Risk Factors and Outcomes of Extended Length of Stay in Older Adults with Intertrochanteric Fracture Surgery: A Retrospective Cohort Study of 2132 Patients
Abstract
1. Introduction
2. Materials and Methods
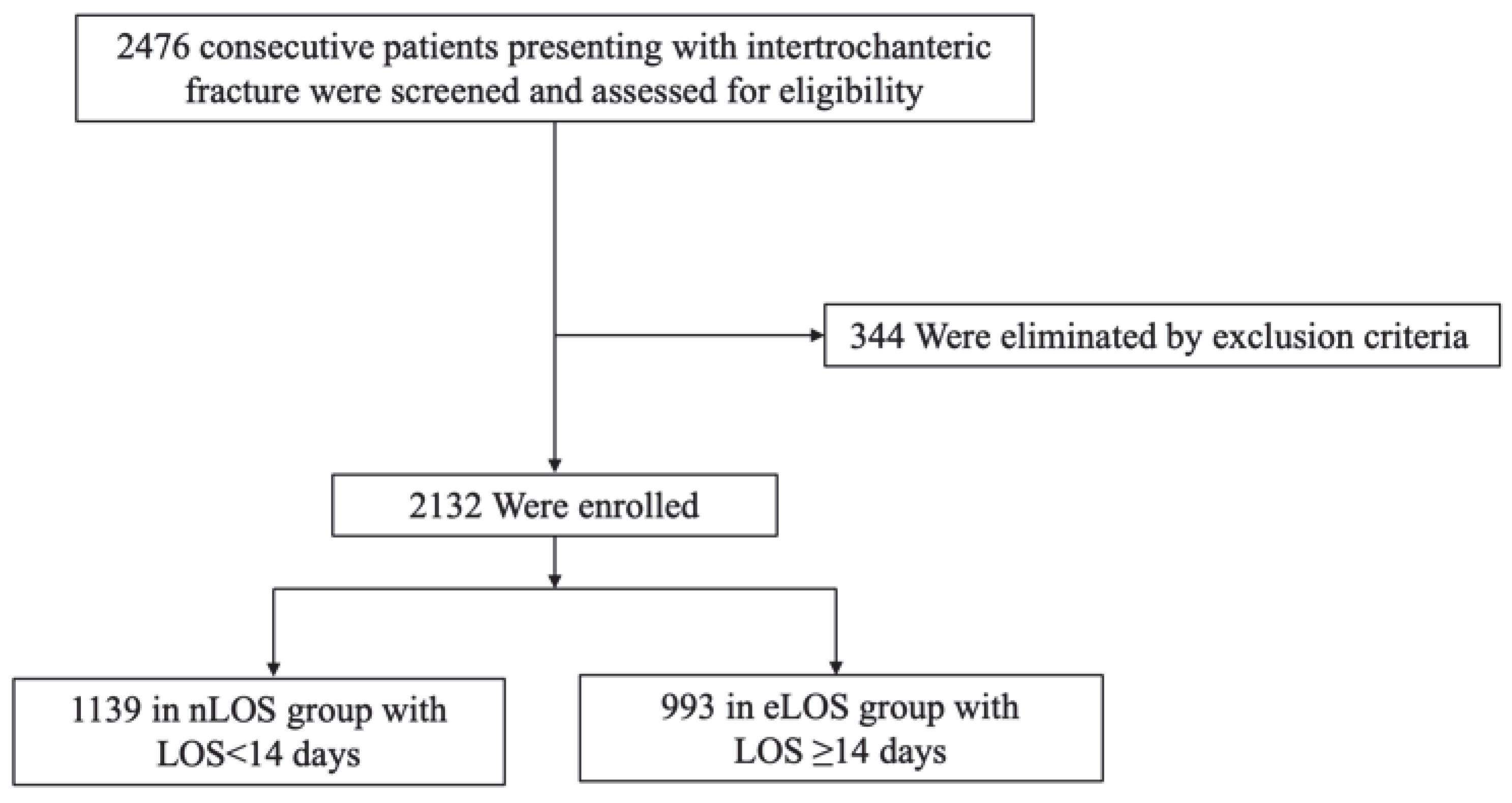
2.1. Study Design, Setting, and Population
2.2. Perioperative Treatment and Surgical Procedure
2.3. Data Collection
2.4. Definitions
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| IF | Intertrochanteric fractures |
| eLOS | Extended length of hospital stay |
| IMN | Intramedullary fixation |
| PFNA | Proximal femoral nail antirotation |
| BMI | Body mass index |
| mECM | Modified Elixhauser comorbidity method |
| NRS | Numerical rating scores |
| GDS | Geriatric Depression Scale |
| FIM | Functional independence measure |
| OR | Odds ratio |
| CI | Confidence interval |
References
- Nazrun, A.S.; Tzar, M.N.; Mokhtar, S.A.; Mohamed, I.N. Systematic review of the outcomes of osteoporotic fracture patients after hospital discharge: Morbidity, subsequent fractures, and mortality. Ther. Clin. Risk Manag. 2014, 10, 937–948. [Google Scholar] [PubMed]
- Zhang, Q.; Wu, Y.; Han, T.; Liu, E. Changes in Cognitive Function and Risk Factors for Cognitive Impairment of the Elderly in China: 2005–2014. Int. J. Environ. Res. Public Health 2019, 16, 2847. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Xu, X.; Zhang, Y.; Hao, H.; Chen, L.; Su, T.; Zhang, Y.; Ma, W.; Xie, Y.; Wang, T.; et al. A model of health education and management for osteoporosis prevention. Exp. Ther. Med. 2016, 12, 3797–3805. [Google Scholar] [CrossRef][Green Version]
- Yoo, J.; Lee, J.S.; Kim, S.; Kim, B.S.; Choi, H.; Song, D.Y.; Kim, W.B.; Won, C.W. Length of hospital stay after hip fracture surgery and 1-year mortality. Osteoporos. Int. 2019, 30, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Zanker, J.; Duque, G. Rapid Geriatric Assessment of Hip Fracture. Clin. Geriatr. Med. 2017, 33, 369–382. [Google Scholar] [CrossRef] [PubMed]
- Braithwaite, R.S.; Col, N.F.; Wong, J.B. Estimating hip fracture morbidity, mortality and costs. J. Am. Geriatr. Soc. 2003, 51, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.A.; Corso, P.S.; Finkelstein, E.A.; Miller, T.R. The costs of fatal and non-fatal falls among older adults. Inj. Prev. 2006, 12, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Burge, R.; Dawson-Hughes, B.; Solomon, D.H.; Wong, J.B.; King, A.; Tosteson, A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J. Bone Miner. Res. 2007, 22, 465–475. [Google Scholar] [CrossRef]
