Humeral and Glenoid Version in Reverse Total Shoulder Arthroplasty: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
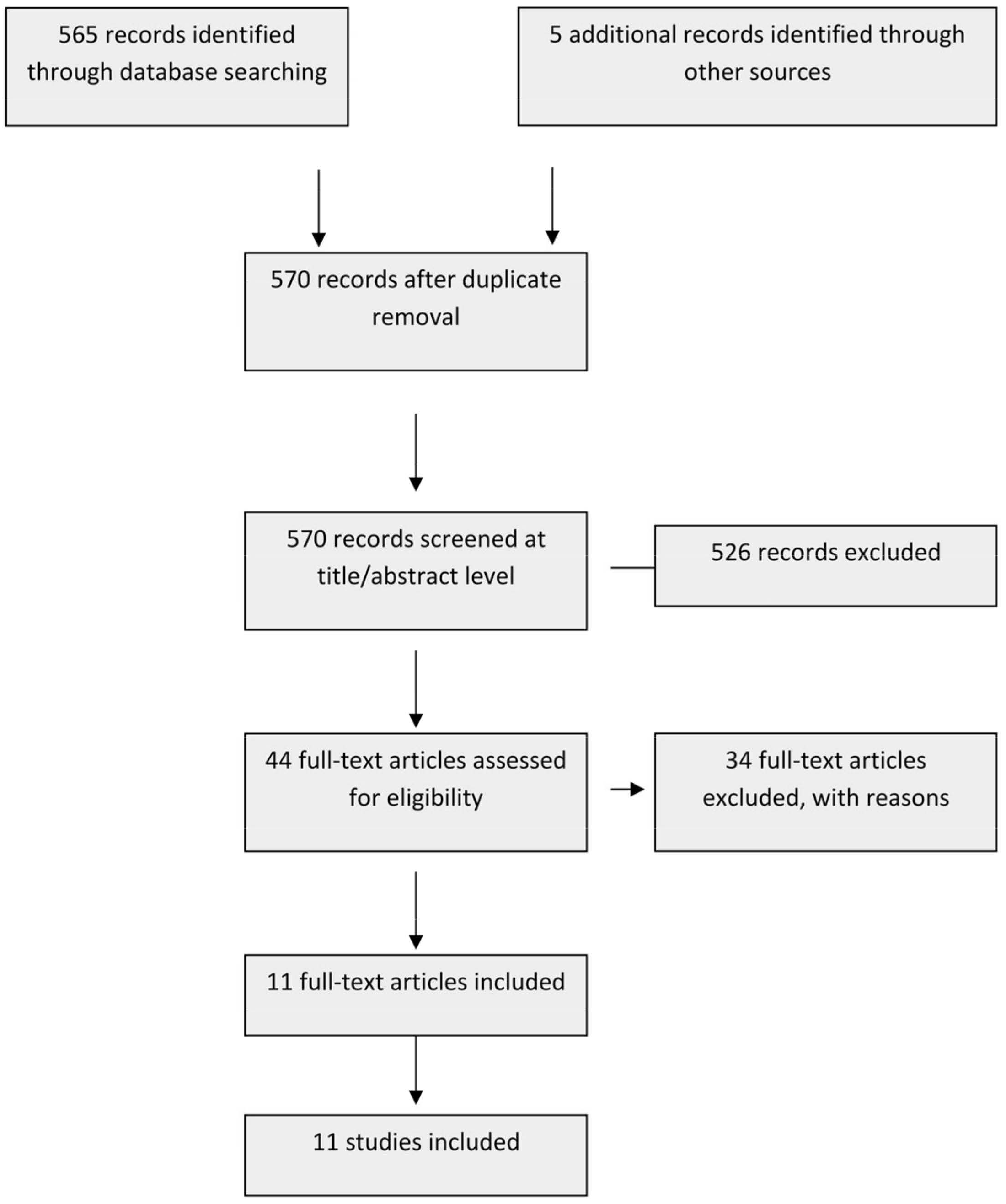
2.1. Study Selection
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Search
2.5. Data Collection Process
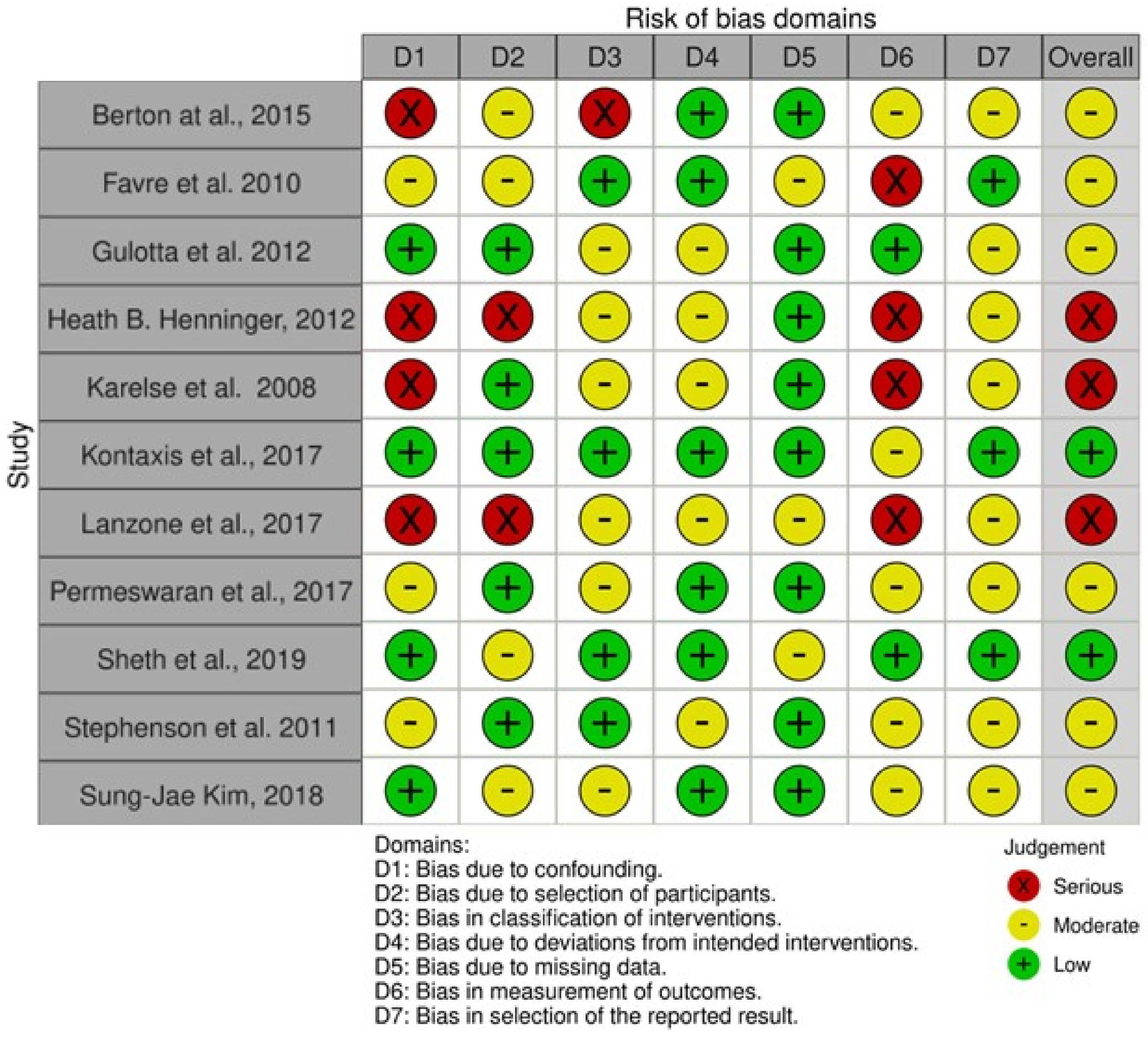
2.6. Study Risk of Bias Assessment
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Quality of Evidence
3.4. Impingement and Range of Motion
3.5. Muscle Forces
3.6. Stability
3.7. Clinical Study
3.8. Implant Design Consideration
4. Discussion
4.1. Limitations
4.2. Strength
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Best, M.J.; Aziz, K.T.; Wilckens, J.H.; McFarland, E.G.; Srikumaran, U. Increasing incidence of primary reverse and anatomic total shoulder arthroplasty in the United States. J. Shoulder Elbow Surg. 2021, 30, 1159–1166. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Papalia, R.; Castagna, A.; De Salvatore, S.; Guerra, E.; Piergentili, I.; Denaro, V. Shoulder replacement: An epidemiological nationwide study from 2009 to 2019. BMC Musculoskelet. Disord. 2022, 23, 889. [Google Scholar] [CrossRef] [PubMed]
- Guery, J.; Favard, L.; Sirveaux, F.; Oudet, D.; Mole, D.; Walch, G. Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J. Bone Jt. Surg. 2006, 88, 1742–1747. [Google Scholar] [CrossRef]
- Wall, B.; Nove-Josserand, L.; O’Connor, D.P.; Edwards, T.B.; Walch, G. Reverse total shoulder arthroplasty: A review of results according to etiology. J. Bone Jt. Surg. 2007, 89, 1476–1485. [Google Scholar] [CrossRef]
- Petrillo, S.; Longo, U.G.; Gulotta, L.V.; Berton, A.; Kontaxis, A.; Wright, T.; Denaro, V. Reverse total shoulder arthroplasty: Research models. Joints 2016, 4, 236–246. [Google Scholar] [CrossRef]
- Berton, A.; Gulotta, L.V.; Longo, U.G.; De Salvatore, S.; Piergentili, I.; Bandini, B.; Lalli, A.; Mathew, J.; Warren, R.F.; Denaro, V. Medialized versus Lateralized Center of Rotation in Reverse Total Shoulder Arthroplasty: A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 5868. [Google Scholar] [CrossRef]
- Chalmers, P.N.; Keener, J.D. Expanding roles for reverse shoulder arthroplasty. Curr. Rev. Musculoskelet. Med. 2016, 9, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Petrillo, S.; Berton, A.; Denaro, V. Reverse total shoulder arthroplasty for the management of fractures of the proximal humerus: A systematic review. Musculoskelet. Surg. 2016, 100, 83–91. [Google Scholar] [CrossRef]
- Boileau, P.; Watkinson, D.J.; Hatzidakis, A.M.; Balg, F. Grammont reverse prosthesis: Design, rationale, and biomechanics. J. Shoulder Elbow Surg. 2005, 14, 147S–161S. [Google Scholar] [CrossRef]
