Myocardial Injury Is Associated with the Incidence of Major Adverse Cardiac Events in Patients with Severe Trauma
Abstract
1. Introduction
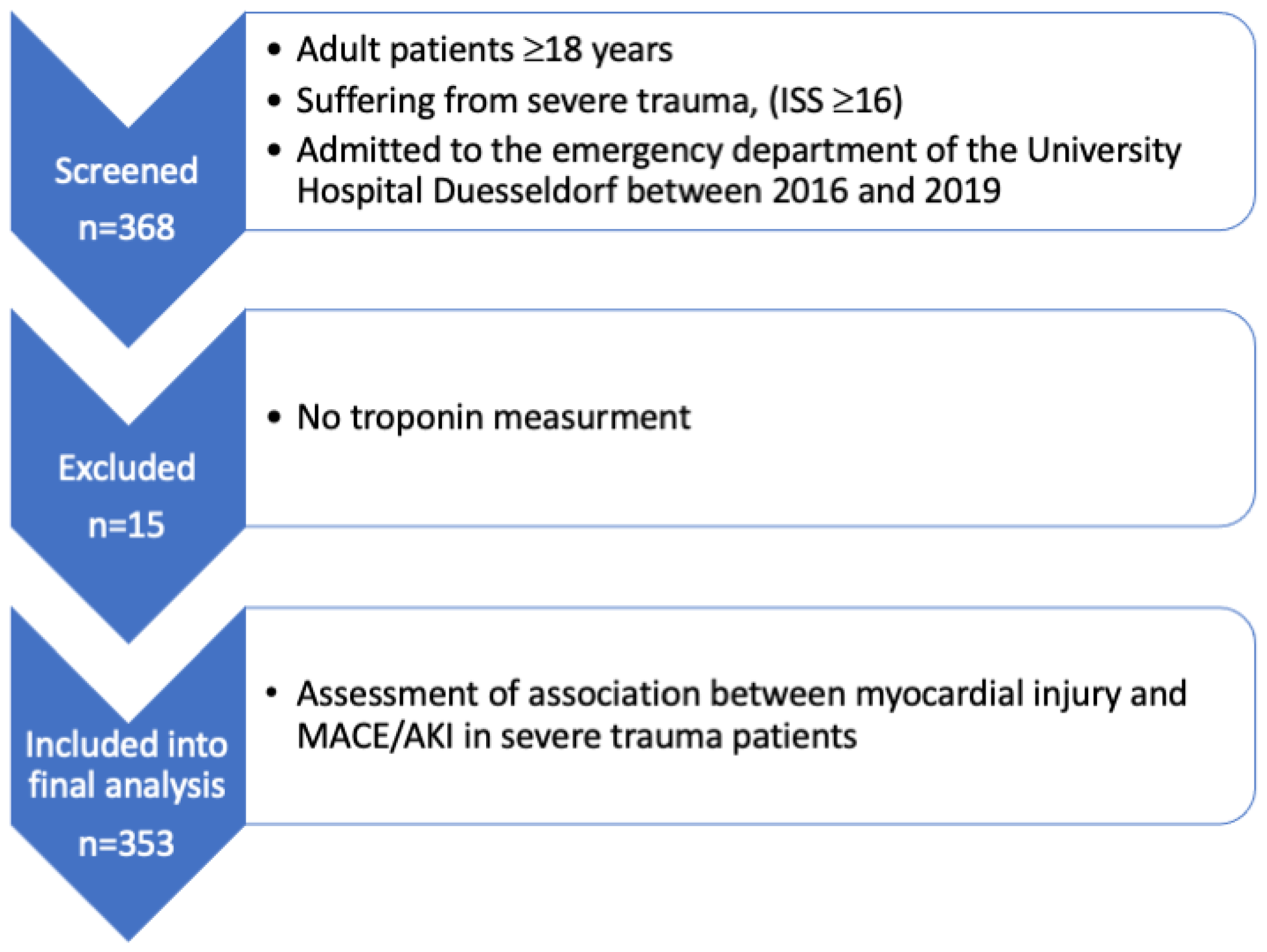
2. Materials and Methods
2.1. Study Population
2.2. Outcome Measures
2.3. Statistical Analysis
2.4. Independent Variable and Covariates
3. Results
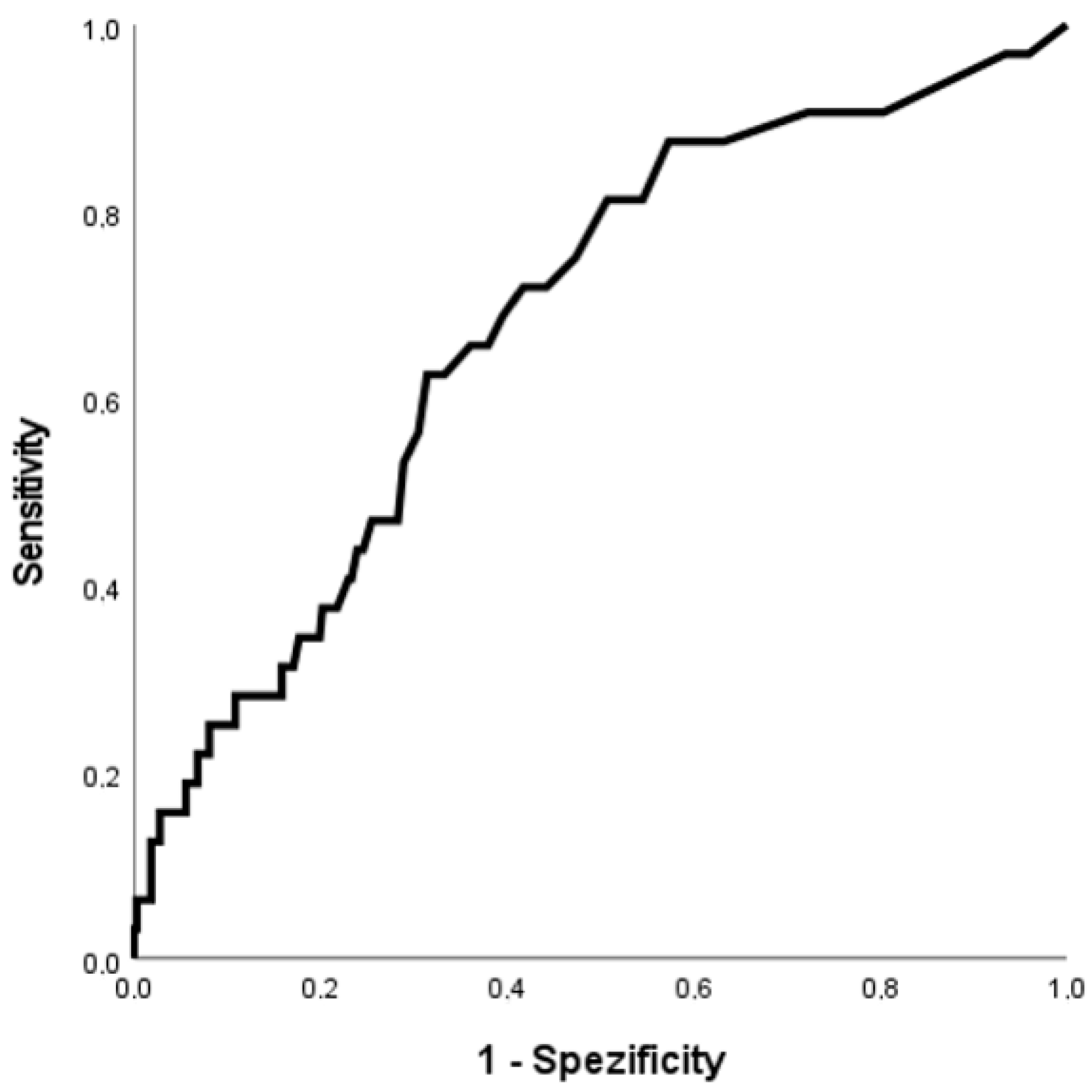
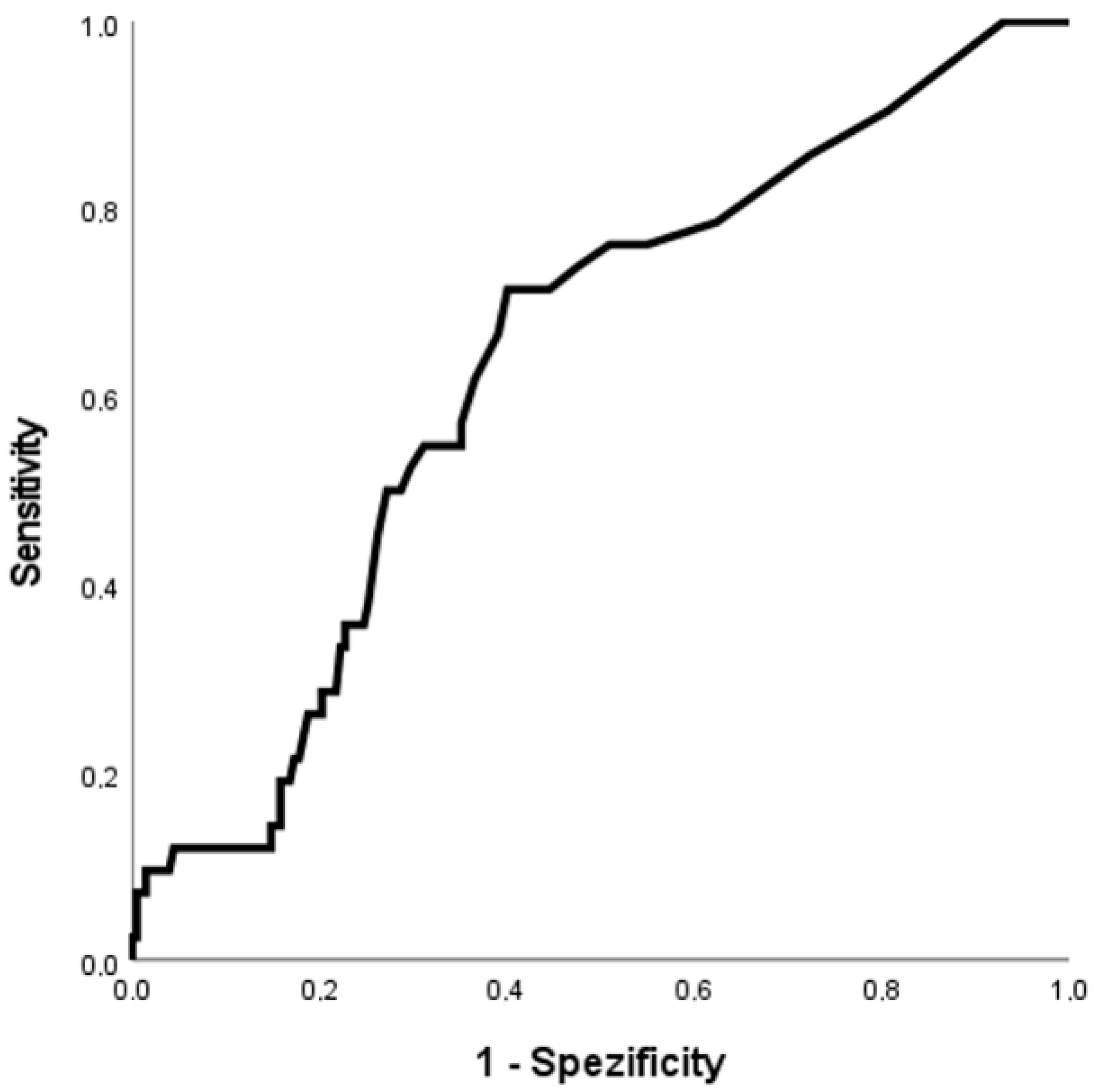
3.1. Discrimination of Myocardial Injury for MACE and AKI
3.2. Multivariate Regression Models
3.3. Association between MACE, AKI, and Mortality in Patients with Severe Trauma
4. Discussion
4.1. MACE and Severe Trauma
4.2. Clinical Relevance
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Variable | Regression Coefficient | Odds Ratio | 95% Confidence Interval | p-Value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Myocardial injury | 0.954 | 2.60 | 1.13 | 5.95 | 0.024 |
| Age per year | 0.009 | 1.009 | 0.99 | 1.03 | 0.349 |
| Coronary artery disease | 0.678 | 1.97 | 0.65 | 5.99 | 0.232 |
| Injury Severity Score | 0.024 | 1.024 | 0.995 | 1.054 | 0.100 |
References
- Destatis Statistisches Bundesamt. Gestorbene: Deutschland, Jahre, Todesursachen, Altersgruppen. Available online: https://www-genesis.destatis.de/genesis/online?operation=previous&levelindex=2&step=2&titel=Ergebnis&levelid=1629917943886&acceptscookies=false#abreadcrumb (accessed on 25 August 2021).