- Schneider, A.M.; Denyer, S.; Brown, N.M. Risk Factors Associated with Extended Length of Hospital Stay after Geriatric Hip Fracture. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2021, 5, e21.00073. [Google Scholar] [CrossRef]
- Garcia, A.E.; Bonnaig, J.V.; Yoneda, Z.T.; Richards, J.E.; Ehrenfeld, J.M.; Obremskey, W.T.; Jahangir, A.A.; Sethi, M.K. Patient variables which may predict length of stay and hospital costs in elderly patients with hip fracture. J. Orthop. Trauma 2012, 26, 620–623. [Google Scholar] [CrossRef]
- Lott, A.; Haglin, J.; Belayneh, R.; Konda, S.R.; Egol, K.A. Admitting Service Affects Cost and Length of Stay of Hip Fracture Patients. Geriatr. Orthop. Surg. Rehabil. 2018, 9, 2151459318808845. [Google Scholar] [CrossRef] [PubMed]
- Kates, S.L.; Blake, D.; Bingham, K.W.; Kates, O.S.; Mendelson, D.A.; Friedman, S.M. Comparison of an organized geriatric fracture program to United States government data. Geriatr. Orthop. Surg. Rehabil. 2010, 1, 15–21. [Google Scholar] [CrossRef]
- Malik, A.T.; Khan, S.N.; Ly, T.V.; Phieffer, L.; Quatman, C.E. The “Hip Fracture” Bundle-Experiences, Challenges, and Opportunities. Geriatr. Orthop. Surg. Rehabil. 2020, 11, 2151459320910846. [Google Scholar] [CrossRef]
- Mechanic, R.; Tompkins, C. Lessons learned preparing for Medicare bundled payments. N. Engl. J. Med. 2012, 367, 1873–1875. [Google Scholar] [CrossRef] [PubMed]
- Burgers, P.T.; Van Lieshout, E.M.; Verhelst, J.; Dawson, I.; de Rijcke, P.A. Implementing a clinical pathway for hip fractures; effects on hospital length of stay and complication rates in five hundred and twenty six patients. Int. Orthop. 2014, 38, 1045–1050. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lau, T.W.; Fang, C.; Leung, F. The effectiveness of a geriatric hip fracture clinical pathway in reducing hospital and rehabilitation length of stay and improving short-term mortality rates. Geriatr. Orthop. Surg. Rehabil. 2013, 4, 3–9. [Google Scholar] [CrossRef]
- Brown, C.A.; Olson, S.; Zura, R. Predictors of length of hospital stay in elderly hip fracture patients. J. Surg. Orthop. Adv. 2013, 22, 160–163. [Google Scholar] [CrossRef]
- Ireland, A.W.; Kelly, P.J.; Cumming, R.G. Total hospital stay for hip fracture: Measuring the variations due to pre-fracture residence, rehabilitation, complications and comorbidities. BMC Health Serv. Res. 2015, 15, 17. [Google Scholar] [CrossRef][Green Version]
- Lefaivre, K.A.; Macadam, S.A.; Davidson, D.J.; Gandhi, R.; Chan, H.; Broekhuyse, H.M. Length of stay, mortality, morbidity and delay to surgery in hip fractures. J. Bone Jt. Surg. Br. 2009, 91, 922–927. [Google Scholar] [CrossRef]
