Femoral Component Rotation in Total Knee Arthroplasty Using a Tibia-First, Gap-Balancing, “Functional Alignment” Technique
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Participants
2.3. Surgical Technique
2.4. Clinical Outcomes
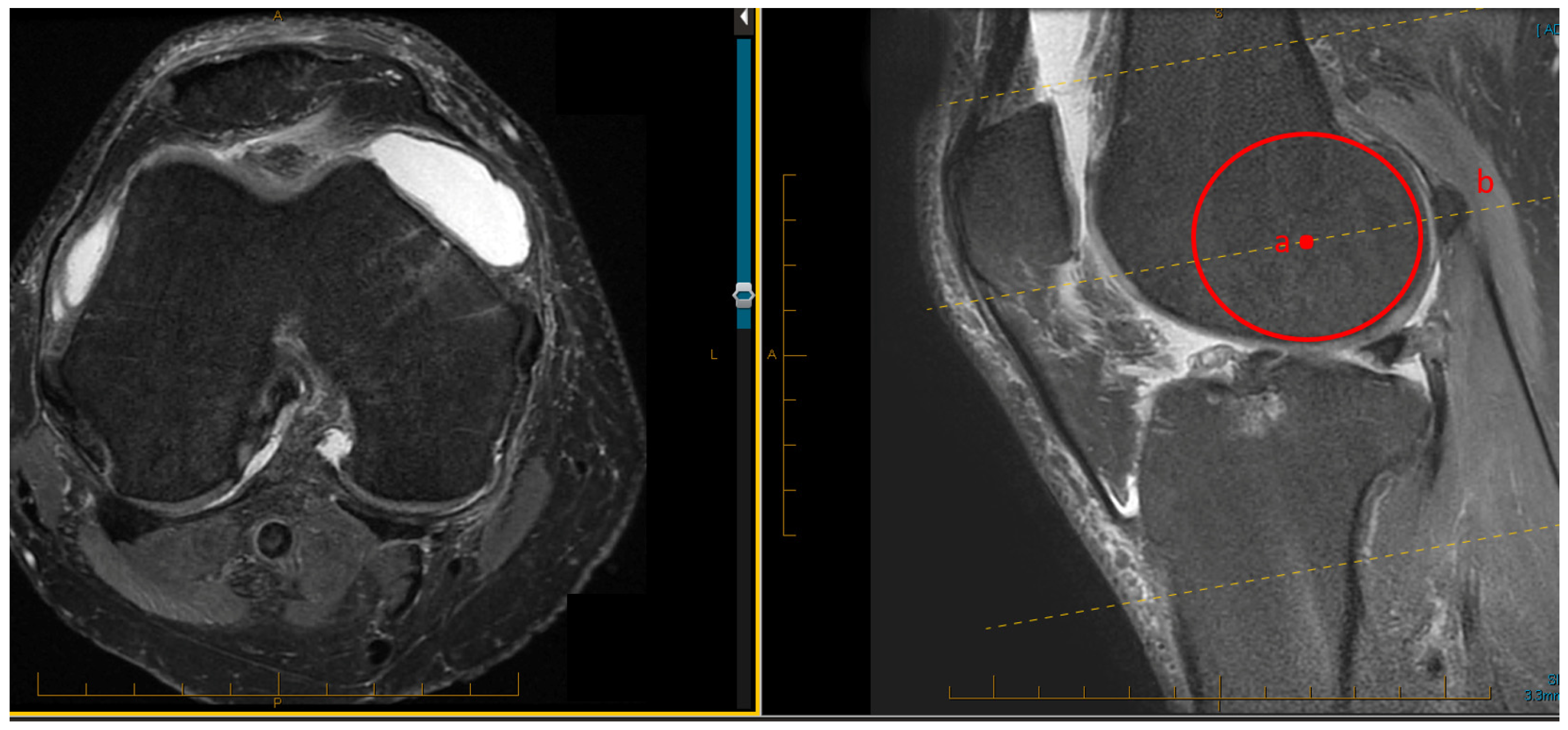
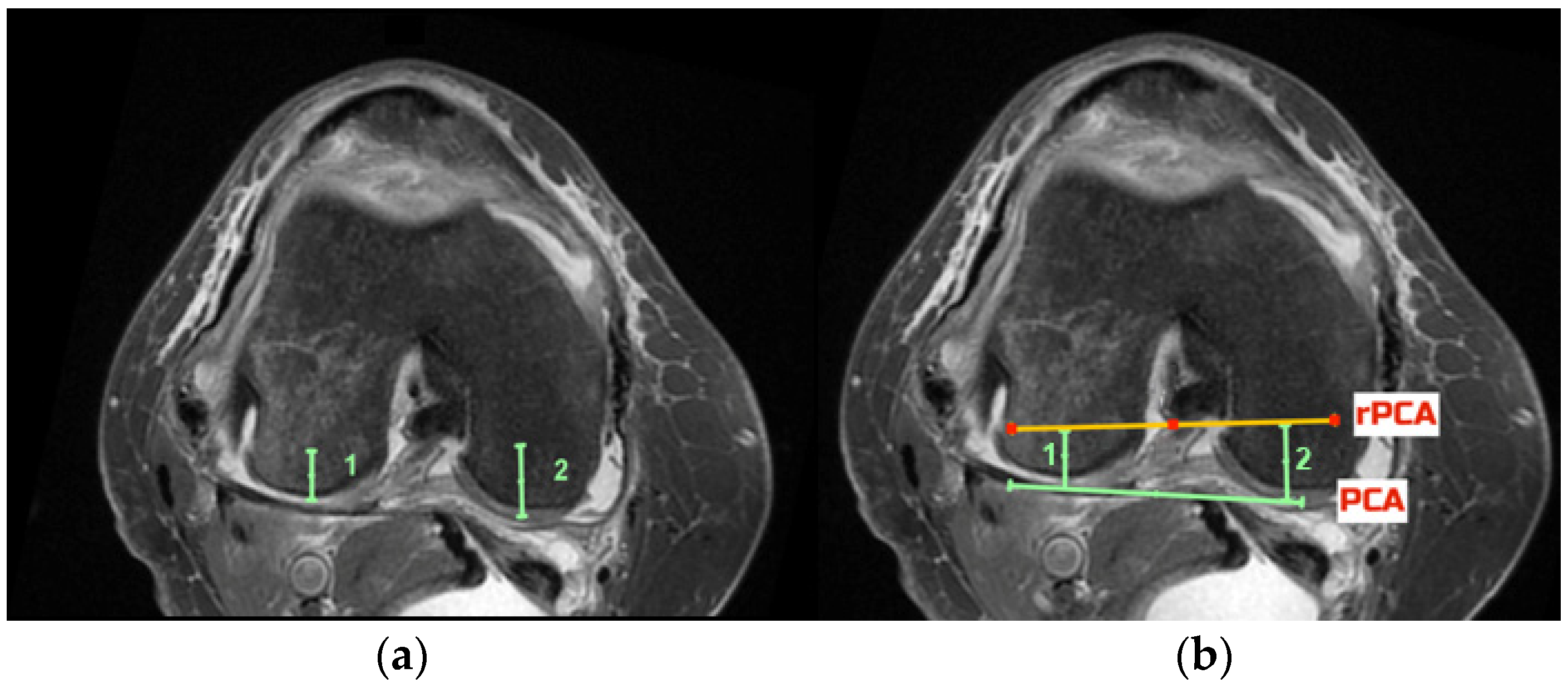
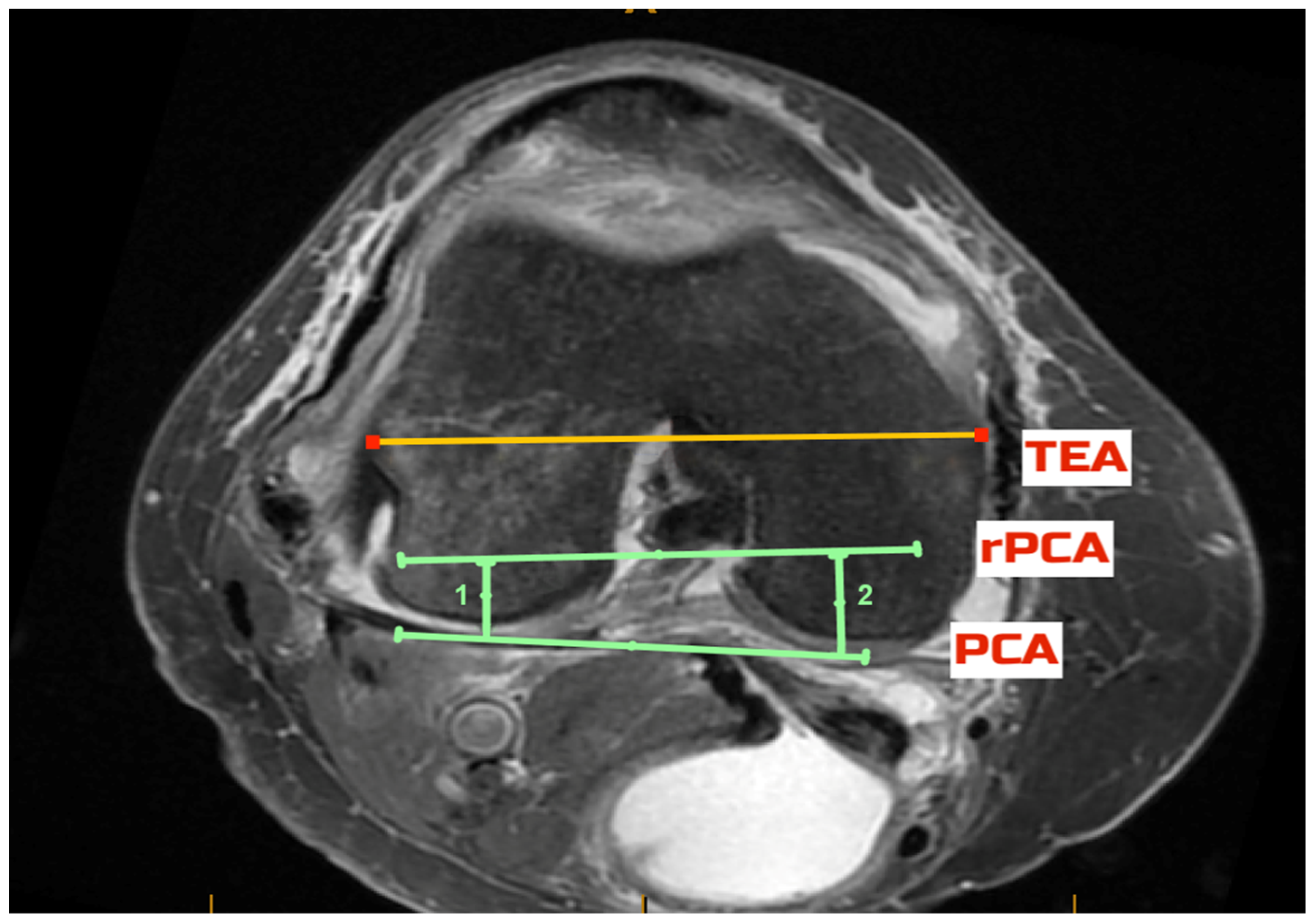
2.5. Radiological Outcomes
2.6. Statistical Analysis
3. Results
3.1. Patient Demographics
3.2. Clinical and Radiological Outcomes
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Castelli, C.C.; Falvo, D.A.; Iapicca, M.L.; Gotti, V. Rotational alignment of the femoral component in total knee arthroplasty. Ann. Transl. Med. 2016, 4, 4. [Google Scholar]
- Nedopil, A.J.; Howell, S.M.; Hull, M.L. Does Malrotation of the Tibial and Femoral Components Compromise Function in Kinematically Aligned Total Knee Arthroplasty? Orthop. Clin. N. Am. 2016, 47, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Daines, B.K.; Dennis, D.A. Gap balancing vs. measured resection technique in total knee arthroplasty. Clin. Orthop. Surg. 2014, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Clatworthy, M.; Lindberg, K.; Wray, W.H.; Sychterz Terefenko, C.J.; Dennis, D.A.; Pollock, D. Rotational Alignment of the femoral component in Computer-assisted total knee replacement surgery. Reconstr. Rev. 2012, 2, 46–51. [Google Scholar]