- Gebhard, F.; Huber-Lang, M. Polytrauma—Pathophysiology and management principles. Langenbeck’s Arch. Surg. 2008, 393, 825–831. [Google Scholar] [CrossRef] [PubMed]
- Nunn, J.F.; Freeman, J. Problems of Oxygenation and Oxygen Transport during Haemorrhage. Anaesthesia 1964, 19, 206–216. [Google Scholar] [CrossRef] [PubMed]
- Cannon, J.W. Hemorrhagic Shock. N. Engl. J. Med. 2018, 378, 370–379. [Google Scholar] [CrossRef] [PubMed]
- Tisherman, S.A.; Alam, H.B.; Rhee, P.M.; Scalea, T.M.; Drabek, T.; Forsythe, R.M.; Kochanek, P.M. Development of the emergency preservation and resuscitation for cardiac arrest from trauma clinical trial. J. Trauma Acute Care Surg. 2017, 83, 803–809. [Google Scholar] [CrossRef] [PubMed]
- Chaudry, I.H. Cellular mechanisms in shock and ischemia and their correction. Am. J. Physiol. 1983, 245, R117–R134. [Google Scholar] [CrossRef] [PubMed]
- Stroda, A.; Thelen, S.; M’Pembele, R.; Adelowo, A.; Jaekel, C.; Schiffner, E.; Bieler, D.; Bernhard, M.; Huhn, R.; Lurati Buse, G.; et al. Incidence and prognosis of myocardial injury in patients with severe trauma. Eur. J. Trauma Emerg. Surg. 2021, 48, 3073–3079. [Google Scholar] [CrossRef] [PubMed]
- Sazgary, L.; Puelacher, C.; Lurati Buse, G.; Glarner, N.; Lampart, A.; Bolliger, D.; Steiner, L.; Gurke, L.; Wolff, T.; Mujagic, E.; et al. Incidence of major adverse cardiac events following non-cardiac surgery. Eur. Heart J. Acute Cardiovasc. Care 2021, 10, 550–558. [Google Scholar] [CrossRef] [PubMed]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; Mickley, H.; Crea, F.; Van de Werf, F.; et al. Fourth universal definition of myocardial infarction. Kardiol. Pol. 2018, 76, 1383–1415. [Google Scholar] [CrossRef] [PubMed]
- Summary of Recommendation Statements. Kidney Int. Suppl. 2012, 2, 8–12. [CrossRef] [PubMed]
- Peduzzi, P.; Concato, J.; Feinstein, A.R.; Holford, T.R. Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J. Clin. Epidemiol. 1995, 48, 1503–1510. [Google Scholar] [CrossRef] [PubMed]
- Naganathar, S.; De’Ath, H.D.; Wall, J.; Brohi, K. Admission biomarkers of trauma-induced secondary cardiac injury predict adverse cardiac events and are associated with plasma catecholamine levels. J. Trauma Acute Care Surg. 2015, 79, 71–77. [Google Scholar] [CrossRef]
- De’Ath, H.D.; Rourke, C.; Davenport, R.; Manson, J.; Renfrew, I.; Uppal, R.; Davies, L.C.; Brohi, K. Clinical and biomarker profile of trauma-induced secondary cardiac injury. Br. J. Surg. 2012, 99, 789–797. [Google Scholar] [CrossRef]