- Greenberg, S.E.; VanHouten, J.P.; Lakomkin, N.; Ehrenfeld, J.; Jahangir, A.A.; Boyce, R.H.; Obremksey, W.T.; Sethi, M.K. Does Admission to Medicine or Orthopaedics Impact a Geriatric Hip Patient’s Hospital Length of Stay? J. Orthop. Trauma 2016, 30, 95–99. [Google Scholar] [CrossRef]
- Eschbach, D.A.; Oberkircher, L.; Bliemel, C.; Mohr, J.; Ruchholtz, S.; Buecking, B. Increased age is not associated with higher incidence of complications, longer stay in acute care hospital and in hospital mortality in geriatric hip fracture patients. Maturitas 2013, 74, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Fu, M.; Zhang, Y.; Guo, J.; Zhao, Y.; Hou, Z.; Wang, Z.; Zhang, Y. Application of integrated management bundle incorporating with multidisciplinary measures improved in-hospital outcomes and early survival in geriatric hip fracture patients with perioperative heart failure: A retrospective cohort study. Aging Clin. Exp. Res. 2022, 34, 1149–1158. [Google Scholar] [CrossRef]
- Downie, W.W.; Leatham, P.A.; Rhind, V.M.; Wright, V.; Branco, J.A.; Anderson, J.A. Studies with pain rating scales. Ann. Rheum. Dis. 1978, 37, 378–381. [Google Scholar] [CrossRef] [PubMed]
- Price, D.D.; Bush, F.M.; Long, S.; Harkins, S.W. A comparison of pain measurement characteristics of mechanical visual analogue and simple numerical rating scales. Pain 1994, 56, 217–226. [Google Scholar] [CrossRef]
- Schreiner, A.S.; Hayakawa, H.; Morimoto, T.; Kakuma, T. Screening for late life depression: Cut-off scores for the Geriatric Depression Scale and the Cornell Scale for Depression in Dementia among Japanese subjects. Int. J. Geriatr. Psychiatry 2003, 18, 498–505. [Google Scholar] [CrossRef]
- Goto, K.; Kataoka, H.; Honda, A.; Yamashita, J.; Morita, K.; Hirase, T.; Sakamoto, J.; Okita, M. Factors Affecting Persistent Postoperative Pain in Patients with Hip Fractures. Pain Res. Manag. 2020, 2020, 8814290. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Wang, Z.; Fu, M.; Di, J.; Zha, J.; Liu, J.; Zhang, G.; Wang, Q.; Chen, H.; Tang, P.; et al. Super elderly patients with intertrochanteric fractures do not predict worse outcomes and higher mortality than elderly patients: A propensity score matched analysis. Aging 2020, 12, 13583–13593. [Google Scholar] [CrossRef]
- Knoll, O.M.; Lakomkin, N.; Shen, M.S.; Adebayo, M.; Kothari, P.; Dodd, A.C.; Attum, B.; Lee, N.; Chona, D.; Sethi, M.K. A predictive model for increased hospital length of stay following geriatric hip fracture. J. Clin. Orthop. Trauma 2019, 10 (Suppl. 1), S84–S87. [Google Scholar] [CrossRef] [PubMed]
