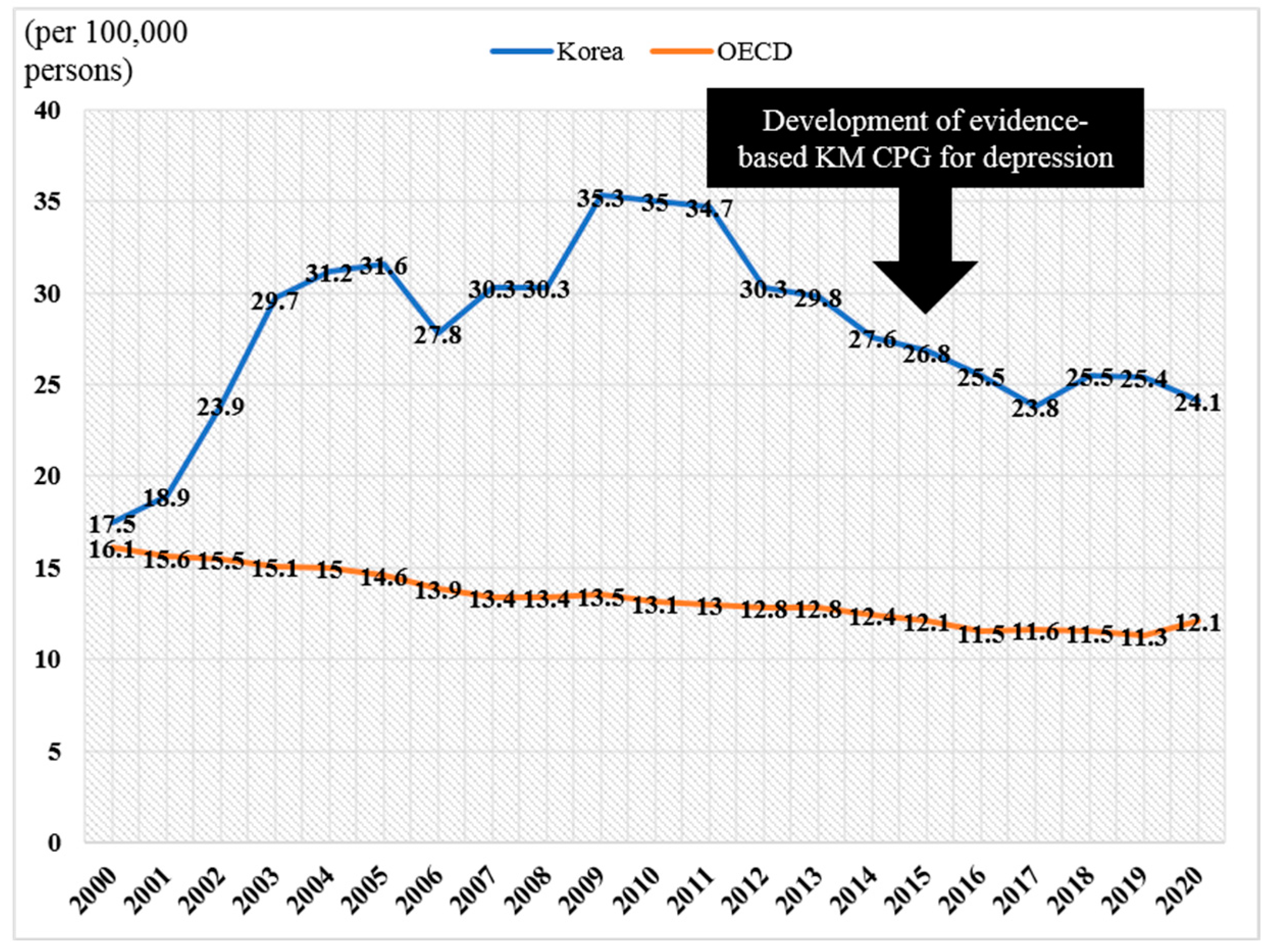
Gap between the Scientificization and Utilization of Korean Medicine for Depressive Disorder in South Korea with the Highest Suicide Rate among OECD Countries
Abstract
1. Introduction
2. Materials and Methods
2.1. Trend Analysis of KM and WM Use for Depressive Disorders
2.1.1. Database
2.1.2. Definition of Depressive Disorders
2.1.3. Statistical Analysis
2.2. Analysis of Efforts to Scientificize KM in the Context of Depressive Disorders
2.2.1. Clinical Practice Guidelines
2.2.2. Research and Development
3. Results
3.1. Trend of KM and WM Use for Depressive Disorders in South Korea
3.1.1. Number of Patients (Yearly)
3.1.2. Number of Visit Days (Yearly)
3.1.3. Number of Claims (Yearly)
3.1.4. Cost (Yearly)
3.2. Efforts to Scientificize KM in the Context of Depressive Disorders
3.2.1. Clinical Practice Guidelines
3.2.2. Research and Development
4. Discussion
4.1. Findings of This Study
4.2. Some Challenges to Fill the Gap
4.3. Limitations of This Study
5. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Collaborators, G.F. Global, regional, and national burden of bone fractures in 204 countries and territories, 1990-2019: A systematic analysis from the Global Burden of Disease Study 2019. Lancet Healthy Longev. 2021, 2, e580–e592. [Google Scholar] [CrossRef]
- Greenberg, P.E.; Fournier, A.A.; Sisitsky, T.; Simes, M.; Berman, R.; Koenigsberg, S.H.; Kessler, R.C. The Economic Burden of Adults with Major Depressive Disorder in the United States (2010 and 2018). Pharmacoeconomics 2021, 39, 653–665. [Google Scholar] [CrossRef] [PubMed]
- Collaborators, C.-M.D. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Bachmann, S. Epidemiology of Suicide and the Psychiatric Perspective. Int. J. Environ. Res. Public Health 2018, 15, 1425. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.U.; Park, J.I.; Lee, S.; Oh, I.H.; Choi, J.M.; Oh, C.M. Changing trends in suicide rates in South Korea from 1993 to 2016: A descriptive study. BMJ Open 2018, 8, e023144. [Google Scholar] [CrossRef]
- Kim, G.E.; Jo, M.W.; Shin, Y.W. Increased prevalence of depression in South Korea from 2002 to 2013. Sci. Rep. 2020, 10, 16979. [Google Scholar] [CrossRef]
- Gartlehner, G.; Wagner, G.; Matyas, N.; Titscher, V.; Greimel, J.; Lux, L.; Gaynes, B.N.; Viswanathan, M.; Patel, S.; Lohr, K.N. Pharmacological and non-pharmacological treatments for major depressive disorder: Review of systematic reviews. BMJ Open 2017, 7, e014912. [Google Scholar] [CrossRef]
