Laparoscopic Adenomyomectomy under Real-Time Intraoperative Ultrasound Elastography Guidance: A Case Series and Feasibility Study
Abstract
1. Introduction
2. Patients and Methods
2.1. Study Design
2.2. Ethical Approval
2.3. Patients
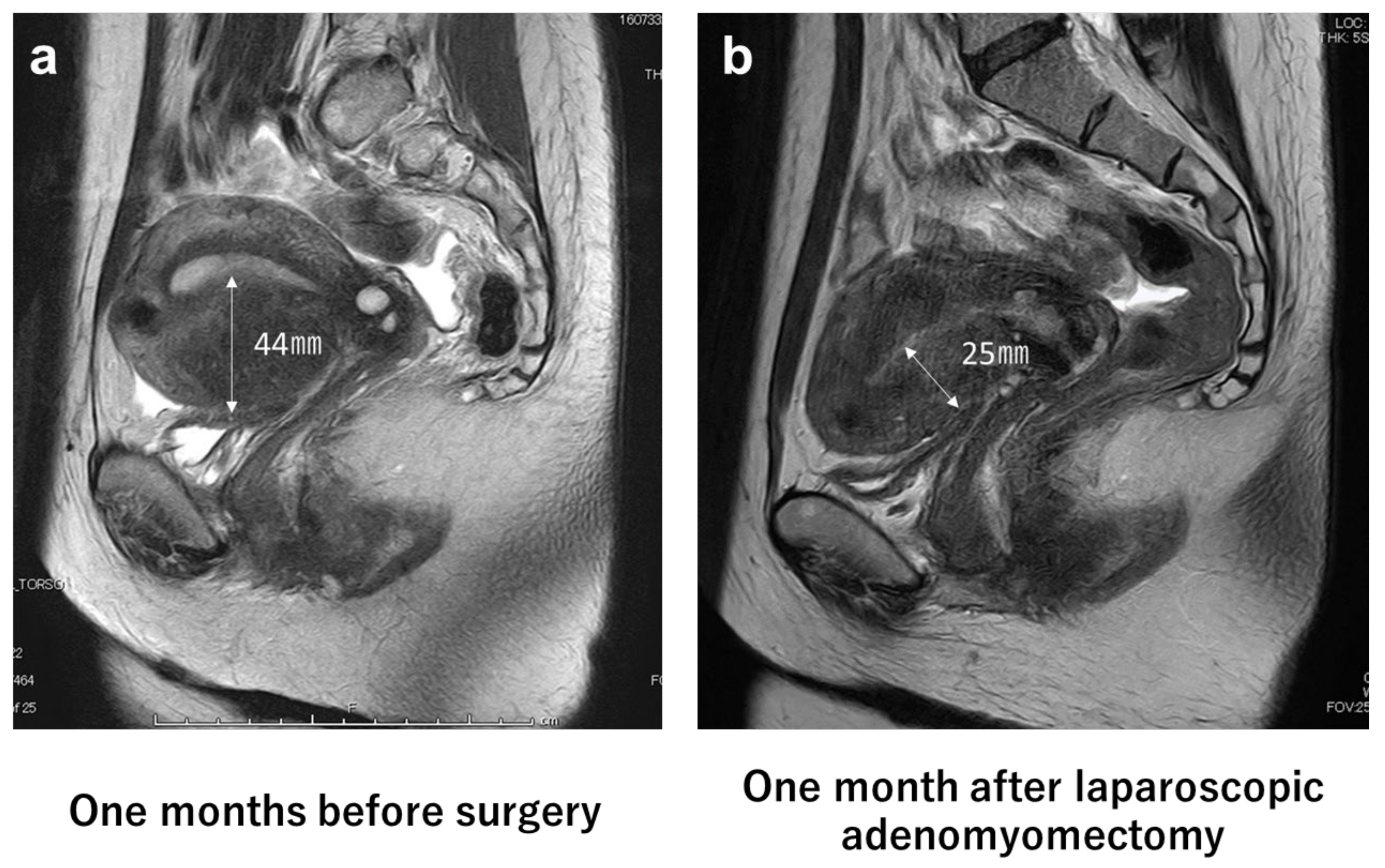
2.4. Diagnosis of Adenomyosis and Calculation of Uterus and Adenomyosis Lesion Volume
2.5. Pre- and Postoperative Hormonal Treatment and Evaluation of Dysmenorrhea
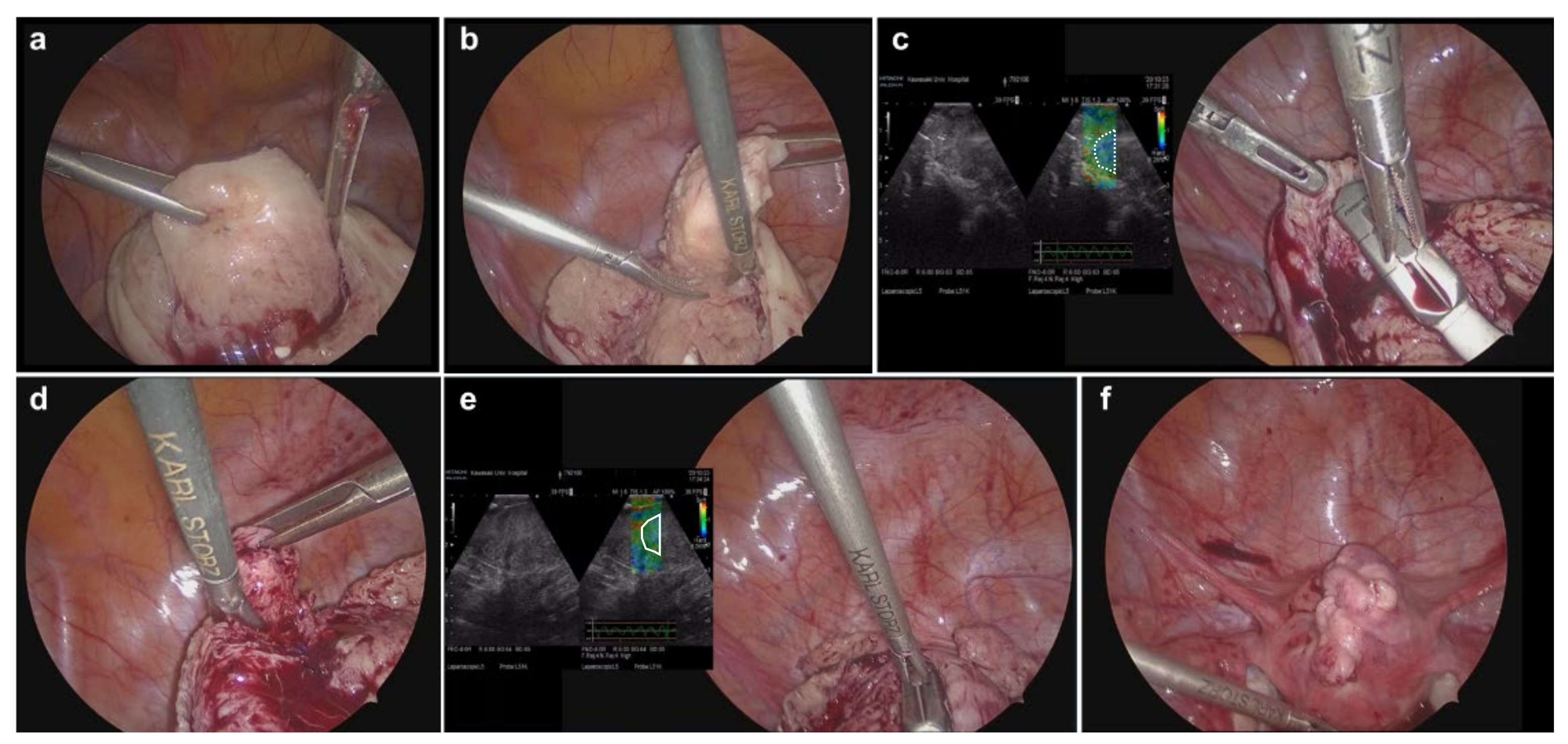
2.6. Surgical Procedures
2.7. Operative Outcome Measures
2.8. Postoperative Follow-Up and an Evaluation of Recurrence
2.9. Statistical Analysis
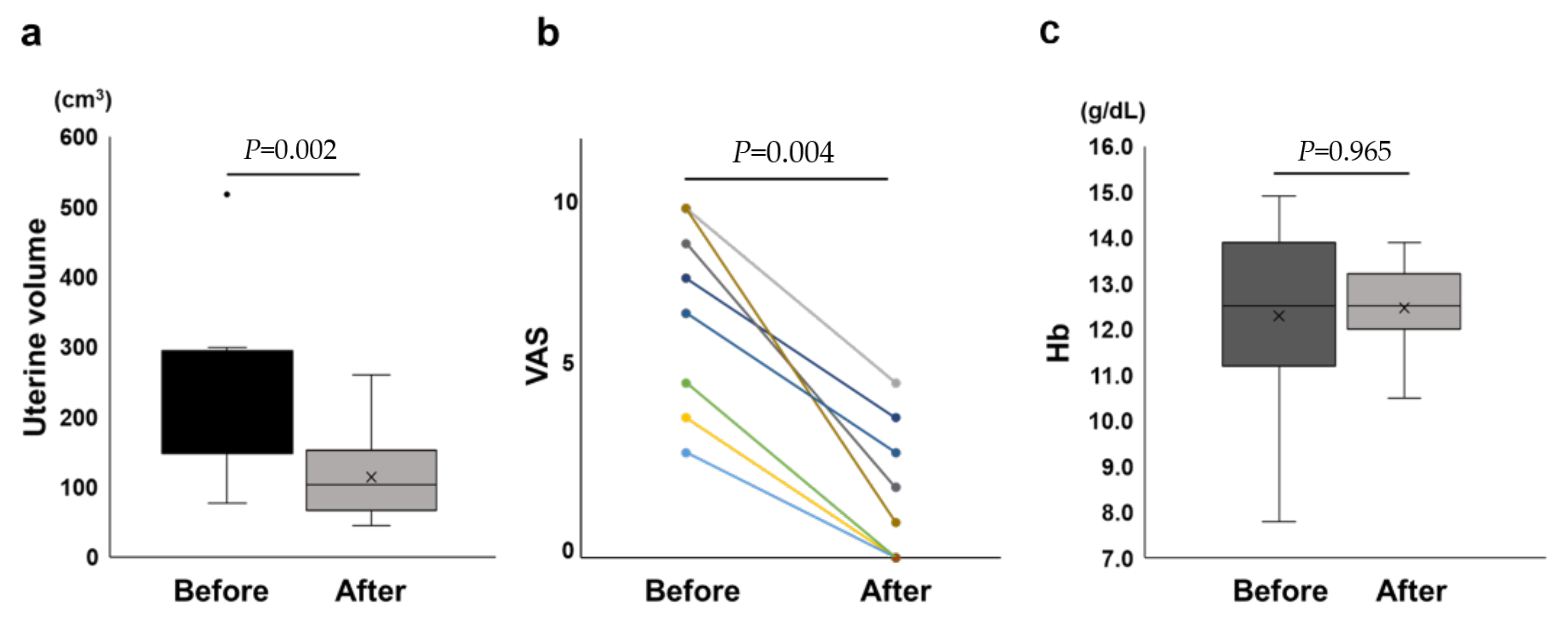
3. Results
3.1. Preoperative Patient Characteristics
3.2. Operative Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bergeron, C.; Amant, F.; Ferenczy, A. Pathology and physiopathology of adenomyosis. Best Pract. Res. Clin. Obstet. Gynaecol. 2006, 20, 511–521. [Google Scholar] [CrossRef] [PubMed]
- Leyendecker, G.; Wildt, L.; Mall, G. The pathophysiology of endometriosis and adenomyosis: Tissue injury and repair. Arch. Gynecol. Obstet. 2009, 280, 529–538. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Ding, D.; Ren, Y.; Guo, S.W. Transvaginal elastosonography as an imaging technique for diagnosing adenomyosis. Reprod. Sci. 2018, 25, 498–514. [Google Scholar] [CrossRef] [PubMed]
- Saremi, A.; Bahrami, H.; Salehian, P.; Hakak, N.; Pooladi, A. Treatment of adenomyomectomy in women with severe uterine adenomyosis using a novel technique. Reprod. Biomed. Online 2014, 28, 753–760. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Wang, L.; Wu, H.; Wei, X.; Duan, Y.; Xu, L.; Yang, Z.; Liu, L. Controlled study of traditional ultrasound and ultrasound elastography on the diagnosis of breast masses. Ultrasound Q. 2015, 31, 250–254. [Google Scholar] [CrossRef]
