Influence of Fracture Reduction on the Functional Outcome after Intramedullary Nail Osteosynthesis in Proximal Humerus Fractures
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Surgical Technique
2.3. Classification
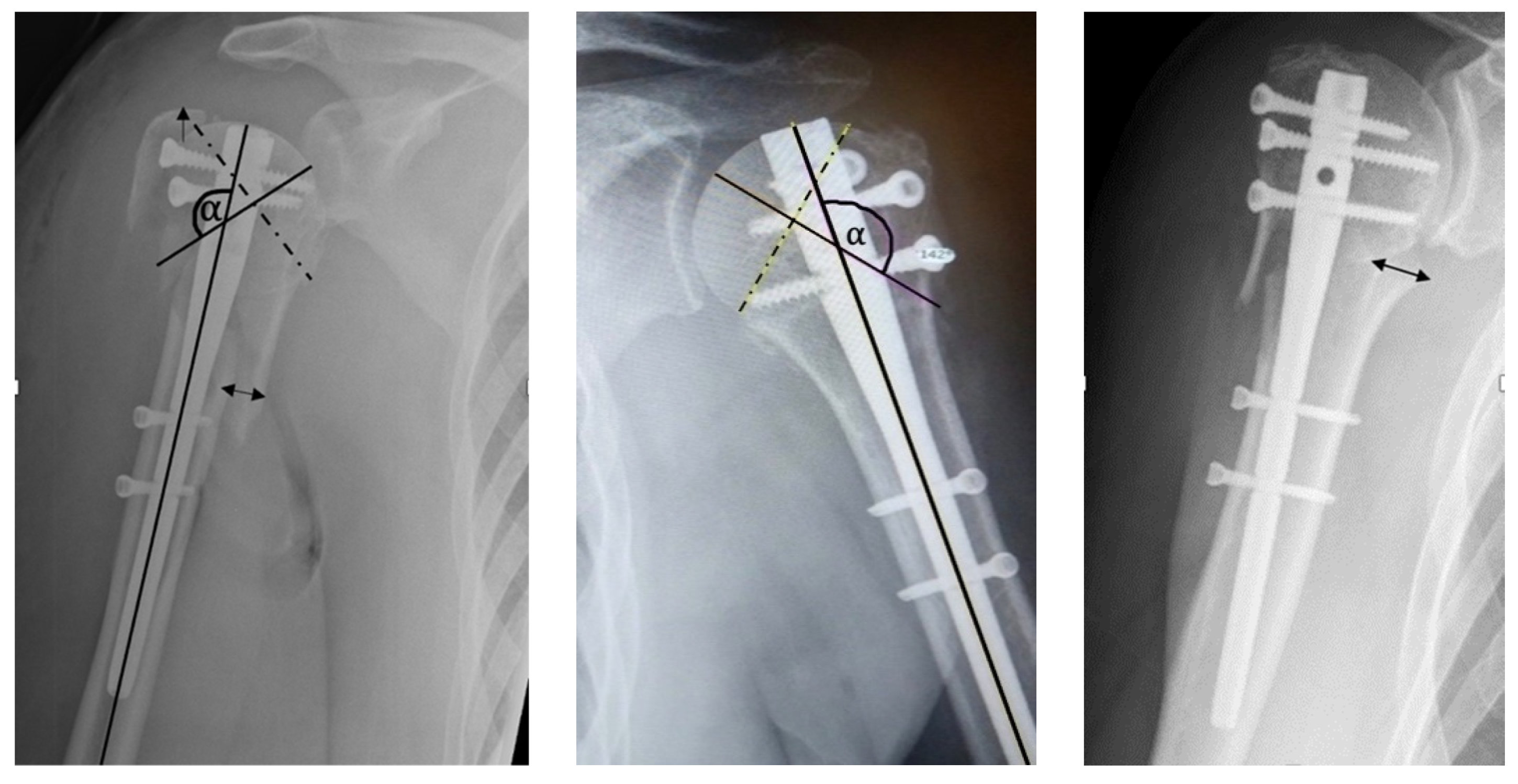
2.4. Radiographic Evaluation
2.5. Clinical Examination and Scores
2.6. Statistical Analysis
3. Results
3.1. Demographics
3.2. Classification
3.3. Radiographic Evaluation
3.4. Clinical Examination and Scores
3.5. Risk Factor Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Müller, U.; Grützner, P.A.; Studier-Fischer, S. Orthopädie und Unfallchirurgie up2date. GeJorg. Thieme Verl. 2020, 15, 127–140. [Google Scholar] [CrossRef]
- Beks, R.B.; Ochen, Y.; Frima, H.; Smeeing, D.P.; van der Meijden, O.; Timmers, T.K.; van der Velde, D.; van Heijl, M.; Leenen, L.P.; Groenwold, R.H.; et al. Operative versus nonoperative treatment of proximal humeral fractures: A systematic review, meta-analysis, and comparison of observational studies and randomized controlled trials. J. Shoulder Elbow Surg. 2018, 27, 1526–1534. [Google Scholar] [CrossRef] [PubMed]
- Tepass, A.; Blumenstock, G.; Weise, K.; Rolauffs, B.; Bahrs, C. Current strategies for the treatment of proximal humeral fractures: An analysis of a survey carried out at 348 hospitals in Germany, Austria, and Switzerland. J. Shoulder Elbow Surg. 2013, 22, e8–e14. [Google Scholar] [CrossRef] [PubMed]
- Krappinger, D.; Bizzotto, N.; Riedmann, S.; Kammerlander, C.; Hengg, C.; Kralinger, F.S. Predicting failure after surgical fixation of proximal humerus fractures. Injury 2011, 42, 1283–1288. [Google Scholar] [CrossRef] [PubMed]
- Lill, H. Die Proximale Humerusfraktur 3 Biomechanische und Knochenmorphologische Grundlagen der Frakturversorgung; Thieme: Stuttgart, Germany, 2006. [Google Scholar]
- Südkamp, N.P.; Audigé, L.; Lambert, S.; Hertel, R.; Konrad, G. Path analysis of factors for functional outcome at one year in 463 proximal humeral fractures. J. Shoulder Elbow Surg. 2011, 20, 1207–1216. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.W.; Shin, S.J. Prognostic factors for unstable proximal humeral fractures treated with locking-plate fixation. J. Shoulder Elbow Surg. 2009, 18, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Hertel, R.; Hempfing, A.; Stiehler, M.; Leunig, M. Predictors of humeral head ischemia after intracapsular fracure of the proximal humerus. J. Shoulder Elbow Surg. 2004, 13, 427–433. [Google Scholar] [CrossRef]
