Factors Associated with Dual-Fluency Walk Speed Improvement after Rehabilitation in Older Patients
Abstract
1. Introduction
2. Materials and Methods
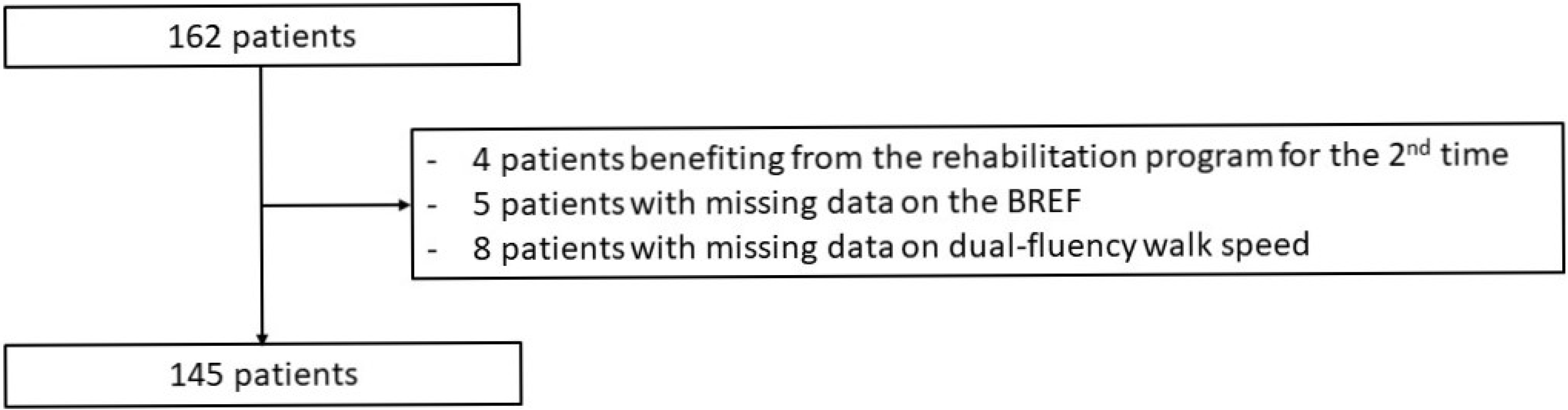
2.1. Study Population
2.2. Walk Assessment and Rehabilitation Program
2.3. Data Collection
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
3.1. Patient Characteristics
3.2. Factors Associated with an Increase in Dual-Task Walk Speed
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Middleton, A.; Fritz, S.L.; Lusardi, M. Walking speed: The functional vital sign. J. Aging Phys. Act. 2015, 23, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Hortobágyi, T.; Lesinski, M.; Gäbler, M.; VanSwearingen, J.M.; Malatesta, D.; Granacher, U. Effects of Three Types of Exercise Interventions on Healthy Old Adults’ Gait Speed: A Systematic Review and Meta-Analysis. Sports Med. 2015, 45, 1627–1643, Erratum in Sports Med. 2016, 46, 453. [Google Scholar] [CrossRef] [PubMed]
- Montero-Odasso, M.; van der Velde, N.; Martin, F.C.; Petrovic, M.; Tan, M.P.; Ryg, J.; Aguilar-Navarro, S.; Alexander, N.B.; Becker, C.; Blain, H.; et al. World guidelines for falls prevention and management for older adults: A global initiative. Age Ageing 2022, 51, afac205. [Google Scholar] [CrossRef] [PubMed]
- Lamoth, C.J.; van Deudekom, F.J.; van Campen, J.P.; Appels, B.A.; de Vries, O.J.; Pijnappels, M. Gait stability and variability measures show effects of impaired cognition and dual tasking in frail people. J. Neuroeng. Rehabil. 2011, 8, 2. [Google Scholar] [CrossRef] [PubMed]
- Lundin-Olsson, L.; Nyberg, L.; Gustafson, Y. “Stops walking when talking” as a predictor of falls in elderly people. Lancet 1997, 349, 617. [Google Scholar] [CrossRef]
- Ceïde, M.E.; Ayers, E.I.; Lipton, R.; Verghese, J. Walking While Talking and Risk of Incident Dementia. Am. J. Geriatr. Psychiatry 2018, 26, 580–588. [Google Scholar] [CrossRef]
- Verghese, J.; Buschke, H.; Viola, L.; Katz, M.; Hall, C.; Kuslansky, G.; Lipton, R. Validity of divided attention tasks in predicting falls in older individuals: A preliminary study. J. Am. Geriatr. Soc. 2002, 50, 1572–1576. [Google Scholar] [CrossRef]
- Beauchet, O.; Annweiler, C.; Dubost, V.; Allali, G.; Kressig, R.W.; Bridenbaugh, S.; Berrut, G.; Assal, F.; Herrmann, F. Stops walking when talking: A predictor of falls in older adults? Eur. J. Neurol. 2009, 16, 786–795. [Google Scholar] [CrossRef]