- Cuijpers, P.; Noma, H.; Karyotaki, E.; Vinkers, C.H.; Cipriani, A.; Furukawa, T.A. A network meta-analysis of the effects of psychotherapies, pharmacotherapies and their combination in the treatment of adult depression. World Psychiatry Off. J. World Psychiatr. Assoc. (WPA) 2020, 19, 92–107. [Google Scholar] [CrossRef] [PubMed]
- Grant, C.L.; Lusk, J.L. A multidisciplinary approach to therapeutic risk management of the suicidal patient. J. Multidiscip. Healthc. 2015, 8, 291–298. [Google Scholar] [CrossRef]
- Hengartner, M.P.; Amendola, S.; Kaminski, J.A.; Kindler, S.; Bschor, T.; Plöderl, M. Suicide risk with selective serotonin reuptake inhibitors and other new-generation antidepressants in adults: A systematic review and meta-analysis of observational studies. J. Epidemiol. Community Health 2021, 75, 523–530. [Google Scholar] [CrossRef]
- Witt, K.; Potts, J.; Hubers, A.; Grunebaum, M.F.; Murrough, J.W.; Loo, C.; Cipriani, A.; Hawton, K. Ketamine for suicidal ideation in adults with psychiatric disorders: A systematic review and meta-analysis of treatment trials. Aust. N. Z. J. Psychiatry 2020, 54, 29–45. [Google Scholar] [CrossRef]
- Kucuker, M.U.; Almorsy, A.G.; Sonmez, A.I.; Ligezka, A.N.; Doruk Camsari, D.; Lewis, C.P.; Croarkin, P.E. A Systematic Review of Neuromodulation Treatment Effects on Suicidality. Front. Hum. Neurosci. 2021, 15, 660926. [Google Scholar] [CrossRef] [PubMed]
- Haller, H.; Anheyer, D.; Cramer, H.; Dobos, G. Complementary therapies for clinical depression: An overview of systematic reviews. BMJ Open 2019, 9, e028527. [Google Scholar] [CrossRef] [PubMed]
- Ng, J.Y.; Nazir, Z.; Nault, H. Complementary and alternative medicine recommendations for depression: A systematic review and assessment of clinical practice guidelines. BMC Complement. Med. Ther. 2020, 20, 299. [Google Scholar] [CrossRef]
- Rhee, T.G.; Evans, R.L.; McAlpine, D.D.; Johnson, P.J. Racial/Ethnic Differences in the Use of Complementary and Alternative Medicine in US Adults With Moderate Mental Distress. J. Prim. Care Community Health 2017, 8, 43–54. [Google Scholar] [CrossRef]
- Ashraf, H.; Salehi, A.; Sousani, M.; Sharifi, M.H. Use of Complementary Alternative Medicine and the Associated Factors among Patients with Depression. Evid.-Based Complement. Altern. Med. Ecam 2021, 2021, 6626394. [Google Scholar] [CrossRef]
