Clinical Characteristics, Risk Factors, and Outcomes of Acute Pulmonary Embolism in Asian Population
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Subject Selection
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Risk Factors
3.3. Clinical Presentation and Severity
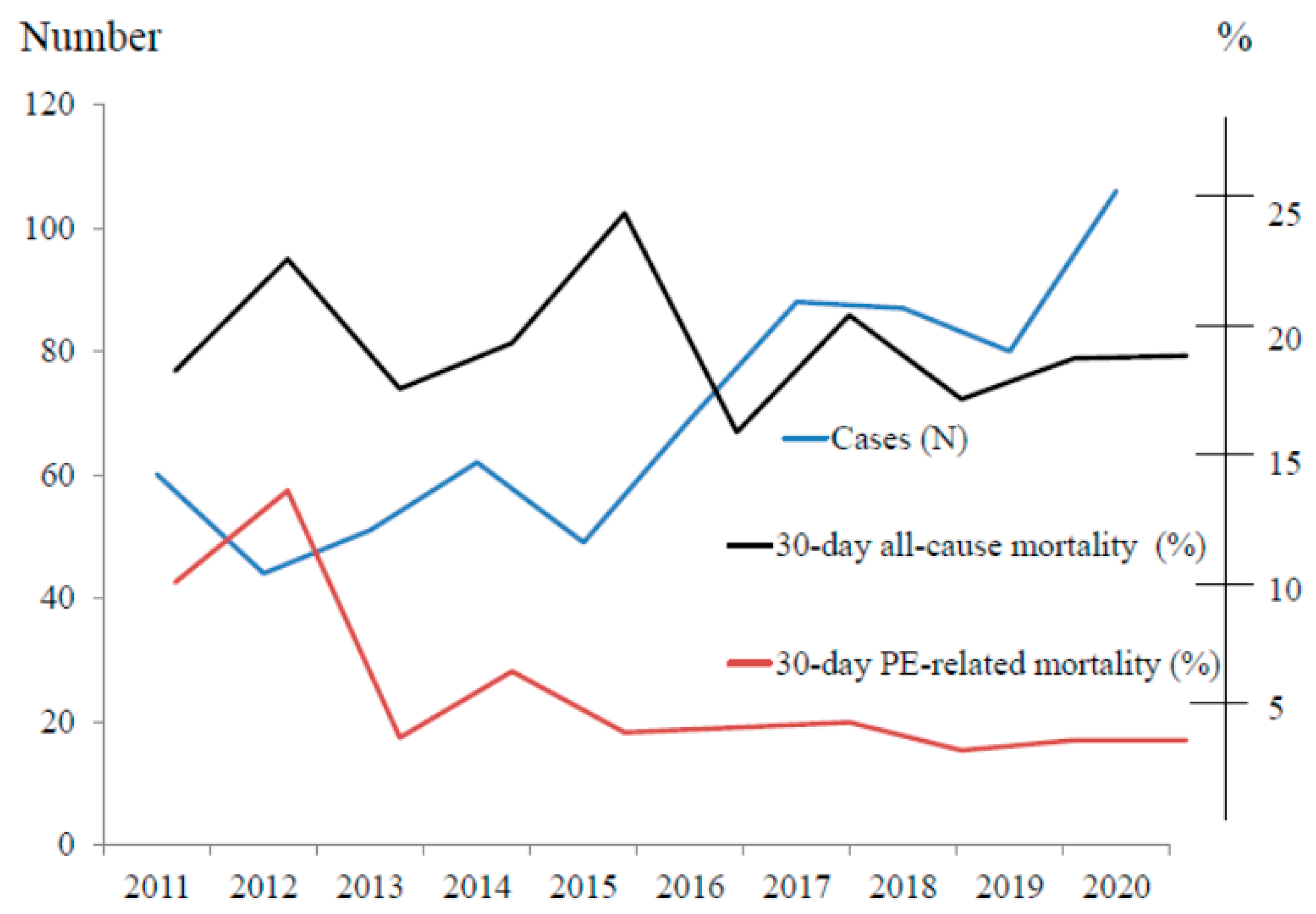
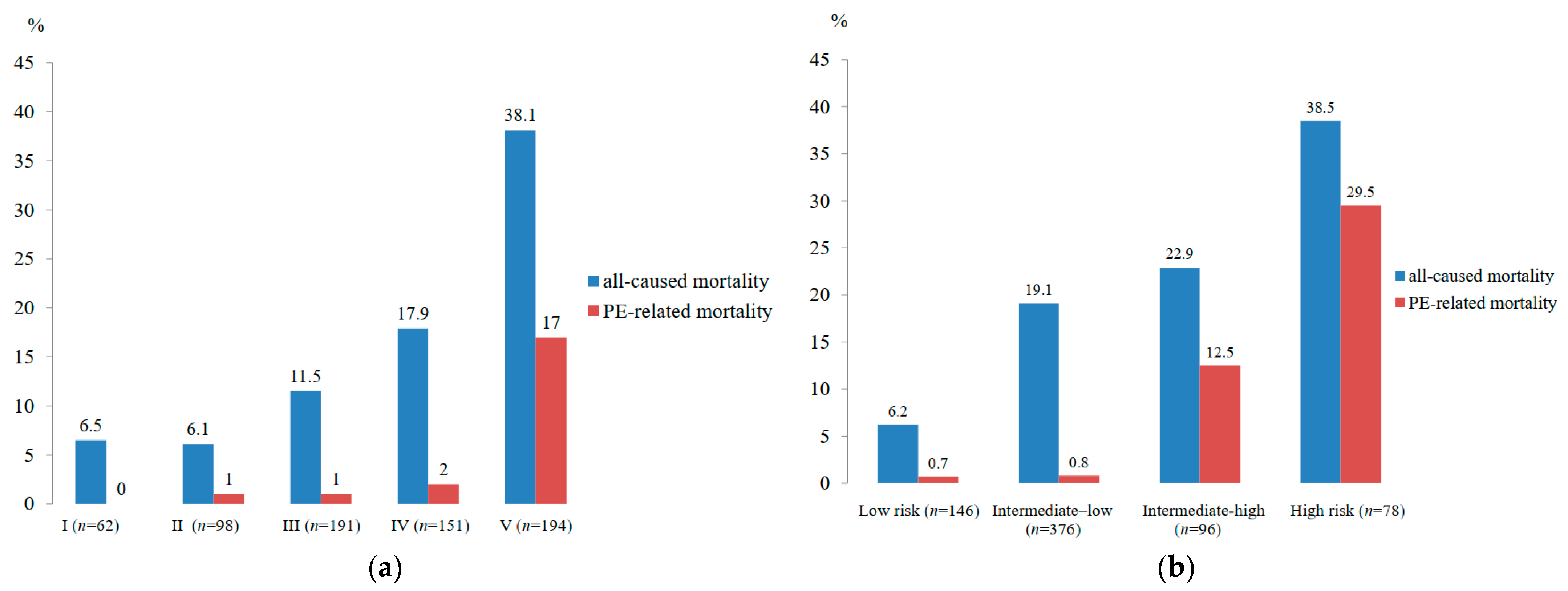
3.4. Treatments and Outcomes of APE
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wendelboe, A.M.; Raskob, G.E. Global burden of thrombosis: Epidemiologic aspects. Circ. Res. 2016, 118, 1340–1347. [Google Scholar] [CrossRef] [PubMed]
- Keller, K.; Hobohm, L.; Ebner, M.; Kresoja, K.P.; Münzel, T.; Konstantinides, S.V.; Lankeit, M. Trends in thrombolytic treatment and outcomes of acute pulmonary embolism in Germany. Eur. Heart J. 2020, 41, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Horlander, K.T.; Mannino, D.M.; Leeper, K.V. Pulmonary embolism mortality in the United States, 1979–1998: An analysis using multiple-cause mortality data. Arch. Intern. Med. 2003, 163, 1711–1717. [Google Scholar] [CrossRef] [PubMed]
- Goldhaber, S.Z.; Visani, L.; De Rosa, M. Acute pulmonary embolism: Clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet 1999, 353, 1386–1389. [Google Scholar] [CrossRef] [PubMed]
- ISTH Steering Committee for World Thrombosis Day. Thrombosis: A major contributor to the global disease burden. J. Thromb. Haemost. 2014, 12, 1580–1590. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.H.; Gallus, A.; Jindal, R.; Wang, C.; Wu, C.C. Incidence of venous thromboembolism in Asian populations: A systematic review. Thromb. Haemost. 2017, 117, 2243–2260. [Google Scholar] [CrossRef]
- Wang, K.L.; Yap, E.S.; Goto, S.; Zhang, S.; Siu, C.W.; Chiang, C.E. The diagnosis and treatment of venous thromboembolism in Asian patients. Thrombosis. J. 2018, 16, 4. [Google Scholar] [CrossRef]
- Konstantinides, S.V.; Meyer, G.; Becattini, C.; Bueno, H.; Geersing, G.J.; Harjola, V.P.; Huisman, M.V.; Humbert, M.; Jennings, C.S.; Jiménez, D.; et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). Eur. Respir. J. 2019, 54, 1901647. [Google Scholar]
- Pantic, N.; Pantic, I.; Jevtic, D.; Mogulla, V.; Oluic, S.; Durdevic, M.; Nordin, T.; Jecmenica, M.; Milovanovic, T.; Gavrancic, T.; et al. Celiac Disease and Thrombotic Events: Systematic Review of Published Cases. Nutrients 2022, 14, 2162. [Google Scholar] [CrossRef]
