Dental and Skeletal Effects of Herbst Appliance, Forsus Fatigue Resistance Device, and Class II Elastics—A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
- Population: At least 10 Class II malocclusion-growing patients with all their permanent teeth present, except the third molars.
- Interventions/Comparators: Herbst or Forsus (non-TAD supported)/Class II elastics.
- Outcomes: Dentoskeletal changes measured by Cephalometric or CBCT analysis
- Study design: Randomized clinical trials and non-randomized trials.
2.3. Information Sources
2.4. Selection Process
2.5. Data Collection
2.6. Data Items
2.7. Study Risk of Bias Assessment
- a.
- Low risk of bias: if all the domains of the study were at low risk of bias.
- b.
- Some concerns: if there were some concerns for at least one domain, but not a high risk of bias for any other domain.
- c.
- High risk of bias: if at least one domain was at high risk of bias or multiple domains raised some concerns.
- a.
- Low risk of bias: if all domains of the study were at low risk of bias.
- b.
- Moderate risk of bias: if all domains of the study were at low or moderate risk of bias.
- c.
- Serious risk of bias: if at least one domain of the study was at serious risk of bias, but not at critical risk of bias in any other domain.
- d.
- Critical risk of bias: if at least one domain of the study was at critical risk of bias.
2.8. Effect Measures
2.9. Synthesis Methods
- a.
- Overjet
- b.
- Overbite
- c.
- Upper incisor inclination
- d.
- Lower incisor inclination
- e.
- Maxillary changes
- SNA angle
- A point (AP change)
- ANS point (AP change)
- f.
- Mandibular changes
- SNB angle
- B point (AP change)
- Pg point (AP change)
- Right and left gonial angle (Co-Go-Me)
- Right and left mandibular length (Co-Gn)
- Right and left mandibular corpus (Go-Gn)
- Right and left mandibular ramus height (Co-Go’)
- g.
- Condylar and glenoid fossa changes
- Right and left Co points (AP change)
- Right and left anterior glenoid fossa (AP change)
- Right and left posterior glenoid fossa (AP change).
2.10. Certainty Assessment
3. Results
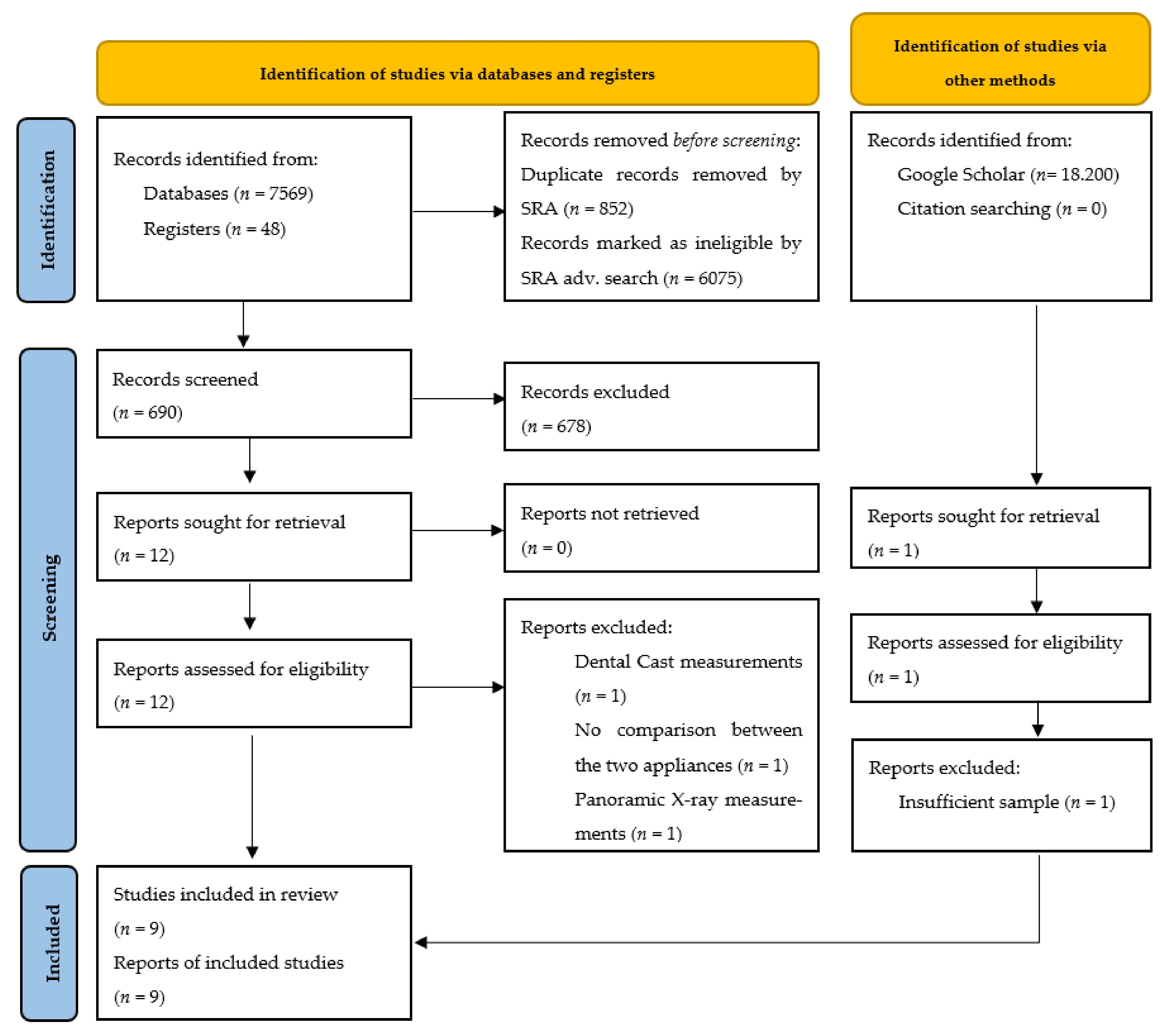
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias in Studies
| Trial Characteristics (Authors, Year of Publication, Study Design) | Patient Baseline Characteristics (Total Patient Number, Number of Females, Mean Baseline Age, Class II Malocclusion) | Intervention/Comparator Characteristics | Method of Outcome Assessment | Outcomes | Outcomes Results (Herbst/Forsus FRD vs. Cl. II El.: Mean ± SD) (Ns: Non-Significant Mean Difference) |
|---|---|---|---|---|---|
| |||||
| Neslon et al. [38] (2000, prospective) | n = 36 (F = 0) Herbst: 13.7y, Cl. II el: 13.5y Bilateral Class II malocclusion |
| Cephalometric radiographs | Short-term dental and skeletal changes |
|
| Neslon et al. [39] (2007, prospective) | n = 30 (F = 0) Herbst: 13.7y, Cl. II el: 13.5y Bilateral Class II malocclusion |
| Cephalometric radiographs | Long-term dental and skeletal changes |
|
| Serbesis-Tsarudis, Pancherz [40] (2008, retrospective) | n = 64 (F = 35) Herbst: 12.4y, Cl. II el.: 12.3y Bilateral Class II malocclusion |
| Cephalometric radiographs | TMJ and Chin position changes |
|
| Jones et al. [41] (2008, retrospective) | n = 68 (F = 28) Forsus FRD: 12.6y, Cl. II el.: 12.2y Bilateral Class II malocclusion |
| Cephalometric radiographs | Dental and skeletal changes |
|
| Aras, Pasaoglu [46] (2016, RCT) | n = 28 (F = 20) Forsus FRD: 14.2 ± 1y, Cl. II el: 13.8 ± 1.2y Class II subdivision |
| Cephalometric radiographs and dental casts measurements | Dental and skeletal changes |
|
| LeCornu et al. [43] (2013, prospective) | n = 14 Herbst: 13y, Cl. II el: 13.4y Bilateral Class II malocclusion |
| CBCT | Skeletal jaw changes and Condyle/Glenoid fossa changes |
|
| Atresh et al. [44] (2018, prospective) | n = 27 (F = 17) Herbst brachyfacial: 13.3y, Herbst mesofacial 12.7y, Cl. II el.: 13.7y Bilateral Class II malocclusion |
| CBCT | Skeletal jaw changes and Condyle/Glenoid fossa changes |
