e-Estesia: A Serious Game for Reducing Arousal, Improving Emotional Regulation and Increasing Wellbeing in Individuals with Gambling Disorder
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
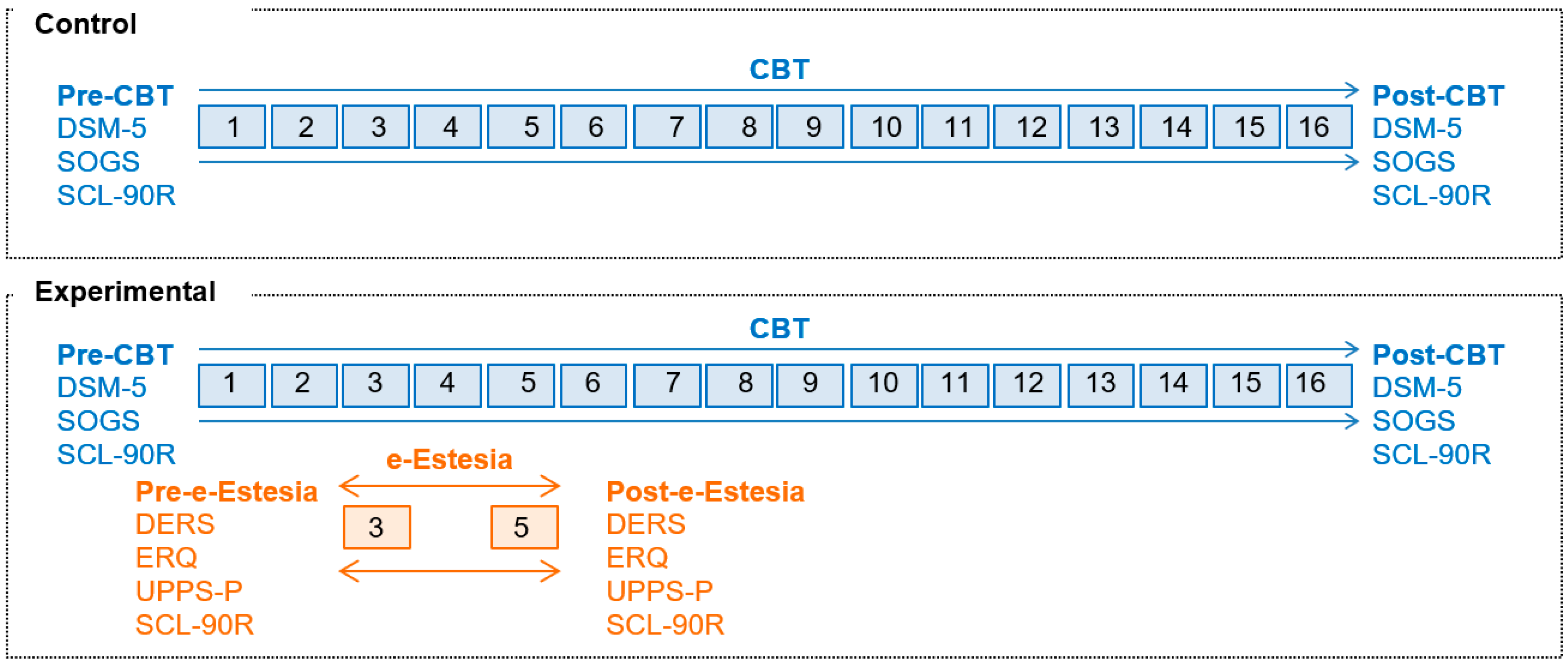
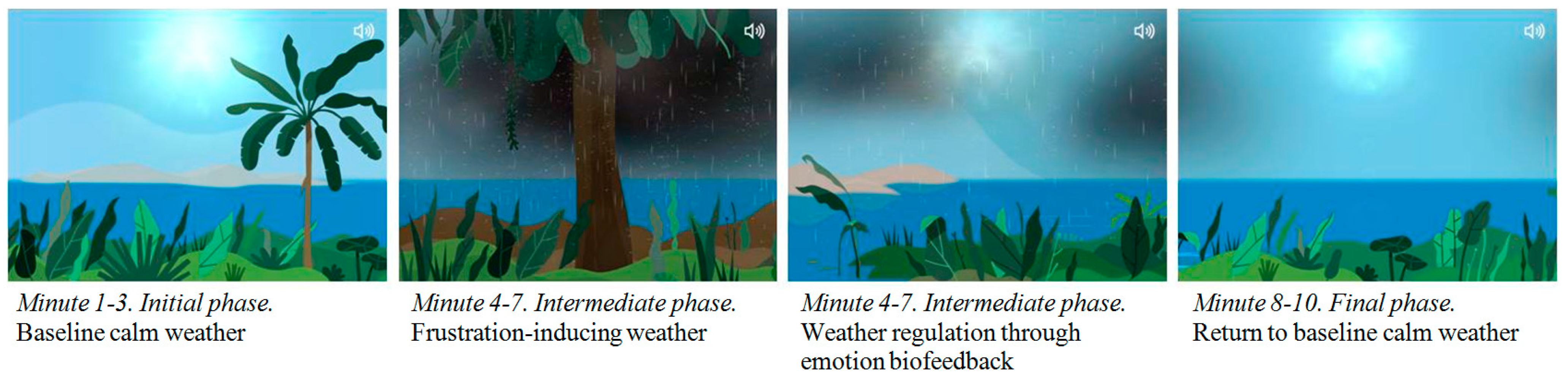
2.2. Procedure
2.3. Measures
2.3.1. Diagnostic Questionnaire for Pathological Gambling (According to the Diagnostic and Statistical Manual of Mental Disorders [DSM] Criteria) [89]
2.3.2. South Oaks Gambling Severity Screen (SOGS) [92]
2.3.3. Symptom Checklist-Revised (SCL-90-R) [94]
2.3.4. Difficulties in Emotion Regulation Scale (DERS; [22])
2.3.5. Emotion Regulation Questionnaire, Spanish Version (ERQ; [97])
2.3.6. Impulsive Behavior Scale (UPPS-P)
2.3.7. Measure of Dropout, Relapses and Compliance
2.3.8. Sociodemographic and Clinical Variables
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Sample
3.2. Analysis of the Pre-Post Changes after the Use of the e-Estesia (Experimental Group, n = 40)
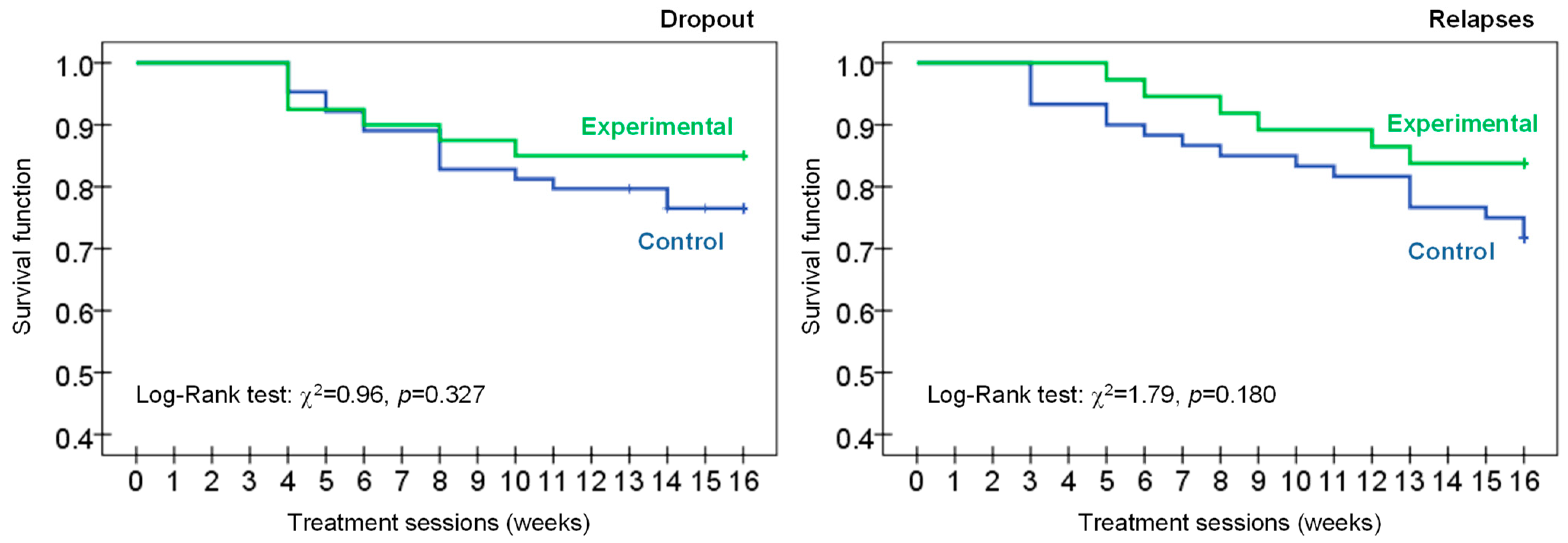
3.3. Analysis of the CBT Outcomes
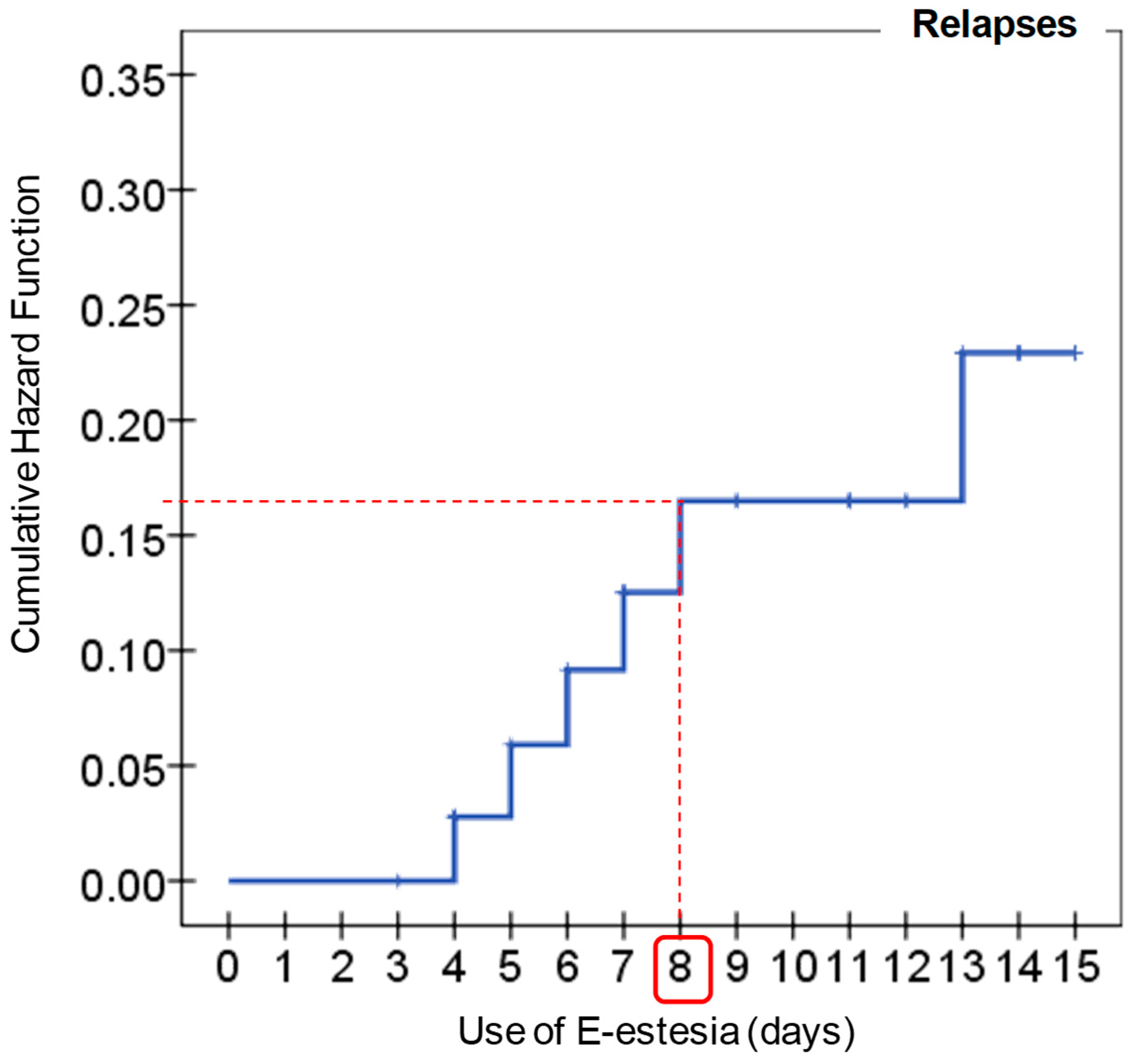
3.4. ROC Study for the Use of the e-Estesia
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Calado, F.; Griffiths, M.D. Problem Gambling Worldwide: An Update and Systematic Review of Empirical Research (2000–2015). J. Behav. Addict. 2016, 5, 592–613. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.D.; Grisham, J.R.; Erskine, A.; Cassedy, E. Deficits in Emotion Regulation Associated with Pathological Gambling. Br. J. Clin. Psychol. 2012, 51, 223–238. [Google Scholar] [CrossRef] [PubMed]
- Rogier, G.; Velotti, P. Narcissistic Implications in Gambling Disorder: The Mediating Role of Emotion Dysregulation. J. Gambl. Stud. 2018, 34, 1241–1260. [Google Scholar] [CrossRef]
- Marchica, L.A.; Keough, M.T.; Montreuil, T.C.; Derevensky, J.L. Emotion Regulation Interacts with Gambling Motives to Predict Problem Gambling among Emerging Adults. Addict. Behav. 2020, 106, 106378. [Google Scholar] [CrossRef] [PubMed]
- Elmas, H.G.; Cesur, G.; Oral, E.T. Alexithymia and Pathological Gambling: The Mediating Role of Difficulties in Emotion Regulation. Turk Psikiyatr. Derg. 2017, 28, 1–7. [Google Scholar] [CrossRef]
- Álvarez-Moya, E.M.; Jiménez-Murcia, S.; Granero, R.; Vallejo, J.; Krug, I.; Bulik, C.M.; Fernández-Aranda, F. Comparison of Personality Risk Factors in Bulimia Nervosa and Pathological Gambling. Compr. Psychiatry 2007, 48, 452–457. [Google Scholar] [CrossRef] [PubMed]
- MacLaren, V.V.; Fugelsang, J.A.; Harrigan, K.A.; Dixon, M.J. The Personality of Pathological Gamblers: A Meta-Analysis. Clin. Psychol. Rev. 2011, 31, 1057–1067. [Google Scholar] [CrossRef]
- Black, D.W.; Coryell, W.H.; Crowe, R.R.; Shaw, M.; McCormick, B.; Allen, J. Personality Disorders, Impulsiveness, and Novelty Seeking in Persons with DSM-IV Pathological Gambling and Their First-Degree Relatives. J. Gambl. Stud. 2014, 31, 1201–1214. [Google Scholar] [CrossRef]
- Kräplin, A.; Bühringer, G.; Oosterlaan, J.; Van den Brink, W.; Goschke, T.; Goudriaan, A.E. Dimensions and Disorder Specificity of Impulsivity in Pathological Gambling. Addict. Behav. 2014, 39, 1646–1651. [Google Scholar] [CrossRef]
- Del Prete, F.; Steward, T.; Navas, J.F.; Fernández-Aranda, F.; Jiménez-Murcia, S.; Oei, T.P.S.; Perales, J.C. The Role of Affect-Driven Impulsivity in Gambling Cognitions: A Convenience-Sample Study with a Spanish Version of the Gambling-Related Cognitions Scale. J. Behav. Addict. 2017, 6, 51–63. [Google Scholar] [CrossRef]
- Blaszczynski, A.; Nower, L. A Pathways Model of Problem and Pathological Gambling. Addiction 2002, 97, 487–499. [Google Scholar] [CrossRef] [PubMed]
- Johansson, A.; Grant, J.E.; Kim, S.W.; Odlaug, B.L.; Götestam, K.G. Risk Factors for Problematic Gambling: A Critical Literature Review. J. Gambl. Stud. 2009, 25, 67–92. [Google Scholar] [CrossRef] [PubMed]
- Álvarez-Moya, E.M.; Ochoa, C.; Jiménez-Murcia, S.; Aymamí, M.N.; Gómez-Peña, M.; Fernández-Aranda, F.; Santamaría, J.; Moragas, L.; Bove, F.; Menchón, J.M. Effect of Executive Functioning, Decision-Making and Self-Reported Impulsivity on the Treatment Outcome of Pathologic Gambling. J. Psychiatry Neurosci. 2011, 36, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, L.R.N.; Grant, J.E.; Odlaug, B.L. Emotion Regulation and Impulsivity in Young Adults. J. Psychiatr. Res. 2012, 46, 651–658. [Google Scholar] [CrossRef]
- Mestre-Bach, G.; Steward, T.; Granero, R.; Fernández-Aranda, F.; Mena-Moreno, T.; Vintró-Alcaraz, C.; Lozano-Madrid, M.; Menchón, J.M.; Potenza, M.N.; Jiménez-Murcia, S. Dimensions of Impulsivity in Gambling Disorder. Sci. Rep. 2020, 10, 397. [Google Scholar] [CrossRef]