- Boileau, P.; Watkinson, D.; Hatzidakis, A.M.; Hovorka, I. Neer Award 2005: The Grammont reverse shoulder prosthesis: Results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J. Shoulder Elbow Surg. 2006, 15, 527–540. [Google Scholar] [CrossRef]
- Levigne, C.; Boileau, P.; Favard, L.; Garaud, P.; Mole, D.; Sirveaux, F.; Walch, G. Scapular notching in reverse shoulder arthroplasty. J. Shoulder Elbow Surg. 2008, 17, 925–935. [Google Scholar] [CrossRef] [PubMed]
- Simovitch, R.W.; Zumstein, M.A.; Lohri, E.; Helmy, N.; Gerber, C. Predictors of scapular notching in patients managed with the Delta III reverse total shoulder replacement. J. Bone Jt. Surg. 2007, 89, 588–600. [Google Scholar] [CrossRef] [PubMed]
- Werner, C.M.; Steinmann, P.A.; Gilbart, M.; Gerber, C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J. Bone Jt. Surg. 2005, 87, 1476–1486. [Google Scholar] [CrossRef]
- Lee, D.H.; Choi, Y.S.; Potter, H.G.; Endo, Y.; Sivakumaran, T.; Lim, T.K.; Chun, T.J. Reverse total shoulder arthroplasty: An imaging overview. Skelet. Radiol. 2020, 49, 19–30. [Google Scholar] [CrossRef]
- Locher, J.; Wilken, F.; Beitzel, K.; Buchmann, S.; Longo, U.G.; Denaro, V.; Imhoff, A.B. Hill-Sachs Off-track Lesions as Risk Factor for Recurrence of Instability After Arthroscopic Bankart Repair. Arthroscopy 2016, 32, 1993–1999. [Google Scholar] [CrossRef]
- Kiet, T.K.; Feeley, B.T.; Naimark, M.; Gajiu, T.; Hall, S.L.; Chung, T.T.; Ma, C.B. Outcomes after shoulder replacement: Comparison between reverse and anatomic total shoulder arthroplasty. J. Shoulder Elbow Surg. 2015, 24, 179–185. [Google Scholar] [CrossRef]
- Gulotta, L.V.; Choi, D.; Marinello, P.; Knutson, Z.; Lipman, J.; Wright, T.; Cordasco, F.A.; Craig, E.V.; Warren, R.F. Humeral component retroversion in reverse total shoulder arthroplasty: A biomechanical study. J. Shoulder Elbow Surg. 2012, 21, 1121–1127. [Google Scholar] [CrossRef]
- Favre, P.; Sussmann, P.S.; Gerber, C. The effect of component positioning on intrinsic stability of the reverse shoulder arthroplasty. J. Shoulder Elbow Surg. 2010, 19, 550–556. [Google Scholar] [CrossRef]
- Kontaxis, A.; Chen, X.; Berhouet, J.; Choi, D.; Wright, T.; Dines, D.M.; Warren, R.F.; Gulotta, L.V. Humeral version in reverse shoulder arthroplasty affects impingement in activities of daily living. J. Shoulder Elbow Surg. 2017, 26, 1073–1082. [Google Scholar] [CrossRef]
- Berton, A.; Gulotta, L.V.; Petrillo, S.; Florio, P.; Longo, U.G.; Denaro, V.; Kontaxis, A. The effect of humeral version on teres minor muscle moment arm, length, and impingement in reverse shoulder arthroplasty during activities of daily living. J. Shoulder Elbow Surg. 2015, 24, 578–586. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Henninger, H.B.; Barg, A.; Anderson, A.E.; Bachus, K.N.; Tashjian, R.Z.; Burks, R.T. Effect of deltoid tension and humeral version in reverse total shoulder arthroplasty: A biomechanical study. J. Shoulder Elbow Surg. 2012, 21, 483–490. [Google Scholar] [CrossRef]
