Reliability of 3D Stereophotogrammetry for Measuring Postoperative Facial Swelling
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Measurements
2.3. Data Processing
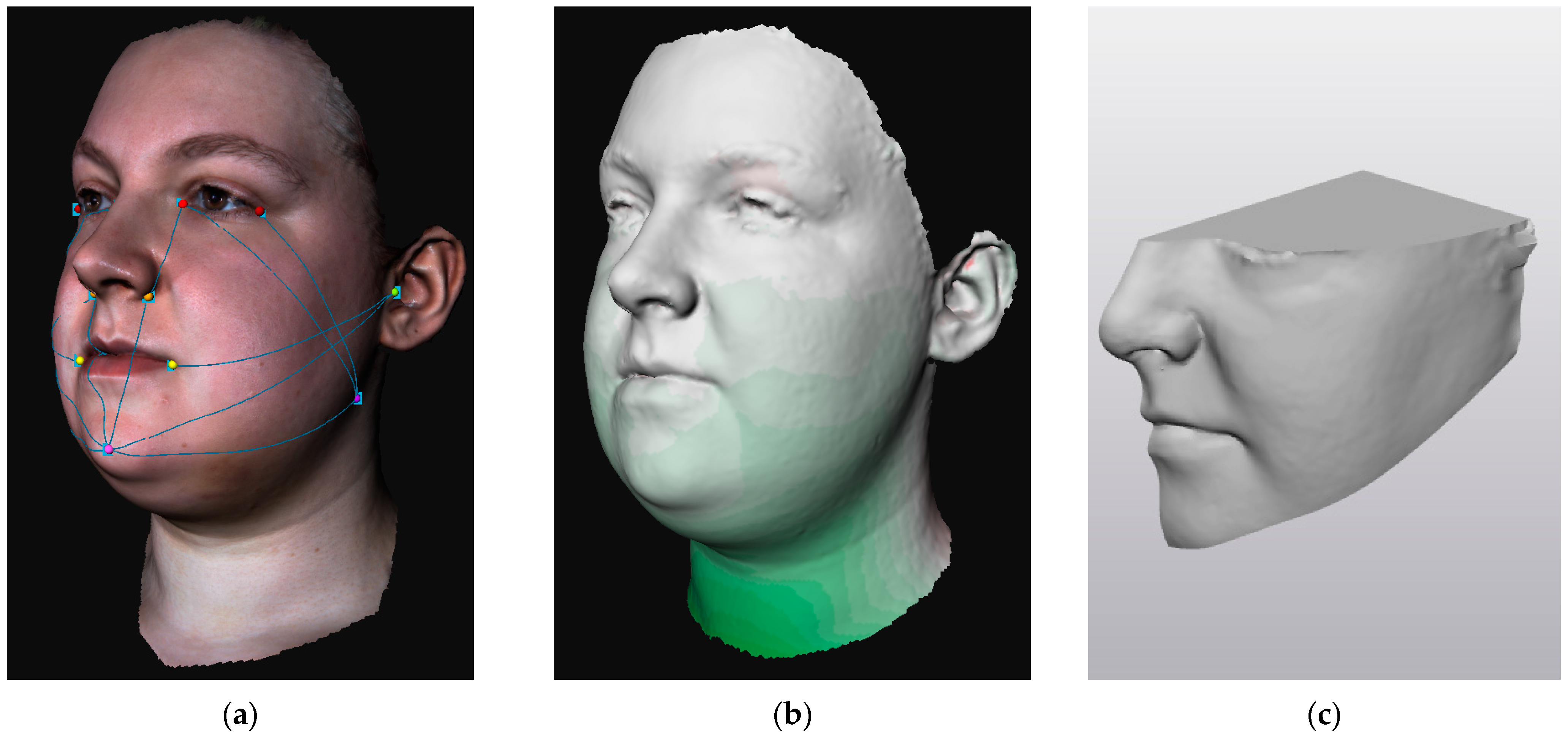
2.3.1. Distance Measurements
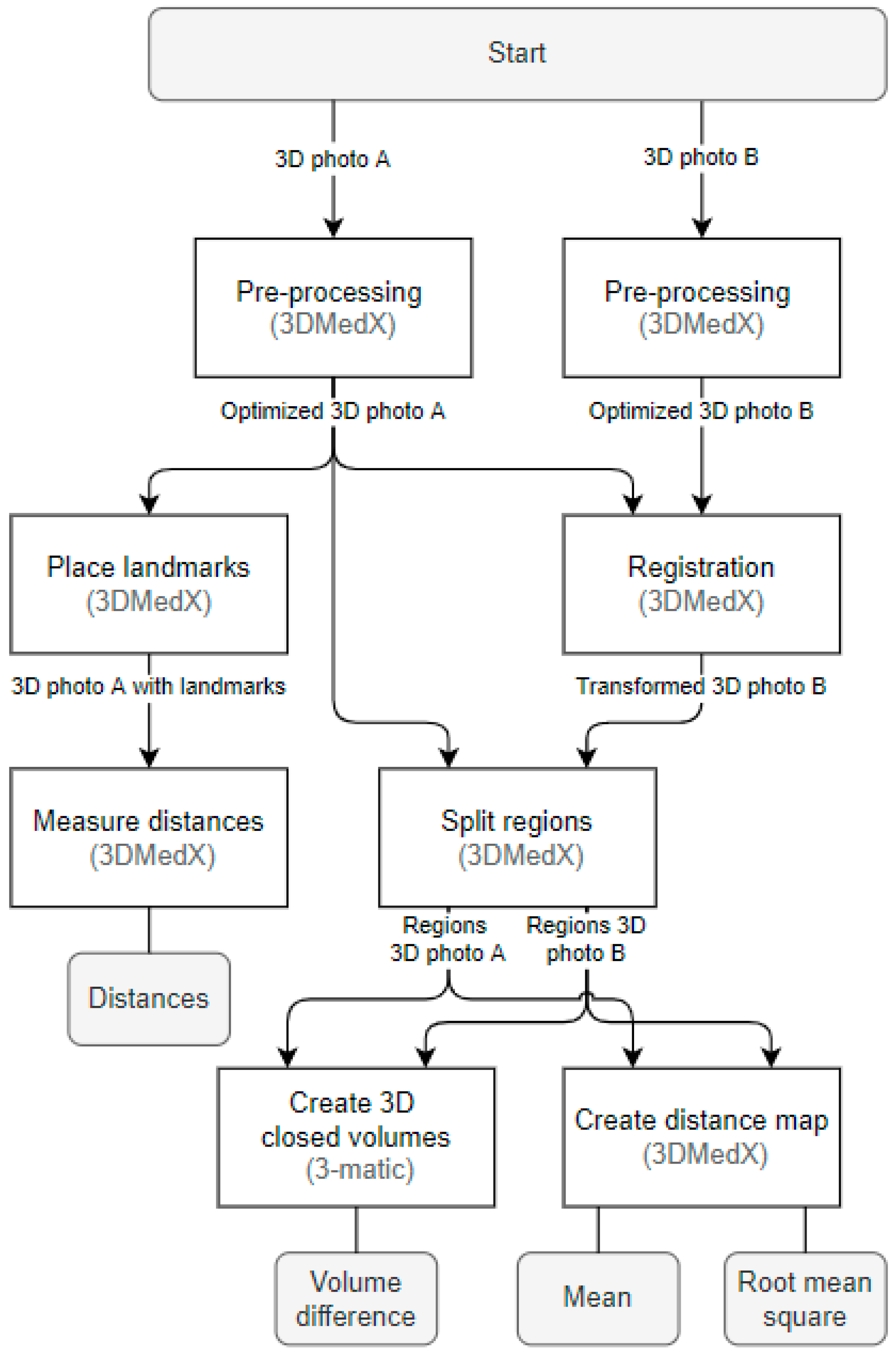
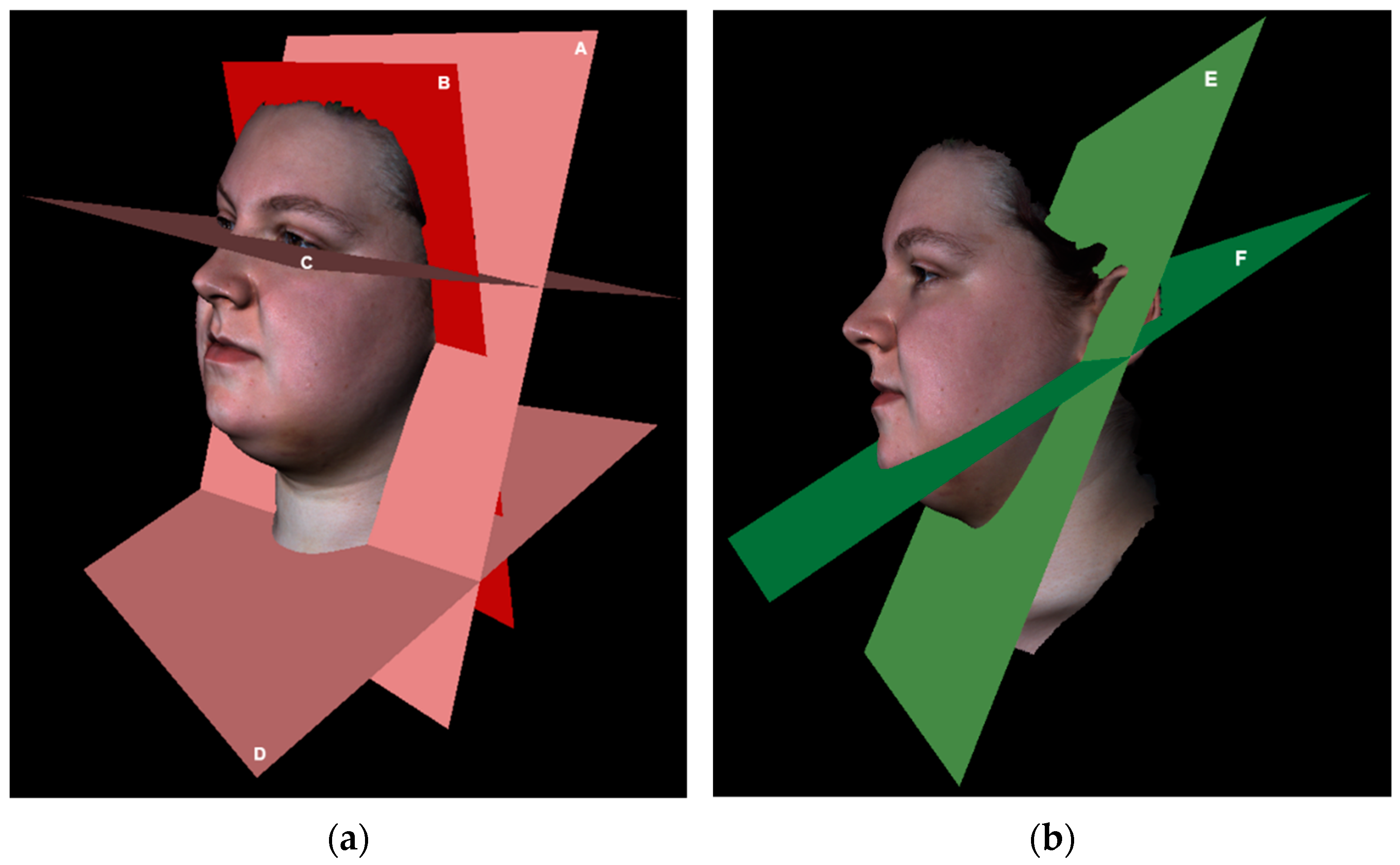
2.3.2. Registration and Region Splitting
2.3.3. Distance Map Parameters
2.3.4. Volume Differences
2.3.5. Reliability
2.4. Statistical Analysis
3. Results
4. Discussion
4.1. Strengths and Limitations
4.2. Clinical Implications
4.3. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rana, M.; Gellrich, N.C.; Joos, U.; Piffkó, J.; Kater, W. 3D Evaluation of Postoperative Swelling Using Two Different Cooling Methods Following Orthognathic Surgery: A Randomised Observer Blind Prospective Pilot Study. Int. J. Oral Maxillofac. Surg. 2011, 40, 690–696. [Google Scholar] [CrossRef] [PubMed]
- Van der Vlis, M.; Dentino, K.M.; Vervloet, B.; Padwa, B.L. Postoperative Swelling after Orthognathic Surgery: A Prospective Volumetric Analysis. J. Oral Maxillofac. Surg. 2014, 72, 2241–2247. [Google Scholar] [CrossRef]
- Koçer, G.; Sönmez, S.; Findik, Y.; Yazici, T. Reliability of the Linear Measurement (Contact) Method Compared with Stereophotogrammetry (Optical Scanning) for the Evaluation of Edema after Surgically Assisted Rapid Maxillary Expansion. Healthcare 2020, 8, 52. [Google Scholar] [CrossRef]
- Semper-Hogg, W.; Fuessinger, M.A.; Dirlewanger, T.W.; Cornelius, C.P.; Metzger, M.C. The Influence of Dexamethasone on Postoperative Swelling and Neurosensory Disturbances after Orthognathic Surgery: A Randomized Controlled Clinical Trial. Head Face Med. 2017, 13, 19. [Google Scholar] [CrossRef] [PubMed]
- Lietz-Kijak, D.; Kijak, E.; Krajczy, M.; Bogacz, K.; Łuniewski, J.; Szczegielniak, J. The Impact of the Use of Kinesio Taping Method on the Reduction of Swelling in Patients after Orthognathic Surgery: A Pilot Study. Med. Sci. Monit. 2018, 24, 3736–3743. [Google Scholar] [CrossRef]
