Abstract
Background. Surface topography (ST) is one of the methods in scoliosis assessment. This study aimed to systematically review the reliability and validity of the ST measurements for assessing scoliosis. Methods. A literature search of four databases was performed and is reported following PRISMA guidelines. The methodological quality was evaluated using Brink and Louw appraisal tool and data extraction was performed. The results were analyzed and synthesized qualitatively using the level of evidence method. Results. Eighteen studies were included and analyzed. Four were evaluated for reliability, six for validity, and eight for reliability and validity. The methodological quality of fourteen studies was high. Good to excellent intra-investigator reliability was shown on asymmetry, sagittal, horizontal, and most frontal ST measurements (evidence level: strong). Asymmetry and most frontal, sagittal, horizontal ST measurements showed good to excellent inter-investigator reliability (evidence level: moderate). When comparing corresponding ST and radiological measurements, good to strong validity was shown on most frontal, sagittal, and asymmetry measurements (evidence level: strong). Formetric measurements had good intra-investigator reliability and validity (evidence level: strong). Conclusions. Most asymmetry, sagittal, and frontal ST measurements showed satisfactory reliability and validity. Horizontal ST measurements showed good reliability and poor validity. The ST technique may have great potential in assessing scoliosis, especially in reducing radiation exposure and performing cosmetic assessments.
Keywords:
scoliosis; assessment; surface topography; reliability; validity; reproducibility; posture 1. Introduction
Scoliosis is a three-dimensional structural deformity of the spine, including abnormal alignment of the vertebrae in the coronal, sagittal, and horizontal planes. According to the different causes, scoliosis can be categorized into several main types [1]: Idiopathic scoliosis (IS), congenital scoliosis (CS), neuromuscular scoliosis (NS), and scoliosis from miscellaneous causes. The most common type is idiopathic scoliosis (IS), and 80% or more [2] of idiopathic scoliosis occurs in adolescents, called adolescent idiopathic scoliosis (AIS). The US Preventive Services Task Force (USPSTF) states that [3] the prevalence of adolescent idiopathic scoliosis in children and adolescents aged 10–16 years is 1% to 3%. Symptoms associated with scoliosis can be influenced by the cause of the disease, the degree of scoliosis, and its progression. Specific symptoms include abnormal appearance, back pain, and psychological problems. In severe cases, it can also lead to respiratory distress, cardiopulmonary dysfunction, and even paralysis [4,5,6,7,8].
Therefore, early detection of scoliosis and timely intervention are essential. The gold standard in diagnosing and evaluating scoliosis is the radiological method, in which the Cobb angle is measured on a spine X-ray. A Cobb angle greater than 10° is the criterion for diagnosing scoliosis. This method is highly accurate and widely used, but some disadvantages cannot be ignored. The first is that radiation exposure may lead to health problems. One study showed that patients required twenty-two X-rays during the 3 years of treatment with the Milwaukee brace [9]. In addition, repeated X-ray exposure may increase cancer risk in patients [10]. A retrospective cohort study [11] of 5573 female patients with scoliosis in the United States showed that the incidence of breast cancer in the subjects was nearly two times higher than healthy individuals. Furthermore, although the morphology of the spine can be shown on radiographs, the Cobb angle is a two-dimensional indicator that does not fully quantify the degree of three-dimensional deformity of the spine.
The drawbacks mentioned above have triggered the development of several radiation-free, three-dimensional methods, such as CT [12,13,14], ultrasound [15,16,17,18], and surface topography technique [19,20,21]. Surface topography is more widely used among these methods since it is low-cost and user-friendly. Commonly used surface topography systems include InSpeck, Quantec, Milwaukee, and Formetric 4D [22]. As a clinical measurement tool, it is crucial to determine the validity and reliability of its measurement. Some of the previous relevant studies focused on reliability and validity, but a systematic review of this literature is lacking.
Therefore, this study aimed to systematically review the reliability and validity of the surface topography measurements for assessing scoliosis. Since various indices can be obtained through the ST technique, we classify the ST measurements into four categories: Frontal, sagittal, horizontal, and asymmetry measurements to achieve more focused results. Frontal, sagittal, and horizontal measurements are those where the anatomical landmarks used in the measurement are located in the corresponding planes. Asymmetry measurements reflect body asymmetry and usually involve more than one plane or more than one body region. Additional analyses were performed regarding the type of scanning (back-only or full-torso) and the automation level (manual or automatic identification of marker points). In terms of reliability, we analyzed intra-investigator and inter-investigator reliability to verify the reproducibility of ST measurements. Radiological measurements are considered the gold standard (especially the Cobb angle) and are well-established and widely used in all phases of scoliosis diagnosis, treatment, and management. It is of great interest to physicians and researchers how ST measurements relate to radiological measurements and in what ways and to what extent ST measurements can replace radiological measurements. Therefore, for validity evaluation, we chose radiological measurements as the reference standard and evaluated the validity by the correlation between ST measurements and radiological measurements.
2. Materials and Methods
2.1. Search Strategy
This study was based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [23]. A systematic search was conducted on four databases (Web of Science, Embase, PubMed, Cochrane Library). We combined search terms and MESH terms in a search strategy developed for PubMed, and adapted this strategy for the other databases. The search strategy of PubMed is shown in Table 1. The search language is English, and a manual search was performed on the references of the included studies.

Table 1.
Search strategy of PubMed.
2.2. Eligibility Criteria
The inclusion criteria are as follows:
- Subjects were patients with idiopathic scoliosis;
- The analysis of the patient’s scoliosis was performed using the surface topography technique;
- The reliability and/or validity of the surface topography measurements was evaluated;
- The surface topographic and radiological data were compared in the validity evaluation.
The exclusion criteria are as follows:
- Subjects had a history of previous spinal surgery or other spinal diseases;
- Subjects with scoliosis of neuromuscular, degenerative or other diagnosable cause;
- Subjects received spinal surgery or other treatment (including spinal orthoses and exercise therapy, etc.) during the experiment;
- Repeatedly published or unavailable full-text literature.
The literature search and screening were conducted by two reviewers independently following the search strategy and eligibility criteria described above. The titles and abstracts of the literature were first reviewed to exclude literature that clearly did not meet the requirements. The full text was read for literature that could not be identified for inclusion or exclusion. The study was included in the systematic review when both reviewers agreed that the study met the inclusion criteria. A third reviewer was consulted in case of any disagreement between the two reviewers during the literature search and screening process.