- Stephenson, D.R.; Oh, J.H.; McGarry, M.H.; Rick Hatch, G.F., 3rd; Lee, T.Q. Effect of humeral component version on impingement in reverse total shoulder arthroplasty. J. Shoulder Elbow Surg. 2011, 20, 652–658. [Google Scholar] [CrossRef] [PubMed]
- Karelse, A.T.; Bhatia, D.N.; De Wilde, L.F. Prosthetic component relationship of the reverse Delta III total shoulder prosthesis in the transverse plane of the body. J. Shoulder Elbow Surg. 2008, 17, 602–607. [Google Scholar] [CrossRef]
- Lanzone, R.; Carbone, S.; Albino, P.; Cassio, J.B.; Métais, P. Retroverted glenoid reconstruction using glenoid plate in reverse shoulder arthroplasty. Musculoskelet. Surg. 2017, 101, 121–127. [Google Scholar] [CrossRef]
- Permeswaran, V.N.; Caceres, A.; Goetz, J.E.; Anderson, D.D.; Hettrich, C.M. The effect of glenoid component version and humeral polyethylene liner rotation on subluxation and impingement in reverse shoulder arthroplasty. J. Shoulder Elbow Surg. 2017, 26, 1718–1725. [Google Scholar] [CrossRef]
- Kim, S.J.; Jang, S.W.; Jung, K.H.; Kim, Y.S.; Lee, S.J.; Yoo, Y.S. Analysis of impingement-free range of motion of the glenohumeral joint after reverse total shoulder arthroplasty using three different implant models. J. Orthop. Sci. 2019, 24, 87–94. [Google Scholar] [CrossRef]
- Sheth, U.; Saltzman, M. Reverse Total Shoulder Arthroplasty: Implant Design Considerations. Curr. Rev. Musculoskelet. Med. 2019, 12, 554–561. [Google Scholar] [CrossRef]
- Jeon, B.K.; Panchal, K.A.; Ji, J.H.; Xin, Y.Z.; Park, S.R.; Kim, J.H.; Yang, S.J. Combined effect of change in humeral neck-shaft angle and retroversion on shoulder range of motion in reverse total shoulder arthroplasty—A simulation study. Clin. Biomech. 2016, 31, 12–19. [Google Scholar] [CrossRef]
- Berhouet, J.; Garaud, P.; Favard, L. Influence of glenoid component design and humeral component retroversion on internal and external rotation in reverse shoulder arthroplasty: A cadaver study. Orthop. Traumatol. Surg. Res. 2013, 99, 887–894. [Google Scholar] [CrossRef] [PubMed]
- Rhee, Y.G.; Cho, N.S.; Moon, S.C. Effects of humeral component retroversion on functional outcomes in reverse total shoulder arthroplasty for cuff tear arthropathy. J. Shoulder Elbow Surg. 2015, 24, 1574–1581. [Google Scholar] [CrossRef] [PubMed]
- Petrillo, S.; Longo, U.G.; Papalia, R.; Denaro, V. Reverse shoulder arthroplasty for massive irreparable rotator cuff tears and cuff tear arthropathy: A systematic review. Musculoskelet. Surg. 2017, 101, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez, S.; Comiskey, C.A.t.; Luo, Z.P.; Pupello, D.R.; Frankle, M.A. Range of impingement-free abduction and adduction deficit after reverse shoulder arthroplasty. Hierarchy of surgical and implant-design-related factors. J. Bone Jt. Surg. 2008, 90, 2606–2615. [Google Scholar] [CrossRef]