|
| Wei et al. [42] (2020, retrospective) | n = 31 (F = 21) Herbst: 13y, Cl. II el: 13.5y, Bilateral Class II malocclusion |
| CBCT | Condylar changes |
|
| Nindra et al. [45] (2021, retrospective) | n = 30 (F = 16) Herbst (splint): 13y 2 m, Cl. II el: 14y 5 m Bilateral Class II malocclusion |
| CBCT | Condyle and Glenoid fossa changes |
|
| Study | Bias Arising from the Randomization Process | Bias Due to Deviations from Intended Interventions | Bias Due to Missing Outcome Data | Bias in the Measurement of the Outcome | Bias in the Selection of the Reported Result | Overall Risk of Bias |
|---|---|---|---|---|---|---|
| Aras, Pasaoglu [46] (2016) | Low for all outcomes (matched randomization was used) | Low for all outcomes (no bias due to departure from the intended intervention is expected) | Low for all outcomes (data were reasonably complete) | Low for all outcomes (objective method of outcome assessment, outcome assessor was blinded) | Low for all outcomes (all reported results correspond to intended outcome) | Low for all outcomes |
| Study | Bias Due to Confounding | Bias in Selection of Participants into the Study | Bias in Classification of Interventions | Bias Due to Deviations from Intended Interventions | Bias Due to Missing Data | Bias in the Measurement of The Outcomes | Bias in the Selection of the Reported Result | Overall Risk of Bias |
|---|---|---|---|---|---|---|---|---|
| Neslon et al. [38] (2000) | Low for all outcomes (Patients were matched based on malocclusion, age, and somatic maturity) | Low for all outcomes (All eligible patients were selected and start of intervention and follow-up coincide) | Low for all outcomes (well defined intervention status) | Low for all outcomes (no bias due to departure from the intended intervention is expected) | Low for all outcomes (no missing outcome data) | Low for all outcomes (all pre-specified variables were measured) | Low for all outcomes (all reported results correspond to intended outcome) | Low for all outcomes |
| Neslon et al. [39] (2007) | Low for all outcomes (Patients were matched based on malocclusion, age, and somatic maturity) | Low for all outcomes (All eligible patients were selected and start of intervention and follow-up coincide) | Low for all outcomes (well defined intervention status) | Low for all outcomes (no bias due to departure from the intended intervention is expected) | Low for all outcomes (no missing outcome data) | Low for all outcomes (all pre-specified variables were measured) | Low for all outcomes (all reported results correspond to intended outcome) | Low for all outcomes |
| Serbesis-Tsarudis, Pancherz [40] (2008) | Low for all outcomes (patients had similar malloclusion, age, treatment time, and eligibility criteria) | Low for all outcomes (All eligible patients were selected and start of intervention and follow-up coincide) | Low for all outcomes (well defined intervention status) | Low for all outcomes (no bias due to departure from the intended intervention is expected) | Low for all outcomes (no missing outcome data) | Low for all outcomes (objective method of outcome assessment, any error is unrelated to intervention status) | Low for all outcomes (all reported results correspond to intended outcome) | Low for all outcomes |
| Jones et al. [41] (2008) | Low for all outcomes (Patients were matched based on malocclusion, gender, age, treatment duration, and angles: ANB, L1-GoMe, SN-GoMe) | Low for all outcomes (All eligible patients were selected and start of intervention and follow-up coincide) | Low for all outcomes (well defined intervention status) | Serious for all outcomes (Forsus FRD patients could have used Cl. II elastics prior to Forsus, or for retention after Forsus use) | Low for all outcomes (no missing outcome data) | Low for all outcomes (objective method of outcome assessment, any error is unrelated to intervention status) | Low for all outcomes (all reported results correspond to intended outcome) | Serious for all outcomes |