2.3. Data Extraction
The content of the data extraction included subject information, surface topography system, acquisition protocol, main evaluation indicators, and results of reliability and validity (including the measurements and methods used to obtain reference measurements used in validity analysis). Two reviewers performed data extraction independently, and the extracted contents were recorded in an abstraction form. A third reviewer was consulted in case of any disagreement.
2.4. Quality Assessment
Methodological quality assessment was performed using the reliability and validity critical appraisal tool proposed by Brink et al. [24]. The tool consists of thirteen items, of which five items relate to both validity and reliability studies, four items to validity studies only, and four items to reliability studies. To reduce the influence on reliability and validity results by the subject’s scoliosis progression, in our review, the appropriate interval between repeated reliability measurements and the index and standard tests was considered within 7 days. Each item could be scored as “yes”, “no” or “not applicable”. As stated in previous studies [25,26,27,28], if a study scored ≥60%, the methodological quality of the study could be considered as high; otherwise, it is considered low. Quality assessment was performed independently by two reviewers using the above-mentioned assessment tools, and any disagreements were resolved by discussion.
2.5. Data Analysis
The included studies showed significant heterogeneity in study design, ST measurements, and outcome measures. A meta-analysis was not performed since no three or more studies involving the same ST measurements were found. Therefore, descriptive analyses and synthesis were conducted, and heterogeneity was examined quantitatively and qualitatively using levels of evidence. The levels of evidence were divided into four categories: Strong, moderate, limited, and conflicting [29]. The specific criteria are shown in Table 2.

Table 2.
Level of evidence.
We classified the ST measurements into four types: Asymmetry, horizontal, sagittal, and frontal measurements (asymmetry measurements reflect body asymmetry and usually involve more than one plane or more than one body region). By categorizing similar measurements in different studies, the reliability and validity of ST measurements can be analyzed more specifically. In addition, analysis in terms of scan type (back-only or full-torso) and the automation level (manual or automatic identification of marker points) is considered.
For reliability results, we focused on intra- and inter-investigator reliability. When evaluating reliability, studies used intra-class correlation coefficient (ICC), Pearson or Spearman correlation coefficient (r), standard error of measurement (SEM), smallest detectable change (SDC), limits of agreement (LoA) or coefficient of variation (CV) to indicate that reliability results were considered adequate. It is important to note that studies using CV and correlation coefficients also need to state that there are no systematic differences (e.g., by t-test); otherwise, the study’s score in the quality assessment was reduced.
For validity results, the main focus is on criterion validity, which is the evaluation of validity by correlation with a reference standard (radiological parameter). Therefore, the use of Pearson or Spearman correlation coefficient (r) to express validity results is considered appropriate.

Table 3.
Criteria for interpreting ICC, r, and CV values.
3. Results
3.1. Articles Selection
According to the inclusion and exclusion criteria, eighteen articles [20,21,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47] were finally included in this systematic review. Four [20,33,41,44] were evaluated for reliability only, six [21,35,36,40,43,45] for validity only, and eight [32,34,37,38,39,42,46,47] for both reliability and validity. The flow chart of literature screening is shown in Figure 1.
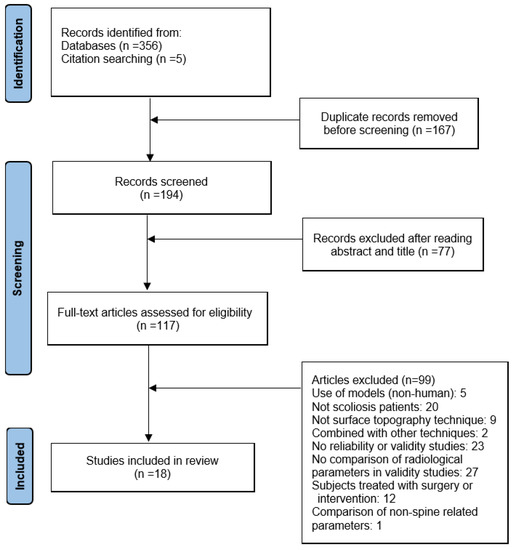
Figure 1.
The flow chart of literature screening.
3.2. Quality Assessment
Of the eighteen included studies, fourteen studies were rated as high-quality (score greater than 60%). Of the eight studies in which both reliability and validity evaluations were conducted, seven [32,34,37,38,42,46,47] were of high-quality. One [41] of the four studies evaluated for reliability only was of high-quality. Of the six studies that underwent validity evaluation only, all were of high-quality. The results of the quality assessment are listed in Table 4. The weak quality assessment is mainly due to the inappropriate or lack of description of the following items: Clarified the qualifications of testers, intra-raters blinded, varied examination order, appropriate period between the reference standard and index test.

Table 4.
Results of study quality assessment.
3.3. Study Characteristics
After data extraction, the study characteristics of eighteen studies are listed in Table 5.

Table 5.
Characteristics of the study.
3.3.1. The Surface Topography Systems
The eighteen studies used seven different surface topography systems (we considered self-designed systems in the same category). Of these, six studies [36,39,40,42,45,46] used in self-designed systems. The Formetric system was used in six studies [32,34,38,41,43,47,48], and the BIOMOD®L system was used in two studies [20,33]; other systems were reported in only one study each. In terms of the measurement area, three [36,37,44] studies were used in systems (the InSpeck system, Vitus Smart Scanner, and a self-designed system) that measured the full torso and the remaining systems (e.g., Formetric, BIOMOD®L) measured the back only.
3.3.2. Participants
Seventeen studies [20,21,32,34,35,36,37,38,39,40,41,42,43,44,45,46,47] stated the age of the subjects. All seventeen studies involved children or/and adolescents or/and young adults younger than 25 years of age. In most studies, subjects younger than 18 years were used. Regarding the sex of the subjects, two [36,39,49] of the eighteen included studies did not specify the sex of the subjects. The remaining sixteen studies included male and female subjects and more female than male subjects, which is consistent with gender differences in the onset of scoliosis.
In terms of scoliosis angle, three [21,32,44] studies did not specify the scoliosis angle of the subjects. Of the fifteen studies that specified the scoliosis angle of the subjects, most of them had subjects with mild, moderate, and severe scoliosis, and only the subjects used in the study by Gorton G. E. [37] et al. were patients with only severe scoliosis (Cobb angle 49–108°). The study by Knott P. et al. [38] also included a group of patients with kyphosis.