- Tomioka, S.; Rosenberg, M.; Fushimi, K.; Matsuda, S. An analysis of equity in treatment of hip fractures for older patients with dementia in acute care hospitals: Observational study using nationwide hospital claims data in Japan. BMC Health Serv. Res. 2020, 20, 830. [Google Scholar] [CrossRef]
- Gil, L.A.; Kothari, A.N.; Brownlee, S.A.; Ton-That, H.; Patel, P.P.; Gonzalez, R.P.; Luchette, F.A.; Anstadt, M.A. Superusers: Drivers of health care resource utilization in the national trauma population. Surgery 2018, 164, 848–855. [Google Scholar] [CrossRef]
- Pincus, D.; Wasserstein, D.; Ravi, B.; Huang, A.; Paterson, J.M.; Jenkinson, R.J.; Kreder, H.J.; Nathens, A.B.; Wodchis, W.B. Medical Costs of Delayed Hip Fracture Surgery. J. Bone Jt. Surg. Am. 2018, 100, 1387–1396. [Google Scholar] [CrossRef] [PubMed]
- Hecht, G.; Slee, C.A.; Goodell, P.B.; Taylor, S.L.; Wolinsky, P.R. Predictive Modeling for Geriatric Hip Fracture Patients: Early Surgery and Delirium Have the Largest Influence on Length of Stay. J. Am. Acad. Orthop. Surg. 2019, 27, e293–e300. [Google Scholar] [CrossRef] [PubMed]
- Bohl, D.D.; Sershon, R.A.; Saltzman, B.M.; Darrith, B.; Della Valle, C.J. Incidence, Risk Factors, and Clinical Implications of Pneumonia after Surgery for Geriatric Hip Fracture. J. Arthroplast. 2018, 33, 1552–1556.e1. [Google Scholar] [CrossRef] [PubMed]
- Lagoe, R.J.; Johnson, P.E.; Murphy, M.P. Inpatient hospital complications and lengths of stay: A short report. BMC Res. Notes 2011, 4, 135. [Google Scholar] [CrossRef] [PubMed]
- Ricci, W.M.; Brandt, A.; McAndrew, C.; Gardner, M.J. Factors affecting delay to surgery and length of stay for patients with hip fracture. J. Orthop. Trauma 2015, 29, e109–e114. [Google Scholar] [CrossRef]
- Basques, B.A.; Bohl, D.D.; Golinvaux, N.S.; Leslie, M.P.; Baumgaertner, M.R.; Grauer, J.N. Postoperative length of stay and 30-day readmission after geriatric hip fracture: An analysis of 8434 patients. J. Orthop. Trauma 2015, 29, e115–e120. [Google Scholar] [CrossRef]
- Narita, K.; Hoshide, S.; Kario, K. Seasonal variation in blood pressure: Current evidence and recommendations for hypertension management. Hypertens. Res. 2021, 44, 1363–1372. [Google Scholar] [CrossRef]
- Arntz, H.R.; Willich, S.N.; Schreiber, C.; Brüggemann, T.; Stern, R.; Schultheiss, H.P. Diurnal, weekly and seasonal variation of sudden death. Population-based analysis of 24,061 consecutive cases. Eur. Heart J. 2000, 21, 315–320. [Google Scholar] [CrossRef]