| LeCornu et al. [43] (2013) | Low for all outcomes (Patients were matched based on cervical vertebral maturity, jaw relationship and malloclusion) | Low for all outcomes (All eligible patients were selected and start of intervention and follow-up coincide) | Low for all outcomes (well defined intervention status) | Low for all outcomes (no bias due to departure from the intended intervention is expected) | Low for all outcomes (no missing outcome data) | Low for all outcomes (all pre-specified variables were measured) | Low for all outcomes (all reported results correspond to intended outcome) | Low for all outcomes |
| Atresh et al. [44] (2018) | Low for all outcomes (Patients were matched based on similar baseline characteristics) | Low for all outcomes (All eligible patients were selected and start of intervention and follow-up coincide) | Low for all outcomes (well defined intervention status) | Low for all outcomes (no bias due to departure from the intended intervention is expected) | Low for all outcomes (data were reasonably complete) | Low for all outcomes (objective method of outcome assessment, any error is unrelated to intervention status) | Low for all outcomes (all reported results correspond to intended outcome) | Low for all outcomes |
| Wei et al. [42] (2020) | Low for all outcomes (Patients were matched based on similar baseline characteristics) | Low for all outcomes (All eligible patients were selected and start of intervention and follow-up coincide) | Low for all outcomes (well defined intervention status) | Low for all outcomes (no bias due to departure from the intended intervention is expected) | Low for all outcomes (data were reasonably complete) | Low for all outcomes (objective method of outcome assessment, any error is unrelated to intervention status) | Low for all outcomes (all reported results correspond to intended outcome) | Low for all outcomes |
| Nindra et al. [45] (2021) | Low for all outcomes (Patients were matched based on similar baseline characteristics) | Low for all outcomes (All eligible patients were selected and start of intervention and follow-up coincide) | Low for all outcomes (well defined intervention status) | Low for all outcomes (no bias due to departure from the intended intervention is expected) | Low for all outcomes (data were reasonably complete) | Low for all outcomes (objective method of outcome assessment, any error is unrelated to intervention status) | Low for all outcomes (all reported results correspond to intended outcome) | Low for all outcomes |
3.4. Results of Individual Studies
3.5. Overjet
3.6. Overbite
3.7. Upper Incisor Inclination and Position
3.8. Lower Incisor Inclination
3.9. Molar Relationship
3.10. Maxillary Changes
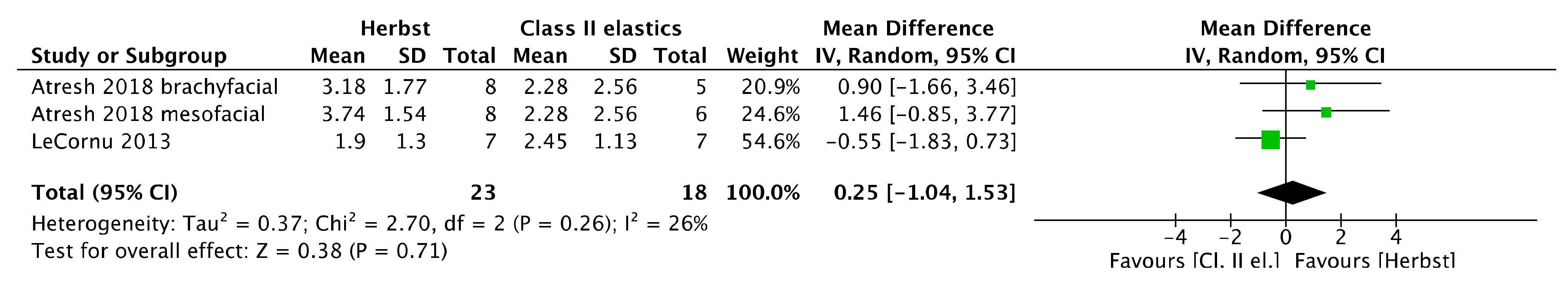
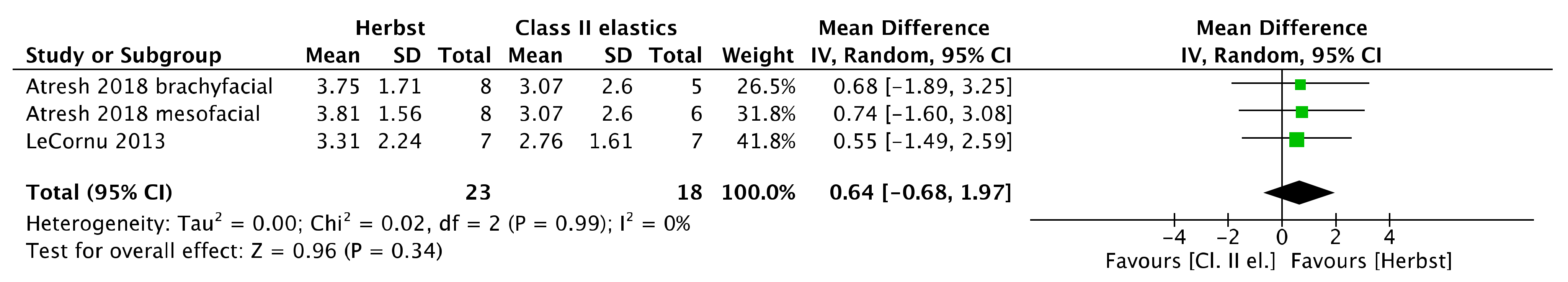
3.11. Mandibular Changes
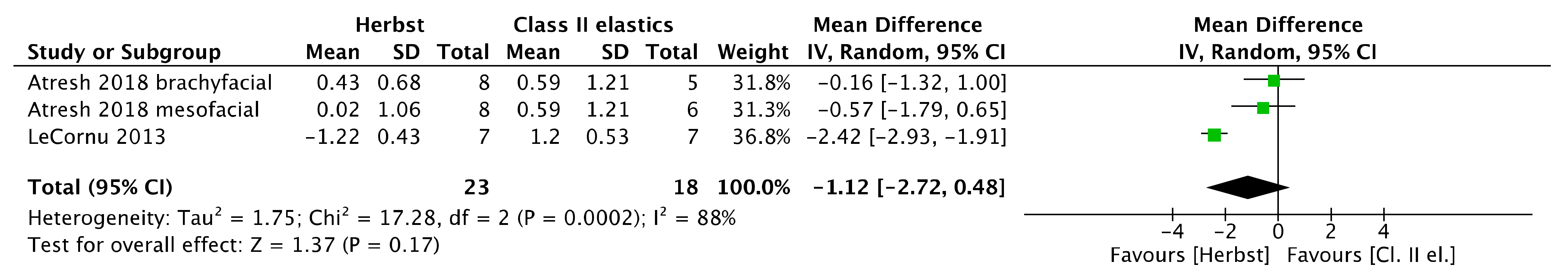
3.12. Condylar Changes
3.13. Glenoid Fossae Changes
3.14. Jaw Relationship
3.15. Results of Meta-Analysis
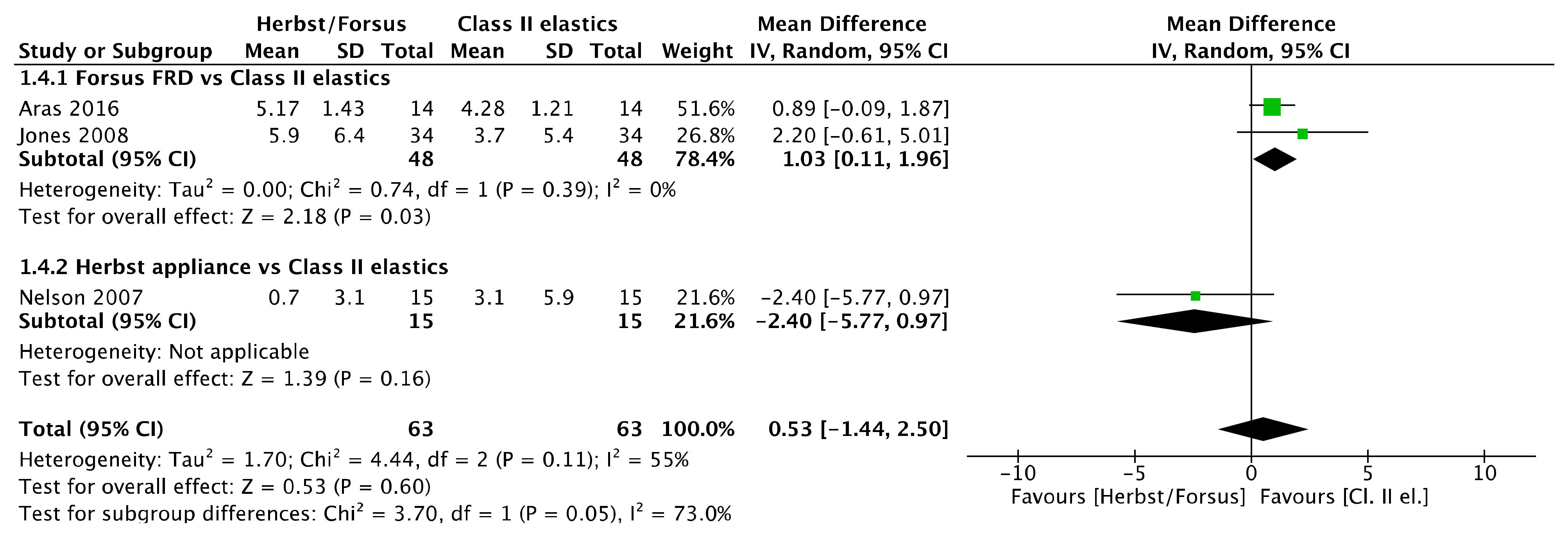
3.15.1. Overjet
3.15.2. Overbite
3.15.3. Upper Incisor Inclination
3.15.4. Lower Incisor Inclination
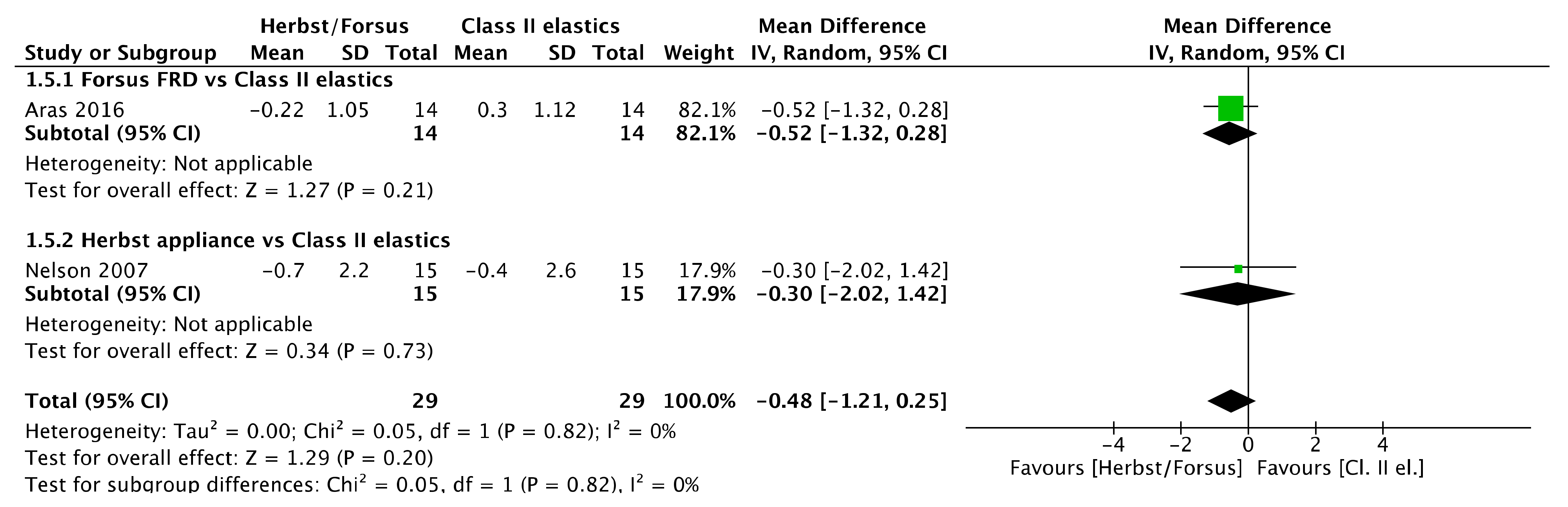
3.15.5. Maxillary Changes
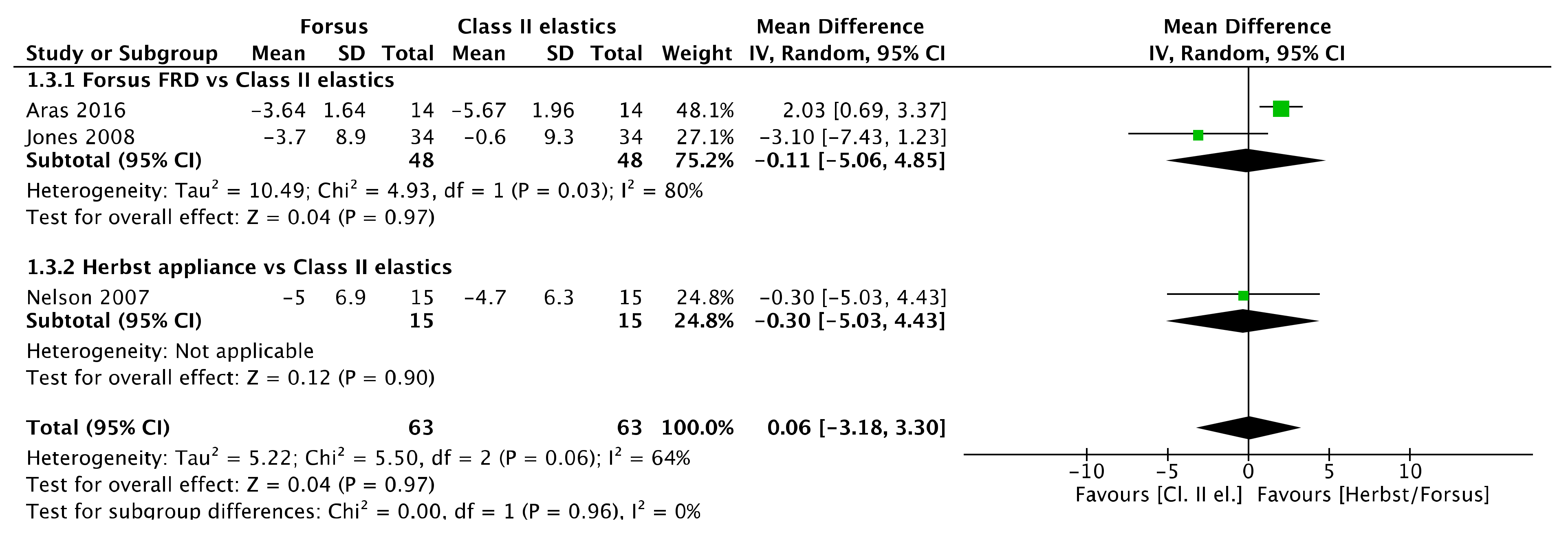
3.15.6. Mandibular Changes
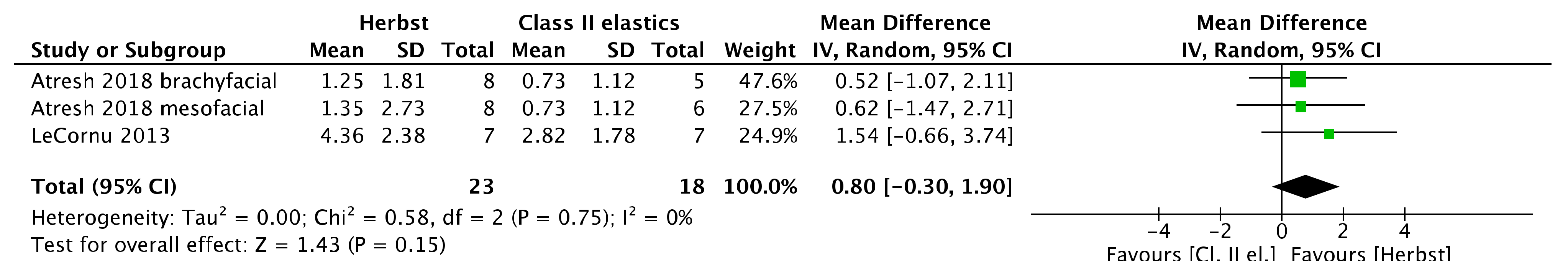
3.15.7. Condylar and Glenoid Fossa Changes
3.16. Sensitivity Analysis
3.17. Reporting Biases Assessment
3.18. Certainty Assessment
4. Discussion
4.1. Summary of Evidence
4.2. Strengths and Limitations
4.3. Critical Appraisal of the Results in the Context of other Evidence
4.4. Clinical Implications and Future Research
5. Conclusions
- Comparing Herbst appliance with Class II elastics, Herbst is equally effective as class II elastics in molar correction but causes a more mesial lower molar movement. Apart from an additional bilateral increase in mandibular length (1.5 mm), no other dental and anteroposterior skeletal differences exist.