Regarding the type of scoliosis, only eight [20,21,33,38,40,45,46] studies specified the curve type of scoliosis in subjects. One [21] of these studies restricted subjects to the curve type of scoliosis that was double spinal curve (convexity to the right in the thoracic region and convexity to the left in the lumbar region), and the curve type of scoliosis in the other seven studies was diverse. The other ten studies did not specify the curve type of scoliosis of the subjects.
3.3.3. Data Acquisition
The data collected in the experiment included radiological data and surface topographic data. The acquisition methods were taking radiographs and scanning the surface topography, respectively. Of the eighteen studies included, X-rays were obtained during the experiments in nine studies [20,32,34,35,37,38,43,45,47]. In the remaining studies, some did not use X-rays, and others used X-rays obtained before the experiment. ST data acquisition for all studies was performed during the experiments.
3.4. Reliability Results
A total of eleven studies [20,32,33,37,38,39,41,42,44,46,47] underwent reliability assessment, and the results are presented in Table 6. The names (including abbreviations) and the definitions for all ST measurements are listed in Table 7. Among them, two studies [20,33] only evaluated the inter-investigator reliability, six studies [37,38,39,41,44,47] only evaluated the intra-investigator reliability, and three studies [32,42,46] evaluated both the inter- and intra-investigator reliability.

Table 6.
Reliability results.

Table 7.
Description of ST measurements.
Of the eleven studies for which reliability was assessed, nine [32,33,37,38,39,41,44,46,47] used the intra-class correlation coefficient (ICC) as the evaluation index, one study [20] used the Spearman correlation coefficient, and one study [42] used the variance coefficient (CV). Of the nine studies that used ICC, five [32,37,41,44,47] specified the ICC type or formula (listed in Table 4), one [45] did not specify the type but stated no systematic difference (p-value < 0.05), and four did not explicitly describe the details of ICC use. The study by Bolzinger M. et al. [20] and Mínguez M. F. et al. [42,43] did not report whether there were systematic differences. Some studies [33,44,47] also used the estimates of measurement errors, such as standard error of measurement (SEM) and smallest detectable change (SDC), and the specific values are extracted and listed in Table 6.
3.4.1. Intra-Investigator Reliability Assessment Results
Nine studies [32,37,38,39,41,42,44,46,47] conducted intra-investigator reliability evaluations. Among them, eight studies [32,37,38,39,41,44,46,47] used the intra-class correlation coefficient as the evaluation index, and one study [42] used the coefficient of variation.
In terms of automation level, six [32,38,42,44,46,47] studies manually identified or placed marker points, and three [37,39,41] studies used automatic identification. The intra-investigator reliability of measurements using both automatic and manual identification is good to excellent (evidence level: strong).
In most of these studies, the type of scan was back-only, with only two studies using a full-torso scan format. Four back-only studies used the Formetric system, and all measurements obtained good to excellent results (evidence level: strong). Moreover, the two studies that used full-torso scan achieved good to excellent results for their measurements (evidence level: moderate).
To further summarize the results regarding different body planes and regions, we divided the ST measurements into four categories: Sagittal, horizontal, frontal, and asymmetry measurements. Asymmetry measurements were used in six studies [37,39,41,42,44,46], sagittal measurements in six studies [32,37,38,41,44,47], frontal measurements in five studies [32,37,38,41,44], and horizontal measurements in four studies [32,37,41,44]. Good to excellent intra-investigator reliability was shown on all asymmetry, sagittal, and horizontal measurements and on most frontal measurements (evidence level: strong). Only the pelvis obliquity (PO) parameter in the study by Tabard-Fougere et al. [32] showed poor results (evidence level: limited). However, pelvis-related parameters were also present in two other studies [41,44], which showed good to excellent results (evidence level: moderate).
3.4.2. Inter-Investigator Reliability Assessment Results
Among the five studies [20,32,33,42,46] for which inter-investigator reliability was evaluated, three studies [32,33,46] used intra-class correlation coefficient (ICC), one study [20] used Spearman correlation coefficient (SCC), and one study [42] used coefficient of variation (CV) as the evaluation index.
All five studies used the back-only scan format, and the systems used included self-designed systems [42,46], Formetric 4D [32], and BIOMOD®L [20,33]. The self-designed systems were similar; both included projectors and their measurements had good inter-investigator reliability (evidence level: moderate). Regarding automation level, four studies [32,33,42,46] manually identified or placed marker points, and only one study [20] used automatic identification. The inter-investigator reliability was good for measurement derived from automatic identification (evidence level: limited) and varied more for manual identification of reference landmarks.
Regarding body parts and planes, three studies [20,42,46] used asymmetry measurements, and two studies [32,33] used sagittal, horizontal, and frontal measurements. The results showed that asymmetry ST measurements including axial plane deformity index (DAPI), horizontal plane deformity index (DHOPI), posterior trunk symmetry index (POTSI), and columnar profile (PC) had good to excellent inter-investigator reliability (evidence level: moderate). Most of the sagittal and frontal measurements had good to excellent reliability, with only some in the lumbar and pelvic regions showing decreased reliability. In particular, the pelvic region measurements showed poor results (evidence level: moderate). The inter-investigator reliability of horizontal measurements was good to excellent, with only one measurement (thoracic gibbosity) [33] showing poor reliability (evidence level: moderate).
3.5. Validity Results
A total of fourteen studies [21,32,34,35,36,37,38,39,40,42,43,45,46,47] were evaluated for validity, and the results are presented in Table 8. The names (including abbreviations) and the definitions for all ST measurements are listed in Table 7. Of these, thirteen studies used the Pearson correlation coefficient as an evaluation measure (only one [32] reported both r and p-values of t-tests), and one used the p-values of t-tests and linear regression.

Table 8.
Validity results.
Due to the variety of measurements, the results can be different when correlating a specific ST measurement with different radiological measurements. Therefore, we made the following classifications: (1) ST measurements and radiological measurements used for comparison are the same (for asymmetry measurements, the same radiological parameter is the Cobb angle); (2) ST measurements and radiological measurements used for comparison are different.
