [Green Version]
- Romero, J.M.; Biser, S.A.; Perry, H.D.; Levinson, D.H.; Doshi, S.J.; Terraciano, A.; Donnenfeld, E.D. Conservative treatment of meibomian gland dysfunction. Eye Contact Lens 2004, 30, 14–19. [Google Scholar] [CrossRef]
- Guillon, M.; Maissa, C.; Wong, S. Eyelid margin modification associated with eyelid hygiene in anterior blepharitis and meibomian gland dysfunction. Eye Contact Lens 2012, 38, 319–325. [Google Scholar] [CrossRef]
- Matsumoto, Y.; Shigeno, Y.; Sato, E.A.; Ibrahim, O.M.; Saiki, M.; Negishi, K.; Ogawa, Y.; Dogru, M.; Tsubota, K. The evaluation of the treatment response in obstructive meibomian gland disease by in vivo laser confocal microscopy. Graefe’s Arch. Clin. Exp. Ophthalmol. 2009, 247, 821–829. [Google Scholar] [CrossRef]
- Pinna, A.; Piccinini, P.; Carta, F. Effect of oral linoleic and γ-linolenic acid on meibomian gland dysfunction. Cornea 2007, 26, 260–264. [Google Scholar] [CrossRef] [PubMed]
- Arita, R.; Itoh, K.; Maeda, S.; Maeda, K.; Furuta, A.; Fukuoka, S.; Tomidokoro, A.; Amano, S. Proposed diagnostic criteria for obstructive meibomian gland dysfunction. Ophthalmology 2009, 116, 2058–2063.e2051. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.; Adil, M.Y.; Chen, X.; Utheim, Ø.A.; Ræder, S.; Tønseth, K.A.; Lagali, N.S.; Dartt, D.A.; Utheim, T.P. Functional and morphological evaluation of meibomian glands in the assessment of meibomian gland dysfunction subtype and severity. Am. J. Ophthalmol. 2020, 209, 160–167. [Google Scholar] [CrossRef] [Green Version]
- Schiffman, R.M.; Christianson, M.D.; Jacobsen, G.; Hirsch, J.D.; Reis, B.L. Reliability and validity of the ocular surface disease index. Arch. Ophthalmol. 2000, 118, 615–621. [Google Scholar] [CrossRef]
- Whitcher, J.P.; Shiboski, C.H.; Shiboski, S.C.; Heidenreich, A.M.; Kitagawa, K.; Zhang, S.; Hamann, S.; Larkin, G.; McNamara, N.A.; Greenspan, J.S. A simplified quantitative method for assessing keratoconjunctivitis sicca from the Sjögren’s Syndrome International Registry. Am. J. Ophthalmol. 2010, 149, 405–415. [Google Scholar] [CrossRef] [Green Version]
- Efron, N. Grading scales for contact lens complications. Ophthalmic Physiol. Opt. 1998, 18, 182–186. [Google Scholar] [CrossRef]
- Bitton, E.; Ngo, W.; Dupont, P. Eyelid hygiene products: A scoping review. Contact Lens Anterior Eye 2019, 42, 591–597. [Google Scholar] [CrossRef]
- Geerling, G.; Tauber, J.; Baudouin, C.; Goto, E.; Matsumoto, Y.; O’Brien, T.; Rolando, M.; Tsubota, K.; Nichols, K.K. The international workshop on meibomian gland dysfunction: Report of the subcommittee on management and treatment of meibomian gland dysfunction. Investig. Ophthalmol. Vis. Sci. 2011, 52, 2050–2064. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perry, H.D.; Doshi-Carnevale, S.; Donnenfeld, E.D.; Solomon, R.; Biser, S.A.; Bloom, A.H. Efficacy of commercially available topical cyclosporine A 0.05% in the treatment of meibomian gland dysfunction. Cornea 2006, 25, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Prabhasawat, P.; Tesavibul, N.; Mahawong, W. A randomized double-masked study of 0.05% cyclosporine ophthalmic emulsion in the treatment of meibomian gland dysfunction. Cornea 2012, 31, 1386–1393. [Google Scholar] [CrossRef] [PubMed]