- A clinical decision regarding the potential for growth acceleration using the Herbst appliance compared to Class II elastics should be made depending on the severity of the Class II malocclusion.
- Comparing Forsus appliance to Class II elastics, Forsus has equivalent dental effects to Class II elastics, but it is more effective in molar correction, overjet reduction, and controlling of the upper incisor inclination.
- High-quality randomized clinical trials with larger sample sizes should be performed to have definitive information about the effectiveness of these treatment methods.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| #1 Forsus | 127 |
| #2 Forsus Fatigue Resistant Device | 75 |
| #3 Herbst | 5224 |
| #4 Herbst Appliance | 3677 |
| #5 Functional appliance | 249,472 |
| #6 Class II appliance | 6537 |
| #7 #1 OR#2 OR#3 OR#4 OR#5 OR#6 | 257,867 |
| #8 Malocclusion, Angle Class II [Mesh] | 6618 |
| #9 Class II | 120,601 |
| #10 Class II malocclusion | 8384 |
| #11 Class II jaw relationship | 1019 |
| #12 skeletal Class II | 3595 |
| #13 dental Class II | 8264 |
| #14 Class II subdivision | 240 |
| #15 #8 OR#9 OR#10 OR#11 OR#12 OR#13 OR#14 | 121,068 |
| #16 #7 AND#15 | 5709 |
| PubMed search string: (Forsus OR “Forsus Fatigue Resistant Device” OR Herbst OR “Herbst Appliance” “Functional appliance” OR “Class II appliance”) AND ((“Malocclusion, Angle Class II” [Mesh]) OR “Class II” OR “Class II malocclusion” OR “Class II jaw relationship” OR “skeletal Class II” OR “dental Class II” OR “Class II subdivision”) | |
| #1 Forsus | 424 |
| #2 “Forsus Fatigue Resistant Device” | 30 |
| #3 Herbst | 263,257 |
| #4 “Herbst Appliance” | 1562 |
| #5 “Functional appliance” | 3101 |
| #6 “Class II appliance” | 16 |
| #7 (Forsus OR "Forsus Fatigue Resistant Device" OR Herbst OR "Herbst Appliance" "Functional appliance" OR "Class II appliance") | 1160 |
| #8 INDEXTERMS("Malocclusion, Angle Class II") | 5765 |
| #9 “Class II” | 292,108 |
| #10 “Class II malocclusion” | 5832 |
| #11 “Class II jaw relationship” | 15 |
| #12 “skeletal Class II” | 2570 |
| #13 “dental Class II” | 152 |
| #14 “Class II subdivision” | 391 |
| #15 ((INDEXTERMS ("Malocclusion, Angle Class II")) OR "Class II" OR "Class II malocclusion" OR "Class II jaw relationship" OR "skeletal Class II" OR "dental Class II" OR "Class II subdivision") | 292,108 |
| #16 (Forsus OR "Forsus Fatigue Resistant Device" OR Herbst OR "Herbst Appliance" "Functional appliance" OR "Class II appliance") AND ((INDEXTERMS ("Malocclusion, Angle Class II")) OR "Class II" OR "Class II malocclusion" OR "Class II jaw relationship" OR "skeletal Class II" OR "dental Class II" OR "Class II subdivision") | 1017 |
| Scopus search string: (Forsus OR "Forsus Fatigue Resistant Device" OR Herbst OR "Herbst Appliance" "Functional appliance" OR "Class II appliance") AND ((INDEXTERMS ("Malocclusion, Angle Class II")) OR "Class II" OR "Class II malocclusion" OR "Class II jaw relationship" OR "skeletal Class II" OR "dental Class II" OR "Class II subdivision") | |
| #1 Forsus | 154 |
| #2 Forsus Fatigue Resistant Device | 87 |
| #3 Herbst | 5014 |
| #4 Herbst Appliance | 430 |
| #5 Functional appliance | 802 |
| #6 Class II appliance | 4 |
| #7 (Forsus or “Forsus Fatigue Resistant Device” or Herbst or “Herbst Appliance” “Functional appliance” or “Class II appliance”) | 5123 |
| #8 exp “Malocclusion, Angle Class II”/ | 8927 |
| #9 Class II | 128,145 |
| #10 Class II malocclusion | 2313 |
| #11 Class II jaw relationship | 29 |
| #12 skeletal Class II | 1221 |
| #13 dental Class II | 152 |
| #14 Class II subdivision | 119 |
| #15 ((exp “Malocclusion, Angle Class II”/) or “Class II” or “Class II malocclusion” or “Class II jaw relationship” or “skeletal Class II” or “dental Class II” or “Class II subdivision”) | 16,777 |
| #16 #7 AND #15 | 261 |
| Embase search string: (Forsus or “Forsus Fatigue Resistant Device” or Herbst or “Herbst Appliance “Functional appliance” or “Class II appliance”) and ((exp “Malocclusion, Angle Class II”/) or “Class II” or “Class II malocclusion” or “Class II jaw relationship” or “skeletal Class II” or “dental Class II” or1 “Class II subdivision”) | |
| #1 Forsus | 36 |
| #2 Forsus Fatigue Resistant Device | 21 |
| #3 Herbst | 530 |
| #4 Herbst Appliance | 63 |
| #5 Functional appliance | 330 |
| #6 Class II appliance | 466 |
| #7 #1 OR#2 OR#3 OR#4 OR#5 OR#6 | 1084 |
| #8 MeSH descriptor: [Malocclusion, Angle Class II] explode all trees | 378 |
| #9 Class II | 153,189 |
| #10 Class II malocclusion | 710 |
| #11 Class II jaw relationship | 80 |
| #12 skeletal Class II | 1878 |
| #13 dental Class II | 3620 |
| #14 Class II subdivision | 35 |
| #15 #9 OR #10 OR #11 OR #12 OR #13 OR #14 | 153,189 |
| #16 #7 AND #15 | 583 |
| CENTRAL search string: (Forsus OR “Forsus Fatigue Resistant Device” OR Herbst OR “Herbst Appliance” “Functional appliance” OR “Class II appliance”) AND (([mh “Malocclusion, Angle Class II”]) OR “Class II” OR “Class II malocclusion” OR “Class II jaw relationship” OR “skeletal Class II” OR “dental Class II” OR “Class II subdivision”) | |
| #1 Forsus | 0 |
| #2 Forsus Fatigue Resistant Device | 0 |
| #3 Herbst | 1 |
| #4 Herbst Appliance | 1 |
| #5 Functional appliance | 8 |
| #6 Class II appliance | 7 |
| #7 Class II | 23 |
| #8 Class II malocclusion | 9 |
| #9 Class II jaw relationship | 1 |
| #10 skeletal Class II | 0 |
| #11 dental Class II | 16 |
| #12 Class II subdivision | 0 |
| #13 Herbst Appliance or Forsus AND Class II malocclusion | 0 |
| #1 Forsus | 5 |
| #2 Forsus Fatigue Resistant Device | 3 |
| #3 Herbst | 16 |
| #4 Herbst Appliance | 14 |
| #5 Functional appliance | 41 |
| #6 Class II appliance | 47 |
| #7 (Forsus) OR (Forsus Fatigue Resistant Device) OR (Herbst) OR (Herbst Appliance) OR (Functional appliance) OR (Class II appliance) | 70 |
| #8 Class II | 235 |
| #9 Class II Malocclusion | 90 |
| #10 Class II jaw relationship | 1 |
| #11 skeletal Class II | 27 |
| #12 dental Class II | 37 |
| #13 Class II subdivision | 0 |
| #14 (Class II) OR (Class II Malocclusion) OR (Class II jaw relationship) OR (skeletal Class II) OR (dental Class II) OR (Class II subdivision) | 235 |
| #15 Condition or Disease: (Class II) OR (Class II Malocclusion) OR (Class II jaw relationship) OR (skeletal Class II) OR (dental Class II) OR (Class II subdivision) Intervention/treatment: (Forsus) OR (Forsus Fatigue Resistant Device) OR (Herbst) OR (Herbst Appliance) OR (Functional appliance) OR (Class II appliance) | 48 |