- Gawande, N.B.; Tumram, N.K.; Dongre, A.P. Cardiac changes in hospitalized patients of trauma. Shock 2014, 42, 211–217. [Google Scholar] [CrossRef] [PubMed]
- De’Ath, H.D.; Manson, J.; Davenport, R.; Glasgow, S.; Renfrew, I.; Davies, L.C.; Uppal, R.; Brohi, K. Trauma-induced secondary cardiac injury is associated with hyperacute elevations in inflammatory cytokines. Shock 2013, 39, 415–420. [Google Scholar] [CrossRef] [PubMed]
- Stroda, A.; Thelen, S.; M’Pembele, R.; Khademlou, N.; Jaekel, C.; Schiffner, E.; Bieler, D.; Bernhard, M.; Huhn, R.; Lurati Buse, G.; et al. Association between hypotension and myocardial injury in patients with severe trauma. Eur. J. Trauma Emerg. Surg. 2022. [Google Scholar] [CrossRef] [PubMed]
- Foucrier, A.; Rodseth, R.; Aissaoui, M.; Ibanes, C.; Goarin, J.P.; Landais, P.; Coriat, P.; Le Manach, Y. The long-term impact of early cardiovascular therapy intensification for postoperative troponin elevation after major vascular surgery. Anesth. Analg. 2014, 119, 1053–1063. [Google Scholar] [CrossRef] [PubMed]
- Devereaux, P.J.; Xavier, D.; Pogue, J.; Guyatt, G.; Sigamani, A.; Garutti, I.; Leslie, K.; Rao-Melacini, P.; Chrolavicius, S.; Yang, H.; et al. Characteristics and short-term prognosis of perioperative myocardial infarction in patients undergoing noncardiac surgery: A cohort study. Ann. Intern. Med. 2011, 154, 523–528. [Google Scholar] [CrossRef] [PubMed]
- Walsh, M.; Devereaux, P.J.; Garg, A.X.; Kurz, A.; Turan, A.; Rodseth, R.N.; Cywinski, J.; Thabane, L.; Sessler, D.I. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: Toward an empirical definition of hypotension. Anesthesiology 2013, 119, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Valentijn, T.M.; Hoeks, S.E.; Martienus, K.A.; Bakker, E.J.; van de Luijtgaarden, K.M.; Verhagen, H.J.; Stolker, R.J.; van Lier, F. Impact of haemoglobin concentration on cardiovascular outcome after vascular surgery: A retrospective observational cohort study. Eur. J. Anaesthesiol. 2013, 30, 664–670. [Google Scholar] [CrossRef] [PubMed]
- Ausset, S.; Auroy, Y.; Verret, C.; Benhamou, D.; Vest, P.; Cirodde, A.; Lenoir, B. Quality of postoperative care after major orthopedic surgery is correlated with both long-term cardiovascular outcome and troponin Ic elevation. Anesthesiology 2010, 113, 529–540. [Google Scholar] [CrossRef] [PubMed]
| Patients with Severe Trauma (n = 353) | Patients with Myocardial Injury (n = 149) | Patients without Myocardial Injury (n = 204) | Patients with MACE (n = 32) | Patients without MACE (n = 321) | |
|---|---|---|---|---|---|
| Baseline characteristics | |||||
| Male sex no. (%) | 256 (72.5%) | 104 (69,8%) | 152 (74.5%) | 28 (87.5%) | 228 (71%) |