- Yaedú, R.Y.F.; Mello, M.D.A.B.; Tucunduva, R.A.; Da Silveira, J.S.Z.; Takahashi, M.P.M.S.; Valente, A.C.B. Postoperative Orthognathic Surgery Edema Assessment with and Without Manual Lymphatic Drainage. J. Craniofac. Surg. 2017, 28, 1816–1820. [Google Scholar] [CrossRef]
- Tozzi, U.; Santagata, M.; Sellitto, A.; Tartaro, G.P. Influence of Kinesiologic Tape on Post-Operative Swelling After Orthognathic Surgery. J. Maxillofac. Oral Surg. 2016, 15, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Gasperini, G.; Rodrigues De Siqueira, I.C.; Rezende Costa, L. Does Low-Level Laser Therapy Decrease Swelling and Pain Resulting from Orthognathic Surgery? Int. J. Oral Maxillofac. Surg. 2014, 43, 868–873. [Google Scholar] [CrossRef]
- Kau, C.H.; Cronin, A.; Durning, P.; Zhurov, A.I.; Richmond, S.; Sandham, A. A New Method for the 3D Measurement of Postoperative Swelling Following Orthognathic Surgery. Orthod. Craniofacial Res. 2006, 9, 31–37. [Google Scholar] [CrossRef]
- Maal, T.J.J.; Verhamme, L.M.; Van Loon, B.; Plooij, J.M.; Rangel, F.A.; Kho, A.; Bronkhorst, E.M.; Bergé, S.J. Variation of the Face in Rest Using 3D Stereophotogrammetry. Int. J. Oral Maxillofac. Surg. 2011, 40, 1252–1257. [Google Scholar] [CrossRef]
- Van der Meer, W.J.; Dijkstra, P.U.; Visser, A.; Vissink, A.; Ren, Y. Reliability and Validity of Measurements of Facial Swelling with a Stereophotogrammetry Optical Three-Dimensional Scanner. Br. J. Oral Maxillofac. Surg. 2014, 52, 922–927. [Google Scholar] [CrossRef] [PubMed]
- Ullah, R.; Turner, P.J.; Khambay, B.S. Accuracy of Three-Dimensional Soft Tissue Predictions in Orthognathic Surgery after Le Fort I Advancement Osteotomies. Br. J. Oral Maxillofac. Surg. 2015, 53, 153–157. [Google Scholar] [CrossRef] [PubMed]
- De Vet, H.C.W.; Terwee, C.B.; Mokkink, L.B.; Knol, D.L. Reliability. In Measurement in Medicine: A Practical Guide; Cambridge University Press: Cambridge, UK, 2011; pp. 96–149. ISBN 9780511996214. [Google Scholar]