| Herbst OR Forsus AND elastics | 18,200 |
| (((Forsus OR “Forsus Fatigue Resistant Device” OR Herbst OR “Herbst Appliance” “Functional appliance” OR “Class II appliance”) AND (“Class II” OR “Class II malocclusion” OR “Class II jaw relationship” OR “skeletal Class II” OR “dental Class II” OR “Class II subdivision”)) OR (elastics) | 690 |
References
- Ackerman, J.L.; Ackerman, M.B.; Kean, M.R. A Philadelphia Fable: How Ideal Occlusion Became the Philosopher’s Stone of Orthodontics. Int. J. Periodontics Restor. Dent. 2007, 27, 409–410. [Google Scholar] [CrossRef]
- Graber, L.; Vanarsdall, R.; Vig, K.; Huang, G. Orthodontics Current Principles and Techniques, 6th ed.; Elsevier: St. Louis, MO, USA, 2017; ISBN 9780323378321. [Google Scholar]
- Alhammadi, M.S.; Halboub, E.; Fayed, M.S.; Labib, A.; El-Saaidi, C. Global Distribution of Malocclusion Traits: A Systematic Review. Dent. Press J. Orthod. 2018, 23, e1–e40. [Google Scholar] [CrossRef] [PubMed]
- Ingervall, B. Prevalence of Dental and Occlusal Anomalies in Swedish Conscripts. Acta Odontol. Scand. 1974, 32, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Brunelle, J.A.; Bhat, M.; Lipton, J.A. Prevalence and Distribution of Selected Occlusal Characteristics in the US Population, 1988–1991. J. Dent. Res. 1996, 75, 706–713. [Google Scholar] [CrossRef]
- Bock, N.C.; von Bremen, J.; Ruf, S. Stability of Class II Fixed Functional Appliance Therapy--a Systematic Review and Meta-Analysis. Eur. J. Orthod. 2016, 38, 129–139. [Google Scholar] [CrossRef]
- Lippold, C.; van den Bos, L.; Hohoff, A.; Danesh, G.; Ehmer, U. Interdisciplinary Study of Orthopedic and Orthodontic Findings in Pre-School Infants. J. Orofac. Orthop. 2003, 64, 330–340. [Google Scholar] [CrossRef]
- Moss, M.L. The Functional Matrix Hypothesis Revisited. 1. The Role of Mechanotransduction. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 8–11. [Google Scholar] [CrossRef]
- Moss, M.L. The Functional Matrix Hypothesis Revisited. 2. The Role of an Osseous Connected Cellular Network. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 221–226. [Google Scholar] [CrossRef]
- Tsolakis, I.A.; Verikokos, C.; Perrea, D.; Alexiou, K.; Gizani, S.; Tsolakis, A.I. Effect of Diet Consistency on Rat Mandibular Growth: A Geometric Morphometric and Linear Cephalometric Study. Biology 2022, 11, 901. [Google Scholar] [CrossRef]
- Karamani, I.I.; Tsolakis, I.A.; Makrygiannakis, M.A.; Georgaki, M.; Tsolakis, A.I. Impact of Diet Consistency on the Mandibular Morphology: A Systematic Review of Studies on Rat Models. Int. J. Environ. Res. Public Health 2022, 19, 2706. [Google Scholar] [CrossRef]
- Tsolakis, I.A.; Perrea, D.; Bitsanis, E.; Verikokos, C.; Tsolakis, A.I. Effects of Diet Consistency on Mandibular Growth. A Review. J. Hell. Vet. Med. Soc. 2019, 70, 1603–1610. [Google Scholar] [CrossRef]
- Proffit, W.R.; Fields, H.W.; Sarver, D.M. Contemporary Orthodontics, 6th ed.; Elsevier: Philadephia, PA, USA, 2019; ISBN 9780323543873. [Google Scholar]
- Pancherz, H.; Fackel, U. The Skeletofacial Growth Pattern Pre-and Post-Dentofacial Orthopaedics. A Long-Term Study of Class II Malocclusions Treated with the Herbst Appliance. Eur. J. Orthod. 1990, 12, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, M.A. Orthodontic Treatment of the Class II Noncompliant Patient; Mosby Ltd.: Maryland Heights, MO, USA, 2006. [Google Scholar] [CrossRef]
- Pancherz, H. Treatment of Class II Malocclusions by Jumping the Bite with the Herbst Appliance. A Cephalometric Investigation. Am. J. Orthod. 1979, 76, 423–442. [Google Scholar] [CrossRef] [PubMed]
- Herbst, E. Atlas und Grundriss der Zahnärztliche Orthopädie; J. F. Lehmann: München, Germany, 1910. [Google Scholar]
- Pancherz, H. The Mechanism of Class II Correction in Herbst Appliance Treatment. A Cephalometric Investigation. Am. J. Orthod. 1982, 82, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Linjawi, A.I.; Abbassy, M.A. Dentoskeletal Effects of the ForsusTM Fatigue Resistance Device in the Treatment of Class II Malocclusion: A Systematic Review and Meta-Analysis. J. Orthod. Sci. 2018, 7, 31–43. [Google Scholar] [CrossRef]
- Janson, G.; Sathler, R.; Fernandes, T.M.F.; Branco, N.C.C.; de Freitas, M.R. Correction of Class II Malocclusion with Class II Elastics: A Systematic Review. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 383–392. [Google Scholar] [CrossRef]
- Combrink, F.J.; Harris, A.M.; Steyn, C.L.; Hudson, A.P. Dentoskeletal and Soft-Tissue Changes in Growing Class II Malocclusion Patients during Nonextraction Orthodontic Treatment. SADJ J. S. Afr. Dent. Assoc. 2006, 61, 344–350. [Google Scholar]
- Nelson, B.; Hansen, K.; Hägg, U. Overjet Reduction and Molar Correction in Fixed Appliance Treatment of Class II, Division 1, Malocclusions: Sagittal and Vertical Components. Am. J. Orthod. Dentofac. Orthop. 1999, 115, 13–23. [Google Scholar] [CrossRef]
- Adams, C.D.; Meikle, M.C.; Norwick, K.W.; Turpin, D.L. Dentofacial Remodelling Produced by Intermaxillary Forces in Macaca Mulatta. Arch. Oral Biol. 1972, 17, 1519–1535. [Google Scholar] [CrossRef] [PubMed]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Altman, D.G.; Booth, A.; et al. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015: Elaboration and Explanation. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef]
- Clark, J.M.; Sanders, S.; Carter, M.; Honeyman, D.; Cleo, G.; Auld, Y.; Booth, D.; Condron, P.; Dalais, C.; Bateup, S.; et al. Improving the Translation of Search Strategies Using the Polyglot Search Translator: A Randomized Controlled Trial. J. Med. Libr. Assoc. 2020, 108, 195–207. [Google Scholar] [CrossRef] [PubMed]
- Clark, J.; Glasziou, P.; del Mar, C.; Bannach-Brown, A.; Stehlik, P.; Scott, A.M. A Full Systematic Review Was Completed in 2 Weeks Using Automation Tools: A Case Study. J. Clin. Epidemiol. 2020, 121, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Mcgowan, J.; Sampson, M.; Salzwedel, D.M.; Cogo, E.; Foerster, V.; Lefebvre, C. CADTH Methods and Guidelines PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Explanation and Elaboration (PRESS E&E); CADTH: Ottawa, ON, Canada, 2016. [Google Scholar]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A Tool for Assessing Risk of Bias in Non-Randomised Studies of Interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Review Manager (RevMan) [Computer Program], Version 5.4; The Cochrane Collaboration: London, UK, 2020.