- Kovács, I.; Demeter, I.; Janka, Z.; Demetrovics, Z.; Maraz, A.; Andó, B. Different Aspects of Impulsivity in Chronic Alcohol Use Disorder with and without Comorbid Problem Gambling. PLoS ONE 2020, 15, e0227645. [Google Scholar] [CrossRef]
- Limbrick-Oldfield, E.H.; Mick, I.; Cocks, R.E.; Flechais, R.S.A.; Turton, S.; Lingford-Hughes, A.; Bowden-Jones, H.; Clark, L. Neural and Neurocognitive Markers of Vulnerability to Gambling Disorder: A Study of Unaffected Siblings. Neuropsychopharmacology 2020, 45, 292–300. [Google Scholar] [CrossRef]
- Ioannidis, K.; Hook, R.; Wickham, K.; Grant, J.E.; Chamberlain, S.R. Impulsivity in Gambling Disorder and Problem Gambling: A Meta-Analysis. Neuropsychopharmacology 2019, 44, 1354–1361. [Google Scholar] [CrossRef]
- Lynam, D.R.; Smith, G.T.; Whiteside, S.P.; Cyders, M.A. The UPPS–P: Assessing Five Personality Pathways to Impulsive Behavior; Purdue University: West Lafayette, IN, USA, 2006. [Google Scholar]
- Cyders, M.A. Impulsivity and the Sexes: Measurement and Structural Invariance of the UPPS-P Impulsive Behavior Scale. Assessment 2013, 20, 86–97. [Google Scholar] [CrossRef]
- Whiteside, S.P.; Lynam, D.R.; Miller, J.D.; Reynolds, S.K. Validation of the UPPS Impulsive Behaviour Scale: A Four-factor Model of Impulsivity. Eur. J. Pers. 2005, 19, 559–574. [Google Scholar] [CrossRef]
- Gratz, K.L.; Roemer, L. Multidimensional Assessment of Emotion Regulation and Dysregulation: Development, Factor Structure, and Initial Validation of the Difficulties in Emotion Regulation Scale. J. Psychopathol. Behav. Assess. 2004, 26, 41–54. [Google Scholar] [CrossRef]
- Aldao, A.; Nolen-Hoeksema, S.; Schweizer, S. Emotion-Regulation Strategies across Psychopathology: A Meta-Analytic Review. Clin. Psychol. Rev. 2010, 30, 217–237. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, L.S.; Elliott, R.; Pos, A. Special Topic: Emotion-Focused Therapy. Eur. Psychother. 2007, 7, 87–93. [Google Scholar]
- Gross, J.J.; Thompson, R.A. Emotion Regulation: Conceptual Foundations. In Handbook of Emotion Regulation; Gross, J.J., Ed.; Guilford Press: New York, NY, USA, 2007; pp. 3–24. [Google Scholar]
- Mennin, D.S.; Holaway, R.M.; Fresco, D.M.; Moore, M.T.; Heimberg, R.G. Delineating Components of Emotion and Its Dysregulation in Anxiety and Mood Psychopathology. Behav. Ther. 2007, 38, 284–302. [Google Scholar] [CrossRef]
- John, O.P.; Gross, J.J. Healthy and Unhealthy Emotion Regulation: Personality Processes, Individual Differences, and Life Span Development. J. Pers. 2004, 72, 1301–1334. [Google Scholar] [CrossRef] [PubMed]
- Shead, N.W.; Hodgins, D.C. Affect-Regulation Expectancies among Gamblers. J. Gambl. Stud. 2009, 25, 357–375. [Google Scholar] [CrossRef]
- Lloyd, J.; Doll, H.; Hawton, K.; Dutton, W.H.; Geddes, J.R.; Goodwin, G.M.; Rogers, R.D. How Psychological Symptoms Relate to Different Motivations for Gambling: An Online Study of Internet Gamblers. Biol. Psychiatry 2010, 68, 733–740. [Google Scholar] [CrossRef]
- Tice, D.M.; Bratslavsky, E. Giving in to Feel Good: The Place of Emotion Regulation in the Context of General Self-Control. Psychol. Inq. 2000, 11, 149–159. [Google Scholar] [CrossRef]
- Ruiz de Lara, C.M.; Navas, J.F.; Perales, J.C. The Paradoxical Relationship between Emotion Regulation and Gambling-Related Cognitive Biases. PLoS ONE 2019, 14, e0220668. [Google Scholar] [CrossRef]
- Mallorquí-Bagué, N.; Mena-Moreno, T.; Granero, R.; Vintró-Alcaraz, C.; Sánchez-González, J.; Fernández-Aranda, F.; Pino-Gutiérrez, A.D.; Mestre-Bach, G.; Aymamí, N.; Gómez-Peña, M.; et al. Suicidal Ideation and History of Suicide Attempts in Treatment-Seeking Patients with Gambling Disorder: The Role of Emotion Dysregulation and High Trait Impulsivity. J. Behav. Addict. 2018, 7, 1112–1121. [Google Scholar] [CrossRef]
- Grant, K.E.; Compas, B.E.; Stuhlmacher, A.F.; Thurm, A.E.; McMahon, S.D.; Halpert, J.A. Stressors and Child and Adolescent Psychopathology: Moving from Markers to Mechanisms of Risk. Psychol. Bull. 2003, 129, 447–466. [Google Scholar] [CrossRef] [PubMed]
- Kopp, M.S.; Réthelyi, J. Where Psychology Meets Physiology: Chronic Stress and Premature Mortality—The Central-Eastern European Health Paradox. Brain Res. Bull. 2004, 62, 351–367. [Google Scholar] [CrossRef] [PubMed]
- Joëls, M.; Baram, T.Z. The Neuro-Symphony of Stress. Nat. Rev. Neurosci. 2009, 10, 459–466. [Google Scholar] [CrossRef]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef]
- Appelhans, B.M.; Luecken, L.J. Heart Rate Variability as an Index of Regulated Emotional Responding. Rev. Gen. Psychol. 2006, 10, 229–240. [Google Scholar] [CrossRef]
