Renal Protection and Hemodynamic Improvement by Impella® Microaxial Pump in Patients with Cardiogenic Shock
Abstract
1. Background
2. Methods and Patients
2.1. Study Design
2.2. Patients
2.3. Renal Resistive Index (RRI)
2.4. Invasive Hemodynamic Measurement (Pulmonalis Catheter, PAC)
2.5. Clinical Data/Parameters
2.6. Statistical Analysis
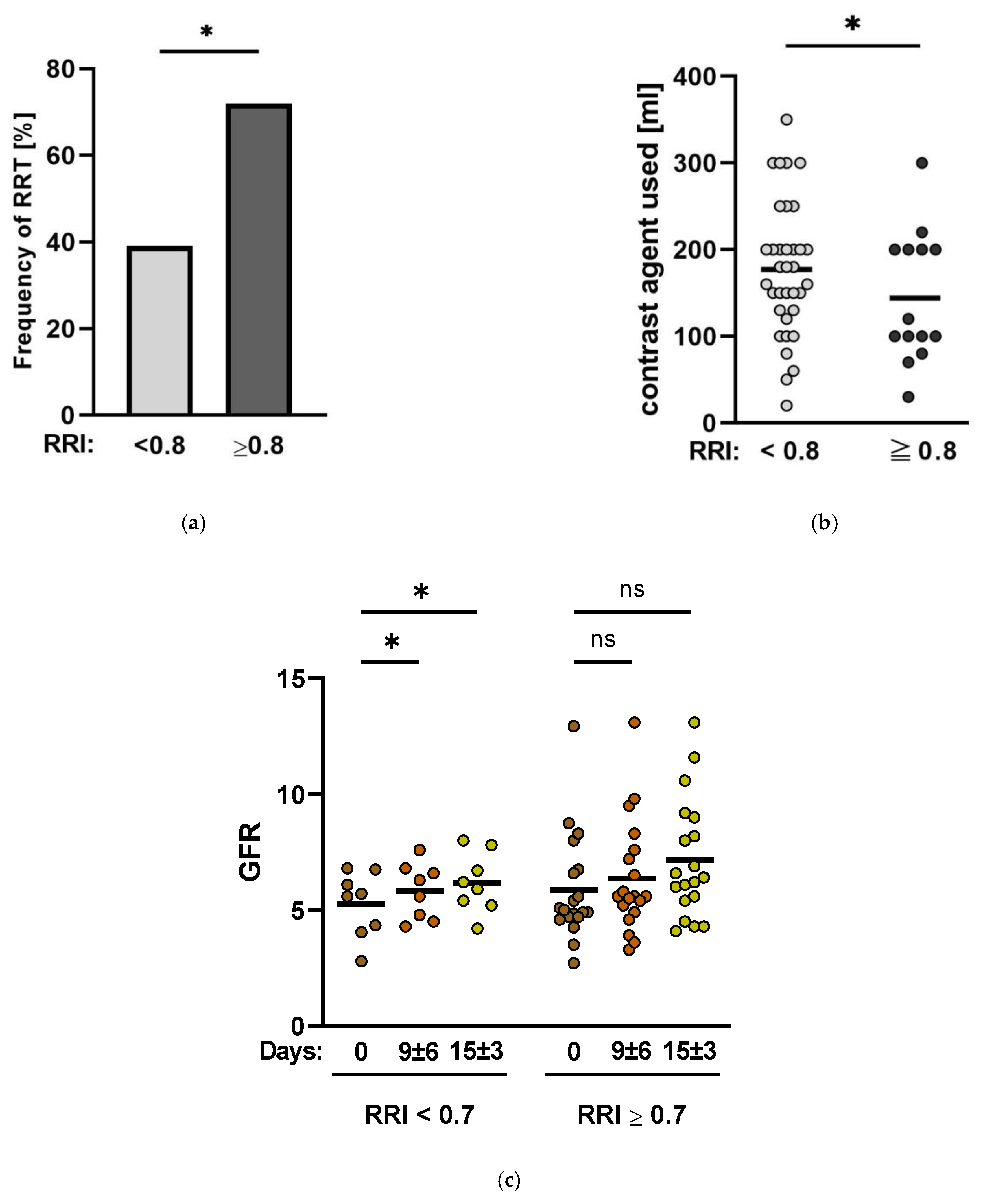
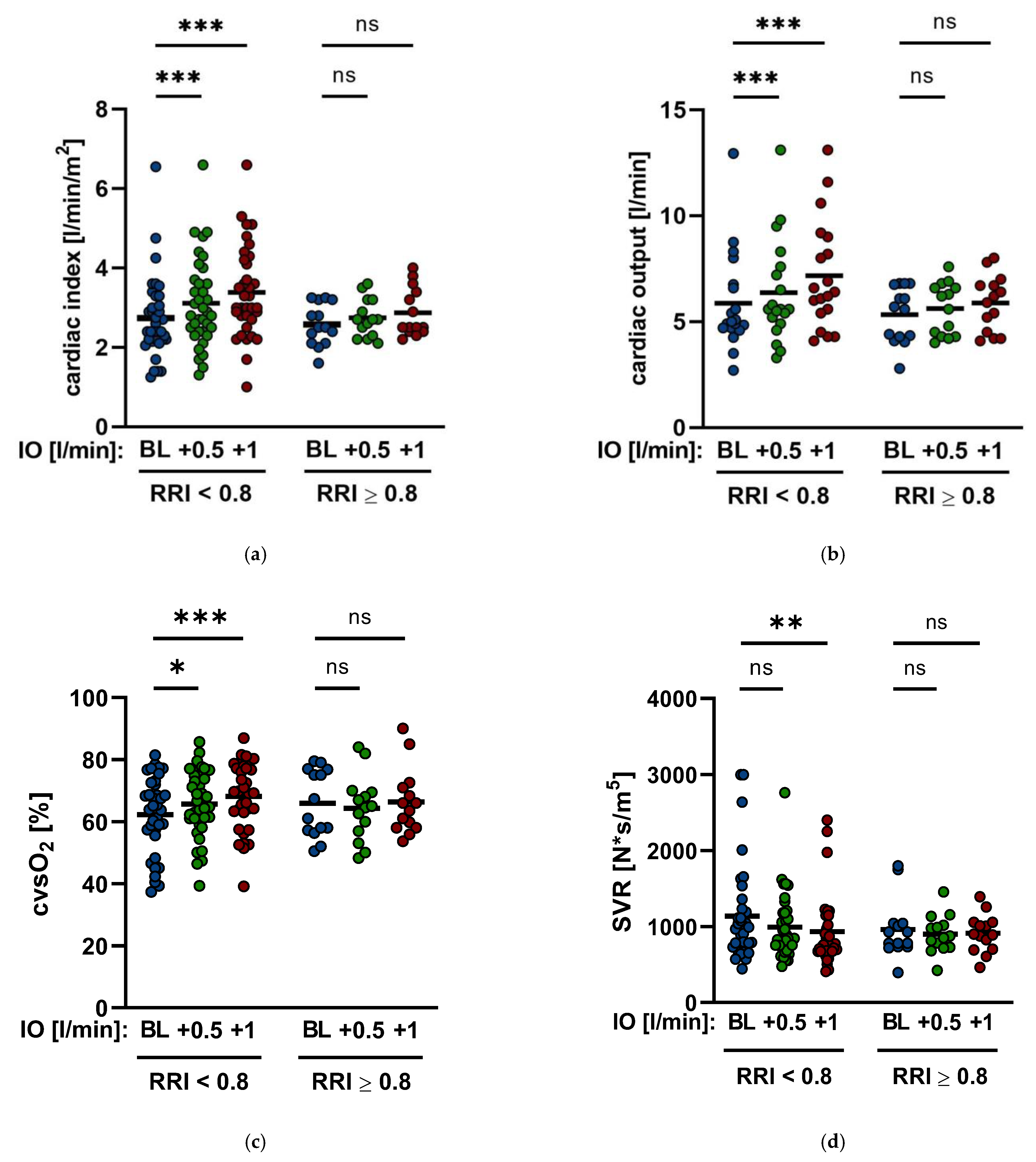
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ghionzoli, N.; Sciaccaluga, C.; Mandoli, G.E.; Vergaro, G.; Gentile, F.; D’Ascenzi, F.; Mondillo, S.; Emdin, M.; Valente, S.; Cameli, M. Cardiogenic shock and acute kidney injury: The rule rather than the exception. Heart Fail. Rev. 2021, 26, 487–496. [Google Scholar] [CrossRef] [PubMed]
- Mikhailovich Mezhonov, E.; Aleksandrovna Vialkina, J.; Aleksandrovna Vakulchik, K.; Vasilevich Shalaev, S. Acute kidney injury in patients with ST-segment elevation acute myocardial infarction: Predictors and outcomes. Saudi J. Kidney Dis. Transplant. 2021, 2, 318–327. [Google Scholar] [CrossRef] [PubMed]
- Tarvasmäki, T.; Haapio, M.; Mebazaa, A.; Sionis, A.; Silva-Cardoso, J.; Tolppanen, H.; Lindholm, M.G. Acute kidney injury in cardiogenic shock: Definitions, incidence, haemodynamic alterations, and mortality. Eur. J. Heart Fail. 2018, 20, 572–581. [Google Scholar] [CrossRef]