- Li, C.; Zhang, C.; Li, J.; Huo, H.; Song, D. Diagnostic accuracy of real-time shear wave elastography for staging of liver fibrosis: A meta-analysis. Med. Sci. Monit. 2016, 22, 1349–1359. [Google Scholar] [CrossRef][Green Version]
- Zhang, M.; Wasnik, A.P.; Masch, W.R.; Rubin, J.M.; Carlos, R.C.; Quint, E.H.; Maturen, K.E. Transvaginal ultrasound shear wave elastography for the evaluation of benign uterine pathologies: A prospective pilot study. J. Ultrasound Med. 2019, 38, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Acar, S.; Millar, E.; Mitkova, M.; Mitkov, V. Value of ultrasound shear wave elastography in the diagnosis of adenomyosis. Ultrasound 2016, 24, 205–213. [Google Scholar] [CrossRef]
- Della Pepa, G.M.; Menna, G.; Stifano, V.; Pezzullo, A.M.; Auricchio, A.M.; Rapisarda, A.; Caccavella, V.M.; La Rocca, G.; Sabatino, G.; Marchese, E.; et al. Predicting meningioma consistency and brain-meningioma interface with intraoperative strain ultrasound elastography: A novel application to guide surgical strategy. Neurosurg. Focus. 2021, 50, E15. [Google Scholar] [CrossRef]
- Ota, Y.; Ota, K.; Takahashi, T.; Suzuki, S.; Sano, R.; Shiota, M. New surgical technique of laparoscopic resection of adenomyosis under real-time intraoperative ultrasound elastography guidance: A case report. Heliyon 2020, 6, e04628. [Google Scholar] [CrossRef]
- Ota, Y.; Ota, K.; Takahashi, T.; Morimoto, Y.; Suzuki, S.; Sano, R.; Ota, I.; Moriya, T.; Shiota, M. A case of elastography-assisted laparoscopic fertility preservation for severe deep endometriosis causing ureteral stenosis and Subtype II adenomyosis. Endocrines 2021, 2, 348–355. [Google Scholar] [CrossRef]
- Tamai, K.; Koyama, T.; Umeoka, S.; Saga, T.; Fujii, S.; Togashi, K. Spectrum of MR features in adenomyosis. Best Pract. Res. Clin. Obstet. Gynaecol. 2006, 20, 583–602. [Google Scholar] [CrossRef]