- Balzarotti, S.; Biassoni, F.; Colombo, B.; Ciceri, M.R. Cardiac Vagal Control as a Marker of Emotion Regulation in Healthy Adults: A Review. Biol. Psychol. 2017, 130, 54–66. [Google Scholar] [CrossRef] [PubMed]
- Edmonds, W.A.; Kennedy, T.D.; Hughes, P.A.; Calzada, P.J. A Single-Participants Investigation of the Effects of Various Biofeedback-Assisted Breathing Patterns on Heart Rate Variability: A Practitioner’s Approach. Biofeedback 2009, 37, 141–146. [Google Scholar] [CrossRef]
- Lin, I.M.; Tai, L.Y.; Fan, S.Y. Breathing at a Rate of 5.5 Breaths per Minute with Equal Inhalation-to-Exhalation Ratio Increases Heart Rate Variability. Int. J. Psychophysiol. 2014, 91, 206–211. [Google Scholar] [CrossRef]
- Park, Y.J.; Park, Y.B. Clinical Utility of Paced Breathing as a Concentration Meditation Practice. Complement. Ther. Med. 2012, 20, 393–399. [Google Scholar] [CrossRef]
- Van Diest, I.; Verstappen, K.; Aubert, A.E.; Widjaja, D.; Vansteenwegen, D.; Vlemincx, E. Inhalation/Exhalation Ratio Modulates the Effect of Slow Breathing on Heart Rate Variability and Relaxation. Appl. Psychophysiol. Biofeedback 2014, 39, 171–180. [Google Scholar] [CrossRef]
- Jerath, R.; Crawford, M.W.; Barnes, V.; Harden, K. Self-Regulation of Breathing as a Primary Treatment for Anxiety. Appl. Psychophysiol. Biofeedback 2015, 40, 107–115. [Google Scholar] [CrossRef]
- Stancák, A.; Pfeffer, D.; Hrudová, L.; Sovka, P.; Dostálek, C. Electroencephalographic Correlates of Paced Breathing. Neuroreport 1993, 4, 723–726. [Google Scholar] [CrossRef] [PubMed]
- Homma, I.; Masaoka, Y. Breathing Rhythms and Emotions. Exp. Physiol. 2008, 93, 1011–1021. [Google Scholar] [CrossRef] [PubMed]
- Lehrer, P.M.; Vaschillo, E.; Vaschillo, B.; Lu, S.-E.; Eckberg, D.L.; Edelberg, R.; Shih, W.J.; Lin, Y.; Kuusela, T.A.; Tahvanainen, K.U.O.; et al. Heart Rate Variability Biofeedback Increases Baroreflex Gain and Peak Expiratory Flow. Psychosom. Med. 2003, 65, 796–805. [Google Scholar] [CrossRef] [PubMed]
- Gross, M.J.; Shearer, D.A.; Bringer, J.D.; Hall, R.; Cook, C.J.; Kilduff, L.P. Abbreviated Resonant Frequency Training to Augment Heart Rate Variability and Enhance On-Demand Emotional Regulation in Elite Sport Support Staff. Appl. Psychophysiol. Biofeedback 2016, 41, 263–274. [Google Scholar] [CrossRef]
- Gruzelier, J.H.; Thompson, T.; Redding, E.; Brandt, R.; Steffert, T. Application of Alpha/Theta Neurofeedback and Heart Rate Variability Training to Young Contemporary Dancers: State Anxiety and Creativity. Int. J. Psychophysiol. 2014, 93, 105–111. [Google Scholar] [CrossRef]
- Chittaro, L.; Sioni, R. Evaluating Mobile Apps for Breathing Training: The Effectiveness of Visualization. Comput. Hum. Behav. 2014, 40, 56–63. [Google Scholar] [CrossRef]
- Patibanda, R.; Mueller, F.; Leskovsek, M.; Duckworth, J. Life Tree: Understanding the Design of Breathing Exercise Games. In Proceedings of the CHI PLAY 2017—Proceedings of the Annual Symposium on Computer-Human Interaction in Play, Amsterdam, The Netherlands, 15 October 2017; Association for Computing Machinery, Inc.: New York, NY, USA, 2017; pp. 19–31. [Google Scholar]
- Carlier, S.; Van Der Paelt, S.; Ongenae, F.; De Backere, F.; De Turck, F. Using a Serious Game to Reduce Stress and Anxiety in Children with Autism Spectrum Disorder. In Proceedings of the ACM International Conference Proceeding Series, Daejeon, Republic of Korea, 10–13 November 2019; Association for Computing Machinery: New York, NY, USA, 2019; pp. 452–461. [Google Scholar]
- Hunter, J.F.; Olah, M.S.; Williams, A.L.; Parks, A.C.; Pressman, S.D. Effect of Brief Biofeedback via a Smartphone App on Stress Recovery: Randomized Experimental Study. JMIR Serious Games 2019, 7, e15974. [Google Scholar] [CrossRef]
- Roo, J.S.; Gervais, R.; Frey, J.; Hachet, M. Inner Garden: Connecting Inner States to a Mixed Reality Sandbox for Mindfulness. In Proceedings of the Conference on Human Factors in Computing Systems, Denver, CO, USA, 6–11 May 2017; Association for Computing Machinery: New York, NY, USA, 2017; Volume 2017-May, pp. 1459–1470. [Google Scholar]
- Russell, M.E.B.; Scott, A.B.; Boggero, I.A.; Carlson, C.R. Inclusion of a Rest Period in Diaphragmatic Breathing Increases High Frequency Heart Rate Variability: Implications for Behavioral Therapy. Psychophysiology 2017, 54, 358–365. [Google Scholar] [CrossRef]
- Delk, K.K.; Gevirtz, R.; Hicks, D.A.; Carden, F.; Rucker, R. The Effects of Biofeedback Assisted Breathing Retraining on Lung Functions in Patients with Cystic Fibrosis. Chest 1994, 105, 23–28. [Google Scholar] [CrossRef][Green Version]
- Barnes, S.; Prescott, J. Empirical Evidence for the Outcomes of Therapeutic Video Games for Adolescents with Anxiety Disorders: Systematic Review. JMIR Serious Games 2018, 6, e3. [Google Scholar] [CrossRef]