- Cosentino, N.; Somaschini, A.; Campodonico, J.; Lucci, C.; Moltrasio, M.; Bonomi, A.; Cornara, S.; Camporotondo, R.; Demarchi, A.; Ferrari, G.d.M.; et al. Acute kidney injury and in-hospital mortality in patients with ST-elevation myocardial infarction of different age groups. Int. J. Cardiol. 2021, 344, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Vallabhajosyula, S.; Dunlay, S.M.; Barsness, G.W.; Vallabhajosyula, S.; Vallabhajosyula, S.; Sundaragiri, P.R.; Gersh, B.J.; Jaffe, A.S.; Kashani, K. Temporal trends, predictors, and outcomes of acute kidney injury and hemodialysis use in acute myocardial infarction-related cardiogenic shock. PLoS ONE 2019, 14, e0222894. [Google Scholar] [CrossRef]
- Lauridsen, M.D.; Gammelager, H.; Schmidt, M.; Rasmussen, T.B.; Shaw, R.E.; Bøtker, H.E.; Sørensen, H.T.; Christiansen, C.F. Acute kidney injury treated with renal replacement therapy and 5-year mortality after myocardial infarction-related cardiogenic shock: A nationwide population-based cohort study. Crit. Care 2015, 19, 452. [Google Scholar] [CrossRef]
- Sheikh, O.; Nguyen, T.; Bansal, S.; Prasad, A. Acute kidney injury in cardiogenic shock: A comprehensive review. Catheter Cardiovasc. Catheter. Cardiovasc. Interv. 2021, 98, E91–E105. [Google Scholar] [CrossRef]
- Karatolios, K.; Chatzis, G.; Markus, B.; Luesebrink, U.; Ahrens, H.; Dersch, W.; Betz, S.; Ploeger, B.; Boesl, E.; O’Neill, W.; et al. Impella support compared to medical treatment for post-cardiac arrest shock after out of hospital cardiac arrest. Resuscitation 2018, 126, 104–110. [Google Scholar] [CrossRef]