- Böckmann, R.; Meyns, J.; Dik, E.; Kessler, P. The Modifications of the Sagittal Ramus Split Osteotomy: A Literature Review. Plast. Reconstr. Surg.-Glob. Open 2014, 2, e271. [Google Scholar] [CrossRef]
- Chiu, C.S.W.; Clark, R.K.F. Reproducibility of Natural Head Position. J. Dentristy 1991, 19, 130–131. [Google Scholar] [CrossRef]
- Smith, B.G.; Lewin, J.S. The Role of Lymphedema Management in Head and Neck Cancer. Curr. Opin. Otolaryngol. Head Neck Surg. 2010, 18, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Plooij, J.M.; Swennen, G.R.J.; Rangel, F.A.; Maal, T.J.J.; Schutyser, F.A.C.; Bronkhorst, E.M.; Kuijpers-Jagtman, A.M.; Bergé, S.J. Evaluation of Reproducibility and Reliability of 3D Soft Tissue Analysis Using 3D Stereophotogrammetry. Int. J. Oral Maxillofac. Surg. 2009, 38, 267–273. [Google Scholar] [CrossRef]
- Gwilliam, J.R.; Cunningham, S.J.; Hutton, T. Reproducibility of Soft Tissue Landmarks on Three-Dimensional Facial Scans. Eur. J. Orthod. 2006, 28, 408–415. [Google Scholar] [CrossRef]
- Aldridge, K.; Boyadjiev, S.A.; Capone, G.T.; Deleon, V.B.; Richtsmeier, J.T. Precision and Error of Three-Dimensional Phenotypic Measures Acquired from 3dMD Photogrammetric Images. Am. J. Med. Genet. 2005, 138A, 247–253. [Google Scholar] [CrossRef]
- Hajeer, M.Y.; Ayoub, A.F.; Millett, D.T.; Bock, M.; Siebert, J.P. Three-Dimensional Imaging in Orthognathic Surgery: The Clinical Application of a New Method. Int. J. Adult Orthodon. Orthognath. Surg. 2002, 17, 318–330. [Google Scholar] [PubMed]
- Walter, S.D.; Eliasziw, M.; Donner, A. Sample Size and Optimal Designs for Reliability Studies. Stat. Med. 1998, 17, 101–110. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Weier, J.P. Quantifying Test-Retest Reliability Using the Intraclass Correlation Coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231–240. [Google Scholar] [CrossRef]
