PRAME Immuno-Expression in Cutaneous Sebaceous Carcinoma: A Single Institutional Experience
Abstract
1. Introduction
2. Materials and Methods
2.1. Case Selection
2.2. PRAME Immunostaining and Assessment of Positivity
2.3. Statistical Analysis
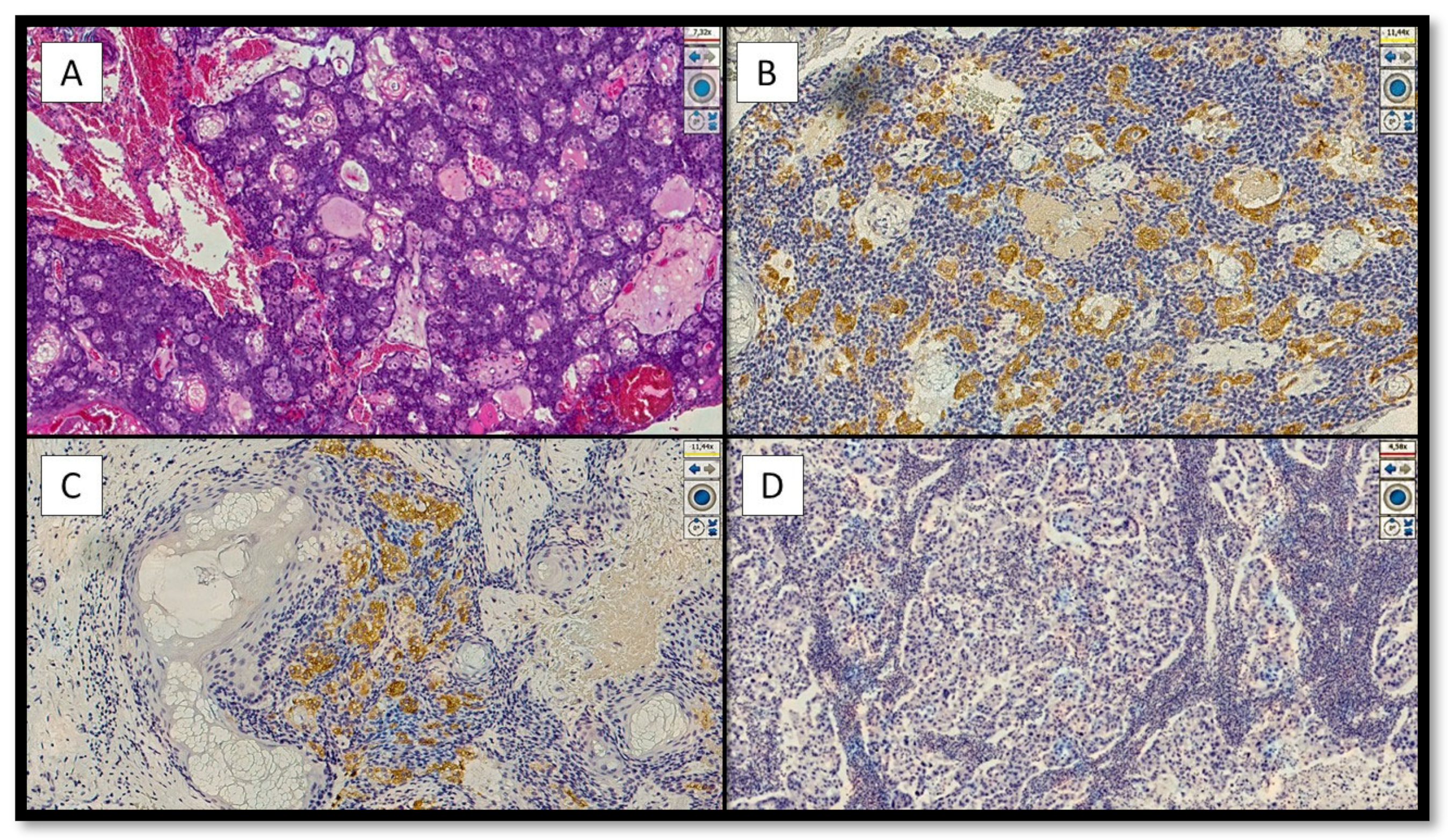
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Naik, A.; Thomas, R.; Al-Khadairi, G.; Bacha, R.; Hendrickx, W.; Decock, J. Cancer testis antigen PRAME: An anti-cancer target with immunomodulatory potential. J. Cell. Mol. Med. 2021, 25, 10376–10388. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, H.; Lethé, B.; Lehmann, F.; Van Baren, N.; Baurain, J.-F.; De Smet, C.; Chambost, H.; Vitale, M.; Moretta, A.; Boon, T.; et al. Characterization of an Antigen That Is Recognized on a Melanoma Showing Partial HLA Loss by CTL Expressing an NK Inhibitory Receptor. Immunity 1997, 6, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Al-Khadairi, G.; Decock, J. Cancer Testis Antigens and Immunotherapy: Where Do We Stand in the Targeting of PRAME? Cancers 2019, 11, 984. [Google Scholar] [CrossRef]
- Xu, Y.; Zou, R.; Wang, J.; Wang, Z.-W.; Zhu, X. The role of the cancer testis antigen PRAME in tumorigenesis and immunotherapy in human cancer. Cell Prolif. 2020, 53, e12770. [Google Scholar] [CrossRef] [PubMed]
- Lezcano, C.; Jungbluth, A.A.; Nehal, K.S.; Hollmann, T.J.; Busam, K.J. PRAME Expression in Melanocytic Tumors. Am. J. Surg. Pathol. 2018, 42, 1456–1465. [Google Scholar] [CrossRef] [PubMed]
- Cazzato, G.; Mangialardi, K.; Falcicchio, G.; Colagrande, A.; Ingravallo, G.; Arezzo, F.; Giliberti, G.; Trilli, I.; Loizzi, V.; Lettini, T.; et al. Preferentially Expressed Antigen in Melanoma (PRAME) and Human Malignant Melanoma: A Retrospective Study. Genes 2022, 13, 545. [Google Scholar] [CrossRef]
- Cazzato, G.; Cascardi, E.; Colagrande, A.; Belsito, V.; Lospalluti, L.; Foti, C.; Arezzo, F.; Dellino, M.; Casatta, N.; Lupo, C.; et al. PRAME Immunoexpression in 275 Cutaneous Melanocytic Lesions: A Double Institutional Experience. Diagnostics 2022, 12, 2197. [Google Scholar] [CrossRef]
- Albertsmeier, M.; Altendorf-Hofmann, A.; Lindner, L.H.; Issels, R.D.; Kampmann, E.; Dürr, H.-R.; Schubert-Fritschle, G.; Angele, M.K.; Kirchner, T.; Jungbluth, A.A.; et al. Cancer Testis Antigens and Immunotherapy: Expression of PRAME Is Associated with Prognosis in Soft Tissue Sarcoma. Cancers 2020, 12, 3612. [Google Scholar] [CrossRef]