- Kishi, Y.; Suginami, H.; Kuramori, R.; Yabuta, M.; Suginami, R.; Taniguchi, F. Four subtypes of adenomyosis assessed by magnetic resonance imaging and their specification. Am. J. Obstet. Gynecol. 2012, 207, 114.e1–114.e7. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.; Xu, P.; Zou, G.; Wang, J.; Zhu, L.; Zhang, X. Extrinsic adenomyosis is associated with postoperative recurrence of ovarian endometrioma. Front. Med. 2021, 8, 815628. [Google Scholar] [CrossRef] [PubMed]
- Lindh, I.; Milsom, I. The influence of intrauterine contraception on the prevalence and severity of dysmenorrhea: A longitudinal population study. Hum. Reprod. 2013, 28, 1953–1960. [Google Scholar] [CrossRef] [PubMed]
- Ota, Y.; Ota, K.; Takahashi, T.; Suzuki, S.; Sano, R.; Shiota, M. A suturing method without exposure of barbs on the wound surface using a unidirectional barbed monofilament absorbable suture (Stratafix™) in laparoscopic myomectomy: A feasibility study. Gynecol. Minim. Invasive Ther. 2021, 10, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Katayama, H.; Kurokawa, Y.; Nakamura, K.; Ito, H.; Kanemitsu, Y.; Masuda, N.; Tsubosa, Y.; Satoh, T.; Yokomizo, A.; Fukuda, H.; et al. Extended Clavien-Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg. Today 2016, 46, 668–685. [Google Scholar] [CrossRef]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef]
- Ye, M.Z.; Deng, X.L.; Zhu, X.G.; Xue, M. Clinical study of high intensity focused ultrasound ablation combined with GnRH-a and LNG-IUS for the treatment of adenomyosis. Zhonghua Fu Chan Ke Za Zhi 2016, 51, 643–649. [Google Scholar] [CrossRef]
- Galazis, N.; Saso, S.; Sorbi, F.; Jones, B.; Landolfo, C.; Al-Memar, M.; Ben-Nagi, J.; Smith, J.R.; Yazbek, J. Intraoperative ultrasound during fertility-sparing surgery: A systematic review and practical applications. Gynecol. Obstet. Investig. 2020, 85, 127–148. [Google Scholar] [CrossRef]