- Koskas, P.; Lagadec, J.; Stirati, S.; Drunat, O.; Wolmark, Y. Intérêt de l’analyse de la sémiologie et de la vitesse de marche du sujet âgé dans l’évaluation du risque de chute à l’aide d’un parcours de marche comportant une double tâche. J. Réadapt. Méd. 2007, 27, 13–20. [Google Scholar] [CrossRef]
- Toulotte, C.; Thevenon, A.; Watelain, E.; Fabre, C. Identification of healthy elderly fallers and non-fallers by gait analysis under dual-task conditions. Clin. Rehabil. 2006, 20, 269–276. [Google Scholar] [CrossRef]
- Mirelman, A.; Herman, T.; Brozgol, M.; Dorfman, M.; Sprecher, E.; Schweiger, A.; Giladi, N.; Hausdorff, J.M. Executive Function and Falls in Older Adults: New Findings from a Five-Year Prospective Study Link Fall Risk to Cognition. PLoS ONE 2012, 7, e40297. [Google Scholar] [CrossRef]
- Plummer, P.; Zukowski, L.A.; Giuliani, C.; Hall, A.M.; Zurakowski, D. Effects of Physical Exercise Interventions on Gait-Related Dual-Task Interference in Older Adults: A Systematic Review and Meta-Analysis. Gerontology 2015, 62, 94–117. [Google Scholar] [CrossRef]
- Uemura, K.; Shimada, H.; Makizako, H.; Doi, T.; Yoshida, D.; Tsutsumimoto, K.; Anan, Y.; Suzuki, T. Cognitive function affects trainability for physical performance in exercise intervention among older adults with mild cognitive impairment. Clin. Interv. Aging 2013, 8, 97–102. [Google Scholar] [CrossRef]
- Vogt, L.; Wieland, K.; Bach, M.; Himmelreich, H.; Banzer, W. Cognitive status and ambulatory rehabilitation outcome in geriatric patients. J. Rehabil. Med. 2008, 40, 876–878. [Google Scholar] [CrossRef][Green Version]
- Diamond, P.T.; Felsenthal, G.; Macciocchi, S.N.; Butler, D.H.; Lally-Cassady, D. Effect of cognitive impairment on rehabilitation outcome. Am. J. Phys. Med. Rehabil. 1996, 75, 40–43. [Google Scholar] [CrossRef]
- Hauer, K.; Becker, C.; Lindemann, U.; Beyer, N. Effectiveness of physical training on motor performance and fall prevention in cognitively impaired older persons: A systematic review. Am. J. Phys. Med. Rehabil. 2006, 85, 847–857. [Google Scholar] [CrossRef]
- Population par Âge, Tableaux de l’Insee. Available online: https://www.insee.fr/fr/statistiques/4277619?sommaire=4318291#consulter (accessed on 16 March 2022).