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; Version 6.3 (Updated February 2022); Cochrane: London, UK, 2022; Available online: https://training.cochrane.org/handbook#how-to-cite (accessed on 18 September 2022).
- Balshem, H.; Helfand, M.; Schünemann, H.J.; Oxman, A.D.; Kunz, R.; Brozek, J.; Vist, G.E.; Falck-Ytter, Y.; Meerpohl, J.; Norris, S.; et al. GRADE Guidelines: 3. Rating the Quality of Evidence. J. Clin. Epidemiol. 2011, 64, 401–406. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, 89. [Google Scholar] [CrossRef]
- Griblasky, I.; Latkauskiene, D.; Jakobsone, G. Evaluation of the Posterior Maxillary Teeth Movements during Class II Correction: 3-Dimensional Superimposition of Casts. Stomatol. Balt. Dent. Maxillofac. J. 2018, 20, 96–101. [Google Scholar]
- Yin, K.; Han, E.; Guo, J.; Yasumura, T.; Grauer, D.; Sameshima, G. Evaluating the Treatment Effectiveness and Efficiency of Carriere Distalizer: A Cephalometric and Study Model Comparison of Class II Appliances. Prog. Orthod. 2019, 20, 24. [Google Scholar] [CrossRef]
- Çoban, G.; Gül Amuk, N.; Yağcı, A.; Akgün, G.; Abbood Abbood, I.H. Evaluation of External Apical Root Resorption Caused by Fixed Functional Treatment of Class II Malocclusion: Cast Splint Herbst Appliance vs. Forsus Fatigue Resistant Device. J. Orofac. Orthop. 2021, 1–10. [Google Scholar] [CrossRef]
- Ambríz, G.M.; la Cruz Pérez, D.J. Changes of angulation of the lower incisor in class ii correction: Comparison forsus vs elastic vs herbst. a retrospective study. In Proceedings of the 49th International Congress 2018, Florence, Italy, 11–13 October 2018. [Google Scholar]
- Nelson, B.; Hansen, K.; Hägg, U. Class II Correction in Patients Treated with Class II Elastics and with Fixed Functional Appliances: A Comparative Study. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 142–149. [Google Scholar] [CrossRef]
- Nelson, B.; Hägg, U.; Hansen, K.; Bendeus, M. A Long-Term Follow-up Study of Class II Malocclusion Correction after Treatment with Class II Elastics or Fixed Functional Appliances. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 499–503. [Google Scholar] [CrossRef]
- Serbesis-Tsarudis, C.; Pancherz, H. “Effective” TMJ and Chin Position Changes in Class II Treatment: Orthodontics versus Orthopedics. Angle Orthod. 2008, 78, 813–818. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.; Buschang, P.H.; Kim, K.B.; Oliver, D.R. Class II Non-Extraction Patients Treated with the Forsus Fatigue Resistant Device versus Intermaxillary Elastics. Angle Orthod. 2008, 78, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Wei, R.Y.; Atresh, A.; Ruellas, A.; Cevidanes, L.H.S.; Nguyen, T.; Larson, B.E.; Mangum, J.E.; Manton, D.J.; Schneider, P.M. Three-Dimensional Condylar Changes from Herbst Appliance and Multibracket Treatment: A Comparison with Matched Class II Elastics. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 505–517.e6. [Google Scholar] [CrossRef]
- Lecornu, M.; Cevidanes, L.H.S.; Zhu, H.; Wu, C.D.; Larson, B.; Nguyen, T. Three-Dimensional Treatment Outcomes in Class II Patients Treated with the Herbst Appliance: A Pilot Study. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 818–830. [Google Scholar] [CrossRef]
- Atresh, A.; Cevidanes, L.H.S.; Yatabe, M.; Muniz, L.; Nguyen, T.; Larson, B.; Manton, D.J.; Schneider, P.M. Three-Dimensional Treatment Outcomes in Class II Patients with Different Vertical Facial Patterns Treated with the Herbst Appliance. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 238–248.e1. [Google Scholar] [CrossRef]
- Nindra, J.; Sidhu, M.S.; Kochhar, A.S.; Dabas, A.; Valletta, R.; Rongo, R.; Spagnuolo, G. Three-Dimensional Evaluation of Condyle-Glenoid Fossa Complex Following Treatment with Herbst Appliance. J. Clin. Med. 2021, 10, 4730. [Google Scholar] [CrossRef] [PubMed]