- Mehta, S.; Bastero-Caballero, R.F.; Sun, Y.; Zhu, R.; Murphy, D.K.; Hardas, B.; Koch, G. Performance of Intraclass Correlation Coefficient (ICC) as a Reliability Index under Various Distributions in Scale Reliability Studies. Stat. Med. 2018, 37, 2734–2752. [Google Scholar] [CrossRef] [PubMed]
| Landmark | Abbreviation | Explanation | Precision |
|---|---|---|---|
| Alare | A | The most lateral point on the alar contour. | Moderate [17,18] to good [19,20] |
| Cheilion | Ch | The point located at the labial commissure. | Very good [19,20] |
| Endocanthion | En | The soft tissue point at the inner commissure of the eye fissure. | Good [20] to very good [17,19] |
| Exocanthion | Ex | The soft tissue point at the outer commissure of the eye fissure. | Good [19,20] to very good [17,18] |
| Soft tissue gonion | Go’ | The most posterior inferior point of the soft tissue over the angle of the mandible. Can also be constructed by bisecting the angle formed by the intersection of the mandibular plane and ramus of the mandible. | Poor [17,18,19,20] |
| Soft tissue hyoid | H’ | The soft tissue midpoint at the transition between head and neck. | Not available * |
| Neck inferior | Ninf | Most inferior point of the (included) neck area, following skin tension lines. | Not available * |
| Neck middle | Nmid | The midpoint of the (included) neck area, following skin tension lines. | Not available * |
| Neck superior | Nsup | Most superior point of the neck area, following skin tension lines. | Not available * |
| Otobasion inferior | OBI | The most inferior point on the earlobe, located at the attachment of the ear to the face. | Good [18] to very good [19] |
| Otobasion superior | OBS | The most superior point of the ear, located at the attachment of the ear to the face. | Not available |
| Soft tissue pogonion | Pg’ | The most anterior midpoint of soft tissue over the mandibular symphysis. | Good [19,20] |
| Subnasal | Sn | The midpoint on the nasolabial soft tissue contour between the columnella crest and the upper lip. | Good [17,19] |
| Tragus | T | Cartilage prominence of the external ear, in front of the concha. | Not available |