The validity results were satisfactory when using the same measurements for comparison. The results of four studies [32,34,35,38] showed that most frontal measurements (mainly scoliosis angles) have good to strong correlations (evidence level: strong). Similarly, in three studies [34,38,47], the sagittal measurements (mainly kyphosis angle and lordosis angle) showed good to strong correlations (evidence level: strong). There was one study exception [38] where two ST measurements (lumbar scoliosis curve and sagittal vertebral axis) showing moderate correlation occurred. Horizontal plane measurements (vertebral rotation) were addressed in only one study, indicating a moderate correlation (evidence level: limited). Regarding asymmetry measurements, six studies analyzed six measurements (PD [36], POTSI [42,45,46], DAPI [42], DHOPI [45,46], RMS [21], and asymmetry index [39,40]), mostly obtaining good to strong results (level of evidence: strong). However, moderate results appear in the calculation of POTSI with Cobb angle [46] and RMS with lumbar Cobb angle [21] (evidence level: limited). Five studies [32,34,38,43,47] in this category used the Formetric system (back-only type) and four of them showed good correlations between corresponding measurements (evidence level: strong). The validity of measurements derived from manual markers and automatic identification did not demonstrate a noticeable difference.
When different measurements were used for comparison, the validity results of the various measures appeared to differ. For example, two studies [45,46] comparing the relationship between PC and different radiological measurements obtained poor to good results (evidence level: moderate). Another study [37] correlated different ST measurements with radiological measurements and obtained moderate validity results (evidence level: limited).
4. Discussion
This systematic review revealed some results with strong evidence levels for both intra-investigator reliability and validity. Regarding intra-investigator reliability: (1) Both automatic and manual identification had good to excellent intra-investigator reliability. (2) The Formetric measurements obtained good to excellent results. (3) Good to excellent intra-investigator reliability was shown on all asymmetry, sagittal, and horizontal measurements and most frontal measurements. Regarding validity, when comparing the same ST and radiological measurements: (1) Most frontal, sagittal, and asymmetry measurements have good to strong results. (2) The Formetric measurements obtained good results. With regard to inter-investigator reliability, no results with a strong level of evidence were found due to the small number of studies (only five) and the differences in measurements used across studies. However, it was still found that the self-designed system (using projectors), asymmetry measurements, and most of the frontal and sagittal measurements (with the exception of lumbar and pelvic regions) had good to excellent inter-reliability at a moderate level of evidence.
The above results show that most ST measurements have satisfactory reliability and validity, especially for asymmetry, frontal, and sagittal measurements (with the exception of lumbar and pelvic regions). The Formetric measurements provide good intra-investigator reliability and validity. Nevertheless, the inter-investigator reliability results need to be further investigated (only one of the included studies addressed the inter-investigator reliability of the Formetric measurements).
Regarding why lumbar and pelvic measurements (pelvis obliquity, pelvic imbalance, lumbar sinuosity) show poor intra- and inter-investigator reliability, we speculated that the reason might be related to the structure of the pelvic area and the artificial placement or selection of the landmarks. On the contrary to radiological methods that can irradiate directly through the skin and soft tissues to the internal skeletal structures of the body, surface topography methods determine the location of anatomical landmarks based on the surface morphology of the human body. Holcombe [50] et al. studied the distribution of subcutaneous fat in humans for each vertebral plane from T6 to the sacrum. They found that the average thickness of subcutaneous fat was greater in the areas on both sides of the lumbar spine (mainly in the L3–L5 vertebral plane) than in other areas of the back. This distribution characteristic leads to a larger distance from the spine to the skin of the back [51] and sometimes more skin folds in the lumbar region.
Moreover, to protect the subject’s privacy, the sacrococcygeal region is often covered by clothing during the test and cannot be fully exposed. Therefore, skin folds, fat content, and clothing obscuration may affect the accuracy of surface topography data measurement and calculation. There are limitations in measurement accuracy in obese patients, patients with asymmetrical muscle surfaces, and patients who have undergone surgery, as mentioned in the study by Asamoah et al. [52]. Among the studies included in our review, three studies [21,34,38] included both thoracic and lumbar segment indices in their results. The comparison revealed that the validity of the thoracic segment indices was better than the lumbar segment indices, which corroborates the influence of the factors mentioned above on the reliability and validity results.
In addition, some ST systems require the operator to manually place the marker points at the specified anatomical locations to increase the accuracy of the measurement. In this case, it is not easy to accurately palpate or locate the marker when placing it due to the privacy of the sacrococcygeal region, and the position of the marker placed by different operators may vary, which may be another type of reason that affects the reliability. In the studies we reviewed, intra-investigator reliability results for manual marker identification were satisfactory, but inter-investigator reliability showed significant differences. Furthermore, this could ensure that operator differences in marker placement and selection affect reliability.
The methodological quality is essential when conducting reliability or validity evaluation. During our quality evaluation, some common methodological weaknesses were identified. First, many studies did not specify the qualifications of the testers, e.g., whether prior training had been conducted. In studies with automatic identification, the impact may not be significant, but for those cases where manual identification of anatomical markers is required, whether the researcher is sufficiently familiar with the location of the anatomical markers will undoubtedly impact the results. Some studies did not ensure that the testers were blinded to the subjects they have examined previously, which may exaggerate intra-investigator reliability. Some studies did not indicate whether the examination order varied, which may also affect the reliability. For example, testers may recall their previous measurements. In addition, possibly for radiation reduction, some studies used X-rays obtained before the experiment, which created a long time interval between ST and radiological measurements and may have affected the validity results. Therefore, the methodological quality can be improved by standardizing testers’ qualifications, using appropriate methods to ensure intra-investigator blinding, using a randomized test sequence, and shortening the time interval between ST and reference standard measurements.
By analyzing the studies [41,44] with better results in the lumbar-pelvic region, we found that automatic marker identification, prescribed subject standing position, and full-torso scan may be responsible for the improved outcomes. Compared with the manual identification of marker points, automatic identification can reduce the influence of operator competence factors on the results. The full-torso scan can provide three-dimensional information from multiple angles, somewhat compensating for the information obtained from the back-only scan. Specifying the subject’s standing position unifies the position and angle of all subjects relative to the device. It may allow the subject to be located at the optimal position and angle for device acquisition. In the analysis of the validity results, we found that in addition to the clarity of the bony markers of the lumbar region and the accuracy of the marker point placement, another possible reason for the poor validity was that the ST parameters and radiological parameters used to establish the correlation did not match. For example, the moderate correlation between rotation range and Cobb angle was shown in the study by Gorton [37] et al. The rotation range is a horizontal plane indicator, and the Cobb angle is a coronal plane indicator, both of which do not lie in the same plane. A similar situation exists in the study of Pino-Almero [45] et al. PC is a composite parameter consisting of three angles measuring the dorsal curvature in the sagittal plane (upper thoracic region, thoracolumbar region, and lumbosacral region, respectively). However, the radiological parameter with which the correlation was established was thoracic lordosis or lumbar lordosis, which is only one of PC’s components and therefore does not show a good correlation.