- Pan, W.H.; Li, L.A.; Tsai, M.J. Temperature extremes and mortality from coronary heart disease and cerebral infarction in elderly Chinese. Lancet 1995, 345, 353–355. [Google Scholar] [CrossRef]
- Spencer, F.A.; Goldberg, R.J.; Becker, R.C.; Gore, J.M. Seasonal distribution of acute myocardial infarction in the second National Registry of Myocardial Infarction. J. Am. Coll. Cardiol. 1998, 31, 1226–1233. [Google Scholar] [CrossRef]
- Kaneko, H.; Suzuki, S.; Goto, M.; Arita, T.; Yuzawa, Y.; Yagi, N.; Murata, N.; Yajima, J.; Oikawa, Y.; Sagara, K.; et al. Presentations and outcomes of patients with acute decompensated heart failure admitted in the winter season. J. Cardiol. 2014, 64, 470–475. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kloner, R.A. Natural and unnatural triggers of myocardial infarction. Prog. Cardiovasc. Dis. 2006, 48, 285–300. [Google Scholar] [CrossRef] [PubMed]
- Argilés, A.; Mourad, G.; Mion, C. Seasonal changes in blood pressure in patients with end-stage renal disease treated with hemodialysis. N. Engl. J. Med. 1998, 339, 1364–1370. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, T.; Yoshii, T.; Higuchi, M.; Morishita, S.; Fushimi, K.; Fujiwara, T.; Okawa, A. Seasonality of mortality and in-hospital complications in hip fracture surgery: Retrospective cohort research using a nationwide inpatient database. Geriatr. Gerontol. Int. 2021, 21, 398–403. [Google Scholar] [CrossRef]
- Ogawa, T.; Yoshii, T.; Morishita, S.; Moriwaki, M.; Okawa, A.; Nazarian, A.; Fushimi, K.; Fujiwara, T. Seasonal impact on surgical site infections in hip fracture surgery: Analysis of 330,803 cases using a nationwide inpatient database. Injury 2021, 52, 898–904. [Google Scholar] [CrossRef]
- Kazaure, H.S.; Martin, M.; Yoon, J.K.; Wren, S.M. Long-term results of a postoperative pneumonia prevention program for the inpatient surgical ward. JAMA Surg. 2014, 149, 914–918. [Google Scholar] [CrossRef]
- Alvi, H.M.; Thompson, R.M.; Krishnan, V.; Kwasny, M.J.; Beal, M.D.; Manning, D.W. Time-to-Surgery for Definitive Fixation of Hip Fractures: A Look at Outcomes Based Upon Delay. Am. J. Orthop. 2018, 47, 71. [Google Scholar] [CrossRef][Green Version]
| Variables | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| Total (n = 2132) | nLOS (n = 1139) | eLOS (n = 993) | p-Value a | OR (95%CI) | p-Value b | |
| Demographics | ||||||
| Gender, n (%) | 0.893 | |||||
| Male | 688 (32.3%) | 369 (32.4%) | 319 (32.1%) | Reference | ||
| Female | 1444 (67.7%) | 770 (67.6%) | 674 (67.9%) | 0.939 (0.766, 1.150) | 0.541 | |
| Age, years | 79.0 ± 7.2 | 79.1 ± 7.3 | 79.0 ±7.1 | 0.724 | 1.016 (0.980, 1.053) | 0.391 |