- Gu, Y.; Roth, J.D.; Howell, S.M.; Hull, M.L. How Frequently Do Four Methods for Mechanically Aligning a Total Knee Arthroplasty Cause Collateral Ligament Imbalance and Change Alignment from Normal in White Patients? AAOS Exhibit Selection. J. Bone Jt. Surg. Am. 2014, 96, e101. [Google Scholar] [CrossRef]
- Lee, S.Y.; Lim, H.C.; Jang, K.M.; Bae, J.H. What Factors Are Associated with Femoral Component Internal Rotation in TKA Using the Gap Balancing Technique? Clin. Orthop. Relat. Res. 2017, 475, 1999–2010. [Google Scholar] [CrossRef][Green Version]
- Romero, J.; Stahelin, T.; Binkert, C.; Pfirrmann, C.; Hodler, J.; Kessler, O. The clinical consequences of flexion gap asymmetry in total kne arthroplasty. J. Arthroplast. 2007, 22, 235–240. [Google Scholar] [CrossRef]
- Dennis, D.A.; Komistek, R.D.; Kim, R.H.; Sharma, A. Gap balancing versus measured resection technique for total knee arthroplasty. Clin. Orthop. Relat. Res. 2010, 468, 102–107. [Google Scholar] [CrossRef]
- Lee, D.S.; Song, E.K.; Seon, J.P.S. Effect of balanced gap total knee arthroplasty on intraoperative laxities and femoral component rotation. J. Arthroplast. 2011, 26, 699–704. [Google Scholar] [CrossRef]
- Heesterbeek, P.J.C.; Jacobs, W.C.H.; Wymenga, A.B. Effects of the balanced gap technique on femoral component rotation in TKA. Clin. Orthop. Relat. Res. 2009, 467, 1015–1022. [Google Scholar] [CrossRef]
- Mercuri, J.J.; Pepper, A.M.; Werner, J.A.; Vigdorchik, J.M. Gap Balancing, Measured Resection, and Kinematic Alignment: How, When, and Why? JBJS Rev. 2019, 7, e2. [Google Scholar] [CrossRef]