- Stoelinga, B.; Hehenkamp, W.J.; Brölmann, H.A.; Huirne, J.A. Real-time elastography for assessment of uterine disorders. Ultrasound Obstet. Gynecol. 2014, 43, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Osada, H. Uterine adenomyosis and adenomyoma: The surgical approach. Fertil. Steril. 2018, 109, 406–417. [Google Scholar] [CrossRef] [PubMed]
- Osada, H.; Silber, S.; Kakinuma, T.; Nagaishi, M.; Kato, K.; Kato, O. Surgical procedure to conserve the uterus for future pregnancy in patients suffering from massive adenomyosis. Reprod. Biomed. Online 2011, 22, 94–99. [Google Scholar] [CrossRef]
- Nishida, M.; Takano, K.; Arai, Y.; Ozone, H.; Ichikawa, R. Conservative surgical management for diffuse uterine adenomyosis. Fertil. Steril. 2010, 94, 715–719. [Google Scholar] [CrossRef] [PubMed]
- Ota, K.; Takahashi, T.; Shiraishi, S.; Mizunuma, H. Combination of microwave endometrial ablation and postoperative dienogest administration is effective for treating symptomatic adenomyosis. J. Obstet. Gynaecol. Res. 2018, 44, 1787–1792. [Google Scholar] [CrossRef]
| Case | Age (Years) | BMI (kg/cm2) | Gravida-Parity | Chief Complaint | Location of Adenomyotic Lesion | Uterine Volume (cm3) | Adenomyotic Lesion Volume (cm3) | Hb (g/dL) | VAS | Preoperative HT |
|---|---|---|---|---|---|---|---|---|---|---|
| Case 1 | 32 | 26.8 | 1-0 | Hypermenorrhea | Anterior | 518 | 155 | 10.5 | 10 | Yes |
| Case 2 | 39 | 19.6 | 1-0 | Hypermenorrhea | Posterior | 295 | 137 | 7.8 | 8 | No |
| Case 3 | 35 | 20.3 | 0 | Dysmenorrhea | Posterior | 78 | 13 | 14.6 | 10 | Yes |
| Case 4 | 37 | 25.6 | 0 | Hypermenorrhea | Posterior | 154 | 62 | 14.9 | 4 | Yes |
| Case 5 | 41 | 24.8 | 0 | Dysmenorrhea | Anterior | 257 | 58 | 11.2 | 3 | Yes |
| Case 6 | 40 | 21.0 | 1-0 | Hypermenorrhea | Anterior | 149 | 29 | 11.2 | 5 | Yes |