| Age group, n (%) | 0.471 | |||||
| 65–69 | 234 (11.0%) | 122 (10.7%) | 112 (11.3%) | Reference | ||
| 70–79 | 851 (39.9%) | 450 (39.5%) | 401 (40.4%) | 0.913 (0.598, 1.394) | 0.674 | |
| 80–89 | 894 (41.9%) | 485 (42.6%) | 409 (41.2%) | 0.714 (0.364, 1.402) | 0.328 | |
| 90–99 | 146 (6.8%) | 76 (6.7%) | 70 (7.0%) | 0.681 (0.252, 1.842) | 0.449 | |
| ≥100 | 7 (0.4%) | 6 (0.5%) | 1 (0.1%) | 0.118 (0.010, 1.429) | 0.093 | |
| BMI, kg/m2, n (%) | 0.076 * | |||||
| Normal (BMI < 24) | 1390 (65.2%) | 757 (66.5%) | 633 (63.7%) | Reference | ||
| Overweight (24 ≤ BMI < 28) | 580 (27.2%) | 309 (27.1%) | 271 (27.3%) | 1.037 (0.836, 1.285) | 0.742 | |
| Obesity (BMI ≥ 28) | 162 (7.6%) | 73 (6.4%) | 89 (9.0%) | 1.654 (1.153, 2.373) | 0.006 * | |
| Residence, n (%) | 0.001 ** | |||||
| Rural | 749 (35.1%) | 437 (38.4%) | 312 (31.4%) | Reference | ||
| Urban | 1383 (64.9%) | 702 (61.6%) | 681 (68.6%) | 1.512 (1.243, 1,840) | <0.001 * | |
| Smoking status, n (%) | 0.939 | |||||
| Never | 1757 (82.4%) | 941 (82.6%) | 816 (82.1%) | |||
| Past | 157 (7.4%) | 84 (7.4%) | 73 (7.4%) | |||
| Current | 218 (10.2%) | 114 (10.0%) | 104 (10.5%) | |||
| Drinking status, n (%) | 0.990 | |||||
| Current | 86 (4.0%) | 46 (4.0%) | 40 (4.0%) | |||
| Never | 2046 (96.0%) | 1093 (96.0%) | 953 (96.0%) | |||
| Surgery-related indicators | ||||||
| Fracture type, n (%) | 0.143 | |||||
| Stable (A1.1–A2.1) | 1159 (54.4%) | 636 (55.8%) | 523 (52.7%) | |||
| Unstable (A2.2–A3.3) | 973 (45.6%) | 503 (44.2%) | 470 (47.3%) | |||
| Time from injury to surgery, days | 6.0 ± 3.1 | 4.9 ± 2.1 | 7.2 ± 3.6 | <0.001 ** | 1.342 (1.293, 1.394) | <0.001 * |
| mECM, n (%) | 0.010 ** | |||||
| <0 | 44 (2.1%) | 30 (2.6%) | 14 (1.4%) | Reference | ||
| 0 | 1077 (50.5%) | 596 (52.3%) | 481 (48.4%) | 2.299 (1,145, 4.615) | 0.019 * | |
| 1–5 | 349 (16.4%) | 182 (16.0%) | 167 (16.8%) | 1.935 (1.332, 3.973) | 0.022 * | |
| 6–13 | 580 (27.2%) | 299 (26.3%) | 281 (28.3%) | 2.071 (1.021, 4.199) | 0.044 * | |
| ≥14 | 82 (3.8%) | 32 (2.8%) | 50 (5.1%) | 2.958 (1.277, 6.854) | 0.011 * | |
| Type of anesthesia, n (%) | 0.249 | |||||
| General | 799 (37.5%) | 414 (36.3%) | 385 (38.8%) | |||
| Regional | 1333 (62.5%) | 725 (63.7%) | 608 (61.2%) | |||
| Duration of operation, min | 99.3 ± 34.9 | 98.3 ± 34.2 | 100.4 ± 35.7 | 0.158 | ||
| Intraoperative blood loss, mL | 238.5 ± 158.1 | 229.0 ± 159.6 | 249.4 ± 155.7 | 0.003 ** | 1.000 (1.000, 1.001) | 0.241 |
| Periopertive clinical indicators | ||||||
| NRS | 5.3 ± 1.8 | 5.4 ± 1.8 | 5.2 ± 1.8 | 0.041 ** | 0.982 (0.931, 1.036) | 0.504 |