- Park, A.; Duncan, S.T.; Nunley, R.M.; Keeney, J.A.; Barrack, R.L.; Nam, D. Relationship of the posterior femoral axis of the “kinematically aligned” total knee arthroplasty to the posterior condylar, transepicondylar, and anteroposterior femoral axes. Knee 2014, 21, 1120–1123. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lozano, R.; Campanelli, V.; Howell, S.; Hull, M. Kinematic alignment more closely restores the groove location and the sulcus angle of the native trochlea than mechanical alignment: Implications for prosthetic design. Knee Surg. Sport. Traumatol. Arthrosc. 2018, 27, 1504–1513. [Google Scholar] [CrossRef] [PubMed]
- Keshmiri, A.; Maderbacher, G.; Baier, C.; Benditz, A.; Grifka, J.; Greimel, F. Kinematic alignment in total knee arthroplasty leads to a better restoration of patellar kinematics compared to mechanic alignment. Knee Surg. Sport. Traumatol. Arthrosc. 2019, 27, 1529–1534. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, J.; Chandrashekar, N.; Gill, B.; Beynnon, B.D.; Slauterbeck, J.R.; Schutt, R.C.; Mansouri, H.; Dabezies, E. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J. Bone Jt. Surg.-Ser. A 2008, 90, 2724–2734. [Google Scholar] [CrossRef]
- Clatworthy, M. Outcome & Survival Analysis of Conventional Measured Resection, Neutral Alignment Attune TKA vs CAS Anatomic Tibia, Balanced Femur, Constitutional Alignment Attune TKA. Orthop. J. Sport. Med. 2017, 5, 2325967117S0015. [Google Scholar]