- Schnetzke, M.; Bockmeyer, J.; Porschke, F.; Studier-Fischer, S.; Grützner, P.A.; Guehring, T. Quality of Reduction Influences Outcome After Locked-Plate Fixation of Proximal Humeral Type-C Fractures. J. Bone Joint Surg. Am. 2016, 98, 1777–1785. [Google Scholar] [CrossRef] [PubMed]
- Neer, C.S., 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. J. Bone Joint Surg. Am. 1970, 52, 1077–1089. [Google Scholar] [CrossRef]
- Constant, C.R.; Gerber, C.; Emery, R.J.; Søjbjerg, J.O.; Gohlke, F.; Boileau, P. A review of the Constant score: Modifications and guidelines for its use. J. Shoulder Elbow Surg. 2008, 17, 355–361. [Google Scholar] [CrossRef]
- Boehm, D.; Wollmerstedt, N.; Doesch, M.; Handwerker, M.; Mehling, E.; Gohlke, F. Development of a questionnaire based on the Constant-Murley-Score for self-evaluation of shoulder function by patients. Unfallchirurg 2004, 107, 397–402. [Google Scholar] [PubMed]
- Hudak, P.L.; Amadio, P.C.; Bombardier, C. The Upper Extremity Collaborative Group (UECG). Development of an upper extremity outcome measure: The DASH (disabilities of the arm, shoulder and hand). Am. J. Ind. Med. 1996, 29, 602–608. [Google Scholar] [CrossRef]
- Siegel, S.; Castellan, N.J.J. Nonparametric Statistics for the Behavioral Sciences; McGraw-Hill: New York, NY, USA, 1988. [Google Scholar]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Blum, J.; Hansen, M.; Rommens, P.M. Angle-stable intramedullary nailing of proximal humerus fractures with the PHN (proximal humeral nail)]. Oper. Orthop. Traumatol. 2009, 21, 296–311. [Google Scholar] [CrossRef] [PubMed]
- Brorson, S.; Rasmussen, J.V.; Frich, L.H.; Olsen, B.S.; Hróbjartsson, A. Benefits and harms of locking plate osteosynthesis in intraarticular (OTA Type C) fractures of the proximal humerus: A systematic review. Injury 2012, 43, 999–1005. [Google Scholar] [CrossRef] [PubMed]
- Harvie, P.; Pollard, T.C.; Chennagiri, R.J.; Carr, A.J. The use of outcome scores in surgery of the shoulder. J. Bone Joint Surg. Br. 2005, 87, 151–154. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Liu, H.; Xing, R.; Mei, W.; Zhang, L.; Ding, L.; Huang, Z.; Wang, P. Effect of intramedullary nail and locking plate in the treatment of proximal humerus fracture: An update systematic review and meta-analysis. J. Orthop. Surg. Res. 2019, 14, 285. [Google Scholar] [CrossRef]