| GDS | 4.1 ± 1.4 | 4.1 ± 1.4 | 4.1 ± 1.4 | 0.995 | ||
| FIM | 83.7 ± 10.4 | 83.8 ± 10.5 | 83.6 ± 10.2 | 0.646 | ||
| Anxiety, n (%) | 0.181 | |||||
| No | 1737 (81.5%) | 916 (80.4%) | 821 (82.7%) | |||
| Yes | 395 (18.5%) | 223 (19.6%) | 172 (17.3%) | |||
| Hb level at admission, g/dL | 0.718 | |||||
| Hb ≥ 12 | 625 (29.3%) | 338 (29.7%) | 287 (28.9%) | |||
| 12 > Hb ≥ 10 | 885 (41.5%) | 475 (41.7%) | 410 (41.3%) | |||
| 10 > Hb ≥ 8 | 512 (24.0%) | 273 (24.0%) | 239 (24.1%) | |||
| Hb < 8 | 110 (5.2%) | 53 (4.6%) | 57 (5.7%) | |||
| Blood transfusion, n (%) | 0.001 ** | |||||
| No | 515 (24.2%) | 308 (27.0%) | 207 (20.8%) | Reference | ||
| Yes | 1617 (75.8%) | 831 (73.0%) | 786 (79.2%) | 1.203 (0.952, 1.519) | 0.121 | |
| Season of admission, n (%) | 0.013 ** | |||||
| Spring | 548 (25.7%) | 301 (26.4%) | 247 (24.9%) | 1.107 (0.847, 1.448) | 0.456 | |
| Summer | 484 (22.7%) | 285 (25.0%) | 199 (20.0%) | Reference | ||
| Autumn | 533 (25.0%) | 270 (23.7%) | 263 (26.5%) | 1.390 (1.063, 1.818) | 0.016 * | |
| Winter | 567 (26.6%) | 283 (24.8%) | 284 (28.6%) | 1.547 (1.186, 2.019) | 0.001 * | |
| Complications during hospitalization, n (%) | ||||||
| Severe complications | 0.127 | |||||
| No | 1780 (83.5%) | 964 (84.6%) | 816 (82.2%) | |||
| Yes | 352 (16.5%) | 175 (15.4%) | 177 (17.8%) | |||
| Cardiac complications | 0.070 * | |||||
| No | 1652 (77.5%) | 900 (79.0%) | 752 (75.7%) | Reference | ||
| Yes | 480 (22.5%) | 239 (21.0%) | 241 (24.3%) | 0.995 (0.788, 1.255) | 0.964 | |
| Pulmonary complications | 0.005 ** | |||||
| No | 1926 (90.3%) | 1048 (92.0%) | 878 (88.4%) | Reference | ||
| Yes | 206 (9.7%) | 91 (8.0%) | 115 (11.6%) | 1.451 (1.057, 1.991) | 0.021 * | |
| Neurological complications | 0.277 | |||||
| No | 1964 (92.1%) | 1056 (92.7%) | 908 (91.4%) | |||
| Yes | 168 (7.9%) | 83 (7.3%) | 85 (8.6%) | |||
| Hematological complications | 0.021 ** | |||||
| No | 1216 (57.0%) | 676 (59.4%) | 540 (54.4%) | Reference | ||
| Yes | 916 (43.0%) | 463 (40.6%) | 453 (45.6%) | 1.060 (0.877, 1.281) | 0.545 | |
| Endocrine/metabolic complications | 0.712 | |||||
| No | 659 (30.9%) | 356 (31.3%) | 303 (30.5%) | |||
| Yes | 1473 (69.1%) | 783 (68.7%) | 690 (69.5%) | |||
| Variables | Total (n = 2132) | nLOS (n = 1139) | eLOS (n = 993) | p-Value |
|---|---|---|---|---|
| Mortality rates (n, %) | ||||
| 1 month | 17 (0.8%) | 6 (0.5%) | 11 (1.1%) | 0.132 |
| 1–3 months | 22 (1.0%) | 11 (1.0%) | 11 (1.1%) | 0.736 |
| 3–6 months | 27 (1.3%) | 17 (1.5%) | 10 (1.0%) | 0.327 |
| 6–12 months | 71 (3.4%) | 40 (3.6%) | 31 (3.2%) | 0.624 |