- Charlier, N.; Zupancic, N.; Fieuws, S.; Denhaerynck, K.; Zaman, B.; Moons, P. Serious Games for Improving Knowledge and Self-Management in Young People with Chronic Conditions: A Systematic Review and Meta-Analysis. J. Am. Med. Informatics Assoc. 2016, 23, 230–239. [Google Scholar] [CrossRef]
- Tárrega, S.; Castro-Carreras, L.; Fernández-Aranda, F.; Granero, R.; Giner-Bartolomé, C.; Aymamí, N.; Gómez-Peña, M.; Santamaría, J.J.; Forcano, L.; Steward, T.; et al. A Serious Videogame as an Additional Therapy Tool for Training Emotional Regulation and Impulsivity Control in Severe Gambling Disorder. Front. Psychol. 2015, 6, 1721. [Google Scholar] [CrossRef] [PubMed]
- Ducharme, P.; Wharff, E.; Hutchinson, E.; Kahn, J.; Logan, G.; Gonzalez-Heydrich, J. Videogame Assisted Emotional Regulation Training: An ACT with RAGE-Control Case Illustration. Clin. Soc. Work J. 2012, 40, 75–84. [Google Scholar] [CrossRef]
- Fagundo, A.B.; Via, E.; Sánchez, I.; Jiménez-Murcia, S.; Forcano, L.; Soriano-Mas, C.; Giner-Bartolomé, C.; Santamaría, J.J.; Ben-Moussa, M.; Konstantas, D.; et al. Physiological and Brain Activity after a Combined Cognitive Behavioral Treatment plus Video Game Therapy for Emotional Regulation in Bulimia Nervosa: A Case Report. J. Med. Internet Res. 2014, 16, e183. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Aranda, F.; Jimenez-Murcia, S.; Santamaría, J.J.; Giner-Bartolomé, C.; Mestre-Bach, G.; Granero, R.; Sánchez, I.; Agüera, Z.; Moussa, M.H.; Magnenat-Thalmann, N.; et al. The Use of Videogames as Complementary Therapeutic Tool for Cognitive Behavioral Therapy in Bulimia Nervosa Patients. Cyberpsychology, Behav. Soc. Netw. 2015, 18, 744–751. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Aranda, F.; Jiménez-Murcia, S.; Santamaría, J.J.; Gunnard, K.; Soto, A.; Kalapanidas, E.; Bults, R.G.A.; Davarakis, C.; Ganchev, T.; Granero, R.; et al. Video Games as a Complementary Therapy Tool in Mental Disorders: PlayMancer, a European Multicentre Study. J. Ment. Health 2012, 21, 364–374. [Google Scholar] [CrossRef]
- Jander, A.; Crutzen, R.; Mercken, L.; Candel, M.; De Vries, H. Effects of a Web-Based Computer-Tailored Game to Reduce Binge Drinking among Dutch Adolescents: A Cluster Randomized Controlled Trial. J. Med. Internet Res. 2016, 18, e4708. [Google Scholar] [CrossRef]
- Jiménez-Murcia, S.; Fernández-Aranda, F.; Kalapanidas, E.; Konstantas, D.; Ganchev, T.; Kocsis, O.; Lam, T.; Santamaría, J.J.; Raguin, T.; Breiteneder, C.; et al. Playmancer Project: A Serious Videogame as an Additional Therapy Tool for Eating and Impulse Control Disorders. Annu. Rev. CyberTherapy Telemed. 2009, 7, 163–166. [Google Scholar] [CrossRef]
- Kato, P.M. Video Games in Health Care: Closing the Gap. Rev. Gen. Psychol. 2010, 14, 113–121. [Google Scholar] [CrossRef]
- Lau, H.M.; Smit, J.H.; Fleming, T.M.; Riper, H. Serious Games for Mental Health: Are They Accessible, Feasible, and Effective? A Systematic Review and Meta-Analysis. Front. Psychiatry 2017, 7, 209. [Google Scholar] [CrossRef] [PubMed]
- Eichenberg, C.; Schott, M. Serious Games for Psychotherapy: A Systematic Review. Games Health J. 2017, 6, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Potenza, M.N.; Balodis, I.M.; Derevensky, J.; Grant, J.E.; Petry, N.M.; Verdejo-Garcia, A.; Yip, S.W. Gambling Disorder. Nat. Rev. Dis. Prim. 2019, 5, 51. [Google Scholar] [CrossRef]
- Yakovenko, I.; Hodgins, D.C. Latest Developments in Treatment for Disordered Gambling: Review and Critical Evaluation of Outcome Studies. Curr. Addict. Rep. 2016, 3, 299–306. [Google Scholar] [CrossRef]
- Cowlishaw, S.; Merkouris, S.; Dowling, N.; Anderson, C.; Jackson, A.; Thomas, S. Psychological Therapies for Pathological and Problem Gambling. Cochrane Database Syst. Rev. 2012, 11, CD008937. [Google Scholar] [CrossRef]
- Di Nicola, M.; De Crescenzo, F.; D’Alò, G.L.; Remondi, C.; Panaccione, I.; Moccia, L.; Molinaro, M.; Dattoli, L.; Lauriola, A.; Martinelli, S.; et al. Pharmacological and Psychosocial Treatment of Adults with Gambling Disorder: A Meta-Review. J. Addict. Med. 2020, 14, e15–e23. [Google Scholar] [CrossRef]
- Rash, C.J.; Petry, N.M. Psychological Treatments for Gambling Disorder. Psychol. Res. Behav. Manag. 2014, 7, 285–295. [Google Scholar] [CrossRef] [PubMed]
- Chrétien, M.; Giroux, I.; Goulet, A.; Jacques, C.; Bouchard, S. Cognitive Restructuring of Gambling-Related Thoughts: A Systematic Review. Addict. Behav. 2017, 75, 108–121. [Google Scholar] [CrossRef]