- Lüsebrink, E.; Kellnar, A.; Krieg, K.; Binzenhöfer, L.; Scherer, C.; Zimmer, S.; Schrage, B.; Fichtner, S.; Petzold, T.; Braun, D.; et al. Percutaneous Transvalvular Microaxial Flow Pump Support in Cardiology. Circulation 2022, 145, 1254–1284. [Google Scholar] [CrossRef]
- Upadhyaya, V.D.; Alshami, A.; Patel, I.; Douedi, S.; Quinlan, A.; Thomas, T.; Prentice, J.; Calderon, D.; Asif, A.; Sen, S.; et al. Outcomes of Renal Function in Cardiogenic Shock Patients With or Without Mechanical Circulatory Support. J. Clin. Med. Res. 2021, 13, 283–292. [Google Scholar] [CrossRef]
- Flaherty, M.P.; Pant, S.; Patel, S.V.; Kilgore, T.; Dassanayaka, S.; Loughran, J.H.; Rawasia, W.; Dawn, B.; Cheng, A.; Bartoli, C.R. Hemodynamic Support With a Microaxial Percutaneous Left Ventricular Assist Device (Impella) Protects Against Acute Kidney Injury in Patients Undergoing High-Risk Percutaneous Coronary Intervention. Circ. Res. 2017, 120, 692–700. [Google Scholar] [CrossRef] [PubMed]
- Chatzis, G.; Markus, B.; Luesebrink, U.; Ahrens, H.; Divchev, D.; Syntila, S.; Scheele, N.; al Eryani, H.; Tousoulis, D.; Schieffer, B.; et al. Early Impella Support in Postcardiac Arrest Cardiogenic Shock Complicating Acute Myocardial Infarction Improves Short- and Long-Term Survival. Crit. Care Med. 2021, 49, 943–955. [Google Scholar] [CrossRef] [PubMed]