- Apreleva, M.; Hasselman, C.T.; Debski, R.E.; Fu, F.H.; Woo, S.L.; Warner, J.J. A dynamic analysis of glenohumeral motion after simulated capsulolabral injury. A cadaver model. J. Bone Jt. Surg. 1998, 80, 474–480. [Google Scholar] [CrossRef]
- Maffulli, N.; Longo, U.G.; Berton, A.; Loppini, M.; Denaro, V. Biological factors in the pathogenesis of rotator cuff tears. Sports Med. Arthrosc. Rev. 2011, 19, 194–201. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Gulotta, L.V.; De Salvatore, S.; Berton, A.; Piergentili, I.; Bandini, B.; Lalli, A.; Denaro, V. The Role of Humeral Neck-Shaft Angle in Reverse Total Shoulder Arthroplasty: 155° versus <155°—A Systematic Review. J. Clin. Med. 2022, 11, 3641. [Google Scholar] [CrossRef]
- Friesenbichler, B.; Grassi, A.; Grobet, C.; Audigé, L.; Wirth, B. Is limited shoulder abduction associated with poor scapulothoracic mobility after reverse shoulder arthroplasty? Arch. Orthop. Trauma Surg. 2021, 141, 587–591. [Google Scholar] [CrossRef]
- Constant, C.R.; Gerber, C.; Emery, R.J.; Sojbjerg, J.O.; Gohlke, F.; Boileau, P. A review of the Constant score: Modifications and guidelines for its use. J. Shoulder Elbow Surg. 2008, 17, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Boileau, P.; Rumian, A.P.; Zumstein, M.A. Reversed shoulder arthroplasty with modified L’Episcopo for combined loss of active elevation and external rotation. J. Shoulder Elbow Surg. 2010, 19, 20–30. [Google Scholar] [CrossRef] [PubMed]
- Gerber, C.; Pennington, S.D.; Lingenfelter, E.J.; Sukthankar, A. Reverse Delta-III total shoulder replacement combined with latissimus dorsi transfer. A preliminary report. J. Bone Jt. Surg. 2007, 89, 940–947. [Google Scholar] [CrossRef]
- Simovitch, R.W.; Helmy, N.; Zumstein, M.A.; Gerber, C. Impact of fatty infiltration of the teres minor muscle on the outcome of reverse total shoulder arthroplasty. J. Bone Jt. Surg. 2007, 89, 934–939. [Google Scholar] [CrossRef]
- Matsen, F.A., 3rd; Boileau, P.; Walch, G.; Gerber, C.; Bicknell, R.T. The reverse total shoulder arthroplasty. J. Bone Jt. Surg. 2007, 89, 660–667. [Google Scholar] [CrossRef]
- Mole, D.; Favard, L. Excentered scapulohumeral osteoarthritis. Rev. Chir. Orthop. Reparatrice Appar. Mot. 2007, 93, 37–94. [Google Scholar]
- Roberts, C.C.; Ekelund, A.L.; Renfree, K.J.; Liu, P.T.; Chew, F.S. Radiologic assessment of reverse shoulder arthroplasty. RadioGraphics 2007, 27, 223–235. [Google Scholar] [CrossRef]
- Van Seymortier, P.; Stoffelen, D.; Fortems, Y.; Reynders, P. The reverse shoulder prosthesis (Delta III) in acute shoulder fractures: Technical considerations with respect to stability. Acta Orthop. Belg. 2006, 72, 474–477. [Google Scholar]