Of the four measurement types we analyzed, the asymmetry measurements are more promising than the other three categories, especially in the three-dimensional or comprehensive evaluation of scoliosis. The analysis showed that both intra- and inter-investigator reliability of asymmetric measurements was good, indicating their good reproducibility. Although asymmetry measurements do not yield the desired correlation when correlating with partial radiological measurements, as mentioned previously, this should not be a limitation for us. In practice, we should be more concerned with its reliability, which indicates whether the results are stable in repeated measurements and whether the results change when different testers perform the test process. Concerning validity, it is unnecessary to be overly concerned with the degree of match with existing radiological measurements. As Goldberg [35] mentioned, ST and radiological parameters measure different aspects of deformity. Rather than focusing significantly on the degree of matching ST measurements with radiological measurements, which limits the application of ST techniques, it is better to select better asymmetry measurements through research and establish corresponding evaluation criteria. In fact, this has been investigated by some researchers. For example, Mínguez [42] et al. used deformity in the axial plane index (DAPI) and posterior trunk symmetry index (POTSI) to establish a diagnostic criterion for scoliosis (DAPI ≤ 3.9% and POTSI ≤ 27.5%) and obtained good sensitivity and specificity. However, the ST technique has not established a gold standard for scoliosis diagnosis, such as the Cobb angle. Perhaps this is where future studies related to ST assessment of scoliosis can be focused. Since the Cobb angle is considered the gold standard in radiological measurements for the diagnosis of scoliosis and has an important place, there are many researchers and physicians who are interested in whether the ST parameter can replace the Cobb angle. Of the fourteen studies in which validity was evaluated, eleven compared the correlation between ST measurements and the Cobb angle. Good to strong correlations were obtained when comparing the ST scoliosis angle with the Cobb angle. Good correlations were also obtained for some asymmetry measurements and moderate or poor correlations for others when comparing the asymmetry measurements with the Cobb angle. The correlation is poor to moderate when comparing ST measurements that differed from the Cobb angle (e.g., rotation range). This indicates that the ST scoliosis angle and some asymmetry measurements can reflect the Cobb angle. However, ST measurements and Cobb angle do not match in other cases. Although the ST scoliosis angle and Cobb angle showed a high correlation in most cases in the relevant studies, the number of studies was limited (only four) and the spinal segments measured were not identical. Therefore, the evidence is not sufficiently strong to suggest that the ST scoliosis angle and Cobb angle can be used interchangeably in testing patients. More relevant studies, consistent results, and higher correlations are still needed to demonstrate that ST parameters and the Cobb angle can interchange.
In addition to being used to diagnose scoliosis, the Cobb angle is widely used by doctors to quantify the effectiveness of surgical or conservative treatments. However, on the contrary to doctors who focus on the internal Cobb angle, patients and their families are more concerned with improving the external shape or aesthetics. The expert consensus of the International Society on Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT) states that we should treat patients according to their future and current needs, where aesthetic issues should be the main reason for treating scoliosis [53]. However, the Cobb angle is not simply correlated with the external shape of the back. James [54] showed four girls with the same 70° Cobb angle in his study, with distinct individual differences in appearance. A study by Thulbourne et al. [55] also noted no clear linear relationship between rib deformity and the Cobb angle. For aesthetic issues, the value of the Cobb angle is not the only influencing factor; asymmetries in the shoulder, scapula, lumbar, and pelvic regions should also be taken into account [56]. Therefore, the surface topography technique may show advantages in evaluating the external shape. For example, asymmetry parameters can be combined with parameters from multiple planes or anatomical landmarks for a comprehensive analysis. The asymmetry parameter better reflects the shape of the back of the human body than traditional parameters (e.g., Cobb angle, thoracic kyphosis) that are analyzed based on a few anatomical landmarks. However, since radiological measurements mainly reflect the internal skeletal arrangement rather than the external shape, to evaluate the validity of ST measurements in reflecting external shape, more appropriate reference standards should be selected (such as the questionnaire on perceived appearance), which may provide more convincing evidence.
In addition to the emphasis on external shape improvement, progression identification is also essential during the follow-up of scoliosis. The need to monitor progress while avoiding the increased risk of cancer from repeated radiation exposures has led to the development of radiation-free methods, such as surface topography. Some studies have explored this issue. For example, Pino-Almero [43] et al. found a good correlation between the difference in DHOPI, POTSI, and Cobb angle in a 6-month interval. If these two parameters were used to follow the progression, a second radiography could be avoided in 70.96% (22 of 31 patients) cases. The result suggests that ST measurements also have the potential to identify the progression of scoliosis. However, there is still a need to demonstrate sensitivity to change and responsiveness to different parameters. Since this component was rarely addressed in the included studies, this point was not addressed in our evaluation and needed further investigation. Due to its non-radiation, non-invasive, and low-cost characteristics and its unique advantages in the three-dimensional evaluation and aesthetic assessment, the surface topography (ST) technique has great potential and promising applications in assessing scoliosis.
The results of this systematic review indicate that the ST technique has outstanding reliability (especially intra-observer reliability) when used for scoliosis assessment. Although some studies showed differences, the validity results were also satisfactory overall. Regarding reliability, accuracy can be improved by standardizing patient posture, calibrating anatomical landmarks, and using automated processing techniques [57]. Regarding validity, methods and standards within the ST technique should be established primarily rather than focusing only on improving its correlation with radiological parameters. The role of the ST technique should be a complement to the Cobb angle, not a substitute for it. Therefore, ST technology can be used in various areas, such as screening, outcome assessment, and follow-up of scoliosis and can provide a different perspective than radiology in assessing and treating scoliosis. Although the PRISMA guidelines were followed for the systematic evaluation, our review still has some limitations, which can be improved in further studies. Methodologically, when conducting literature screening and study quality assessment, we did not use the guidelines proposed by COSMIN, which may be more appropriate in evaluating measurement properties. In addition, some databases we did not use (such as CINAHL or SportDiscuss) may also be relevant to the topic. Moreover, we did not report on the agreement between reviewers during the inclusion or exclusion decision, data extraction, and methodological quality assessment phases. Furthermore, in the validity assessment, our criteria for interpreting correlation coefficients, although more commonly used, are relatively low (e.g., compared with those suggested by COSMIN) and may not be adequate to indicate that ST measurements could replace radiological measurements. At present, we are aware of COSMIN guidelines on conducting systematic reviews of measurements and that these documents could have guided the design of the search and the conducting of a more thorough quality appraisal. In the future, we will try to use the COSMIN guidelines to improve the quality of systematic reviews.