- Papa, A.; Tursi, A.; Danese, S.; Rapaccini, G.; Gasbarrini, A.; Papa, V. Venous Thromboembolism in Patients with Inflammatory Bowel Disease: The Role of Pharmacological Therapy and Surgery. J. Clin. Med. 2020, 9, 2115. [Google Scholar] [CrossRef]
- van Maanen, R.; Trinks-Roerdink, E.M.; Rutten, F.H.; Geersing, G.J. A systematic review and meta-analysis of diagnostic delay in pulmonary embolism. Eur. J. Gen. Pract. 2022, 28, 165–172. [Google Scholar] [CrossRef]
- Mansella, G.; Keil, C.; Nickel, C.H.; Eken, C.; Wirth, C.; Tzankov, A.; Peterson, C.J.; Aujesky, D.; Bingisser, R. Delayed Diagnosis in Pulmonary Embolism: Frequency, Patient Characteristics, and Outcome. Respiration 2020, 99, 589–597. [Google Scholar] [CrossRef]
- Wiener, R.S.; Schwartz, L.M.; Woloshin, S. Time trends in pulmonary embolism in the United States: Evidence of overdiagnosis. Arch. Intern. Med. 2011, 171, 831–837. [Google Scholar] [CrossRef]
- Park, T.Y.; Jung, J.W.; Choi, J.C.; Shin, J.W.; Kim, J.Y.; Choi, B.W.; Park, I.W. Epidemiological trend of pulmonary thromboembolism at a tertiary hospital in Korea. Korean. J. Intern. Med. 2017, 32, 1037–1044. [Google Scholar] [CrossRef][Green Version]
- Jiménez, D.; de Miguel-Díez, J.; Guijarro, R.; Trujillo-Santos, J.; Otero, R.; Barba, R.; Muriel, A.; Meyer, G.; Yusen, R.D.; Monreal, M.; et al. Trends in the Management and Outcomes of Acute Pulmonary Embolism: Analysis from the RIETE Registry. J. Am. Coll. Cardiol. 2016, 67, 162–170. [Google Scholar] [CrossRef]
- Sompradeekul, S.; Ittimakin, S. Clinical characteristics and outcome of Thai patients with acute pulmonary embolism. J. Med. Assoc. Thai. 2007, 90 (Suppl. S2), 59–67. [Google Scholar]
- Reechaipichitkul, W.; Wongthawa, N. Etiologies and treatment of acute pulmonary embolism at Srinagarind Hospital. Asian. Biomedicine. 2012, 6, 111–116. [Google Scholar]
- Chew, H.K.; Wun, T.; Harvey, D.; Zhou, H.; White, R.H. Incidence of venous thromboembolism and its effect on survival among patients with common cancers. Arch. Intern. Med. 2006, 166, 458–464. [Google Scholar] [CrossRef]
- Font, C.; Carmona-Bayonas, A.; Beato, C.; Reig, Ò.; Sáez, A.; Jiménez-Fonseca, P.; Plasencia, J.M.; Calvo-Temprano, D.; Sanchez, M.; Benegas, M.; et al. Clinical features and short-term outcomes of cancer patients with suspected and unsuspected pulmonary embolism: The EPIPHANY study. Eur. Respir. J. 2017, 49, 1600282. [Google Scholar] [CrossRef]