| Age (years) | 55 ± 21 | 62 ± 22 | 50 ± 18 | 62 ± 20 | 54 ± 21 |
| Adipositas (body mass index ≥ 30 kg/m²) | 3 (0.8%) | 2 (1.3%) | 1 (0.5%) | 1 (3.1%) | 2 (0.6%) |
| Comorbidities | |||||
| Coronary artery disease | 28 (7.9%) | 16 (10.7%) | 12 (5.9%) | 5 (15.6%) | 23 (7.2%) |
| Chronic kidney disease (≥CKD III) | 9 (2.5%) | 7 (4.7%) | 2 (1.0%) | 2 (6.3%) | 7 (2.2%) |
| Diabetes mellitus | 22 (6.2%) | 9 (6.0%) | 13 (6.5%) | 3 (9.4%) | 19 (5.9%) |
| History of arterial hypertension | 85 (24.1%) | 41 (27.5%) | 44 (21.6%) | 11 (34.4%) | 74 (23.1%) |
| Peripheral artery disease | 5 (1.4%) | 3 (2.0%) | 2 (1.0%) | 1 (3.1%) | 4 (1.2%) |
| ASA physical status | |||||
| ASA I | 159 (45%) | 47 (35.3%) | 112 57.1%) | 9 (30%) | 150 (50.2%) |
| ASA II | 111 (31.4%) | 57 (42.9%) | 54 27.6%) | 13 (43.3%) | 98 (32,8%) |
| ASA III | 52 (14.7%) | 24 (18%) | 28 (14.3%) | 8 (26.7%) | 44 (14.7%) |
| ASA IV | 7 (2.0%) | 5 (3.8%) | 2 (1.0%) | / | 7 (2.3%) |
| Trauma-related data | |||||
| ISS | 28 ± 12 25 (19–33) | 30 ± 12 26 (22–38) | 26 ± 10 22 (17–29) | 32 ± 13 28 (22–40) | 27 ± 11 25 (18–33) |
| GCS at ED arrival | 8 ± 5 3 (3–14) | 6 ± 5 3 (3–9) | 9 ± 5 10 (3–15) | 5 ± 4 3 (3–7) | 8 ± 5 4 (3–15) |
| Laboratory values | |||||
| Hb (g/dL) | 12.3 ± 2.4 | 11.5 ± 2.5 | 12.8 ± 2.2 | 11.9 ± 3.3 | 12.3 ± 2.3 |
| INR | 1.4 ± 0.8 | 1.6 ± 1.0 | 1.2 ± 0.5 | 1.9 ± 1.5 | 1.3 ± 0.7 |
| PTT (s) | 31.7 ± 24.4 | 38.0 ± 32.6 | 27.3 ± 15.0 | 44.1 ± 37.4 | 30.5 ± 22.4 |
| Base excess | −3.8 ± 5.7 | −5.7 ± 6.7 | −2.5 ± 4.5 | −8.0 ± 7.6 | −3.4 ± 5.4 |
| HsTnT initial (ng/mL) | 63.3 ± 415.7 11.0 (6.0–28.5) | 139.8 ± 633.1 36.0 (21.0–75.0) | 7.5 ± 3.0 7.0 (5.0–10.0) | 321 ± 1336.9 22 (11.3–76.8) | 37.6 ± 98.1 11 (6–26) |
| Creatinine initial (mg/dL) | 1.04 ± 0.62 | 1.16 ± 0.51 1.1 (0.88–1.3) | 0.95 ± 0.68 0.9 (0.73–1.07) | 1.15 ± 0.6 1.0 (0.89–1.28) | 1.03 ± 0.62 0.98 (0.79–1.1) |
| Outcome | |||||
| Death in hospital | 92 (26.1%) | 67 (45%) | 25 (12.3%) | 20 (62.5%) | 72 (22.4%) |
| Myocardial injury | 149 (42.2%) | 149 (100%) | 0 (0%) | 22 (68.8%) | 127 (39.6%) |
| In-hospital MACE | 32 (9.1%) | 22 (14.8%) | 10 (4.9%) | 32 (100%) | / |
| Non-fatal cardiac arrest | 20 (5.7%) | 16 (10.7% | 4 (2.0% | 20 (62.5%) | / |
| Myocardial infarction | 2 (0.6%) | 2 (1.3%) | 0 (0%) | 2 (6.3%) | / |
| New-onset arrythmia | 9 (2.5%) | 5 (3.4%) | 4 (2.0%) | 9 (28.1%) | / |
| Stroke | 5 (1.4%) | 3 (2.0%) | 2 (1.0%) | 5 (15.6%) | / |
| AKI 1 | 42 (17.2%) | 26 (26.0%) | 16 (11.1%) | 10 (40%) | 32 (14.6%) |