In addition, due to the limited number of included studies, some ST measurements were not adequately studied. Inter-investigator reliability for frontal, sagittal, and horizontal measurements did not obtain higher levels of evidence, especially for horizontal measurements, which showed inconsistent results. On the validity results of horizontal measurements, the evidence level was limited since only one study was involved. Studies on the reliability of horizontal measurements could be the focus in future studies. The inter-investigator reliability of automatic and manual identification methods also needs further investigation. For measurements from other common systems, such as InSpeck and Quantec, the evidence was not as conclusive.
Concerning the characteristics of the included studies, the subjects we included were all younger than 25 years of age. It is not possible to reflect whether different age groups may affect the reliability of ST measurements for evaluating scoliosis (e.g., older patients with degenerative scoliosis may have different results). With regard to the validity evaluation, we used a single reference standard. If other advantages of ST are considered, more diverse reference standards should be selected. Moreover, we did not review the sensitivity and responsiveness of ST measurements in identifying scoliosis progression. All of the above can be improved in future studies.
5. Conclusions
This study analyzed the reliability and validity of the surface topography technique for evaluating scoliosis through a systematic review of eighteen studies. The majority of the asymmetry, sagittal, and frontal ST measurements showed satisfactory reliability and validity. Horizontal ST measurements showed good reliability and poor validity. This review suggests that the ST technique may have great potential in assessing scoliosis, especially in reducing radiation exposure and performing cosmetic assessments.
Author Contributions
Conceptualization, X.S. and Y.L.; validation, R.D.; formal analysis, X.S., R.D. and Z.W.; investigation, X.S., R.D. and Z.W.; writing—original draft preparation, X.S.; writing—review and editing, X.S. and Y.L.; supervision, Y.L.; project administration, R.D. and Z.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- El-Hawary, R.; Chukwunyerenwa, C. Update on evaluation and treatment of scoliosis. Pediatr. Clin. 2014, 61, 1223–1241. [Google Scholar] [CrossRef]
- Asher, M.A.; Burton, D.C. Adolescent idiopathic scoliosis: Natural history and long term treatment effects. Scoliosis 2006, 1, 2. [Google Scholar] [CrossRef] [PubMed]
- Grossman, D.C.; Curry, S.J.; Owens, D.K.; Barry, M.J.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W.; Kemper, A.R.; Krist, A.H.; Kurth, A.E. Screening for adolescent idiopathic scoliosis: US preventive services task force recommendation statement. JAMA 2018, 319, 165–172. [Google Scholar]
- Baird, C.; Gardner, A. A report of the number of adolescents screened as warranting further investigation for depression and social anxiety in a pre-operative cohort with idiopathic scoliosis. Surg. J. R. Coll. Surg. Edinb. Irel. 2021, 19, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.P.; Lin, Y.L.; Huang, H.L.; Lu, H.F.; Wang, S.T.; Chi, Y.C.; Hung, K.S.; Chen, H.Y. Scoliosis and the Subsequent Risk of Depression A Nationwide Population-based Cohort Study in Taiwan. Spine 2016, 41, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Amaricai, E.; Suciu, O.; Onofrei, R.R.; Miclaus, R.S.; Iacob, R.E.; Catan, L.; Popoiu, C.M.; Cerbu, S.; Boia, E. Respiratory function, functional capacity, and physical activity behaviours in children and adolescents with scoliosis. J. Int. Med. Res. 2020, 48, 300060519895093. [Google Scholar] [CrossRef]
- Ramirez, N.; Johnston, C.E.; Browne, R.H. The prevalence of back pain in children who have idiopathic scoliosis. J. Bone Jt. Surg. Am. Vol. 1997, 79A, 364–368. [Google Scholar] [CrossRef]
- Mohammadi, P.; Akbari, M.; Sarrafzadeh, J.; Moradi, Z. Comparison of respiratory muscles activity and exercise capacity in patients with idiopathic scoliosis and healthy individuals. Physiother. Theory Pract. 2014, 30, 552–556. [Google Scholar] [CrossRef]
- Rao, P.S.; Gregg, E.C. A Revised Estimate of the Risk of Carcinogenesis from X-Rays To Scoliosis Patients. Investig. Radiol. 1984, 19, 58–60. [Google Scholar] [CrossRef]
- Don, S. Radiosensitivity of children: Potential for overexposure in CR and DR and magnitude of doses in ordinary radiographic examinations. Pediatr. Radiol. 2004, 34, S167–S172. [Google Scholar] [CrossRef]
- Doody, M.M.; Lonstein, J.E.; Stovall, M.; Hacker, D.G.; Luckyanov, N.; Land, C.E.; Collaborators, U.S.C.S. Breast cancer mortality after diagnostic radiography: Findings from the US Scoliosis Cohort Study. Spine 2000, 25, 2052–2063. [Google Scholar] [CrossRef] [PubMed]
- Adam, C.J.; Izatt, M.T.; Harvey, J.R.; Askin, G.N. Variability in Cobb angle measurements using reformatted computerized tomography scans. Spine 2005, 30, 1664–1669. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.S.; Hwang, C.J.; Jung, H.S.; Lee, D.H.; Park, J.W.; Cho, J.H.; Yang, J.J.; Park, S. Association Between Vertebral Rotation Pattern and Curve Morphology in Adolescent Idiopathic Scoliosis. World Neurosurg. 2020, 143, E243–E252. [Google Scholar] [CrossRef] [PubMed]