- Tolchard, B. Cognitive-Behavior Therapy for Problem Gambling: A Critique of Current Treatments and Proposed New Unified Approach. J. Ment. Health 2017, 26, 283–290. [Google Scholar] [CrossRef]
- Menchon, J.M.; Mestre-Bach, G.; Steward, T.; Fernández-Aranda, F.; Jiménez-Murcia, S. An Overview of Gambling Disorder: From Treatment Approaches to Risk Factors. F1000Research 2018, 7, 434. [Google Scholar] [CrossRef]
- Pallesen, S.; Molde, H.; Arnestad, H.M.; Laberg, J.C.; Skutle, A.; Iversen, E.; Støylen, I.J.; Kvale, G.; Holsten, F. Outcome of Pharmacological Treatments of Pathological Gambling: A Review and Meta-Analysis. J. Clin. Psychopharmacol. 2007, 27, 357–364. [Google Scholar] [CrossRef]
- Petry, N.M.; Ginley, M.K.; Rash, C.J. A Systematic Review of Treatments for Problem Gambling. Psychol. Addict. Behav. 2017, 31, 951–961. [Google Scholar] [CrossRef] [PubMed]
- Aragay, N.; Jiménez-Murcia, S.; Granero, R.; Fernández-Aranda, F.; Ramos-Grille, I.; Cardona, S.; Garrido, G.; Anisul Islam, M.; Menchón, J.M.; Vallès, V. Pathological Gambling: Understanding Relapses and Dropouts. Compr. Psychiatry 2015, 57, 58–64. [Google Scholar] [CrossRef]
- Melville, K.M.; Casey, L.M.; Kavanagh, D.J. Psychological Treatment Dropout among Pathological Gamblers. Clin. Psychol. Rev. 2007, 27, 944–958. [Google Scholar] [CrossRef][Green Version]
- Pfund, R.A.; Peter, S.C.; Whelan, J.P.; Meyers, A.W. When Does Premature Treatment Termination Occur? Examining Session-by-Session Dropout among Clients with Gambling Disorder. J. Gambl. Stud. 2018, 34, 617–630. [Google Scholar] [CrossRef]
- Pfund, R.A.; Peter, S.C.; Whelan, J.P.; Meyers, A.W.; Ginley, M.K.; Relyea, G. Is More Better? A Meta-Analysis of Dose and Efficacy in Face-to-Face Psychological Treatments for Problem and Disordered Gambling. Psychol. Addict. Behav. 2020, 34, 557–568. [Google Scholar] [CrossRef]
- Swift, J.K.; Callahan, J.; Levine, J.C. Using Clinically Significant Change to Identify Premature Termination. Psychotherapy 2009, 46, 328–335. [Google Scholar] [CrossRef] [PubMed]
- Giordano, R.; Donati, M.A.; Zamboni, L.; Fusina, F.; Primi, C.; Lugoboni, F. Alter Game: A Study Protocol on a Virtual “Serious Game” for Relapse Prevention in Patients with Gambling Disorder. Front. Psychiatry 2022, 13, 854088. [Google Scholar] [CrossRef]
- Yáñez-Gómez, R.; Cascado-Caballero, D.; Sevillano, J.L. Academic Methods for Usability Evaluation of Serious Games: A Systematic Review. Multimed. Tools Appl. 2017, 76, 5755–5784. [Google Scholar] [CrossRef]
- Zyda, M. From Visual Simulation to Virtual Reality to Games. Comput. Long Beach Calif. 2005, 38, 25–32. [Google Scholar] [CrossRef]
- Fleming, T.M.; Bavin, L.; Stasiak, K.; Hermansson-Webb, E.; Merry, S.N.; Cheek, C.; Lucassen, M.; Lau, H.M.; Pollmuller, B.; Hetrick, S. Serious Games and Gamification for Mental Health: Current Status and Promising Directions. Front. Psychiatry 2017, 7, 215. [Google Scholar] [CrossRef] [PubMed]
- Clarke, D. Intrinsic and Extrinsic Barriers to Health Care: Implications for Problem Gambling. Int. J. Ment. Health Addict. 2007, 5, 279–291. [Google Scholar] [CrossRef]
- Rodriguez, A.; Rey, B.; Vara, M.D.; Wrzesien, M.; Alcaniz, M.; Banos, R.M.; Perez-Lopez, D. A VR-Based Serious Game for Studying Emotional Regulation in Adolescents. IEEE Comput. Graph. Appl. 2015, 35, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Stinchfield, R. Reliability, Validity, and Classification Accuracy of a Measure of DSM-IV Diagnostic Criteria for Pathological Gambling. Am. J. Psychiatry 2003, 160, 180–182. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013; ISBN 0890425558. [Google Scholar]
- Jiménez-Murcia, S.; Stinchfield, R.; ÁLvarez-Moya, E.; Jaurrieta, N.; Bueno, B.; Granero, R.; Aymamí, M.N.; Gómez-Peña, M.; Martínez-Giménez, R.; Fernández-Aranda, F.; et al. Reliability, Validity, and Classification Accuracy of a Spanish Translation of a Measure of DSM-IV Diagnostic Criteria for Pathological Gambling. J. Gambl. Stud. 2009, 25, 93–104. [Google Scholar] [CrossRef]
- Lesieur, H.R.; Blume, S.B. The South Oaks Gambling Screen (SOGS): A New Instrument for the Identification of Pathological Gamblers. Am. J. Psychiatry 1987, 144, 1184–1188. [Google Scholar] [CrossRef]
- Echeburúa, E.; Báez, C.; Fernández-Montalvo, J.; Páez, D. Cuestionario de Juego Patológico de South Oaks (SOGS): Validación Española. Análisis Y Modif. Conduct. 1994, 20, 769–791. [Google Scholar]
- Derogatis, L.R. SCL-90-R. Cuestionario de 90 Síntomas; Ediciones, T., Ed.; SAGE Publications Inc.: Madrid, Spain, 1997. [Google Scholar]
- Gonzalez De Rivera, J.L.; Derogatis, L.R.; De las Cuevas, C.; Gracia Marco, R.; Rodríguez-Pulido, F.; Henry-Benitez, M.; Monterrey, A. The Spanish Version of the SCL-90-R. Normative Data in the General Population. Towson Clin. Psychom. Res. 1989, 43–67. [Google Scholar]