- Hansen, A.H.; Kristoffersen, A.E. The use of CAM providers and psychiatric outpatient services in people with anxiety/depression: A cross-sectional survey. BMC Complement. Altern. Med. 2016, 16, 461. [Google Scholar] [CrossRef]
- Kim, D.; Shih, C.C.; Cheng, H.C.; Kwon, S.H.; Kim, H.; Lim, B. A comparative study of the traditional medicine systems of South Korea and Taiwan: Focus on administration, education and license. Integr. Med. Res. 2021, 10, 100685. [Google Scholar] [CrossRef]
- Kwon, C.Y.; Shin, S.; Lee, B.; Seo, J.C.; Nam, J.H.; Park, J.H.; Jung, S.E.; Ha, D.J.; Moon, W.; Kim, N.; et al. Disease-based evidence map for the second-wave development of evidence-based Korean medicine clinical practice guidelines in Korea. Integr. Med. Res. 2022, 11, 100868. [Google Scholar] [CrossRef]
- Kyoung, D.S.; Kim, H.S. Understanding and Utilizing Claim Data from the Korean National Health Insurance Service (NHIS) and Health Insurance Review & Assessment (HIRA) Database for Research. J. Lipid Atheroscler. 2022, 11, 103–110. [Google Scholar] [CrossRef]
- Ng, S.M.; Fong, T.C.; Wang, X.L.; Wang, Y.J. Confirmatory factor analysis of the stagnation scale—A traditional Chinese medicine construct operationalized for mental health practice. Int. J. Behav. Med. 2012, 19, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Kwon, C.Y.; Chung, S.Y.; Kim, J.W. Hwabyung: A Mental Disorder Related to Suppressed Emotions and Somatic Symptoms Reminiscent of Being on Fire. Psychosom. Med. 2020, 82, 529–531. [Google Scholar] [CrossRef]
- EBM-Based Depression Korean Medicine Clinical Practice Guideline Development Committee [Korea Institute of Oriental Medicine & The Korean Society of Oriental Neuropsychiatry]. Korean Medicine Clinical Practice Guideline of Depression; Elsevier LLC: Daejeon, Republic of Korea, 2015; pp. 1–278. [Google Scholar]
- Wexler, L.M.; Gone, J.P. Culturally responsive suicide prevention in indigenous communities: Unexamined assumptions and new possibilities. Am. J. Public Health 2012, 102, 800–806. [Google Scholar] [CrossRef]
- Chu, J.; Robinett, E.N.; Ma, J.K.L.; Shadish, K.Y.; Goldblum, P.; Bongar, B. Cultural versus classic risk and protective factors for suicide. Death Stud. 2019, 43, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.K.; Fancher, T.L.; Ratanasen, M.; Conner, K.R.; Duberstein, P.R.; Sue, S.; Takeuchi, D. Lifetime Suicidal Ideation and Suicide Attempts in Asian Americans. Asian Am. J. Psychol. 2010, 1, 18–30. [Google Scholar] [CrossRef] [PubMed]