- Fotopoulou, G.; Poularas, I.; Kokkoris, S.; Charitidou, E.; Boletis, I.; Brountzos, E.; Benetos, A.; Zakynthinos, S.; Routsi, C. Renal Resistive Index on Intensive Care Unit Admission Correlates With Tissue Hypoperfusion Indices and Predicts Clinical Outcome. Shock 2022, 57, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Cauwenberghs, N.; Kuznetsova, T. Determinants and prognostic significance of the renal resistive index. Pulse 2016, 3, 172–178. [Google Scholar] [CrossRef]
- Haitsma Mulier, J.L.G.; Rozemeijer, S.; Röttgering, J.G.; Spoelstra-de Man, A.M.E.; Elbers, P.W.G.; Roel Tuinman, P. Renal resistive index as an early predictor and discriminator of acute kidney injury in critically ill patients; A prospective observational cohort study. PLoS ONE 2018, 13, e0197967. [Google Scholar] [CrossRef]
- Darmon, M.; Schortgen, F.; Vargas, F.; Liazydi, A.; Schlemmer, B.; Brun-Buisson, C.; Brochard, L. Diagnostic accuracy of Doppler renal resistive index for reversibility of acute kidney injury in critically ill patients. Intensive Care Med. 2011, 37, 68–76. [Google Scholar] [CrossRef]
- Tublin, M.E.; Bude, R.O.; Platt, J.F. The resistive index in renal Doppler sonography: Where do we stand? Am. J. Roentgenol. 2003, 180, 885–892. [Google Scholar] [CrossRef]
- Toledo, C.; Thomas, G.; Schold, J.D.; Arrigain, S.; Gornik, H.L.; Nally, J.V.; Navaneethan, S.D. Renal resistive index and mortality in chronic kidney disease. Hypertension 2015, 66, 382–388. [Google Scholar] [CrossRef]