- Sripa, B.; Pairojkul, C. Cholangiocarcinoma: Lessons from Thailand. Curr. Opin. Gastroenterol. 2008, 24, 349–356. [Google Scholar] [CrossRef]
- Klok, F.A.; Huisman, M.V. Management of incidental pulmonary embolism. Eur. Respir. J. 2017, 49, 1700275. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Liang, L.; Zhai, Z.; He, H.; Xie, W.; Peng, X.; Wang, C.; Investigators for National Cooperative Project for Prevention and Treatment of PTE-DVT. Pulmonary embolism incidence and fatality trends in chinese hospitals from 1997 to 2008: A multicenter registration study. PLoS ONE 2011, 6, e26861. [Google Scholar] [CrossRef] [PubMed]
- Laporte, S.; Mismetti, P.; Décousus, H.; Uresandi, F.; Otero, R.; Lobo, J.L.; Monreal, M.; RIETE Investigators. Clinical predicttors for fatal pulmonary embolism in 15,520 patients with venous thromboembolism: Findings from the Registro Informatizado de la Enfermedad TromboEmbolica venosa (RIETE) Registry. Circulation 2008, 117, 1711–1716. [Google Scholar] [CrossRef] [PubMed]
- Stein, P.D.; Matta, F.; Hughes, P.G.; Hughes, M.J. Nineteen-Year Trends in Mortality of Patients Hospitalized in the United States with High-Risk Pulmonary Embolism. Am. J. Med. 2021, 134, 1260–1264. [Google Scholar] [CrossRef]
| Characteristics (n = 696) | Mean ± SD or n (%) |
|---|---|
| Age (years) | 57.7 ± 15.7 (range 15–98) |
| Sex | |
| Male sex | 286 (41.1) |
| Female sex | 410 (58.9) |
| Suspected APE | 468 (67.2) |
| Incidental APE | 228 (32.8) |
| Co-morbidities | 388 (55.7) |
| Hypertension | 305 (43.8) |
| Diabetes mellitus | 114 (16.4) |
| Renal diseases | 69 (9.9) |
| Chronic obstructive pulmonary disease | 38 (5.5) |
| Cirrhosis | 31 (4.5) |
| CAD with prior myocardial infarction | 30 (4.3) |
| Other chronic lung problems | 28 (4.0) |
| Hematologic diseases | 25 (3.6) |
| Connective tissue disease | 22 (3.2) |
| Thalassemia | 20 (2.9) |
| Obstructive sleep apnea | 15 (2.2) |
| Obesity (BMI ≥ 30 kg/m2) | 12 (1.7) |
| Nephrotic syndrome | 11 (1.6) |
| Splenectomy | 10 (1.4) |
| HIV infection | 9 (1.3) |
| Vasculitis | 3 (0.4) |
| Pregnancy | 2 (0.3) |
| Ulcerative colitis | 1 (0.1) |
| Active smoking | 24 (3.4) |
| Chronic alcohol drinking | 24 (3.4) |
| Medications | |