- Gracitelli, M.E.; Malavolta, E.A.; Assunção, J.H.; Kojima, K.E.; dos Reis, P.R.; Silva, J.S.; Ferreira Neto, A.A.; Hernandez, A.J. Locking intramedullary nails compared with locking plates for two- and three-part proximal humeral surgical neck fractures: A randomized controlled trial. J. Shoulder Elbow Surg. 2016, 25, 695–703. [Google Scholar] [CrossRef] [PubMed]
- Boudard, G.; Pomares, G.; Milin, L.; Lemonnier, I.; Coudane, H.; Mainard, D.; Delagoutte, J.P. Locking plate fixation versus antegrade nailing of 3- and 4-part proximal humerus fractures in patients without osteoporosis. Comparative retrospective study of 63 cases. Orthop. Traumatol. Surg. Res. 2014, 100, 917–924. [Google Scholar] [CrossRef]
- Von Rüden, C.; Trapp, O.; Hierholzer, C.; Prohaska, S.; Wurm, S. Bühren Intramedullary nailing vs. locking plate osteosynthesis in proximal humeral fractures: Long-term outcome. Unfallchirurg 2015, 118, 686–692. (In German) [Google Scholar] [CrossRef]
- Jawa, A.; Burnikel, D. Treatment of Proximal Humeral Fractures. JBJS Rev. 2016, 4, e2. [Google Scholar] [CrossRef] [PubMed]



| Anatomical Parameter | Anatomical | Acceptable | Malreduction |
|---|---|---|---|
| Head-Shaft-Displacement | Anatomical | <5 mm | >5 mm |
| Head-Shaft-Alignment | Normal, 120–150° | Minor varus, <120–100° | Valgus, >150°, <110° |
| Cranialization of the Greater Tuberosity | Anatomical | <5 mm | >5 mm |
| Parameter | N (%) or Mean ± SD (Range) | Data Distribution (Normality Test) |
|---|---|---|
| Gender male female | 15 (35.7%) 27 (64.3%) | --- |
| Age [years] | 65.5 ± 14.4 (22.9 to 86.1) | failed p < 0.001 † p < 0.001 ‡ |
| Handedness right left | 38 (90.5%) 4 (9.5%) | --- |
| Injured side right left | 24 (57.1%) 18 (42.9%) | --- |
| Injured side dominant non-dominant | 27 (64.3%) 15 (35.7%) | --- |
| Neer-classification III IV | 13 (31.0%) 29 (69.0%) | --- |
| Follow-up [months] | 43.0 ± 22.5 (12.6 to 88.5) | failed p < 0.001 † p < 0.001 ‡ |
| Kappa Values | p Value | Percentage Agreement | Level of Agreement a | |
|---|---|---|---|---|
| AO classification | 0.783 | <001 | 35/42 (83.3%) | good |
| Neer classification | 0.380 | 0.002 | 33/42 (78.6%) | fair |
| DASH score | 49.8 ± 24.3 (24.1 to 121.6) | Failed p = 0.022 †, p = 0.001 ‡ |
| SST score | 62.9 ± 26.9 (.0 to 100.0) | Passed p = 0.107 †, p = 0.074 ‡ |
| Constant Score injured side | 60.0 ± 23.0(16 to 99) | Failed, p = 0.006 †, p = 0.004 ‡ |