- Gavaskar, A.S.; Vijayraj, K.; Subramanian, S.M. Intraoperative CT navigation for glenoid component fixation in reverse shoulder arthroplasty. Indian J. Orthop. 2013, 47, 104–106. [Google Scholar] [CrossRef] [PubMed]
| Author, yr | Type of Study/LOE | Aim | Sample Size | Sample Anteversion/ Retroversion | Size and Type of Implant | Version Degrees | Abduction/Scaption Degrees | Conclusion |
|---|---|---|---|---|---|---|---|---|
| Berton et al., 2015 [20] | CS, IV | To investigate how the version of humeral fixation can affect the TM rotational moment arm and muscle length as well as impingement after RTSA | A3-dimensional shoulder model | Adapted version of the Newcastle Shoulder Model that resembles the geometry of a commercially available reverse shoulder prosthesis Delta III prosthesis (DePuy International, Leeds, UK) | Four humeral fixation versions were tested: +20°, 0°, −20°, and −40° (+anteverted; -retroverted) | Humeral abduction in scapular plane from 0° to 150°) | The 0 and 20 retroversion was the optimum compromise between sufficient TM length and moment arm with minimum impingement | |
| Favre et al., 2010 [18] | BS Study, BcS | Effects of component positioning on intrinsic stability | 150 trials | Delta III RTSA (DePuy Orthopaedics, Inc., Warsaw, IN, USA) size 36 | Version of the glenosphere: from 20° retroversion to 20° anteversion in 10° steps. Version of the humeral component: neutral, 10°, 20° retroversion and anteversion | 20° and 90° abduction | Effect of humeral component version was highly significant. Implanting the humeral component in neutral or some anteversion can improve anterior stability | |
| Gulotta et al., 2012 [17] | BS Study, BcS | Effects of humeral component retroversion on the muscle forces across the shoulder joint during scaption | Biomet Comprehensive RTSA (Biomet Inc, Warsaw, IN, USA) | 0°, 20°, 30°, and 40° of retroversion | 30° and 60° of scaption | Increasing retroversion did not affect the muscle force | ||
| Impingement-free IR and ER allowed for varying humeral retroversions | 9 mm stem, cemented, neck-shaft angle 147°, 36 mm glenosphere | Placing the implant in 0° to 20° of retroversion maximizes IR with the arm at the side. Concomitant latissimus dorsi transfer is recommended for patients with a deficient teres minor | ||||||
| Henninger, 2012 [25] | BS Study | Effects of humeral version and deltoid tension on (1) ROM in glenohumeral abduction, degree of ER of a flexed arm | 6 cadaveris shoulders (retroversion) | Aequalis Reverse Shoulder (Tornier, Edina, MN, USA) 6.5 mm humeral stem, 36 mm glenosphere | 0°, 10°, 20° of retroversion. 9 combinations of humeral version and implant thickness | Resting abduction and 60° scapular abduction | RTSA reduced ER compared with intact shoulder. Deltoid tension and humeral version had little effect on ER | |