- Xiao, B.; Zhang, Y.B.; Yan, K.; Jiang, J.L.; Ma, C.Y.; Xing, Y.G.; Liu, B.; Tian, W. Where should Scoliometer and EOS Imaging be Applied when Evaluating Spinal Rotation in Adolescent Idiopathic Scoliosis-A Preliminary Study with Reference to CT Images. Glob. Spine J. 2022, in press. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.W.; Chen, X.T.; Yu, C.H. A real-time freehand 3D ultrasound imaging method for scoliosis assessment. J. Appl. Clin. Med. Phys. 2022, 23, e13709. [Google Scholar] [CrossRef] [PubMed]
- Lai, K.K.L.; Lee, T.T.Y.; Lee, M.K.S.; Hui, J.C.H.; Zheng, Y.P. Validation of Scolioscan Air-Portable Radiation-Free Three-Dimensional Ultrasound Imaging Assessment System for Scoliosis. Sensors 2021, 21, 2858. [Google Scholar] [CrossRef]
- Pang, H.; Wong, Y.S.; Yip, B.H.K.; Hung, A.L.H.; Chu, W.C.W.; Lai, K.K.L.; Zheng, Y.P.; Chung, T.W.H.; Sharma, G.; Cheng, J.C.Y.; et al. Using Ultrasound To Screen for Scoliosis To Reduce Unnecessary Radiographic Radiation: A Prospective Diagnostic Accuracy Study on 442 Schoolchildren. Ultrasound Med. Biol. 2021, 47, 2598–2607. [Google Scholar] [CrossRef]
- Zhang, J.H.; Li, H.J.; Yu, B. Three-Dimensional Assessment of Scoliosis Based on Ultrasound Data. In Proceedings of the Eighth International Conference on Machine Vision (Icmv 2015), Barcelona, Spain, 19–20 November 2015; Volume 9875. [Google Scholar] [CrossRef]
- Roy, S.; Grunwald, A.T.D.; Alves-Pinto, A.; Maier, R.; Cremers, D.; Pfeiffer, D.; Lampe, R. A Noninvasive 3D Body Scanner and Software Tool towards Analysis of Scoliosis. Biomed Res. Int. 2019, 2019, 4715720. [Google Scholar] [CrossRef]
- Bolzinger, M.; Bernardini, I.; Thevenin Lemoine, C.; Gallini, A.; Accadbled, F.; Sales de Gauzy, J. Monitoring adolescent idiopathic scoliosis by measuring ribs prominence using surface topography device. Spine Deform. 2021, 9, 1349–1354. [Google Scholar] [CrossRef]
- Yildirim, Y.; Tombak, K.; Karasin, S.; Yuksel, I.; Nur, A.H.; Ozsoy, U. Assessment of the reliability of hand-held surface scanner in the evaluation of adolescent idiopathic scoliosis. Eur. Spine J. 2021, 30, 1872–1880. [Google Scholar] [CrossRef]
- Liu, X.; Thometz, J.; Tassone, J.; Paulsen, L.; Lyon, R. Historical review and experience with the use of surface topographic systems in children with idiopathic scoliosis. ISIS 2013, 2, 9. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, n71. [Google Scholar] [CrossRef] [PubMed]
- Brink, Y.; Louw, Q.A. Clinical instruments: Reliability and validity critical appraisal. J. Eval. Clin. Pract. 2012, 18, 1126–1132. [Google Scholar] [CrossRef] [PubMed]
- Barrett, E.; McCreesh, K.; Lewis, J. Reliability and validity of non-radiographic methods of thoracic kyphosis measurement: A systematic review. Man. Ther. 2014, 19, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Keogh, J.W.; Cox, A.; Anderson, S.; Liew, B.; Olsen, A.; Schram, B.; Furness, J. Reliability and validity of clinically accessible smartphone applications to measure joint range of motion: A systematic review. PLoS ONE 2019, 14, e0215806. [Google Scholar] [CrossRef]
- Schrama, P.P.; Stenneberg, M.S.; Lucas, C.; Van Trijffel, E. Intraexaminer reliability of hand-held dynamometry in the upper extremity: A systematic review. Arch. Phys. Med. Rehabil. 2014, 95, 2444–2469. [Google Scholar] [CrossRef]
- Bellet, R.N.; Adams, L.; Morris, N.R. The 6-minute walk test in outpatient cardiac rehabilitation: Validity, reliability and responsiveness—a systematic review. Physiotherapy 2012, 98, 277–286. [Google Scholar] [CrossRef]
- Van Tulder, M.; Furlan, A.; Bombardier, C.; Bouter, L.; Editorial Board of the Cochrane Collaboration Back Review Group. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine 2003, 28, 1290–1299. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Madelin, G.; Babb, J.; Xia, D.; Regatte, R.R. Repeatability of quantitative sodium magnetic resonance imaging for estimating pseudo-intracellular sodium concentration and pseudo-extracellular volume fraction in brain at 3 T. PLoS ONE 2015, 10, e0118692. [Google Scholar] [CrossRef]
- Tabard-Fougere, A.; Bonnefoy-Mazure, A.; Hanquinet, S.; Lascombes, P.; Armand, S.; Dayer, R. Validity and Reliability of Spine Rasterstereography in Patients With Adolescent Idiopathic Scoliosis. Spine 2017, 42, 98–105. [Google Scholar] [CrossRef] [PubMed]
- de Sèze, M.; Randriaminahisoa, T.; Gaunelle, A.; de Korvin, G.; Mazaux, J.M. Inter-observer reproducibility of back surface topography parameters allowing assessment of scoliotic thoracic gibbosity and comparison with two standard postures. Ann. Phys. Rehabil. Med. 2013, 56, 599–612. [Google Scholar] [CrossRef] [PubMed]
- Frerich, J.M.; Hertzler, K.; Knott, P.; Mardjetko, S. Comparison of radiographic and surface topography measurements in adolescents with idiopathic scoliosis. Open Orthop. J. 2012, 6, 261–265. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, C.J.; Kaliszer, M.; Moore, D.P.; Fogarty, E.E.; Dowling, F.E. Surface topography, Cobb angles, and cosmetic change in scoliosis. Spine 2001, 26, E55–E63. [Google Scholar] [CrossRef]
- Gonzalez-Ruiz, J.M.; Perez-Nunez, M.I.; Garcia-Alfaro, M.D.; Bastir, M. Geometric morphometrics of adolescent idiopathic scoliosis: A prospective observational study. Eur. Spine J. 2021, 30, 612–619. [Google Scholar] [CrossRef]
- Gorton, G.E.; Young, M.L.; Masso, P.D. Accuracy, Reliability, and Validity of a 3-Dimensional Scanner for Assessing Torso Shape in Idiopathic Scoliosis. Spine 2012, 37, 957–965. [Google Scholar] [CrossRef]