- Byun, Y.-j.; Kwon, S.M.; Seo, K.Y.; Kim, S.W.; Kim, E.K.; Park, W.C. Efficacy of combined 0.05% cyclosporine and 1% methylprednisolone treatment for chronic dry eye. Cornea 2012, 31, 509–513. [Google Scholar] [CrossRef]
- Lee, H.; Chung, B.; Kim, K.S.; Seo, K.Y.; Choi, B.J. Effects of topical loteprednol etabonate on tear cytokines and clinical outcomes in moderate and severe meibomian gland dysfunction: Randomized clinical trial. Am. J. Ophthalmol. 2014, 158, 1172–1183.e1171. [Google Scholar] [CrossRef]
- Ma, X.; Lu, Y. Efficacy of intraductal meibomian gland probing on tear function in patients with obstructive meibomian gland dysfunction. Cornea 2016, 35, 725–730. [Google Scholar] [CrossRef]
- Kasetsuwan, N.; Suwajanakorn, D.; Tantipat, C.; Reinprayoon, U. The Efficacy Between Conventional Lid Hygiene and Additional Thermal Pulsatile System in Meibomian Gland Dysfunction Patients Treated with Long-Term Anti-Glaucoma Medications in a Randomized Controlled Trial. Clin. Ophthalmol. 2020, 14, 2891. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, Y.A.; Camp, A.; Feuer, W.; Karp, C.L.; Wellik, S.; Galor, A. Compliance and subjective patient responses to eyelid hygiene. Eye Contact Lens 2017, 43, 213. [Google Scholar] [CrossRef]
| Initial 2-Month Compliance Group of Eyelid Hygiene | ||||
|---|---|---|---|---|
| Total (N = 1015) | Eyelid Hygiene (N = 543) | Control (N = 485) | p | |
| Age (Mean ± SD) | 38.7 ± 16.8 | 38.6 ± 16.5 | 38.8 ± 17.0 | 0.848 |
| Sex (% of male) | 72.1 | 75.6 | 74.2 | 0.462 |
| Ocular surface inflammation (%) | 69.2 | 67.4 | 71.2 | 0.196 |
| Anti-inflammatory treatment (%) | 58.0 | 57.3 | 58.8 | 0.629 |
| MGD parameters | ||||
| MGD subtype (%) | 0.069 | |||
| High-secretory high-quality | 39.9 | 39.1 | 40.9 | - |
| High-secretory low-quality | 33.0 | 34.6 | 31.1 | - |
| Low-secretory high-quality | 7.6 | 5.8 | 9.7 | - |
| Low-secretory low-quality | 19.5 | 20.5 | 18.3 | - |
| MGD stage (%) | 0.400 | |||
| Stage 0 | 5.8 | 5.6 | 6.0 | - |
| Stage 1 | 27.3 | 26.3 | 28.4 | - |
| Stage 2 | 35.3 | 34.2 | 36.6 | - |
| Stage 3 | 23.9 | 26.4 | 21.1 | - |
| Stage 4 | 7.7 | 7.5 | 8.0 | - |
| DED parameters | ||||
| OSDI scores (0–100) | 17.7 ± 9.9 | 17.4 ± 10.1 | 18.0 ± 9.6 | 0.331 |
| FTBUT (seconds) | 7.4 ± 3.1 | 7.5 ± 3.2 | 7.2 ± 3.0 | 0.123 |
| Schirmer I test (mm) | 11.4 ± 4.3 | 11.4 ± 4.4 | 11.2 ± 4.0 | 0.448 |
| Corneal staining score (%) | 0.479 | |||
| Score 0 | 21.9 | 23.2 | 20.4 | - |
| Score 1 | 41.7 | 39.7 | 44.0 | - |
| Score 2 | 21.5 | 22.4 | 20.5 | - |
| Score 3 | 14.9 | 14.7 | 15.1 | - |
| 95% CI | ||||
|---|---|---|---|---|
| Estimate β | Lower | Upper | p | |
| Fixed effects | ||||
| Treatment group | ||||
| Eyelid Hygiene | 0.717 | 0.694 | 0.741 | <0.001 * |
| Control | Reference | |||