- Rincé, G.; Couturier, C.; Berrut, G.; Dylis, A.; Montero-Odasso, M.; Deschamps, T. Impact of an individual personalised rehabilitation program on mobility performance in older-old people. Aging Clin. Exp. Res. 2021, 33, 2821–2830. [Google Scholar] [CrossRef]
- Priest, A.W.; Salamon, K.B.; Hollman, J.H. Age-related differences in dual task walking: A cross sectional study. J. Neuroeng. Rehabil. 2008, 5, 29. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31, Erratum in Age Ageing 2019, 48, 601. [Google Scholar] [CrossRef]
- Friedman, P.J.; Baskett, J.J.; Richmond, D.E. Cognitive impairment and its relationship to gait rehabilitation in the elderly. N. Z. Med. J. 1989, 102, 603–606. [Google Scholar] [PubMed]
- Dubois, B.; Slachevsky, A.; Litvan, I.; Pillon, B. The FAB: A Frontal Assessment Battery at bedside. Neurology 2000, 55, 1621–1626. [Google Scholar] [CrossRef] [PubMed]
- Katz, S.; Downs, T.D.; Cash, H.R.; Grotz, R.C. Progress in development of the index of ADL. Gerontologist 1970, 10, 20–30. [Google Scholar] [CrossRef] [PubMed]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef]
- Millán-Calenti, J.C.; Tubío, J.; Pita-Fernández, S.; González-Abraldes, I.; Lorenzo, T.; Fernández-Arruty, T.; Maseda, A. Prevalence of functional disability in activities of daily living (ADL), instrumental activities of daily living (IADL) and associated factors, as predictors of morbidity and mortality. Arch. Gerontol. Geriatr. 2010, 50, 306–310. [Google Scholar] [CrossRef]
- Weiss, A.; Mirelman, A.; Buchman, A.S.; Bennett, D.A.; Hausdorff, J.M. Using a body-fixed sensor to identify subclinical gait difficulties in older adults with IADL disability: Maximizing the output of the timed up and go. PLoS ONE 2013, 8, e68885. [Google Scholar] [CrossRef]
- Aoki, K.; Sakuma, M.; Endo, N. The impact of exercise and vitamin D supplementation on physical function in community-dwelling elderly individuals: A randomized trial. J. Orthop. Sci. 2018, 23, 682–687. [Google Scholar] [CrossRef]
- Annweiler, C.; Henni, S.; Walrand, S.; Montero-Odasso, M.; Duque, G.; Duval, G.T. Vitamin D and walking speed in older adults: Systematic review and meta-analysis. Maturitas 2017, 106, 8–25. [Google Scholar] [CrossRef]
- Hale, M.; Shah, S.; Clegg, A. Frailty, inequality and resilience. Clin. Med. 2019, 19, 219–223. [Google Scholar] [CrossRef]
- Brandler, T.C.; Wang, C.; Oh-Park, M.; Holtzer, R.; Verghese, J. Depressive symptoms and gait dysfunction in the elderly. Am. J. Geriatr. Psychiatry 2012, 20, 425–432. [Google Scholar] [CrossRef]
- Murri, M.B.; Triolo, F.; Coni, A.; Tacconi, C.; Nerozzi, E.; Escelsior, A.; Respino, M.; Neviani, F.; Bertolotti, M.; Bertakis, K.; et al. Instrumental assessment of balance and gait in depression: A systematic review. Psychiatry Res. 2020, 284, 112687. [Google Scholar] [CrossRef]