| Current antiplatelet | 62 (8.9) |
| Current anticoagulant | 35 (5.0) |
| Venous thromboembolism | |
| Current DVT proven by imaging | 245 (35.3) |
| Prior PE > 3 months | 12 (1.7) |
| Prior PE < 3 months | 4 (0.6) |
| Previous DVT, PE | 45 (6.5) |
| Wells score, 2-level | 4.49 ± 2.54 |
| Wells score ≤ 4 | 296 (42.5) |
| Wells score > 4 | 400 (57.5) |
| Wells score, 3-level | |
| Wells score < 2 | 144 (20.7) |
| Wells score 2–6 | 401 (57.6) |
| Wells score > 6 | 151 (21.7) |
| Characteristics (n = 696) | Mean ± SD or n (%) |
|---|---|
| Symptoms | |
| Dyspnea | |
| at rest | 453 (65.3) |
| at exertion | 274 (39.5) |
| Cough | 162 (23.3) |
| Respiratory failure (on invasive MV) | 129 (18.6) |
| Chest pain | 115 (16.5) |
| substernal | 64/115 (55.7) |
| pleuritic | 44/115 (38.2) |
| angina-like | 7/115 (6.1) |
| Syncope | 54 (7.8) |
| Palpitation | 52 (7.5) |
| Hemoptysis | 38 (5.5) |
| Dizziness | 33 (4.8) |
| Fever | 27 (3.9) |
| Altered mental status | 23 (3.3) |
| Cyanosis | 11 (1.6) |
| Diaphoresis | 9 (1.3) |
| Physical findings | |
| Oxygen desaturation (SpO2 < 90%) | 333 (48.3) |
| Room air SpO2 (%) | 89.4 ± 7.9 (38–100) |
| Tachycardia (HR > 110/min) | 326 (46.9) |
| HR (beats/min) | 105.4 ± 18.4 (46–160) |
| Tachypnea (RR ≥ 30/min) | 158 (22.7) |
| RR (breaths/min) | 24.3 ± 6.1 (14–60) |
| Extremity swelling suggestive of DVT | 127 (18.3) |
| leg | 104/127 (88.9) |
| thigh | 9/127 (7.7) |
| upper extremity | 4/127 (3.4) |
| Pain on limb palpation | 40 (5.8) |
| Low BP (<90/60 mmHg) | 83 (11.9) |
| SBP (mmHg) | 116.4 ± 21.9 (50–200) |
| DBP (mmHg) | 72.3 ± 13.9 (20–130) |
| Rales (crackles) | 142 (20.4) |
| Decreased breath sounds | 110 (15.8) |
| Wheeze & rhonchi | 37 (5.3) |
| Increased P2 | 26 (3.7) |
| Right ventricular lift | 23 (3.3) |
| Jugular venous distension | 22 (3.2) |
| Characteristics (n = 696) | n (%) |
|---|---|
| Acute treatment | |
| Heparin | |
| LMWH alone | 403 (57.9) |
| UFH alone | 127 (18.2) |
| UFH + LMWH | 104 (14.9) |
| Fondaparinux | 4 (0.6) |
| Thrombolytic therapy | 37 (5.3) |
| Surgical thromboembolectomy | 12 (1.7) |
| IVC filter | 14 (2.0) |
| Supportive care | 11 (1.6) |
| No treatment due to contraindication | 25 (3.6) |
| Denied treatment | 9 (1.3) |
| Long term treatment | |
| Warfarin | 252 (36.2) |
| LMWH | 247 (35.5) |
| DOACs | 40 (5.7) |
| Outcomes | Median (IQR) or n (%) |