| (2) force required to abduct the arm | From resting abduction position to 65° of glenohumeral abduction in the scapular plane | Humeral version and implant thickness did not influence abduction forces | ||||||
| (3) force required to dislocate the implant in a lateral or anterior direction | Resting abduction position in neutral and 90° ER | Version and deltoid tension did not significantly alter dislocation forces | ||||||
| Karelse et al., 2008 [27] | RSC Study, II | Relation between the positioning of the components in the transverse plane and its consequences on IR/ER of the shoulder | 27 patients | Delta III prosthesis (DePuy International, Leeds, UK) 36 mm glenosphere in 9 patients, 42 mm glensphere in 18 patients | Mean glenohumeral component relationship: 34° with variation from +6° to 59°. | Arm adducted in the coronal plane | To achieve the optimal position of the prosthetic components it should be used a spatial reference system of axes in the sagittal or coronal plane of the body | |
| Kontaxis et al., 2017 [19] | PS CO study, II | To determine how humeral version affects impingement in activities of daily living | 30 virtual arthritic shoulders (Mean age: 71.6 years) | 30 virtual arthritic shoulders (anteversion) 30 virtual arthritic shoulders (retroversion) | Comprehensive RTSA (Biomet, Inc., Warsaw, IN, USA) 28 mm diameter glenoid baseplate; 36 mm diameter standard glenosphere without offset; size 4 humeral “platform” long stem; 44 mm diameter standard onlay humeral tray; and a 44 to 36 mm diameter standard humeral bearingThe neck/shaft angle of the prosthesis and the humeral cut was at 135° | Each of the 30 arthritic shoulders were placed into 5 versions: −40°,−20°, 0°, +20°, and +40° | Largest impingement-free abduction (118° ± 19°) found in −40° version; smallest abduction (19° ± 13°) found in +40° version | Maximizing ROM in standardized tests may not reduce the risk of impingement. An average 0° of humeral version should be preferred |
| Lanzone et al., 2017 [28] | CS, IV | To evaluate the clinical and radiological results of RSA with glenoid plating in a series of patients affected by cuff tear glenohumeral arthropathy with glenoid retroversion >15° | 20 patients (Mean age: 75 ± 5 (61–81)) | Preoperative mean glenoid retroversion: 24° (range 15°–38°, SD 7) Postoperatove mean glenoid retroversion: 2° (range 0°–7°, SD 2) | Retroverted glenoid reconstruction with glenoid plates in RSA is an alternative method to address severe glenoid deficiency | |||