- Feldman, R.; Schreiber, S.; Pick, C.G.; Been, E. Gait, Balance and Posture in Major Mental Illnesses: Depression, Anxiety and Schizophrenia. Austin Med. Sci. 2020, 5, 1039. [Google Scholar]
- Umegaki, H.; Yanagawa, M.; Komiya, H.; Matsubara, M.; Fujisawa, C.; Suzuki, Y.; Kuzuya, M. Polypharmacy and gait speed in individuals with mild cognitive impairment. Geriatr. Gerontol. Int. 2019, 19, 730–735. [Google Scholar] [CrossRef]
- Peron, E.P.; Gray, S.L.; Hanlon, J.T. Medication use and functional status decline in older adults: A narrative review. Am. J. Geriatr. Pharmacother. 2011, 9, 378–391. [Google Scholar] [CrossRef]
- Morris, R.; Lord, S.; Bunce, J.; Burn, D.; Rochester, L. Gait and cognition: Mapping the global and discrete relationships in ageing and neurodegenerative disease. Neurosci. Biobehav. Rev. 2016, 64, 326–345. [Google Scholar] [CrossRef]
- Peel, N.M.; Alapatt, L.J.; Jones, L.V.; Hubbard, R.E. The Association Between Gait Speed and Cognitive Status in Community-Dwelling Older People: A Systematic Review and Meta-analysis. J. Gerontol. A Biol. Sci. Med. Sci. 2019, 74, 943–948. [Google Scholar] [CrossRef]
- Zhang, W.; Low, L.F.; Gwynn, J.D.; Clemson, L. Interventions to Improve Gait in Older Adults with Cognitive Impairment: A Systematic Review. J. Am. Geriatr. Soc. 2019, 67, 381–391. [Google Scholar] [CrossRef]
| Total Population n = 145 | Increase in Dual-Task Walk Speed n = 62 (43%) | No Increase in Dual-Task Walk Speed n = 83 (57%) | p-Value | |
|---|---|---|---|---|
| Age in years, mean (SD) | 83.6 (5.4) | 84.2 (5.4) | 83.1 (5.3) | 0.228 |
| Female, n (%) | 103 (71) | 47 (76) | 56 (67) | 0.355 |
| MMSE, mean (SD) | 25.6 (3.8) | 26.2 (4.0) | 25.1 (3.6) | 0.028 |
| FAB, mean (SD) | 12.2 (4.3) | 12.4 (4.2) | 12.1 (4.4) | 0.678 |
| ADL, mean (SD) | 5.4 (1.0) | 5.3 (1.0) | 5.4 (0.9) | 0.773 |
| IADL, mean (SD) | 5.5 (2.3) | 5.7 (2.3) | 5.3 (2.3) | 0.292 |
| Charlson Comorbidity Index, mean (SD) | 1.1 (1.2) | 1.1 (1.3) | 1.1 (1.2) | 0.997 |
| Number of drugs, mean (SD) | 5.7 (3.1) | 6.1 (3.1) | 5.4 (3.2) | 0.138 |
| Number of psychotropic drugs, mean (SD) | 0.7 (0.8) | 0.8 (0.9) | 0.7 (0.8) | 0.428 |
| BMI in kg/m2, mean (SD) | 25.2 (4.8) | 25.4 (4.6) | 25.1 (4.9) | 0.318 |
| Vitamin D (ng/mL), mean (SD) | 23.0 (12.0) | 19.6 (9.8) | 26.1 (13.2) | 0.015 |
| Severe sarcopenia, n (%) | 7 (5) | 2 (3) | 5 (6) | 0.462 |
| History of fall, n (%) | 117 (81) | 48 (77) | 69 (83) | 0.403 |
| History of repeated falls, n (%) | 84 (58) | 34 (55) | 50 (60) | 0.610 |
| Osteoarthritis, n (%) | 46 (32) | 18 (29) | 28 (34) | 0.588 |
| Reduced visual acuity, n (%) | 58 (40) | 26 (42) | 32 (39) | 0.661 |
| Neurosensorial disorders, n (%) | 35 (24) | 12 (19) | 23 (28) | 0.243 |
| Depressive syndrome, n (%) | 54 (37) | 27 (44) | 27 (33) | 0.288 |
| Initial fluency walking speed in m/s, mean (SD) | 0.60 (0.20) | 0.54 (0.20) | 0.65 (0.19) | 0.001 |