|---|---|
| 30-day all-cause mortality | 133 (19.1) |
| 30-day PE-related mortality | 39 (5.6) |
| 30-day non-PE-related mortality | 94 (13.5) |
| Sepsis | 37 (39.4) |
| Pneumonia | 25 (26.6) |
| Cancer | 11 (11.7) |
| Septic shock | 10 (10.6) |
| Others | 11 (10.7) |
| Major bleeding | 57 (8.2%) |
| UGIH | 34 (4.9) |
| ICH | 11 (1.6) |
| LGIH | 8 (1.1) |
| Hemoptysis | 4 (0.6) |
| Recurrent PE within 14 days | 2 (0.3) |
| Hemodynamic collapse | 37 (5.3) |
| Mechanical ventilation (MV) support | 158 (22.7) |
| MV days (median, IQR) | 4 (2, 10) |
| Vasopressor | 90 (12.9) |
| Turn to CTEPH | 25 (3.6%) |
| Hospital stay (days) (median, IQR) | 12 (6, 23) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bumroongkit, C.; Deesomchok, A.; Liwsrisakun, C.; Pothirat, C.; Theerakittikul, T.; Limsukon, A.; Trongtrakul, K.; Tajarernmuang, P.; Niyatiwatchanchai, N.; Phrommintikul, A.; et al. Clinical Characteristics, Risk Factors, and Outcomes of Acute Pulmonary Embolism in Asian Population. J. Clin. Med. 2022, 11, 6954. https://doi.org/10.3390/jcm11236954
Bumroongkit C, Deesomchok A, Liwsrisakun C, Pothirat C, Theerakittikul T, Limsukon A, Trongtrakul K, Tajarernmuang P, Niyatiwatchanchai N, Phrommintikul A, et al. Clinical Characteristics, Risk Factors, and Outcomes of Acute Pulmonary Embolism in Asian Population. Journal of Clinical Medicine. 2022; 11(23):6954. https://doi.org/10.3390/jcm11236954
Chicago/Turabian StyleBumroongkit, Chaiwat, Athavudh Deesomchok, Chalerm Liwsrisakun, Chaicharn Pothirat, Theerakorn Theerakittikul, Atikun Limsukon, Konlawij Trongtrakul, Pattraporn Tajarernmuang, Nutchanok Niyatiwatchanchai, Arintaya Phrommintikul, and et al. 2022. "Clinical Characteristics, Risk Factors, and Outcomes of Acute Pulmonary Embolism in Asian Population" Journal of Clinical Medicine 11, no. 23: 6954. https://doi.org/10.3390/jcm11236954
APA StyleBumroongkit, C., Deesomchok, A., Liwsrisakun, C., Pothirat, C., Theerakittikul, T., Limsukon, A., Trongtrakul, K., Tajarernmuang, P., Niyatiwatchanchai, N., Phrommintikul, A., Chaikitmongkol, T., Euathrongchit, J., Rimsukcharoenchai, C., Inchai, J., & Chaiwong, W. (2022). Clinical Characteristics, Risk Factors, and Outcomes of Acute Pulmonary Embolism in Asian Population. Journal of Clinical Medicine, 11(23), 6954. https://doi.org/10.3390/jcm11236954