| Case 7 | 42 | 28.1 | 0 | Dysmenorrhea, hypermenorrhea | Anterior | 224 | 11 | 13.9 | 8 | Yes |
| Case 8 | 31 | 22.0 | 0 | Dysmenorrhea | Posterior | 88 | 14 | 12.5 | 7 | Yes |
| Case 9 | 33 | 20.7 | 0 | Dysmenorrhea | Posterior | 167 | 19 | 12.4 | 9 | Yes |
| Case 10 | 32 | 17.5 | 0 | Dysmenorrhea | Posterior | 239 | 90 | 12.6 | 10 | Yes |
| Case 11 | 35 | 21.3 | 0 | Wish to have a child | Posterior | 300 | 101 | 13.6 | 7 | No |
| Case | Operation | Concurrent Operation | Operative Time (min) | Operative Bleeding (mL) | Resected Weight (g) | Uterine Volume (cm3) | Hb (g/dL) | VAS (6 Months Later) | VAS (12 Months Later) | Postoperative HT | Follow-up Period (Months) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Case 1 | LAM | None | 127 | 450 | 180.0 | 261 | 13.9 | 2 | 2 | No | 30 |
| Case 2 | LAM | None | 115 | 300 | 64.0 | 154 | 10.5 | 3 | 5 | No | 14 |
| Case 3 | LAM | LM+EDE | 125 | 150 | 1.5 | 56 | 13.0 | 5 | 2 | Yes | 18 |
| Case 4 | LAM | None | 96 | 10 | 50.0 | 79 | 13.2 | 0 | 0 | Yes | 14 |
| Case 5 | LAM | None | 125 | 150 | 50.0 | 152 | 12.5 | 0 | 0 | Yes | 12 |
| Case 6 | LAM | None | 88 | 50 | 28.5 | NA | 12.1 | 0 | 0 | Yes | 16 |
| Case 7 | LAM | LM | 122 | 150 | 17.0 | 103 | 13.5 | 4 | 0 | Yes | 15 |
| Case 8 | LAM | LC+EDE | 147 | 10 | 10.0 | 45 | 11.1 | 0 | NA | Yes | 11 |
| Case 9 | LAM | EDE | 111 | 50 | 8.5 | 71 | 12.1 | 2 | NA | Yes | 9 |
| Case 10 | LAM | LM | 135 | 300 | 68.0 | 121 | 12.0 | 1 | NA | Yes | 8 |
| Case 11 | LAM | LM+LC+EDE | 188 | 100 | 102.5 | 104 | 13.2 | 3 | NA | Yes | 7 |
| Case | Uterine Volume (cm3) | Hb (g/dL) | VAS | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Before | After | Percentage Change (%) | Before | After | Percentage of Change (%) | Before | Six Months Later | Percentage of Change (%) | |
| Case 1 | 518 | 261 | −50 | 10.5 | 13.9 | 32 | 10 | 2 | −80 |
| Case 2 | 295 | 154 | −48 | 7.8 | 10.5 | 35 | 8 | 3 | −63 |