- Lubas, A.; Kade, G.; Niemczyk, S. Renal resistive index as a marker of vascular damage in cardiovascular diseases. Int. Urol. Nephrol. 2014, 46, 395–402. [Google Scholar] [CrossRef]
- Markus, B.; Patsalis, N.; Chatzis, G.; Luesebrink, U.; Ahrens, H.; Schieffer, B.; Karatolios, K. Impact of microaxillar mechanical left ventricular support on renal resistive index in patients with cardiogenic shock after myocardial infarction: A pilot trial to predict renal organ dysfunction in cardiogenic shock. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 158–163. [Google Scholar] [CrossRef]
- Ponte, B.; Pruijm, M.; Ackermann, D.; Vuistiner, P.; Eisenberger, U.; Guessous, I.; Rousson, V.; Mohaupt, M.G.; Alwan, H.; Ehret, G.; et al. Reference values and factors associated with renal resistive index in a family-based population study. Hypertension 2014, 63, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Pruijm, M.; Ponte, B.; Ackermann, D.; Vuistiner, P.; Paccaud, F.; Guessous, I.; Ehret, G.; Eisenberger, U.; Mohaupt, M.; Burnier, M.; et al. Heritability, determinants and reference values of renal length: A family-based population study. Eur. Radiol. 2013, 23, 2899–2905. [Google Scholar] [CrossRef] [PubMed]
- Boddi, M.; Natucci, F.; Ciani, E. The internist and the renal resistive index: Truths and doubts. Intern. Emerg. Med. 2015, 1, 893–905. [Google Scholar] [CrossRef] [PubMed]
- Schnell, D.; Darmon, M. Bedside Doppler ultrasound for the assessment of renal perfusion in the ICU: Advantages and limitations of the available techniques. Crit. Ultrasound J. 2015, 7, 24. [Google Scholar] [CrossRef] [PubMed]