- Saint Arnault, D.; Kim, O. Is there an Asian idiom of distress? Somatic symptoms in female Japanese and Korean students. Arch. Psychiatr. Nurs. 2008, 22, 27–38. [Google Scholar] [CrossRef]
- Ostermaier, A.; Barth, N.; Schneider, A.; Linde, K. On the edges of medicine—A qualitative study on the function of complementary, alternative, and non-specific therapies in handling therapeutically indeterminate situations. BMC Fam. Pract. 2019, 20, 55. [Google Scholar] [CrossRef]
- Rugg, S.; Paterson, C.; Britten, N.; Bridges, J.; Griffiths, P. Traditional acupuncture for people with medically unexplained symptoms: A longitudinal qualitative study of patients’ experiences. Br. J. Gen. Pract. J. R. Coll. Gen. Pract. 2011, 61, e306–e315. [Google Scholar] [CrossRef]
- Paterson, C.; Taylor, R.S.; Griffiths, P.; Britten, N.; Rugg, S.; Bridges, J.; McCallum, B.; Kite, G. Acupuncture for ’frequent attenders’ with medically unexplained symptoms: A randomised controlled trial (CACTUS study). Br. J. Gen. Pract. J. R. Coll. Gen. Pract. 2011, 61, e295–e305. [Google Scholar] [CrossRef]
- Lee, I.S.; Chae, Y. Cognitive components of acupuncture treatment. Integr. Med. Res. 2021, 10, 100754. [Google Scholar] [CrossRef]
- Kwon, C.-Y.; Lee, B. The efficacy of acupuncture on suicidal behavior: A protocol for systematic review and meta-analysis. AIMS Public Health 2022, 9, 651–660. [Google Scholar] [CrossRef]
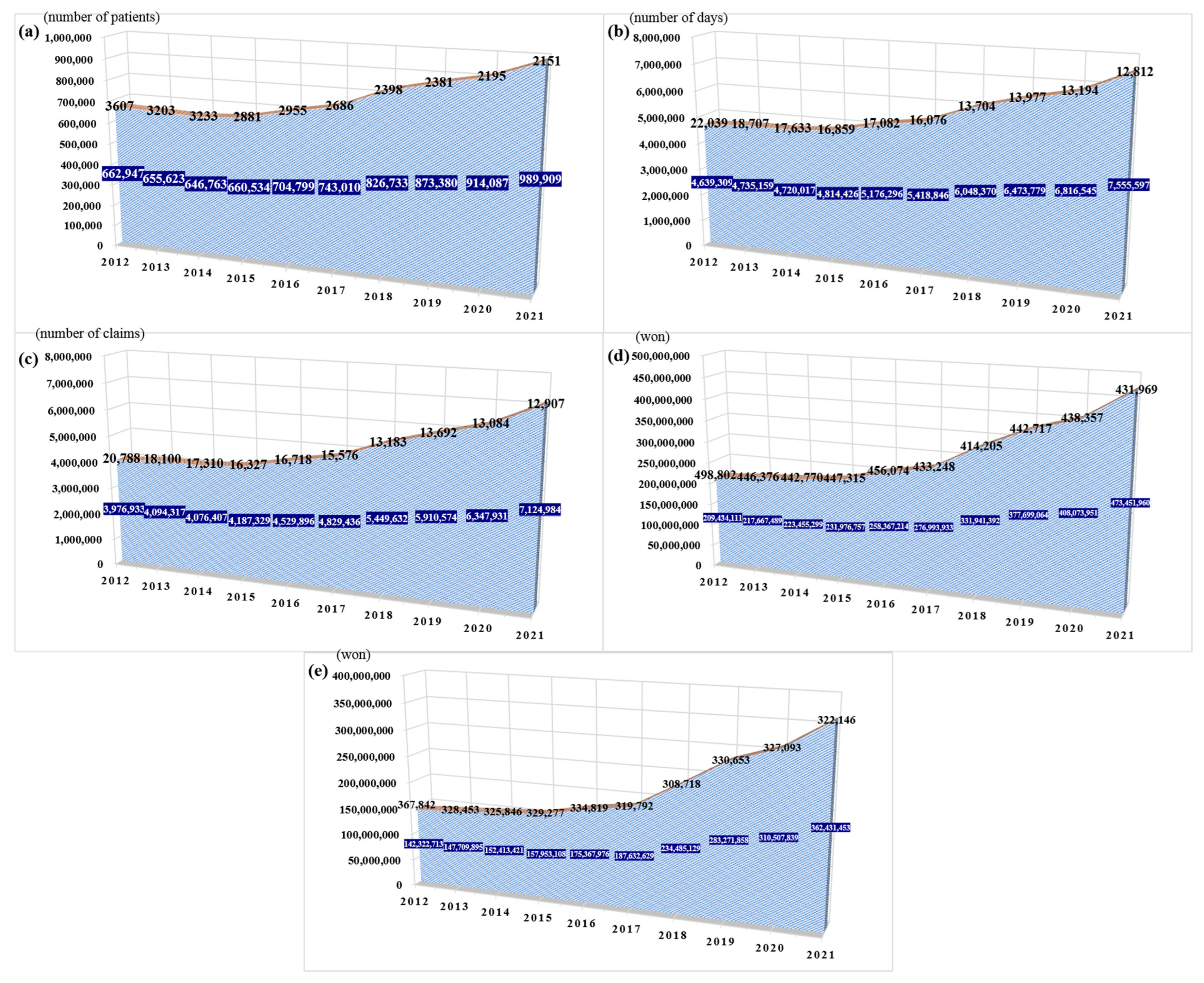
| Year | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 |
|---|---|---|---|---|---|---|---|---|---|---|
| Number of patients (yearly) | ||||||||||
| WM | 662,947 | 655,623 | 646,763 | 660,534 | 704,799 | 743,010 | 826,733 | 873,380 | 914,087 | 989,909 |
| KM model 1 | 3607 | 3203 | 3233 | 2881 | 2955 | 2686 | 2398 | 2381 | 2195 | 2151 |
| KM model 2 | 31,539 | 29,135 | 28,081 | 25,784 | 24,686 | 23,973 | 24,119 | 23,965 | 21,473 | 21,072 |
| Number of visit days (yearly) | ||||||||||
| WM | 4,639,309 | 4,735,159 | 4,720,017 | 4,814,426 | 5,176,296 | 5,418,846 | 6,048,370 | 6,473,779 | 6,816,545 | 7,555,597 |
| KM model 1 | 22,039 | 18,707 | 17,633 | 16,859 | 17,082 | 16,076 | 13,704 | 13,977 | 13,194 | 12,812 |
| KM model 2 | 144,549 | 132,134 | 129,542 | 120,657 | 115,444 | 113,517 | 119,264 | 118,280 | 112,400 | 112,914 |