| Permeswaran et al., 2017 [29] | RSC study, III | To determine how changes in glenoid component version affect the arm abduction angle at which impingement occurs | 35 different clinically representative models (computer modeling) | 7 virtual shoulders (anteversion) 21 virtual shoulders (retroversion) | Aequalis Ascend Reverse Flex convertible shoulder system Computer models of the 36 mm Aequalis Ascend Reverse Flex implant system | 5° anteversion; neutral; 5°, 10°, and 20° retroversion | 35° of abduction during flexion to replicate arm swinging | Rotating modern radially asymmetric humeral polyethylene liners posteriorly can reduce the risk of subluxation leading to dislocation and increase ER range of motion |
| Sheth et al., 2019 [31] | SR, III | To provide a review of RTSA designs | Multiple implant-related variables exist on both the humeral and glenoid side that play a role in maximizing implant efficiency | |||||
| Stephenson et al., 2011 [26] | Effects of humeral component version on impingement of the humeral prosthesis against the scapula | 7 cadaveric shoulders | Aequalis Reverse Shoulder (Tornier, Edina, MN, USA) 6.5 mm stem, 36 mm metaphyseal component, a 36 ± 9-mm polyethylene insert, a 36 mm glenosphere, and a 29 mm glenoid baseplate | 20° of anteversion, neutral version, 20° and 40° of retroversion | 0°, 30°, and 60° of glenohumeral abduction in the scapular plane | Placing humeral component between 20° and 40° of retroversion restores a functional arc of motion without impingement | ||
| Kim, 2018 [30] | BS Study, BcS | Investigating impingement-free ROM of the gleno-humeral joint following RTSA with three types of implant models using computational motion analysis | 7 patients | 7 shoulders (retroversion) | GROUP I: AequalisTM-Reversed Shoulder System (Tornier Inc, Edina, MN, USA) GROUP II: AequalisTM-Reversed II Shoulder (Tornier, Amsterdam, The Netherlands) GROUP III: ComprehensiveTM Reverse Shoulder (Biomet Ortho-paedics, LLC, Warsaw, IN) | Humerus retroversion: -group I, 0°, 10°, 20° -group II, 0°, 10°, 20° -group III, 0°, 20°, 30°, 40° | For abduction, group III showed significantly greater mean maximal abduction compared to group II. No significant differences were found between Group I and II. | Humerus retroversion affected both IR and ER, especially in lateralization design (Group II and Group III). |
| Topic | Author, Year | Conclusion |
|---|---|---|
| Impingement and range of movement | Berton et al., 2015 [20] | Anteverted fixation maximized moment arm, but also increased inferior impingement. Moreover, 40° humeral retroversion displayed the largest ROM, while the 20° anteversion showed the smallest one |
| Gulotta el al., 2011 [17] | Placing the implant in 0° to 20° of retroversion maximizes IR with the arm at the side. Concomitant latissimus dorsi transfer is recommended for patients with a deficient teres minor | |