- Damman, K.; Navis, G.; Smilde, T.D.J.; Voors, A.A.; van der Bij, W.; van Veldhuisen, D.J.; Hillege, H. Decreased cardiac output, venous congestion and the association with renal impairment in patients with cardiac dysfunction. Eur. J. Heart Fail. 2007, 9, 872–878. [Google Scholar] [CrossRef]
- Grande, D.; Terlizzese, P.; Iacoviello, M. Role of imaging in the evaluation of renal dysfunction in heart failure patients. World J. Nephrol. 2017, 6, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Rozemeijer, S.; Haitsma Mulier, J.L.G.; Röttgering, J.G.; Paul, W.G.; Elbers Angélique, M.E.; Man, S.; Tuinman, P.R.; de Waard, H.; Straaten, M. Renal Resistive index: Response to shock and its determideterminantsin critically ill patients. Shock 2019, 1, 43–51. [Google Scholar] [CrossRef]

| Demographics and Characteristics | |
|---|---|
| Age (years) | 67 ± 13 |
| Female (%) | 26 |
| Male (%) | 74 |
| 1-vessel CHD (%) | 28 |
| 2-vessel CHD (%) | 26 |
| 3-vessel-CHD (%) | 36 |
| BMI | 26.4 ± 3.4 |
| SAP (mmHg) during measurements | 113 ± 19 |
| DAP (mmHg) during measurements | 60 ± 11 |
| MAP (mmHg) during measurements | 85.4 ± 17 |
| Baseline Creatinine (mg/dL) (at Impella® insertion) | 2.89 ± 2.8 |
| Impella® (days) | 9 ± 6 |
| Impella®-support (min/max. L/min) | 1.5/2.5 L/min ± 0.4 L/min |
| Noradrenaline (µg/kg/min) overall cohort | 0.12 ± 0.19 |