- Hervás, G.; Jódar, R. Adaptación Al Castellano de La Escala de Dificultades En La Regulación Emocional the Spanish Version of the Difficulties in Emotion Regulation Scale. Clínica y Salud 2008, 19, 139–156. [Google Scholar]
- Cabello, R.; Salguero, J.M.; Fernández-Berrocal, P.; Gross, J.J. A Spanish Adaptation of the Emotion Regulation Questionnaire. Eur. J. Psychol. Assess. 2013, 29, 234–240. [Google Scholar] [CrossRef]
- Verdejo-García, A.; Lozano, O.; Moya, M.; Alcázar, M.A.; Pérez-García, M. Psychometric Properties of a Spanish Version of the UPPS-P Impulsive Behavior Scale: Reliability, Validity and Association with Trait and Cognitive Impulsivity. J. Pers. Assess. 2010, 92, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Mena-Moreno, T.; Fernández-Aranda, F.; Granero, R.; Munguía, L.; Steward, T.; López-González, H.; del Pino-Gutiérrez, A.; Lozano-Madrid, M.; Gómez-Peña, M.; Moragas, L.; et al. A Serious Game to Improve Emotion Regulation in Treatment-Seeking Individuals with Gambling Disorder: A Usability Study. Front. Psychol. 2021, 12, 621953. [Google Scholar] [CrossRef] [PubMed]
- Levine, T.R.; Hullett, C.R. Eta Squared, Partial Eta Squared, and Misreporting of Effect Size in Communication Research. Hum. Commun. Res. 2002, 28, 612–625. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 1988. [Google Scholar]
- Finner, H.; Roters, M. On the False Discovery Rate and Expected Type I Errors. Biometrical J. 2001, 43, 985–1000. [Google Scholar] [CrossRef]
- Jiménez-Murcia, S.; Álvarez-Moya, E.M.; Granero, R.; Aymami, M.N.; Gómez-Peña, M.; Jaurrieta, N.; Sans, B.; Rodriguez-Marti, J.; Vallejo, J. Cognitive-Behavioral Group Treatment for Pathological Gambling: Analysis of Effectiveness and Predictors of Therapy Outcome. Psychother. Res. 2007, 17, 544–552. [Google Scholar] [CrossRef]
- Brezinka, V. Ricky and the Spider—A Video Game to Support Cognitive Behavioural Treatment of Children with Obsessive-Compulsive Disorder. Clin. Neuropsychiatry 2013, 10, 6–12. [Google Scholar] [CrossRef]
- Fagundo, A.B.; Santamaría, J.J.; Forcano, L.; Giner-Bartolomé, C.; Jiménez-Murcia, S.; Sánchez, I.; Granero, R.; Ben-Moussa, M.; Magnenat-Thalmann, N.; Konstantas, D.; et al. Video Game Therapy for Emotional Regulation and Impulsivity Control in a Series of Treated Cases with Bulimia Nervosa. Eur. Eat. Disord. Rev. 2013, 21, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Merry, S.N.; Stasiak, K.; Shepherd, M.; Frampton, C.; Fleming, T.; Lucassen, M.F.G. The Effectiveness of SPARX, a Computerised Self Help Intervention for Adolescents Seeking Help for Depression: Randomised Controlled Non-Inferiority Trial. BMJ 2012, 344, e2598. [Google Scholar] [CrossRef]
- Santamaria, J.J. Serious Games as Additional Psychological Support: A Review of the Literature. J. CyberTherapy Rehabil. 2011, 4, 469. [Google Scholar]
- Yusof, N.; Rias, R.M.; Yusoff, E.H. Serious Games in Mental Health Treatment: Review of Literature. In Proceedings of the Knowledge Management International Conference (KMICe), Langkawi, Malaysia, 12–15 August 2014; pp. 12–15. [Google Scholar]
- Ly, K.H.; Carlbring, P.; Andersson, G. Behavioral Activation-Based Guided Self-Help Treatment Administered through a Smartphone Application: Study Protocol for a Randomized Controlled Trial. Trials 2012, 13, 62. [Google Scholar] [CrossRef]
- Malone, T.W.; Lepper, M.R. Making Learning Fun: A Taxonomy of Intrinsic Motivations for Learning. Aptit. Learn. Instr. 1987, 2, 223–253. [Google Scholar] [CrossRef]
- Alexiou, A.; Schippers, M.; Oshri, I. Positive Psychology and Digital Games: The Role of Emotions and Psychological Flow in Serious Games Development. Psychology 2012, 03, 1243–1247. [Google Scholar] [CrossRef]
- Schunk, D.H.; Pintrich, P.R.; Meece, J.L. Motivation in Education: Theory, Research, and Applications; Pearson: Saddle River, NJ, USA, 2008; ISBN 9780132281553. [Google Scholar]
- Rogier, G.; Zobel, S.B.; Velotti, P. Pathological Personality Facets and Emotion (Dys)Regulation in Gambling Disorder. Scand. J. Psychol. 2020, 61, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Del Pino-Gutiérrez, A.; Jiménez-Murcia, S.; Fernández-Aranda, F.; Agüera, Z.; Granero, R.; Hakansson, A.; Fagundo, A.B.; Bolao, F.; Valdepérez, A.; Mestre-Bach, G.; et al. The Relevance of Personality Traits in Impulsivity-Related Disorders: From Substance Use Disorders and Gambling Disorder to Bulimia Nervosa. J. Behav. Addict. 2017, 6, 396–405. [Google Scholar] [CrossRef] [PubMed]