| Distance Measurement According to M.D. Anderson Cancer Center [16] | Landmarks on 3D Photograph | |
|---|---|---|
| 1 | Tragus to mental protuberance | T to Pg’ |
| 2 | Tragus to mouth angle | T to Ch |
| 3 | Mental protuberance to internal eye corner | Pg via A to En |
| 4 | Mandibular angle to external eye corner | Go’ to Ex |
| 5 | Mandibular angle to internal eye corner | Go’ to En |
| 6 | Mandibular angle to nasal wing | Go’ to A |
| 7 | Mandibular angle to metal protuberance | Go’ to Pg’ |
| Head diagonal | Diagonal circumference: chin to crown of the head | Left OBS via Pg’ to right OBS |
| Head vertical | Vertical circumference: in front of the ear | Left OBS via left Go’, H, and right Go’ to right OBS |
| Neck superior | Superior neck circumference | Left N Nsup via mid Nsup to right Nsup |
| Neck middle | Middle neck circumference | Left Nmid via mid Nmid to right Nmid |
| Neck inferior | Inferior neck circumference | Left Ninf via mid Ninf to right Ninf |
| Plane | Defined by | Explanation |
|---|---|---|
| Frankfurter | Landmarks: left and right Ex and one OBS of choice. | Part of the 3D photograph superior to this plane is excluded, defining the superior border of the facial regions. |
| Face–submental | Landmarks: left and right OBI and Pg’. | Splits the face region from the submental region. |
| Submental–neck | Landmarks: left and right OBI and H’. | Splits the submental region from the neck region. |
| Neck inferior | Landmarks: left, middle, and right Ninf. | Part of the 3D photograph inferior to this plane is excluded, defining the inferior border of the neck region. |
| Mid | Landmarks: Pg’, Sn, and midpoint between left and right Ex. | Splits the face in left and right regions. |
| Head posterior | Landmarks: left and right OBI and one OBS of choice. | Part of the 3D photograph posterior to this plane is excluded, defining the posterior border of the facial regions. |