| Noradrenaline (µg/kg/min) RRI ≥ 0.8 | 0.36 ± 0.34 |
| Noradrenaline (µg/kg/min) RRI < 0.8 | 0.12 ± 0.24 |
| Dobutamine (µg/kg/min) overall cohort | 3.1 ± 2.67 |
| Dobutamine (µg/kg/min) RRI ≥ 0.8 | 5.9 ± 2.5 |
| Dobutamine (µg/kg/min) RRI < 0.8 | 3.9 ± 2.5 |
| Renal longitudinal length (cm) | 9.32 ± 1.1 |
| Renal parenchymal thickness (cm) | 2.1 ± 0.4 |
| LVEF at Impella® insertion (%) | 37 ± 18 |
| Baseline | +0.5 L/min | +1.0 L/min | Baseline | |
|---|---|---|---|---|
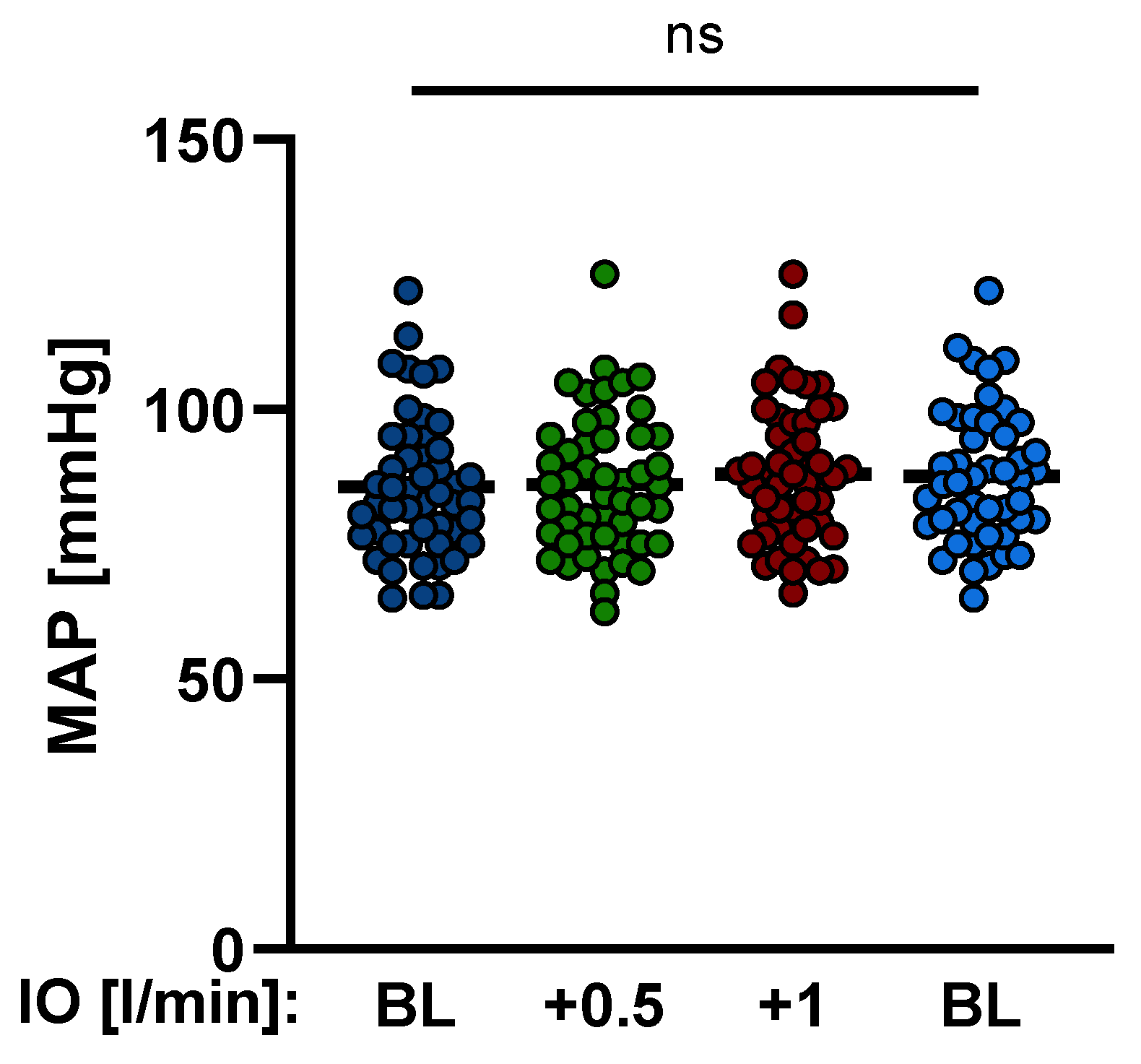
| MAP (mmHg) | 85.6 ± 12.1 | 86.1 ± 12.7 | 89.1 ± 12.8 | 87.7 ± 12.5 |
| SAP (mmHg) | 110.9 ± 18.1 | 111.1 ± 18.8 | 111.53 ± 18.9 | 111.86 ± 17.5 |
| DAP (mmHg) | 59.61 ± 11.1 | 59.88 ± 11.0 | 60.22 ± 11.9 | 60.6 ± 12.4 |
| Noradrenaline (µg/kg/min) | 0.12 ± 0.19 | 0.12 ± 0.19 | 0.12 ± 0.19 | 0.12 ± 0.19 |
| Dobutamine (µg/kg/min) | 3.1 ± 2.67 | 3.1 ± 2.67 | 3.1 ± 2.67 | 3.1 ± 2.67 |
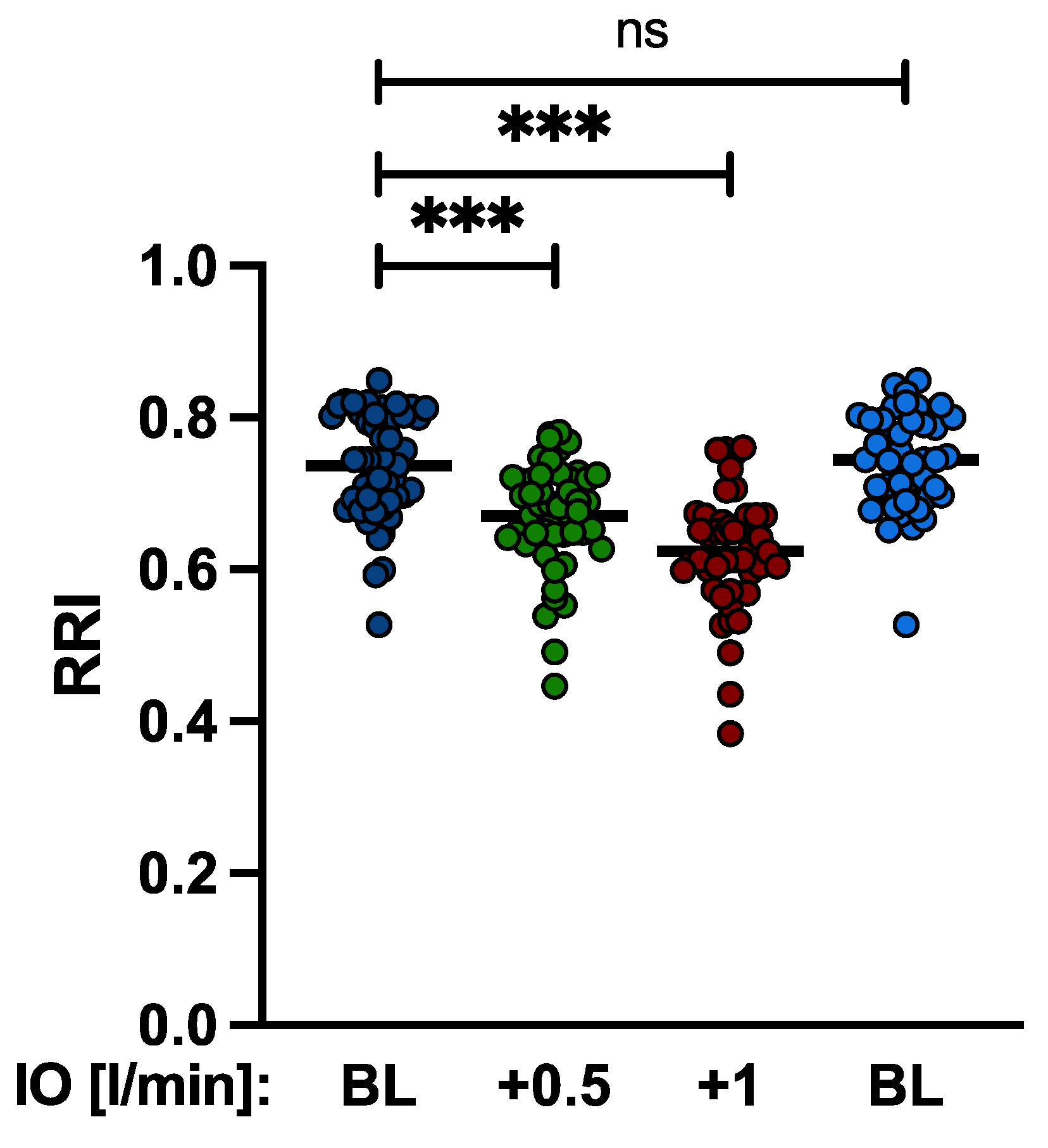
| RRI | 0.736 ± 0.07 | 0.67 ± 0.07 | 0.62 ± 0.077 | 0.74 ± 0.06 |
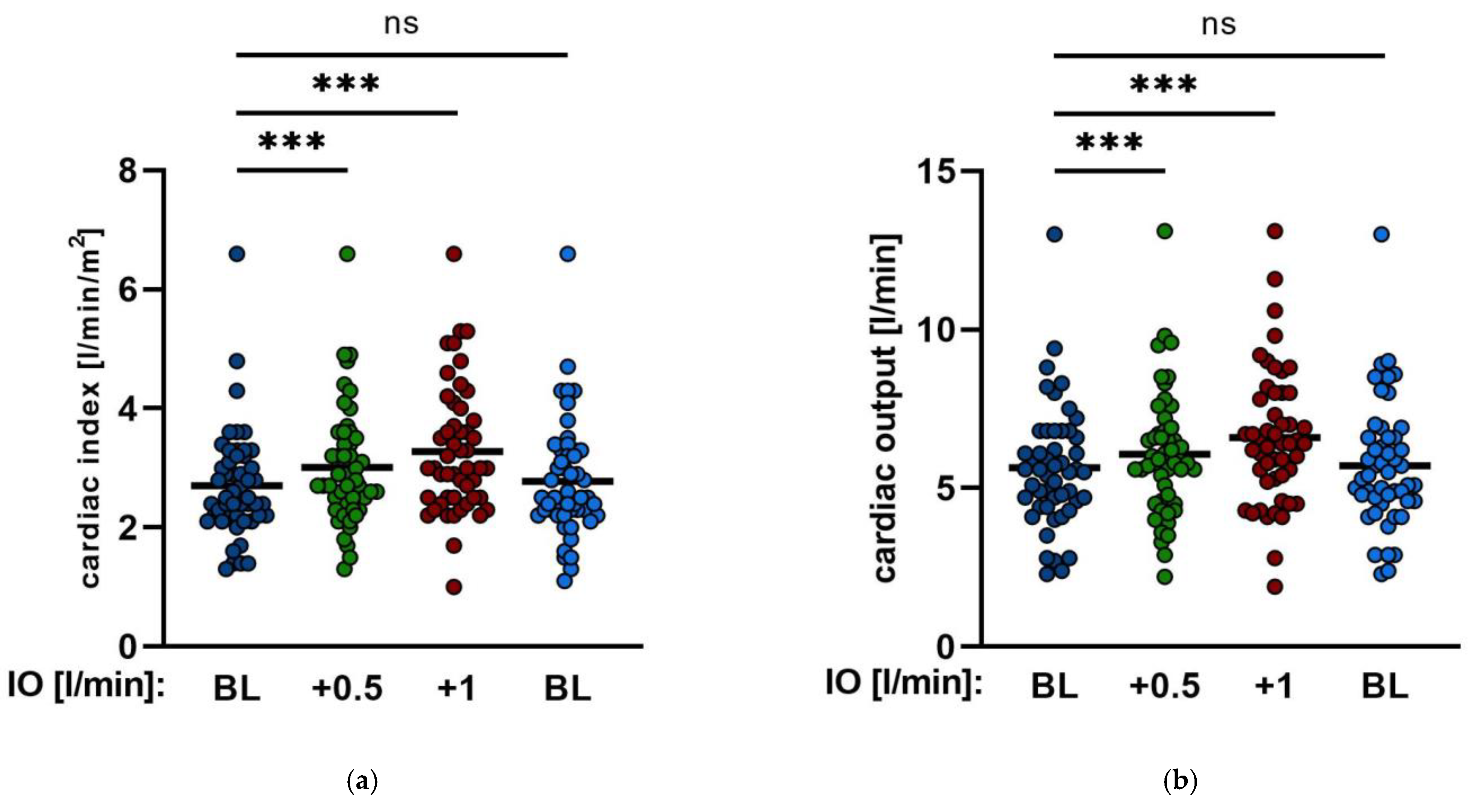
| CI | 2.7 ± 0.86 | 3.0 ± 0.98 | 3.3 ± 1.1 | 2.8 ± 0.98 |
| CO (L/min) | 5.6 ± 1.9 | 6.1 ± 2 | 6.6 ± 2.1 | 5.3 ± 2.2 |
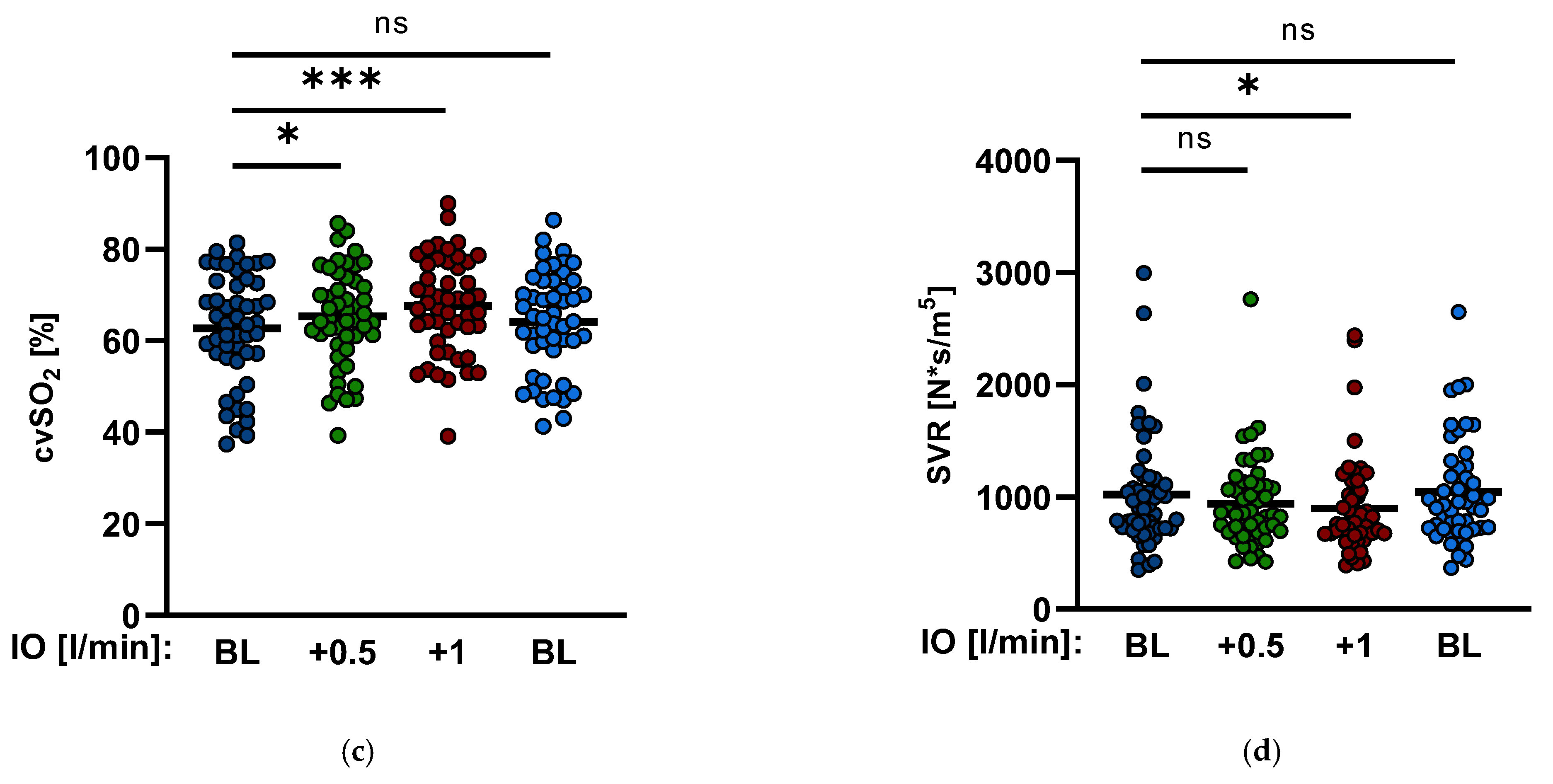
| SVR (s·cm−5) | 1035 ± 514 | 966 ± 392 | 902 ± 371 | 1055 ± 453 |
| cvsO2 (%) | 62.6 ± 11.8 | 65.1 ± 10.6 | 67.4 ± 10.5 | 64 ± 11 |
| RRI | ≥0.8 (n = 14) | <0.8 (n = 36) |
|---|---|---|
| baseline | 0.815 ± 0.12 | 0.707 ± 0.06 |