- Pujol, J.-L.; De Pas, T.; Rittmeyer, A.; Vallières, E.; Kubisa, B.; Levchenko, E.; Wiesemann, S.; Masters, G.A.; Shen, R.; Tjulandin, S.A.; et al. Safety and Immunogenicity of the PRAME Cancer Immunotherapeutic in Patients with Resected Non–Small Cell Lung Cancer: A Phase I Dose Escalation Study. J. Thorac. Oncol. 2016, 11, 2208–2217. [Google Scholar] [CrossRef]
- Sun, Z.; Wu, Z.; Zhang, F.; Guo, Q.; Li, L.; Li, K.; Chen, H.; Zhao, J.; Song, D.; Huang, Q.; et al. PRAME is critical for breast cancer growth and metastasis. Gene 2016, 594, 160–164. [Google Scholar] [CrossRef]
- Neumann, E.; Engelsberg, A.; Decker, J.; Störkel, S.; Jaeger, E.; Huber, C.; Seliger, B. Heterogeneous expression of the tumor-associated antigens RAGE-1, PRAME, and glycoprotein 75 in human renal cell carcinoma: Candidates for T-cell-based immunotherapies? Cancer Res. 1998, 58, 4090–4095. [Google Scholar]
- Zhang, W.; Barger, C.J.; Eng, K.H.; Klinkebiel, D.; Link, P.A.; Omilian, A.; Bshara, W.; Odunsi, K.; Karpf, A.R. PRAME expression and promoter hypomethylation in epithelial ovarian cancer. Oncotarget 2016, 7, 45352–45369. [Google Scholar] [CrossRef]
- Ding, K.; Wang, X.-M.; Fu, R.; Ruan, E.-B.; Liu, H.; Shao, Z.-H. PRAME Gene Expression in Acute Leukemia and Its Clinical Significance. Cancer Biol. Med. 2012, 9, 73–76. [Google Scholar] [CrossRef]
- Luk, S.J.; Van Der Steen, D.M.; Hagedoorn, R.S.; Jordanova, E.S.; Schilham, M.W.; Bovée, J.V.; Cleven, A.H.; Falkenburg, J.F.; Szuhai, K.; Heemskerk, M.H. PRAME and HLA Class I expression patterns make synovial sarcoma a suitable target for PRAME specific T-cell receptor gene therapy. OncoImmunology 2018, 7, e1507600-11. [Google Scholar] [CrossRef]
- Ng, J.K.; Choi, P.C.; Chow, C.; Li, J.J.; Chan, A.W.; Cheung, C.M.; Ip, E.C.; Ng, H.; To, K. PRAME immunostain expression in sebaceous lesions, cutaneous carcinomas and adnexal structures. Pathology 2022, 54, 721–728. [Google Scholar] [CrossRef]
- Cesinaro, A.M.; Piana, S.; Paganelli, A.; Pedroni, G.; Santandrea, G.; Maiorana, A. PRAME expression in cellular neurothekeoma: A study of 11 cases. J. Cutan. Pathol. 2022, 49, 338–342. [Google Scholar] [CrossRef]