- Knott, P.; Sturm, P.; Lonner, B.; Cahill, P.; Betsch, M.; McCarthy, R.; Kelly, M.; Lenke, L.; Betz, R. Multicenter Comparison of 3D Spinal Measurements Using Surface Topography With Those From Conventional Radiography. Spine Deform. 2016, 4, 98–103. [Google Scholar] [CrossRef]
- Sudo, H.; Kokabu, T.; Abe, Y.; Iwata, A.; Yamada, K.; Ito, Y.M.; Iwasaki, N.; Kanai, S. Automated noninvasive detection of idiopathic scoliosis in children and adolescents: A principle validation study. Sci. Rep. 2018, 8, 17714. [Google Scholar] [CrossRef]
- Kokabu, T.; Kawakami, N.; Uno, K.; Kotani, T.; Suzuki, T.; Abe, Y.; Maeda, K.; Inage, F.; Ito, Y.M.; Iwasaki, N.; et al. Three-dimensional depth sensor imaging to identify adolescent idiopathic scoliosis: A prospective multicenter cohort study. Sci. Rep. 2019, 9, 9678. [Google Scholar] [CrossRef]
- Manca, A.; Monticone, M.; Cugusi, L.; Doria, C.; Tranquilli-Leali, P.; Deriu, F. Back surface measurements by rasterstereography for adolescent idiopathic scoliosis: From reproducibility to data reduction analyses. Eur. Spine J. 2018, 27, 2130–2138. [Google Scholar] [CrossRef]
- Mínguez, M.F.; Buendía, M.; Cibrián, R.M.; Salvador, R.; Laguía, M.; Martín, A.; Gomar, F. Quantifier variables of the back surface deformity obtained with a noninvasive structured light method: Evaluation of their usefulness in idiopathic scoliosis diagnosis. Eur. Spine J. 2007, 16, 73–82. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mangone, M.; Raimondi, P.; Paoloni, M.; Pellanera, S.; Di Michele, A.; Di Renzo, S.; Vanadia, M.; Dimaggio, M.; Murgia, M.; Santilli, V. Vertebral rotation in adolescent idiopathic scoliosis calculated by radiograph and back surface analysis-based methods: Correlation between the Raimondi method and rasterstereography. Eur. Spine J. 2013, 22, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Pazos, V.; Cheriet, F.; Danserau, J.; Ronsky, J.; Zernicke, R.F.; Labelle, H. Reliability of trunk shape measurements based on 3-D surface reconstructions. Eur. Spine J. 2007, 16, 1882–1891. [Google Scholar] [CrossRef] [PubMed]
- Pino-Almero, L.; Minguez-Rey, M.F.; de Anda, R.; Salvador-Palmer, M.R.; Sentamans-Segarra, S. Correlation between Topographic Parameters Obtained by Back Surface Topography Based on Structured Light and Radiographic Variables in the Assessment of Back Morphology in Young Patients with Idiopathic Scoliosis. Asian Spine J. 2017, 11, 219–229. [Google Scholar] [CrossRef]
- Pino-Almero, L.; Mínguez-Rey, M.F.; Sentamans-Segarra, S.; Salvador-Palmer, M.R.; Anda, R.M.C.-O.d.; La O., J.L.-d. Quantification of topographic changes in the surface of back of young patients monitored for idiopathic scoliosis: Correlation with radiographic variables. J. Biomed. Opt. 2016, 21, 116001. [Google Scholar] [CrossRef] [PubMed]
- Tabard-Fougère, A.; Bonnefoy-Mazure, A.; Dhouib, A.; Valaikaite, R.; Armand, S.; Dayer, R. Radiation-free measurement tools to evaluate sagittal parameters in AIS patients: A reliability and validity study. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2019, 28, 536–543. [Google Scholar] [CrossRef]
- Applebaum, A.; Cho, W.; Nessim, A.; Kim, K.; Tarpada, S.P.; Yoon, S.H.; Pujar, B.; Kim, D.; Kim, S.Y. Establishing the validity of surface topography for assessment of scoliosis: A prospective study. Spine Deform. 2021, 9, 685–689. [Google Scholar] [CrossRef]
- Liu, X.-C.; Tassone, J.C.; Thometz, J.G.; Paulsen, L.C.; Lyon, R.M.; Marquez-Barrientos, C.; Tarima, S.; Johnson, P.R. Development of a 3-Dimensional Back Contour Imaging System for Monitoring Scoliosis Progression in Children. Spine Deform. 2013, 1, 102–107. [Google Scholar] [CrossRef]
- Holcombe, S.A.; Wang, S.C. Subcutaneous fat distribution in the human torso. In Proceedings of the IRCOBI Conference, Berlin, Germany, 10–12 September 2014. [Google Scholar]
- Parenteau, C.S.; Zhang, P.; Holcombe, S.; Kohoyda-Inglis, C.; Wang, S.C. Analysis of morphomics parameters by gender and BMI groups: Thorax shape and H-point location. In Proceedings of the IRCOBI Conference, Gothenburg, Sweden, 11–13 September 2013; pp. 11–13. [Google Scholar]
- Asamoah, V.; Mellerowicz, H.; Venus, J.; Klockner, C. The effectiveness of diagnostic procedures of spinal diseases. Surface analysis of the back. Orthopade 2000, 29, 480–489. [Google Scholar] [CrossRef]
- Negrini, S.; Grivas, T.B.; Kotwicki, T.; Maruyama, T.; Rigo, M.; Weiss, H.R. Why do we treat adolescent idiopathic scoliosis? What we want to obtain and to avoid for our patients. SOSORT 2005 Consensus paper. Scoliosis Spinal Disord. 2006, 1, 4. [Google Scholar] [CrossRef]
- James, J.I.P. Idiopathic scoliosis: The prognosis, diagnosis, and operative indications related to curve patterns and the age at onset. J. Bone Jt. Surg. Br. Vol. 1954, 36, 36–49. [Google Scholar] [CrossRef] [PubMed]
- Thulbourne, T.; Gillespie, R. The rib hump in idiopathic scoliosis. Measurement, analysis and response to treatment. J. Bone Jt. Surg. Br. Vol. 1976, 58, 64–71. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zaina, F.; Negrini, S.; Atanasio, S. TRACE (Trunk Aesthetic Clinical Evaluation), a routine clinical tool to evaluate aesthetics in scoliosis patients: Development from the Aesthetic Index (AI) and repeatability. Scoliosis 2009, 4, 3. [Google Scholar] [CrossRef] [PubMed]
- Patias, P.; Grivas, T.B.; Kaspiris, A.; Aggouris, C.; Drakoutos, E. A review of the trunk surface metrics used as Scoliosis and other deformities evaluation indices. Scoliosis Spinal Disord. 2010, 5, 12. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).