| Neck posterior | Landmarks: left and right OBI; Plane defined by the landmarks: left and right A, and one OBS of choice. | Part of the 3D photograph posterior to this plane is excluded, defining the posterior border of the neck region. |
| Parameter | ICC (95% CI) | SEM (mm) | SDC | ||
|---|---|---|---|---|---|
| Distances on 3D photograph (mm) | Right face | 1 | 0.915 (0.739–0.975) | 0.89 (0.6%) | 2.46 (1.6%) |
| 2 | 0.922 (0.763–0.977) | 0.74 (0.6%) | 2.04 (1.7%) | ||
| 3 | 0.929 (0.782–0.979) | 0.84 (0.7%) | 2.32 (2.0%) | ||
| 4 | 0.949 (0.835–0.985) | 0.51 (0.5%) | 1.41 (1.3%) | ||
| 5 | 0.974 (0.916–0.992) | 0.27 (0.2%) | 0.74 (0.5%) | ||
| 6 | 0.925 (0.768–0.978) | 0.56 (0.5%) | 1.56 (1.3%) | ||
| 7 | 0.877 (0.638–0.963) | 1.30 (1.1%) | 3.59 (3.1%) | ||
| Overall | 0.985 (0.977–0.991) | 0.32 (0.3%) | 0.89 (0.7%) | ||
| Left face | 1 | 0.965 (0.887–0.990) | 0.40 (0.3%) | 1.12 (0.7%) | |
| 2 | 0.933 (0.791–0.980) | 0.69 (0.6%) | 1.91 (1.6%) | ||
| 3 | 0.987 (0.956–0.996) | 0.18 (0.2%) | 0.50 (0.4%) | ||
| 4 | 0.877 (0.639–0.962) | 1.15 (1.1%) | 3.18 (3.0%) | ||
| 5 | 0.950 (0.837–0.985) | 0.51 (0.4%) | 1.40 (1.1%) | ||
| 6 | 0.818 (0.501–0.943) | 1.44 (1.2%) | 3.99 (3.4%) | ||
| 7 | 0.886 (0.656–0.996) | 1.50 (1.3%) | 4.16 (3.6%) | ||
| Overall | 0.987 (0.957–0.996) | 0.33 (0.3%) | 0.93 (0.8%) | ||
| Neck circumference | Superior | 0.974 (0.912–0.992) | 0.77 (0.4%) | 2.12 (0.6%) | |
| Middle | 0.936 (0.794–0.981) | 2.72 (0.8%) | 7.53 (2.2%) | ||
| Inferior | 0.978 (0.926–0.994) | 0.61 (0.3%) | 1.68 (0.8%) | ||
| Overall | 0.994 (0.988–0.997) | 0.56 (0.2%) | 1.55 (0.5%) | ||
| Head circumference | Diagonal | 0.975 (0.915–0.993) | 0.79 (0.4%) | 2.20 (1.2%) | |
| Vertical | 0.952 (0.799–0.987) | 1.41 (0.7%) | 3.90 (2.1%) | ||
| Overall | 0.962 (0.888–0.985) | 0.26 (0.1%) | 0.71 (0.4%) | ||
| Overall | 0.998 (0.998–0.999) | 0.19 (0.1%) | 0.52 (0.3%) | ||
| Mean distance map (mm) | Right face | 0.980 (0.903–0.995) | 0.02 (2.6%) | 0.05 (7.4%) | |
| Left face | 0.987 (0.975–0.996) | 0.01 (1.5%) | 0.04 (4.3%) | ||