- Aras, I.; Pasaoglu, A. Class II Subdivision Treatment with the Forsus Fatigue Resistant Device vs Intermaxillary Elastics. Angle Orthod. 2017, 87, 371–376. [Google Scholar] [CrossRef]
- Voudouris, J.C.; Woodside, D.G.; Altuna, G.; Kuftinec, M.M.; Angelopoulos, G.; Bourque, P.J. Condyle-Fossa Modifications and Muscle Interactions during Herbst Treatment, Part 1. New Technological Methods. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 604–613. [Google Scholar] [CrossRef]
- Voudouris, J.C.; Woodside, D.G.; Altuna, G.; Angelopoulos, G.; Bourque, P.J.; Lacouture, C.Y. Condyle-Fossa Modifications and Muscle Interactions during Herbst Treatment, Part 2. Results and Conclusions. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 13–29. [Google Scholar] [CrossRef]
- Cevidanes, L.H.C.; Oliveira, A.E.F.; Grauer, D.; Styner, M.; Proffit, W.R. Clinical Application of 3D Imaging for Assessment of Treatment Outcomes. Semin. Orthod. 2011, 17, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Cevidanes, L.H.C.; Heymann, G.; Cornelis, M.A.; DeClerck, H.J.; Tulloch, J.F.C. Superimposition of 3-Dimensional Cone-Beam Computed Tomography Models of Growing Patients. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 94. [Google Scholar] [CrossRef] [PubMed]






| Outcomes | Anticipated Mean Post-Treatment Difference Herbst/Forsus FRD vs. Class II Elastics (95% CI) | No. of Participants (Studies) | Certainty of Evidence (GRADE) |
|---|---|---|---|
| Overjet | The mean difference in overjet was 0.41 mm less in the intervention group (1.18, 0.35) | 126 participants (1 RCT, 2 observational studies) | ⊕⊕OO Low [39,41,46] ** |
| Overbite | The mean difference in overbite was 0.43 mm less in the intervention group (−0.88, 0.01) | 58 participants (1 RCT, 1 observational study) | ⊕⊕⊕⊕ High [39,46], ** |
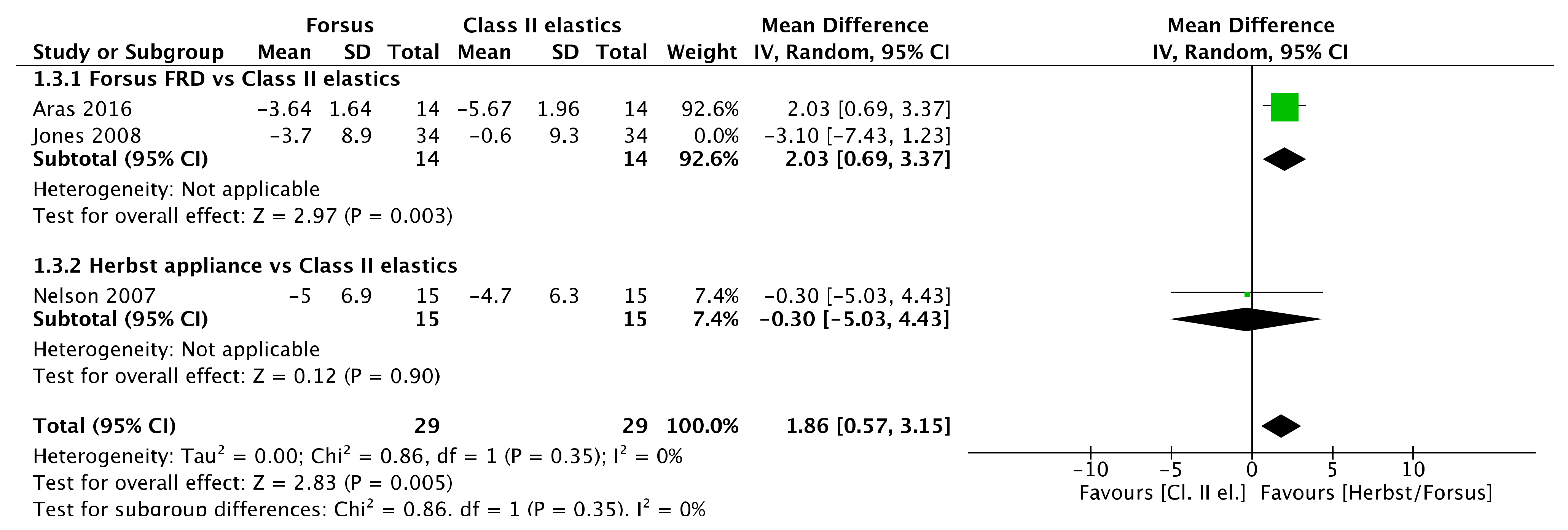
| Upper incisor inclination | The mean difference in upper incisor inclination was 1.86° less in the intervention group (0.57, 3.15) | 58 participants (1 RCT, 1 observational study) | ⊕⊕⊕⊕ High [39,46] ** |
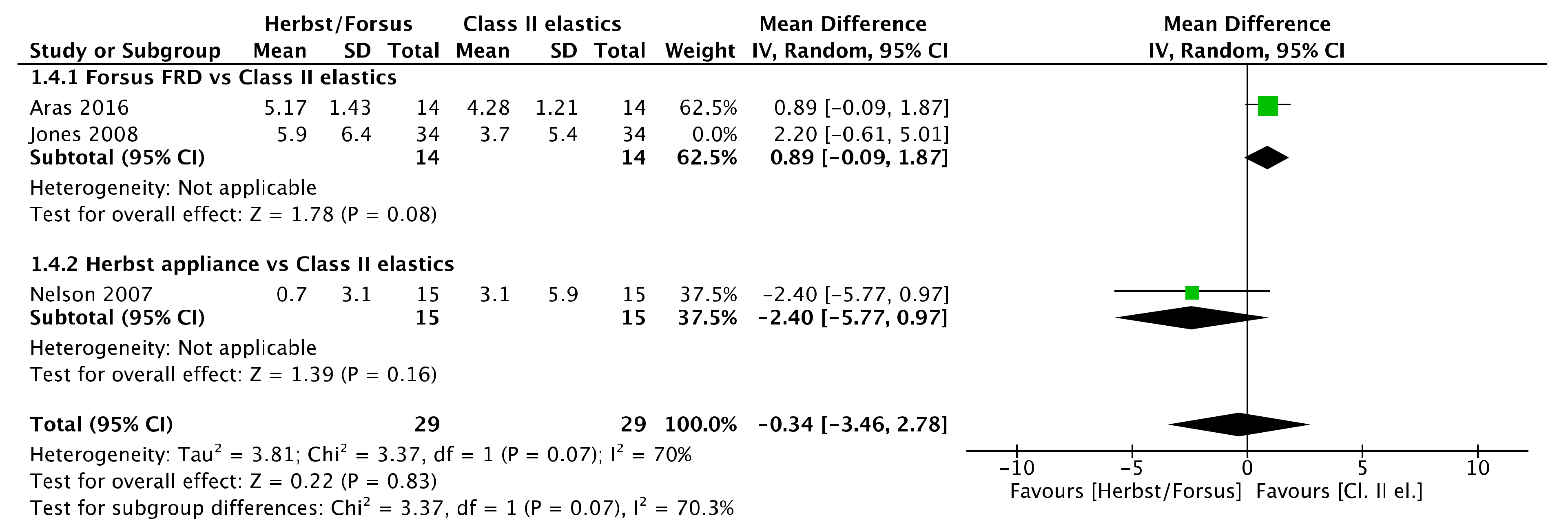
| Lower incisor inclination | The mean difference in upper incisor inclination was 0.53° more in the intervention group (−1.44, 2.50) | 126 participants (1 RCT, 2 observational studies) | ⊕⊕OO Low [43,44], ** |
| SNA angle | The mean difference in SNA angle was 0.48° less in the intervention group (1.21, 0.25) | 58 participants (1 RCT, 1 observational study) | ⊕⊕⊕⊕ High [39,46],** |
| A point (AP change) | The mean difference in A point was 1.12 mm less anteriorly in the intervention group (−2.72, 0.48) | 41 participants (2 observational studies) | ⊕OOO Very Low [43,44], * |
| ANS point (AP change) | The mean difference in ANS point was 0.3 mm less anteriorly in the intervention group (−1.91, 1.31) | 41 participants (2 observational studies) | ⊕OOO Very Low [43,44], * |
| SNB angle | The mean difference in SNB angle was 0.08° more in the intervention group (−0.50, 0.67) | 58 participants (1 RCT, 1 observational study) | ⊕⊕⊕⊕ High [39,46], ** |
| B point (AP change) | The mean difference in B point was 0.73 mm more anteriorly in the intervention group (−0.002, 1,46) | 41 participants (2 observational studies) | ⊕⊕OO Low [43,44], * |
| Pg point (AP change) | The mean difference in Pg point was 0.8 mm more anteriorly in the intervention group (−0.3, 1.9) | 41 participants (2 observational studies) | ⊕⊕OO Low [43,44], * |
| right gonial angle | The mean difference in right gonial angle was 1.01° greater in the intervention group (−0.03, 2.04) | 41 participants (2 observational studies) | ⊕⊕OO Low [43,44], * |
| left gonial angle | The mean difference in left gonial angle was 0.12° greater in the intervention group (−0.61, 0.85) | 41 participants (2 observational studies) | ⊕⊕OO Low [43,44], * |
| right mandibular length | The mean difference in right mandibular length was 1.41 mm greater in the intervention group (0.03, 2.79) | 41 participants (2 observational studies) | ⊕⊕OO Low [43,44], * |