- Hrycaj, S.M.; Szczepanski, J.; Zhao, L.; Siddiqui, J.; Thomas, D.G.; Lucas, D.R.; Patel, R.M.; Harms, P.W.; Bresler, S.C.; Chan, M.P. PRAME expression in spindle cell melanoma, malignant peripheral nerve sheath tumor, and other cutaneous sarcomatoid neoplasms: A comparative analysis. Histopathology 2022, 81, 818–825. [Google Scholar] [CrossRef]
- Elsensohn, A.; Hanson, J.; Ferringer, T.C. Preferentially expressed antigen in melanoma expression in nonmelanoma skin cancers and melanocytes in surrounding skin. J. Cutan. Pathol. 2021, 48, 1150–1155. [Google Scholar] [CrossRef]
- Elder, D.; Massi, D.; Scolyer, R.; Willemze, R. WHO Classification of Skin Tumours, 4th ed.; IARC: Lyon, France, 2018; pp. 211–212. [Google Scholar]
- Owen, J.L.; Kibbi, N.; Worley, B.; Kelm, R.C.; Wang, J.V.; A Barker, C.; Behshad, R.; Bichakjian, C.K.; Bolotin, D.; Bordeaux, J.S.; et al. Sebaceous carcinoma: Evidence-based clinical practice guidelines. Lancet Oncol. 2019, 20, e699–e714. [Google Scholar] [CrossRef]
- Prieto-Granada, C.; Rodriguez-Waitkus, P. Sebaceous Carcinoma of the Eyelid. Cancer Control 2016, 23, 126–132. [Google Scholar] [CrossRef]
- Kibbi, N.; Worley, B.; Owen, J.L.; Kelm, R.C.; Bichakjian, C.K.; Chandra, S.; Demirci, H.; Kim, J.; Nehal, K.S.; Thomas, J.R.; et al. Sebaceous carcinoma: Controversies and their evidence for clinical practice. Arch. Dermatol. Res. 2020, 312, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Donnell, S.A.; LeBlanc, R.E.; Yan, S.; Parra, O.; Momtahen, S.; Sriharan, A.; Linos, K. Comparison of adipophilin and recently introduced PReferentially expressed Antigen in MElanoma immunohistochemistry in the assessment of sebaceous neoplasms: A pilot study. J. Cutan. Pathol. 2021, 48, 1252–1261. [Google Scholar] [CrossRef] [PubMed]
| Number of Case | Age | Gender | Topography | Treatment | PRAME Immunoexpression | WHO Grade |
|---|---|---|---|---|---|---|
| 1 | 89 | M | Upper Eyelid | Surgery + re-excision | Negative (3) | I |
| 2 | 76 | F | Lower Eyelid | Surgery + re-excision | Positive (6) | I |
| 3 | 78 | M | Eyelid | Surgery + re-excision | Negative (2) | II |
| 4 | 92 | M | Scalp | Surgery | Positive (5) | I |
| 5 | 83 | M | Scalp | Surgery | Negative (2) | II |
| 6 | 96 | F | Left preauricular | Surgery | Negative (3) | II |
| 7 | 68 | F | Right auricular | Surgery | Negative (3) | II |