| Constant Score healthy side | 82.2 ± 9.5 (55 to 100) | Passed p = 0.200 †, p = 0.036 ‡ |
| Score | Group 1 | Group 2 | p-Value |
|---|---|---|---|
| DASH score | 45.2 ± 24.4 (24.1 to 100.0) | 51.9 ± 21.9 (24.1 to 91.4) | p = 0.307 |
| SST score | 69.3 ± 30.1 (.0 to 100.0) | 58.6 ± 24.2 (8.3 to 91.7) | p = 0.400 |
| CS injured side | 67.2 ± 22.4 (16 to 99) | 55.2 ± 22.5 (19 to 88) | p = 0.095 |
| Regression Parameter | 95% CI | |||||||
|---|---|---|---|---|---|---|---|---|
| Predictor | Beta | SE Beta | Wald’s χ2 | df | p-Value | OR | Lower | Upper |
| Age | 0.353 | 0.195 | 3.259 | 1 | 0.071 | 1.42 | 0.97 | 2.08 |
| Gender | −1.198 | 2.463 | 0.237 | 1 | 0.627 | 0.30 | 0.00 | 37.67 |
| AO classification | −3.471 | 2.382 | 2.124 | 1 | 0.145 | 0.03 | 0.00 | 3.31 |
| Head-shaft-displacement | 1.917 | 0.888 | 4.185 | 1 | 0.041 | 6.15 | 1.08 | 35.08 |
| Head-shaft-alignment | 0.181 | 0.135 | 1.998 | 1 | 0.158 | 1.21 | 0.93 | 1.58 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hättich, A.; Harloff, T.J.; Sari, H.; Schlickewei, C.; Cramer, C.; Strahl, A.; Frosch, K.-H.; Mader, K.; Klatte, T.O. Influence of Fracture Reduction on the Functional Outcome after Intramedullary Nail Osteosynthesis in Proximal Humerus Fractures. J. Clin. Med. 2022, 11, 6861. https://doi.org/10.3390/jcm11226861
Hättich A, Harloff TJ, Sari H, Schlickewei C, Cramer C, Strahl A, Frosch K-H, Mader K, Klatte TO. Influence of Fracture Reduction on the Functional Outcome after Intramedullary Nail Osteosynthesis in Proximal Humerus Fractures. Journal of Clinical Medicine. 2022; 11(22):6861. https://doi.org/10.3390/jcm11226861
Chicago/Turabian StyleHättich, Annika, Tim Jodokus Harloff, Hatice Sari, Carsten Schlickewei, Christopher Cramer, André Strahl, Karl-Heinz Frosch, Konrad Mader, and Till Orla Klatte. 2022. "Influence of Fracture Reduction on the Functional Outcome after Intramedullary Nail Osteosynthesis in Proximal Humerus Fractures" Journal of Clinical Medicine 11, no. 22: 6861. https://doi.org/10.3390/jcm11226861
APA StyleHättich, A., Harloff, T. J., Sari, H., Schlickewei, C., Cramer, C., Strahl, A., Frosch, K.-H., Mader, K., & Klatte, T. O. (2022). Influence of Fracture Reduction on the Functional Outcome after Intramedullary Nail Osteosynthesis in Proximal Humerus Fractures. Journal of Clinical Medicine, 11(22), 6861. https://doi.org/10.3390/jcm11226861