| +0.5 L/min | 0.722 ± 0.056 | 0.648 ± 0.065 |
| +1 L/min | 0.669 ± 0.075 | 0.614 ± 0.076 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patsalis, N.; Kreutz, J.; Chatzis, G.; Syntila, S.; Griewing, S.; Pirlet-Grant, C.; Schlegel, M.; Schieffer, B.; Markus, B. Renal Protection and Hemodynamic Improvement by Impella® Microaxial Pump in Patients with Cardiogenic Shock. J. Clin. Med. 2022, 11, 6817. https://doi.org/10.3390/jcm11226817
Patsalis N, Kreutz J, Chatzis G, Syntila S, Griewing S, Pirlet-Grant C, Schlegel M, Schieffer B, Markus B. Renal Protection and Hemodynamic Improvement by Impella® Microaxial Pump in Patients with Cardiogenic Shock. Journal of Clinical Medicine. 2022; 11(22):6817. https://doi.org/10.3390/jcm11226817
Chicago/Turabian StylePatsalis, Nikolaos, Julian Kreutz, Georgios Chatzis, Styliani Syntila, Sebastian Griewing, Carly Pirlet-Grant, Malte Schlegel, Bernhard Schieffer, and Birgit Markus. 2022. "Renal Protection and Hemodynamic Improvement by Impella® Microaxial Pump in Patients with Cardiogenic Shock" Journal of Clinical Medicine 11, no. 22: 6817. https://doi.org/10.3390/jcm11226817
APA StylePatsalis, N., Kreutz, J., Chatzis, G., Syntila, S., Griewing, S., Pirlet-Grant, C., Schlegel, M., Schieffer, B., & Markus, B. (2022). Renal Protection and Hemodynamic Improvement by Impella® Microaxial Pump in Patients with Cardiogenic Shock. Journal of Clinical Medicine, 11(22), 6817. https://doi.org/10.3390/jcm11226817