| 8 | 63 | M | Not reported | Surgery + re-excision | Positive (4) | I |
| 9 | 70 | M | Forehead | Surgery + re-excision | Negative (3) | III |
| 10 | 67 | M | Left subscapularis | Surgery + re-excision | Positive (6) | I |
| 11 | 70 | M | Chest | Surgery + re-excision | Negative (2) | II |
| 12 | 98 | F | Right leg | Surgery | Positive (4) | I |
| 13 | 76 | F | Forehead | Surgery | Negative (2) | II |
| 14 | 29 | F | Chest | Surgery | Negative (2) | II |
| 15 | 70 | F | Lower eyelid | Surgery | Positive (5) | I |
| 16 | 61 | M | Forehead | Surgery + re-excision | Negative (3) | III |
| 17 | 79 | M | Neck | Surgery | Negative (2) | II |
| 18 | 67 | F | Forehead | Surgery | Positive (4) | I |
| 19 | 62 | M | Upper eyelid | Surgery + re-excision | Negative (2) | II |
| 20 | 88 | M | Right cheekbone | Surgery | Negative (2) | II |
| 21 | 86 | F | Conjunctival | Surgery + re-excision | Negative (2) | III |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cazzato, G.; Colagrande, A.; Ingravallo, G.; Lettini, T.; Filoni, A.; Ambrogio, F.; Bonamonte, D.; Dellino, M.; Lupo, C.; Casatta, N.; et al. PRAME Immuno-Expression in Cutaneous Sebaceous Carcinoma: A Single Institutional Experience. J. Clin. Med. 2022, 11, 6936. https://doi.org/10.3390/jcm11236936
Cazzato G, Colagrande A, Ingravallo G, Lettini T, Filoni A, Ambrogio F, Bonamonte D, Dellino M, Lupo C, Casatta N, et al. PRAME Immuno-Expression in Cutaneous Sebaceous Carcinoma: A Single Institutional Experience. Journal of Clinical Medicine. 2022; 11(23):6936. https://doi.org/10.3390/jcm11236936
Chicago/Turabian StyleCazzato, Gerardo, Anna Colagrande, Giuseppe Ingravallo, Teresa Lettini, Angela Filoni, Francesca Ambrogio, Domenico Bonamonte, Miriam Dellino, Carmelo Lupo, Nadia Casatta, and et al. 2022. "PRAME Immuno-Expression in Cutaneous Sebaceous Carcinoma: A Single Institutional Experience" Journal of Clinical Medicine 11, no. 23: 6936. https://doi.org/10.3390/jcm11236936
APA StyleCazzato, G., Colagrande, A., Ingravallo, G., Lettini, T., Filoni, A., Ambrogio, F., Bonamonte, D., Dellino, M., Lupo, C., Casatta, N., Resta, L., Maiorano, E., Cascardi, E., & Marzullo, A. (2022). PRAME Immuno-Expression in Cutaneous Sebaceous Carcinoma: A Single Institutional Experience. Journal of Clinical Medicine, 11(23), 6936. https://doi.org/10.3390/jcm11236936
