| Henninger et al., 2012 [25] | RTSA reduced ER compared with intact shoulder. Deltoid tension and humeral version had little effect on ER | |
| Kim et al., 2018 [30] | Increasing humeral retroversion increases ER and decreases IR | |
| Kontaxis et al., 2017 [19] | Maximizing ROM by increasing humeral retroversion may not reduce the risk of impingement. An average 0° of humeral version should be preferred | |
| Lanzone et al., 2017 [28] | Restoring glenoid version around 0° yields the most optimal outcomes | |
| Permeswaran et al., 2017 [29] | Retroversion of the glenoid component reduces the risk of subluxation and increases ER and ROM | |
| Stephenson et al., 2011 [26] | Placing humeral component between 20° and 40° of retroversion restores a functional arc of motion without impingement | |
| Muscle forces | Berton et al., 2015 [20] | The 0° and 20° retroversion was the optimum compromise between sufficient teres minor length and moment arm with minimum impingement |
| Gulotta et al., 2011 [17] | Increasing retroversion did not affect the muscle force | |
| Henninger et al., 2012 [25] | Humeral version and implant thickness did not influence abduction forces | |
| Stability | Favre et al., 2010 [18] | Effect of humeral component version was highly significant. Implanting the humeral component in neutral or some anteversion can improve anterior stability |
| Henninger et al., 2012 [25] | Version and deltoid tension did not significantly alter dislocation forces |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berton, A.; Longo, U.G.; Gulotta, L.V.; De Salvatore, S.; Piergentili, I.; Calabrese, G.; Roberti, F.; Warren, R.F.; Denaro, V. Humeral and Glenoid Version in Reverse Total Shoulder Arthroplasty: A Systematic Review. J. Clin. Med. 2022, 11, 7416. https://doi.org/10.3390/jcm11247416
Berton A, Longo UG, Gulotta LV, De Salvatore S, Piergentili I, Calabrese G, Roberti F, Warren RF, Denaro V. Humeral and Glenoid Version in Reverse Total Shoulder Arthroplasty: A Systematic Review. Journal of Clinical Medicine. 2022; 11(24):7416. https://doi.org/10.3390/jcm11247416
Chicago/Turabian StyleBerton, Alessandra, Umile Giuseppe Longo, Lawrence V. Gulotta, Sergio De Salvatore, Ilaria Piergentili, Giovanni Calabrese, Federica Roberti, Russell F. Warren, and Vincenzo Denaro. 2022. "Humeral and Glenoid Version in Reverse Total Shoulder Arthroplasty: A Systematic Review" Journal of Clinical Medicine 11, no. 24: 7416. https://doi.org/10.3390/jcm11247416
APA StyleBerton, A., Longo, U. G., Gulotta, L. V., De Salvatore, S., Piergentili, I., Calabrese, G., Roberti, F., Warren, R. F., & Denaro, V. (2022). Humeral and Glenoid Version in Reverse Total Shoulder Arthroplasty: A Systematic Review. Journal of Clinical Medicine, 11(24), 7416. https://doi.org/10.3390/jcm11247416