| Follow-up (FU) period (each 2-month) | 0.715 | 0.691 | 0.740 | <0.001 * |
| Interaction between the groups and FU period | ||||
| Eyelid Hygiene | 0.764 | 0.747 | 0.783 | <0.001 * |
| Control | Reference | |||
| Age | 1.015 | 1.011 | 1.018 | <0.001 * |
| Sex | ||||
| Male | 0.968 | 0.862 | 1.082 | 0.560 |
| Female | Reference | |||
| Ocular surface Inflammation | ||||
| Present | 1.298 | 1.141 | 1.449 | <0.001 * |
| Absent | Reference | |||
| Anti-inflammatory treatments | ||||
| Performed | 0.946 | 0.904 | 0.991 | 0.001 * |
| Not performed | Reference | |||
| MGD subtype, baseline | <0.001 * | |||
| Low-secretory low-quality | 8.174 | 6.959 | 9.602 | <0.001 * |
| Low-secretory high-quality | 4.646 | 4.263 | 5.568 | <0.001 * |
| High-secretory low-quality | 2.852 | 2.316 | 3.532 | <0.001 * |
| High-secretory high-quality | Reference | |||
| Threshold | ||||
| MGD stage 4 | 55.257 | 43.948 | 77.478 | <0.001 * |
| MGD stage 3 | 22.874 | 18.616 | 28.361 | <0.001 * |
| MGD stage 2 | 9.885 | 8.240 | 11.882 | <0.001 * |
| MGD stage 1 | 1.474 | 1.244 | 1.751 | <0.001 * |
| MGD stage 0 | Reference | |||
| Treatment Duration | ||||||
|---|---|---|---|---|---|---|
| Eyelid hygiene Group | 2 months | 4 months | 6 months | 8 months | 10 months | 12 months |
| vs. baseline | vs. 2 months | vs. 4 months | vs. 6 months | vs. 8 months | vs. 10 months | |
| Estimate ß | 0.180 | 0.700 | 0.699 | 1.130 | 0.871 | 1.060 |
| p-value | <0.001 * | 0.002 * | 0.004 * | 0.345 | 0.312 | 0.610 |
| Withdrawal Period | ||||||
|---|---|---|---|---|---|---|
| Withdrawal Group | Baseline | 2 months | 4 months | 6 months | 8 months | 10 months |
| vs. Control Group | ||||||
| Estimate ß | 0.255 | 0.460 | 0.890 | 0.904 | 1.065 | 1.081 |
| p-value | <0.001 * | 0.001 * | 0.665 | 0.775 | 0.880 | 0.954 |
| vs. Eyelid hygiene Group | ||||||
| Estimate ß | 0.900 | 1.656 | 5.112 | 5.284 | 5.212 | 5.171 |
| p-value | 0.712 | 0.122 | <0.001 * | <0.001 * | <0.001 * | <0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahn, H.; Kim, B.Y.; Kim, J.; Ji, Y.W.; Jun, I.; Kim, T.-i.; Lee, H.K.; Seo, K.Y. How Long to Continue Eyelid Hygiene to Treat Meibomian Gland Dysfunction. J. Clin. Med. 2022, 11, 529. https://doi.org/10.3390/jcm11030529
Ahn H, Kim BY, Kim J, Ji YW, Jun I, Kim T-i, Lee HK, Seo KY. How Long to Continue Eyelid Hygiene to Treat Meibomian Gland Dysfunction. Journal of Clinical Medicine. 2022; 11(3):529. https://doi.org/10.3390/jcm11030529
Chicago/Turabian StyleAhn, Hyunmin, Bo Yi Kim, Jinyoung Kim, Yong Woo Ji, Ikhyun Jun, Tae-im Kim, Hyung Keun Lee, and Kyoung Yul Seo. 2022. "How Long to Continue Eyelid Hygiene to Treat Meibomian Gland Dysfunction" Journal of Clinical Medicine 11, no. 3: 529. https://doi.org/10.3390/jcm11030529
APA StyleAhn, H., Kim, B. Y., Kim, J., Ji, Y. W., Jun, I., Kim, T.-i., Lee, H. K., & Seo, K. Y. (2022). How Long to Continue Eyelid Hygiene to Treat Meibomian Gland Dysfunction. Journal of Clinical Medicine, 11(3), 529. https://doi.org/10.3390/jcm11030529