| 12–24 months | 118 (5.9%) | 65 (6.1%) | 53 (5.7%) | 0.703 |
| Functional Outcomes (n, %) | 0.408 | |||
| Independent walking | 768 (36.0%) | 427 (37.5%) | 341 (34.3%) | |
| Use of walking aids | 660 (31.0%) | 343 (30.1%) | 317 (31.9%) | |
| Use of wheelchair | 133 (6.2%) | 76 (6.7%) | 57 (5.7%) | |
| Bedridden | 84 (3.9%) | 45 (4.0%) | 39 (3.9%) | |
| Death | 487 (22.9%) | 248 (21.7%) | 239 (24.2%) | |
| Destination after discharge (n, %) | 0.027 * | |||
| Home | 1548 (72.6%) | 855 (75.1%) | 693 (69.8%) | |
| Other hospitals | 150 (7.0%) | 78 (6.8%) | 72 (7.3%) | |
| Rehabilitation facilities | 245 (11.5%) | 121 (10.6%) | 124 (12.5%) | |
| Nursing homes | 189 (8.9%) | 85 (7.5%) | 104 (10.5%) |
| Variables | eLOS | |||
|---|---|---|---|---|
| Uncontrol for mECM | Control for mECM | |||
| Spearman’s r Statistic | p-Value | Partial Correlation Coefficient | p-Value | |
| BMI | −0.021 | 0.333 | −0.018 | 0.418 |
| Residence | 0.073 | 0.001 * | 0.073 | 0.001 * |
| Time from injury to surgery | 0.328 | <0.001 * | 0.358 | <0.001 * |
| Season of admission | 0.052 | 0.017 * | 0.051 | 0.018 * |
| Pulmonary complications | 0.061 | 0.005 * | 0.057 | 0.009 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Long, Y.; Wang, T.; Xu, X.; Ran, G.; Zhang, H.; Dong, Q.; Zhang, Q.; Guo, J.; Hou, Z. Risk Factors and Outcomes of Extended Length of Stay in Older Adults with Intertrochanteric Fracture Surgery: A Retrospective Cohort Study of 2132 Patients. J. Clin. Med. 2022, 11, 7366. https://doi.org/10.3390/jcm11247366
Long Y, Wang T, Xu X, Ran G, Zhang H, Dong Q, Zhang Q, Guo J, Hou Z. Risk Factors and Outcomes of Extended Length of Stay in Older Adults with Intertrochanteric Fracture Surgery: A Retrospective Cohort Study of 2132 Patients. Journal of Clinical Medicine. 2022; 11(24):7366. https://doi.org/10.3390/jcm11247366
Chicago/Turabian StyleLong, Yubin, Tao Wang, Xin Xu, Guangyuan Ran, Heng Zhang, Qi Dong, Qi Zhang, Junfei Guo, and Zhiyong Hou. 2022. "Risk Factors and Outcomes of Extended Length of Stay in Older Adults with Intertrochanteric Fracture Surgery: A Retrospective Cohort Study of 2132 Patients" Journal of Clinical Medicine 11, no. 24: 7366. https://doi.org/10.3390/jcm11247366
APA StyleLong, Y., Wang, T., Xu, X., Ran, G., Zhang, H., Dong, Q., Zhang, Q., Guo, J., & Hou, Z. (2022). Risk Factors and Outcomes of Extended Length of Stay in Older Adults with Intertrochanteric Fracture Surgery: A Retrospective Cohort Study of 2132 Patients. Journal of Clinical Medicine, 11(24), 7366. https://doi.org/10.3390/jcm11247366