- Krmpotich, T.; Mikulich-Gilbertson, S.; Sakai, J.; Thompson, L.; Banich, M.T.; Tanabe, J. Impaired Decision-Making, Higher Impulsivity, and Drug Severity in Substance Dependence and Pathological Gambling. J. Addict. Med. 2015, 9, 273. [Google Scholar] [CrossRef] [PubMed]
- Savvidou, L.G.; Fagundo, A.B.; Fernández-Aranda, F.; Granero, R.; Claes, L.; Mallorquí-Baqué, N.; Verdejo-García, A.; Steiger, H.; Israel, M.; Moragas, L.; et al. Is Gambling Disorder Associated with Impulsivity Traits Measured by the UPPS-P and Is This Association Moderated by Sex and Age? Compr. Psychiatry 2017, 72, 106–113. [Google Scholar] [CrossRef] [PubMed]
- Albein-Urios, N.; Martinez-González, J.M.; Lozano, O.; Verdejo-Garcia, A. Monetary Delay Discounting in Gambling and Cocaine Dependence with Personality Comorbidities. Addict. Behav. 2014, 39, 1658–1662. [Google Scholar] [CrossRef] [PubMed]
- Engel, A.; Caceda, R. Can Decision Making Research Provide a Better Understanding of Chemical and Behavioral Addictions? Curr. Drug Abuse Rev. 2015, 8, 75–85. [Google Scholar] [CrossRef]
- Farstad, S.M.; Von Ranson, K.M.; Hodgins, D.C.; El-Guebaly, N.; Casey, D.M.; Schopflocher, D.P. The Influence of Impulsiveness on Binge Eating and Problem Gambling: A Prospective Study of Gender Differences in Canadian Adults. Psychol. Addict. Behav. 2015, 29, 805–812. [Google Scholar] [CrossRef]
- Jara-Rizzo, M.F.; Navas, J.F.; Steward, T.; López-Gómez, M.; Jiménez-Murcia, S.; Fernández-Aranda, F.; Perales, J.C. Impulsivity and Problem Awareness Predict Therapy Compliance and Dropout from Treatment for Gambling Disorder. Adicciones 2019, 31, 147–159. [Google Scholar] [CrossRef]
- Mallorquí-Bagué, N.; Vintró-Alcaraz, C.; Verdejo-García, A.; Granero, R.; Fernández-Aranda, F.; Magaña, P.; Mena-Moreno, T.; Aymamí, N.; Gómez-Peña, M.; del Pino-Gutiérrez, A.; et al. Impulsivity and Cognitive Distortions in Different Clinical Phenotypes of Gambling Disorder: Profiles and Longitudinal Prediction of Treatment Outcomes. Eur. Psychiatry 2019, 61, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Leblond, J.; Ladouceur, R.; Blaszczynski, A. Which Pathological Gamblers Will Complete Treatment? Br. J. Clin. Psychol. 2003, 42, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Knezevic-Budisin, B.; Pedden, V.; White, A.; Miller, C.J.; Hoaken, P.N.S. A Multifactorial Conceptualization of Impulsivity. J. Individ. Differ. 2015, 36, 191–198. [Google Scholar] [CrossRef]
- Sharma, L.; Markon, K.E.; Clark, L.A. Toward a Theory of Distinct Types of “Impulsive” Behaviors: A Meta-Analysis of Self-Report and Behavioral Measures. Psychol. Bull. 2014, 140, 374–408. [Google Scholar] [CrossRef] [PubMed]
- Maccallum, F.; Blaszczynski, A.; Ladouceur, R.; Nower, L. Functional and Dysfunctional Impulsivity in Pathological Gambling. Pers. Individ. Dif. 2007, 43, 1829–1838. [Google Scholar] [CrossRef]
- Navas, J.F.; Contreras-Rodríguez, O.; Verdejo-Román, J.; Perandrés-Gómez, J.; Albein-Urios, N.; Verdejo-García, A.; Perales, J.C. Trait and Neurobiological Underpinnings of Negative Emotion Regulation in Gambling Disorder. Addiction 2017, 112, 1086–1094. [Google Scholar] [CrossRef]
- Pace, U.; Zappulla, C.; Di Maggio, R.; Passanisi, A.; Craparo, G.; Di Maggio, R.; Zappulla, C. Characteristics of Regular Gamblers in Italy: The Role of Control and Emotion Regulation. Clin. Neuropsychiatry 2015, 12, 111–117. [Google Scholar]
- Lage, G.M.; Albuquerque, M.R.; Fuentes, D.; Corrêa, H.; Malloy-Diniz, L.F. Sex Differences in Dimensions of Impulsivity in a Non-Clinical Sample. Percept. Mot. Skills 2013, 117, 601–607. [Google Scholar] [CrossRef]
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
|---|---|---|---|---|---|---|---|---|
| 1 | DSM 5 criteria | --- | 0.589† | 0.342† | 0.252† | 0.208 | 0.378† | 0.349† |
| 2 | SOGS total | 0.834† | --- | 0.023 | 0.016 | 0.091 | 0.310† | 0.363† |
| 3 | DERS Total score | 0.314† | 0.284† | --- | 0.407† | 0.054 | 0.411† | 0.377† |
| 4 | ERQ Suppression | 0.302† | 0.268† | 0.431† | --- | 0.350† | 0.180 | 0.213 |
| 5 | ERQ Reappraisal | 0.062 | -0.028 | 0.099 | 0.307† | --- | 0.223 | 0.190 |
| 6 | UPPS-P Total score | 0.162 | 0.030 | 0.603† | 0.405† | 0.026 | --- | 0.312† |
| 7 | SCL-90-R GSI | 0.034 | 0.127 | 0.472† | 0.433† | 0.019 | 0.289† | --- |
| Control (CO) | Experimental (EXP) | Contrasts | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 64) | (n = 40) | Inter. | Factor Group (CO-EXP) | Factor Time (Pre-Post) | |||||||||||||||
| Pre-CBT | Post-CBT | Pre-CBT | Post-CBT | Group | Pre-CBT | Post-CBT | Control | Experimental | |||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Time | p | η2 | p | η2 | p | η2 | Power | p | η2 | Power | |
| GD severity | |||||||||||||||||||