| Case 3 | 78 | 56 | −28 | 14.6 | 13 | −11 | 10 | 5 | −50 |
| Case 4 | 154 | 79 | −49 | 14.9 | 13.2 | −11 | 4 | 0 | −100 |
| Case 5 | 257 | 152 | −41 | 11.2 | 12.5 | 12 | 3 | 0 | −100 |
| Case 6 | 149 | NA | NA | 11.2 | 12.1 | 8 | 5 | 0 | −100 |
| Case 7 | 224 | 103 | −54 | 13.9 | 13.5 | −3 | 8 | 4 | −50 |
| Case 8 | 88 | 45 | −49 | 12.5 | 11.1 | −11 | 7 | 0 | −100 |
| Case 9 | 167 | 71 | −57 | 12.4 | 12.1 | −2 | 9 | 2 | −78 |
| Case 10 | 239 | 121 | −49 | 12.6 | 12 | −5 | 10 | 1 | −90 |
| Case 11 | 300 | 104 | −65 | 13.6 | 13.2 | −3 | 7 | 3 | −57 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ota, Y.; Ota, K.; Takahashi, T.; Morimoto, Y.; Suzuki, S.; Sano, R.; Shiota, M. Laparoscopic Adenomyomectomy under Real-Time Intraoperative Ultrasound Elastography Guidance: A Case Series and Feasibility Study. J. Clin. Med. 2022, 11, 6707. https://doi.org/10.3390/jcm11226707
Ota Y, Ota K, Takahashi T, Morimoto Y, Suzuki S, Sano R, Shiota M. Laparoscopic Adenomyomectomy under Real-Time Intraoperative Ultrasound Elastography Guidance: A Case Series and Feasibility Study. Journal of Clinical Medicine. 2022; 11(22):6707. https://doi.org/10.3390/jcm11226707
Chicago/Turabian StyleOta, Yoshiaki, Kuniaki Ota, Toshifumi Takahashi, Yumiko Morimoto, Soichiro Suzuki, Rikiya Sano, and Mitsuru Shiota. 2022. "Laparoscopic Adenomyomectomy under Real-Time Intraoperative Ultrasound Elastography Guidance: A Case Series and Feasibility Study" Journal of Clinical Medicine 11, no. 22: 6707. https://doi.org/10.3390/jcm11226707
APA StyleOta, Y., Ota, K., Takahashi, T., Morimoto, Y., Suzuki, S., Sano, R., & Shiota, M. (2022). Laparoscopic Adenomyomectomy under Real-Time Intraoperative Ultrasound Elastography Guidance: A Case Series and Feasibility Study. Journal of Clinical Medicine, 11(22), 6707. https://doi.org/10.3390/jcm11226707