| Number of claims (yearly) | ||||||||||
| WM | 3976,933 | 4,094,317 | 4,076,407 | 4,187,329 | 4,529,896 | 4,829,436 | 5,449,632 | 5,910,574 | 6,347,931 | 7,124,984 |
| KM model 1 | 20,788 | 18,100 | 17,310 | 16,327 | 16,718 | 15,576 | 13,183 | 13,692 | 13,084 | 12,907 |
| KM model 2 | 141,875 | 131,532 | 129,307 | 120,413 | 116,179 | 114,383 | 119,877 | 118,762 | 112,993 | 113,556 |
| Government insurance total cost (yearly, KRW) | ||||||||||
| WM | 209,434,111 | 217,667,489 | 223,455,299 | 231,976,757 | 258,367,214 | 276,993,933 | 331,941,392 | 377,699,064 | 408,073,951 | 473,451,960 |
| KM model 1 | 498,802 | 446,376 | 442,770 | 447,315 | 456,074 | 433,248 | 414,205 | 442,717 | 438,357 | 431,969 |
| KM model 2 | 2,954,019 | 2,707,927 | 2,842,348 | 2,759,091 | 2,994,491 | 3,353,658 | 3,974,904 | 4,252,291 | 4,482,472 | 4,587,991 |
| Out-of-pocket total cost (yearly, KRW) | ||||||||||
| WM | 142,322,713 | 147,709,895 | 152,413,421 | 157,953,108 | 175,367,976 | 187,632,629 | 234,485,129 | 283,271,858 | 310,507,839 | 362,431,453 |
| KM model 1 | 367,842 | 328,453 | 325,846 | 329,277 | 334,819 | 319,792 | 308,718 | 330,653 | 327,093 | 322,146 |
| KM model 2 | 2,188,161 | 2,010,743 | 2,117,269 | 2,049,623 | 2,208,916 | 2,466,432 | 2,936,312 | 3,111,706 | 3,248,129 | 3,312,030 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, C.-Y. Gap between the Scientificization and Utilization of Korean Medicine for Depressive Disorder in South Korea with the Highest Suicide Rate among OECD Countries. J. Clin. Med. 2022, 11, 7022. https://doi.org/10.3390/jcm11237022
Kwon C-Y. Gap between the Scientificization and Utilization of Korean Medicine for Depressive Disorder in South Korea with the Highest Suicide Rate among OECD Countries. Journal of Clinical Medicine. 2022; 11(23):7022. https://doi.org/10.3390/jcm11237022
Chicago/Turabian StyleKwon, Chan-Young. 2022. "Gap between the Scientificization and Utilization of Korean Medicine for Depressive Disorder in South Korea with the Highest Suicide Rate among OECD Countries" Journal of Clinical Medicine 11, no. 23: 7022. https://doi.org/10.3390/jcm11237022
APA StyleKwon, C.-Y. (2022). Gap between the Scientificization and Utilization of Korean Medicine for Depressive Disorder in South Korea with the Highest Suicide Rate among OECD Countries. Journal of Clinical Medicine, 11(23), 7022. https://doi.org/10.3390/jcm11237022