| left mandibular length | The mean difference in left mandibular length was 1.47 mm greater in the intervention group (0.16, 2.79) | 41 participants (2 observational studies) | ⊕⊕OO Low [43,44], * |
| right mandibular corpus length | The mean difference in right mandibular corpus was 0.25 mm greater in the intervention group (−1.04, 1.53) | 41 participants (2 observational studies) | ⊕⊕OO Low [43,44], * |
| left mandibular corpus length | The mean difference in right mandibular corpus was 0.93 mm greater in the intervention group (−0.04, 1.90) | 41 participants (2 observational studies) | ⊕⊕OO Low [43,44], * |
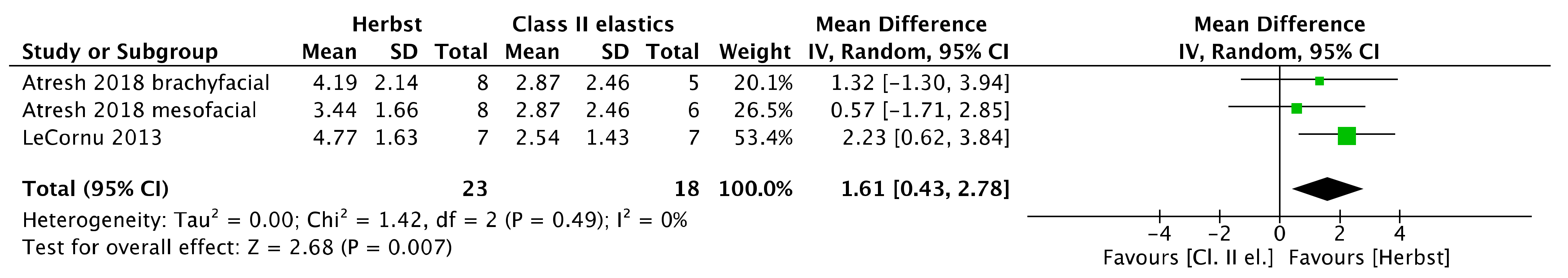
| right mandibular ramus height | The mean difference in right mandibular ramus height was 1.61 mm greater in the intervention group (0.43, 2.78) | 41 participants (2 observational studies) | ⊕⊕OO Low [43,44], * |
| left mandibular ramus height | The mean difference in left mandibular ramus height was 0.64 mm greater in the intervention group (−0.68, 1.97) | 41 participants (2 observational studies) | ⊕⊕OO Low [43,44], * |
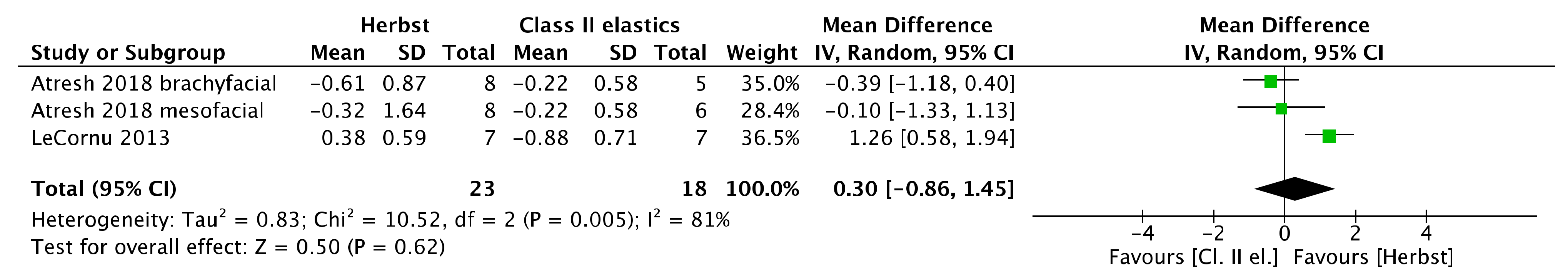
| right Co point (AP change) | The mean difference in right Co point was 0.3 mm more anteriorly in the intervention group (−0.86, 1.45) | 41 participants (2 observational studies) | ⊕OOO Very Low [43,44], * |
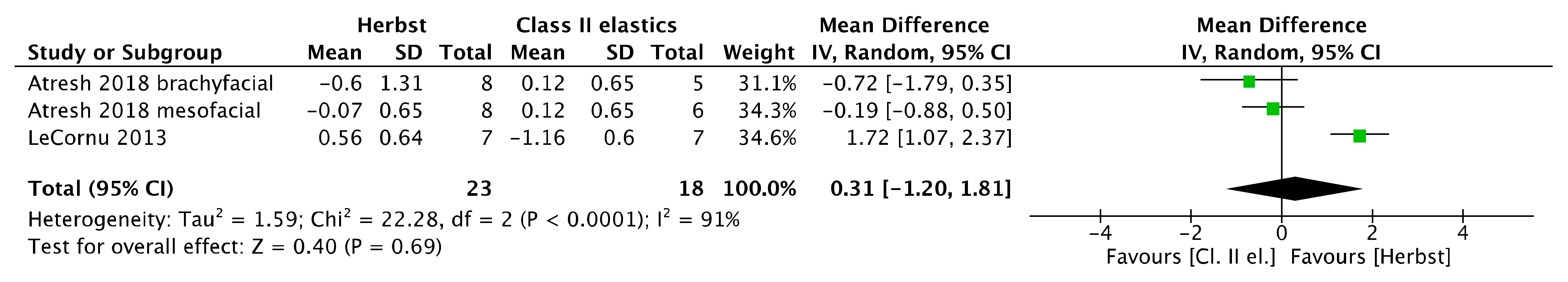
| left Co point (AP change) | The mean difference in left Co point was 0.31 mm more anteriorly in the intervention group (−1.2, 1.81) | 41 participants (2 observational studies) | ⊕OOO Very Low [43,44], * |
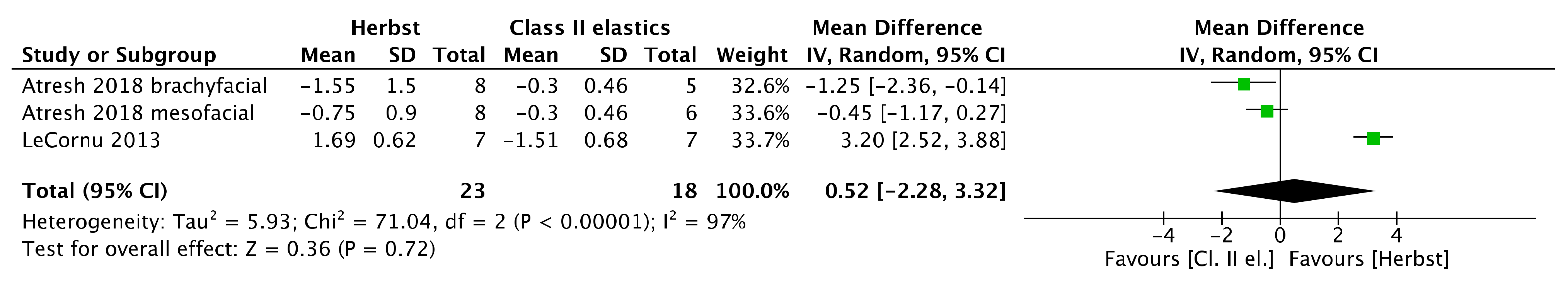
| right anterior glenoid fossa (AP change) | The mean difference in right anterior glenoid fossa was 0.52 mm more anteriorly in the intervention group (−2.28, 3.32). | 41 participants (2 observational studies) | ⊕OOO Very Low [43,44], * |
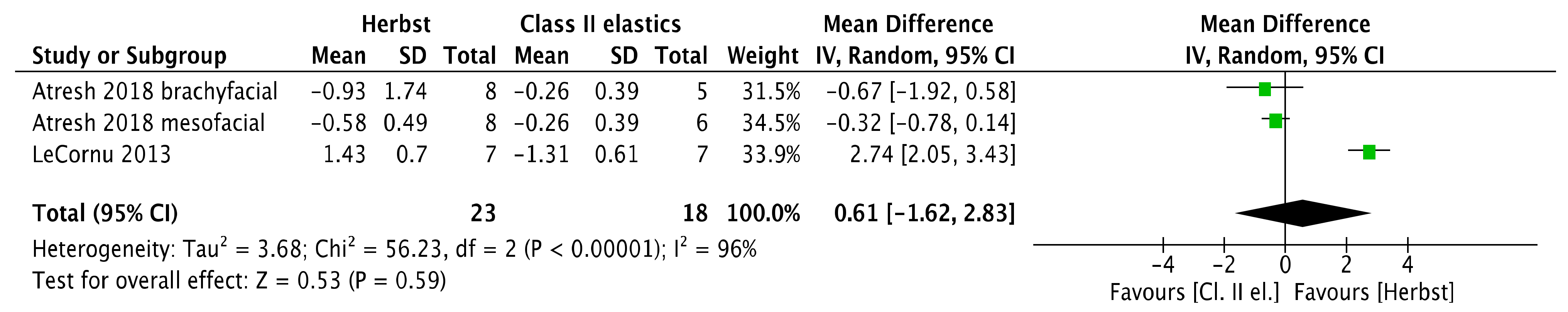
| left anterior glenoid fossa (AP change) | The mean difference in left anterior glenoid fossa was 0.61 mm more anteriorly in the intervention group (−1.62, 2.83). | 41 participants (2 observational studies) | ⊕OOO Very Low [43,44], * |
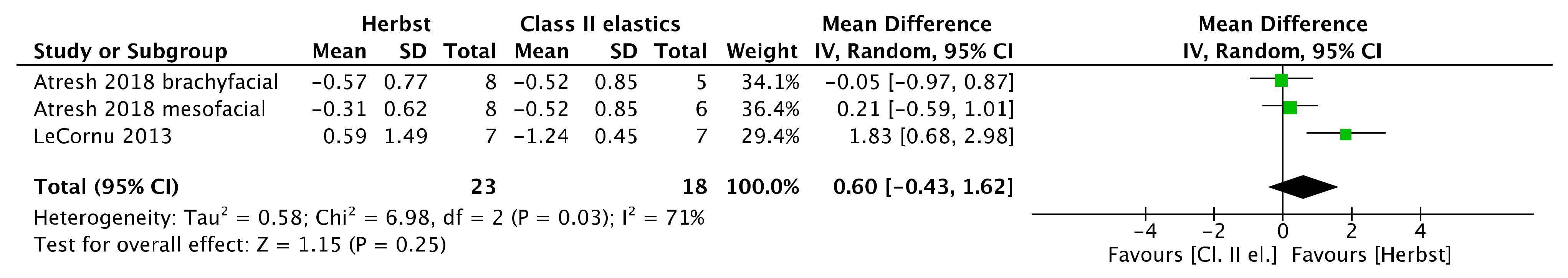
| right posterior glenoid fossa (AP change) | The mean difference in right posterior glenoid fossa was 0.6 mm more anteriorly in the intervention group (−0.43, 1.62). | 41 participants (2 observational studies) | ⊕OOO Very Low [43,44], * |
| left posterior glenoid fossa (AP change) | The mean difference in left posterior glenoid fossa was 0.57 mm in the intervention group (−0.8, 1.93). | 41 participants (2 observational studies) | ⊕OOO Very Low [43,44], * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matthaios, S.; Tsolakis, A.I.; Haidich, A.-B.; Galanis, I.; Tsolakis, I.A. Dental and Skeletal Effects of Herbst Appliance, Forsus Fatigue Resistance Device, and Class II Elastics—A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 6995. https://doi.org/10.3390/jcm11236995
Matthaios S, Tsolakis AI, Haidich A-B, Galanis I, Tsolakis IA. Dental and Skeletal Effects of Herbst Appliance, Forsus Fatigue Resistance Device, and Class II Elastics—A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2022; 11(23):6995. https://doi.org/10.3390/jcm11236995
Chicago/Turabian StyleMatthaios, Stefanos, Apostolos I. Tsolakis, Anna-Bettina Haidich, Ioannis Galanis, and Ioannis A. Tsolakis. 2022. "Dental and Skeletal Effects of Herbst Appliance, Forsus Fatigue Resistance Device, and Class II Elastics—A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 11, no. 23: 6995. https://doi.org/10.3390/jcm11236995
APA StyleMatthaios, S., Tsolakis, A. I., Haidich, A.-B., Galanis, I., & Tsolakis, I. A. (2022). Dental and Skeletal Effects of Herbst Appliance, Forsus Fatigue Resistance Device, and Class II Elastics—A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 11(23), 6995. https://doi.org/10.3390/jcm11236995