| DSM 5 criteria | 7.39 | 1.39 | 2.13 | 2.04 | 7.10 | 1.75 | 1.93 | 2.13 | 0.848 | 0.350 | 0.009 | 0.634 | 0.002 | 0.001 * | 0.761 † | 1.000 | 0.001 * | 0.658 † | 1.000 |
| SOGS total | 11.1 | 3.14 | 6.11 | 3.85 | 11.1 | 3.32 | 4.78 | 3.17 | 0.152 | 0.946 | 0.000 | 0.069 | 0.032 | 0.001* | 0.442 † | 1.000 | 0.001* | 0.440 † | 1.000 |
| Psyc. (SCL-90R) | |||||||||||||||||||
| Somatization | 0.91 | 0.79 | 0.48 | 0.42 | 0.88 | 0.82 | 0.33 | 0.40 | 0.863 | 0.482 | 0.005 | 0.132 | 0.022 | 0.001 * | 0.209 † | 0.999 | 0.001 * | 0.155 † | 0.990 |
| Obsess-comp. | 1.16 | 0.85 | 0.61 | 0.51 | 0.94 | 0.63 | 0.44 | 0.37 | 0.565 | 0.703 | 0.001 | 0.083 | 0.029 | 0.001 * | 0.327 † | 1.000 | 0.001 * | 0.280 † | 1.000 |
| Sensitivity | 1.02 | 0.87 | 0.47 | 0.54 | 0.90 | 0.78 | 0.32 | 0.39 | 0.863 | 0.482 | 0.005 | 0.132 | 0.022 | 0.001 * | 0.209 † | 0.999 | 0.001 * | 0.155 † | 0.990 |
| Depression | 1.54 | 1.03 | 0.67 | 0.60 | 1.46 | 0.96 | 0.48 | 0.45 | 0.565 | 0.703 | 0.001 | 0.083 | 0.029 | 0.001 * | 0.327 † | 1.000 | 0.001 * | 0.280 † | 1.000 |
| Anxiety | 1.04 | 0.79 | 0.44 | 0.46 | 0.94 | 0.83 | 0.32 | 0.42 | 0.914 | 0.522 | 0.004 | 0.177 | 0.018 | 0.001 * | 0.250 † | 1.000 | 0.001 * | 0.181 † | 0.997 |
| Hostility | 0.89 | 0.86 | 0.45 | 0.49 | 0.71 | 0.75 | 0.37 | 0.60 | 0.597 | 0.278 | 0.012 | 0.434 | 0.006 | 0.001 * | 0.132 † | 0.974 | 0.016 * | 0.055 | 0.676 |
| Phobic anxiety | 0.42 | 0.60 | 0.17 | 0.23 | 0.30 | 0.38 | 0.09 | 0.11 | 0.723 | 0.279 | 0.011 | 0.047 * | 0.038 | 0.001 * | 0.124 † | 0.965 | 0.012 * | 0.060 | 0.716 |
| Paranoia | 0.94 | 0.78 | 0.43 | 0.42 | 0.79 | 0.78 | 0.37 | 0.38 | 0.589 | 0.355 | 0.008 | 0.459 | 0.005 | 0.001 * | 0.212 † | 0.999 | 0.001 * | 0.104 † | 0.927 |
| Psychotic | 0.92 | 0.77 | 0.37 | 0.37 | 0.88 | 0.76 | 0.20 | 0.22 | 0.434 | 0.757 | 0.001 | 0.012 * | 0.061 | 0.001 * | 0.260 † | 1.000 | 0.001 * | 0.244 † | 1.000 |
| GSI | 1.07 | 0.74 | 0.50 | 0.45 | 0.96 | 0.67 | 0.35 | 0.33 | 0.771 | 0.461 | 0.005 | 0.073 | 0.031 | 0.001 * | 0.274 † | 1.000 | 0.001 * | 0.214 † | 0.999 |
| PST | 46.9 | 22.0 | 25.1 | 17.6 | 44.8 | 20.2 | 20.9 | 13.5 | 0.653 | 0.620 | 0.002 | 0.197 | 0.016 | 0.001 * | 0.362 † | 1.000 | 0.001 * | 0.298 † | 1.000 |
| PSDI | 1.85 | 0.59 | 1.41 | 0.38 | 1.76 | 0.60 | 1.25 | 0.50 | 0.612 | 0.450 | 0.006 | 0.065 | 0.033 | 0.001 * | 0.205 † | 0.999 | 0.001 * | 0.179 † | 0.997 |
| Control n = 64 | Experimental n = 40 | ||||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | p | C-V | Power | |
| Risk of dropout | |||||||
| Yes | 15 | 23.4% | 6 | 15.0% | 0.297 | 0.102 | 0.186 |
| No | 49 | 76.6% | 34 | 85.0% | |||
| Risk of relapses | |||||||
| Yes | 17 | 28.3% | 6 | 16.2% | 0.173 | 0.138 † | 0.160 |
| No | 43 | 71.7% | 31 | 83.8% | |||
| Compliance with rules | |||||||
| Bad | 22 | 36.1% | 5 | 13.5% | 0.015 * | 0.245 † | 0.779 |
| Good | 39 | 63.9% | 32 | 86.5% | |||
| Mean | SD | Mean | SD | p | η2 | power | |
| Number of sessions attended | 13.64 | 4.04 | 14.48 | 3.72 | 0.271 | 0.01 | 0.906 |
| Number of relapses | 0.75 | 1.95 | 0.27 | 0.69 | 0.007 * | 0.02 | 0.836 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mena-Moreno, T.; Munguía, L.; Granero, R.; Lucas, I.; Fernández-Aranda, F.; Gómez-Peña, M.; Moragas, L.; Verdejo-García, A.; Menchón, J.M.; Jiménez-Murcia, S. e-Estesia: A Serious Game for Reducing Arousal, Improving Emotional Regulation and Increasing Wellbeing in Individuals with Gambling Disorder. J. Clin. Med. 2022, 11, 6798. https://doi.org/10.3390/jcm11226798
Mena-Moreno T, Munguía L, Granero R, Lucas I, Fernández-Aranda F, Gómez-Peña M, Moragas L, Verdejo-García A, Menchón JM, Jiménez-Murcia S. e-Estesia: A Serious Game for Reducing Arousal, Improving Emotional Regulation and Increasing Wellbeing in Individuals with Gambling Disorder. Journal of Clinical Medicine. 2022; 11(22):6798. https://doi.org/10.3390/jcm11226798
Chicago/Turabian StyleMena-Moreno, Teresa, Lucero Munguía, Roser Granero, Ignacio Lucas, Fernando Fernández-Aranda, Mónica Gómez-Peña, Laura Moragas, Antonio Verdejo-García, José M. Menchón, and Susana Jiménez-Murcia. 2022. "e-Estesia: A Serious Game for Reducing Arousal, Improving Emotional Regulation and Increasing Wellbeing in Individuals with Gambling Disorder" Journal of Clinical Medicine 11, no. 22: 6798. https://doi.org/10.3390/jcm11226798
APA StyleMena-Moreno, T., Munguía, L., Granero, R., Lucas, I., Fernández-Aranda, F., Gómez-Peña, M., Moragas, L., Verdejo-García, A., Menchón, J. M., & Jiménez-Murcia, S. (2022). e-Estesia: A Serious Game for Reducing Arousal, Improving Emotional Regulation and Increasing Wellbeing in Individuals with Gambling Disorder. Journal of Clinical Medicine, 11(22), 6798. https://doi.org/10.3390/jcm11226798