| Variable | Regression Coefficient | Odds Ratio | 95% Confidence Interval | p-Value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Myocardial injury | 1.088 | 2.97 | 1.31 | 6.72 | 0.009 |
| Age per year | 0.007 | 1.007 | 0.99 | 1.03 | 0.446 |
| Coronary artery disease | 0.605 | 1.83 | 0.61 | 5.51 | 0.282 |
| Variable | Regression Coefficient | Odds Ratio | 95% Confidence interval | p-Value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Myocardial injury | 0.763 | 2.144 | 1.031 | 4.459 | 0.041 |
| Age per year | 0.028 | 1.029 | 1.009 | 1.049 | 0.003 |
| Sex | −0.74 | 0.477 | 0.182 | 1.253 | 0.133 |
| CKD * ≥ III | 0.848 | 2.335 | 0.519 | 10.511 | 0.269 |
| Cohort | Mortality | Odds Ratio (95% CI) | Adjusted Odds Ratio * (95% CI) |
|---|---|---|---|
| Patients without MACE and AKI (n = 187) | N = 12 6.4% | 0.064 (0.30–0.138) | 0.077 (0.04–0.17) |
| Patients with MACE (no AKI) (n = 15) | N = 6 40% | 2.09 (0.72–6.06) | 2.26 (0.73–7.07) |
| Patients with AKI (no MACE) (n = 32) * | N = 13 40.6% | 4.0 (1.80–8.90) | 3.19 (1.38–7.36) |
| Patients with MACE and AKI (n = 10) | N = 8 80% | 13.23 (2.75–63.6) | 9.15 (1.18–46.20) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stroda, A.; Jaekel, C.; M’Pembele, R.; Guenther, A.; Tenge, T.; Thielmann, C.M.; Thelen, S.; Schiffner, E.; Bieler, D.; Bernhard, M.; et al. Myocardial Injury Is Associated with the Incidence of Major Adverse Cardiac Events in Patients with Severe Trauma. J. Clin. Med. 2022, 11, 7432. https://doi.org/10.3390/jcm11247432
Stroda A, Jaekel C, M’Pembele R, Guenther A, Tenge T, Thielmann CM, Thelen S, Schiffner E, Bieler D, Bernhard M, et al. Myocardial Injury Is Associated with the Incidence of Major Adverse Cardiac Events in Patients with Severe Trauma. Journal of Clinical Medicine. 2022; 11(24):7432. https://doi.org/10.3390/jcm11247432
Chicago/Turabian StyleStroda, Alexandra, Carina Jaekel, René M’Pembele, Alexander Guenther, Theresa Tenge, Carl Maximilian Thielmann, Simon Thelen, Erik Schiffner, Dan Bieler, Michael Bernhard, and et al. 2022. "Myocardial Injury Is Associated with the Incidence of Major Adverse Cardiac Events in Patients with Severe Trauma" Journal of Clinical Medicine 11, no. 24: 7432. https://doi.org/10.3390/jcm11247432
APA StyleStroda, A., Jaekel, C., M’Pembele, R., Guenther, A., Tenge, T., Thielmann, C. M., Thelen, S., Schiffner, E., Bieler, D., Bernhard, M., Huhn, R., Lurati Buse, G., & Roth, S. (2022). Myocardial Injury Is Associated with the Incidence of Major Adverse Cardiac Events in Patients with Severe Trauma. Journal of Clinical Medicine, 11(24), 7432. https://doi.org/10.3390/jcm11247432