| Submental | 0.974 (0.915–0.992) | 0.04 (1.4%) | 0.10 (4.0%) | ||
| Neck | 0.920 (0.722–0.977) | 0.34 (9.2%) | 0.93 (25.6%) | ||
| Overall | 0.950 (0.909–0.972) | 0.15 (7.6%) | 0.40 (21.1%) | ||
| Root mean square distance map | Right face | 0.924 (0.761–0.977) | 0.07 (5.2%) | 0.20 (14.3%) | |
| Left face | 0.974 (0.917–0.922) | 0.03 (1.8%) | 0.08 (4.9%) | ||
| Submental | 0.950 (0.836–0.985) | 0.07 (2.4%) | 0.20 (6.6%) | ||
| Neck | 0.895 (0.679–0.969) | 0.53 (6.2%) | 1.46 (17.2%) | ||
| Overall | 0.971 (0.950–0.984) | 0.14 (3.8%) | 0.39 (10.7%) | ||
| Volume difference (mL) | Right face | 0.942 (0.814–0.983) | 0.62 (11.7%) | 1.72 (32.5%) | |
| Left face | 0.955 (0.851–0.987) | 0.53 (5.5%) | 1.48 (15.3%) | ||
| Submental | 0.979 (0.928–0.994) | 0.23 (1.4%) | 0.64 (3.8%) | ||
| Neck | 0.905 (0.692–0.972) | 5.09 (14.8%) | 14.1 (41.0%) | ||
| Overall | 0.914 (0.853–0.951) | 2.65 (16.0%) | 7.34 (44.5%) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buitenhuis, M.B.; Klijn, R.J.; Rosenberg, A.J.W.P.; Speksnijder, C.M. Reliability of 3D Stereophotogrammetry for Measuring Postoperative Facial Swelling. J. Clin. Med. 2022, 11, 7137. https://doi.org/10.3390/jcm11237137
Buitenhuis MB, Klijn RJ, Rosenberg AJWP, Speksnijder CM. Reliability of 3D Stereophotogrammetry for Measuring Postoperative Facial Swelling. Journal of Clinical Medicine. 2022; 11(23):7137. https://doi.org/10.3390/jcm11237137
Chicago/Turabian StyleBuitenhuis, Margje B., Reinoud J. Klijn, Antoine J. W. P. Rosenberg, and Caroline M. Speksnijder. 2022. "Reliability of 3D Stereophotogrammetry for Measuring Postoperative Facial Swelling" Journal of Clinical Medicine 11, no. 23: 7137. https://doi.org/10.3390/jcm11237137
APA StyleBuitenhuis, M. B., Klijn, R. J., Rosenberg, A. J. W. P., & Speksnijder, C. M. (2022). Reliability of 3D Stereophotogrammetry for Measuring Postoperative Facial Swelling. Journal of Clinical Medicine, 11(23), 7137. https://doi.org/10.3390/jcm11237137