| Time interval between initial and final assessments, mean (SD) | 132 (66) | 116 (66) | 144 (64) | 0.001 |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| OR (IC 95%) | p | OR (IC 95%) | p | |
| Age | 1.04 (0.98; 1.11) | 0.227 | 1.15 (0.98; 1.35) | 0.095 |
| Female | 1.51 (0.72; 3.17) | 0.275 | 0.95 (0.08; 11.05) | 0.968 |
| MMSE | 1.08 (0.99; 1.19) | 0.096 | 0.83 (0.62; 1.13) | 0.233 |
| FAB | 1.02 (0.95; 1.10) | 0.607 | 0.97 (0.76; 1.24) | 0.807 |
| ADL | 0.94 (0.66; 1.33) | 0.720 | 0.95 (0.39; 2.31) | 0.908 |
| IADL | 1.08 (0.93; 1.26) | 0.307 | 2.50 (1.26; 4.94) | 0.009 |
| Charlson index | 1.04 (0.79; 1.36) | 0.780 | 1.61 (0.69; 3.74) | 0.268 |
| Number of medications | 1.07 (0.96; 1.19) | 0.207 | 1.41 (1.04; 1.92) | 0.027 |
| Number of psychotropic drugs | 1.19 (0.79; 1.79) | 0.404 | - | - |
| BMI | 1.01 (0.95; 1.09) | 0.685 | 1.02 (0.87; 1.20) | 0.814 |
| Blood vitamin D level | 0.95 (0.91; 0.99) | 0.021 | 0.83 (0.72; 0.95) | 0.008 |
| Severe sarcopenia | 0.48 (0.09; 2.59) | 0.397 | 0.01 (0.00; 0.32) | 0.016 |
| History of fall | 0.70 (0.30; 1.59) | 0.390 | 0.33 (0.02; 4.35) | 0.396 |
| History of repeated falls | 0.80 (0.41; 1.56) | 0.515 | - | - |
| Depression | 1.5 (0.77; 3.01) | 0.230 | 15.85 (1.32; 190.40) | 0.029 |
| Osteoarthritis | 0.80 (0.39; 1.6) | 0.533 | 0.30 (0.04; 2.57) | 0.271 |
| Initial fluency walking speed | 0.97 (0.95; 0.99) | 0.001 | 0.92 (0.86; 0.98) | 0.014 |
| Time interval between initial and final assessments | 0.99 (0.99; 1.00) | 0.015 | 0.98 (0.96; 1.00) | 0.026 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cubillé, M.; Couturier, C.; Rincé, G.; Deschamps, T.; Derkinderen, P.; de Decker, L.; Berrut, G.; Chapelet, G. Factors Associated with Dual-Fluency Walk Speed Improvement after Rehabilitation in Older Patients. J. Clin. Med. 2022, 11, 7443. https://doi.org/10.3390/jcm11247443
Cubillé M, Couturier C, Rincé G, Deschamps T, Derkinderen P, de Decker L, Berrut G, Chapelet G. Factors Associated with Dual-Fluency Walk Speed Improvement after Rehabilitation in Older Patients. Journal of Clinical Medicine. 2022; 11(24):7443. https://doi.org/10.3390/jcm11247443
Chicago/Turabian StyleCubillé, Marion, Catherine Couturier, Guy Rincé, Thibault Deschamps, Pascal Derkinderen, Laure de Decker, Gilles Berrut, and Guillaume Chapelet. 2022. "Factors Associated with Dual-Fluency Walk Speed Improvement after Rehabilitation in Older Patients" Journal of Clinical Medicine 11, no. 24: 7443. https://doi.org/10.3390/jcm11247443
APA StyleCubillé, M., Couturier, C., Rincé, G., Deschamps, T., Derkinderen, P., de Decker, L., Berrut, G., & Chapelet, G. (2022). Factors Associated with Dual-Fluency Walk Speed Improvement after Rehabilitation in Older Patients. Journal of Clinical Medicine, 11(24), 7443. https://doi.org/10.3390/jcm11247443