- Hazratwala, K.; O’Callaghan, W.; Dhariwal, S.; Wilkinson, M. Wide variation in tibial slopes and trochlear angles in the arthritic knee: A CT evaluation of 4116 pre-operative knees. Knee Surg. Sport. Traumatol. Arthrosc. 2021, 30, 3049–3060. [Google Scholar] [CrossRef]
- Callaghan, W.B.O.; Gouk, C.; Wilkinson, M.P.R.; Haztratwala, K. Computer-Aided Surgery-Navigated, Functional Alignment Total Knee Arthroplasty: A Surgical Technique. Arthroplast. Today 2022, 14, 121–127. [Google Scholar] [CrossRef]
- Corona, K.; Cerciello, S.; Vasso, M.; Toro, G.; Braile, A.; Arnold, M.P.; Schiavone Panni, A. Femoral component malrotation is not correlated with poor clinical outcomes after total knee arthroplasty. Knee Surg. Sport. Traumatol. Arthrosc. 2020, 28, 3879–3887. [Google Scholar] [CrossRef]
- Niki, Y.; Kobayashi, S.; Nagura, T.; Udagawa, K.; Harato, K. Joint Line Modification in Kinematically Aligned Total Knee Arthroplasty Improves Functional Activity but Not Patient Satisfaction. J. Arthroplast. 2018, 33, 2125–2130. [Google Scholar] [CrossRef]
- Wakelin, A.; Twiggs, J.G.; Wakelin, E.A.; Salazar, J.; Roe, J.P.; Solomon, M.; Parker, D.A.; Fritsch, B.; Liu, D.; Miles, B.P.; et al. Recent Advances in Arthroplasty Surgical Alteration of the Coronal and Axial Knee Alignment during TKA Correlates with Reduced Patient Reported Outcomes. Recent Adv. Arthroplast. 2019, 3, 84–93. [Google Scholar]
- Li, S.; Luo, X.; Wang, P.; Sun, H.; Wang, K.; Sun, X. Clinical Outcomes of Gap Balancing vs Measured Resection in Total Knee Arthroplasty: A Systematic Review and Meta-Analysis Involving 2259 Subjects. J. Arthroplast. 2018, 33, 2684–2693. [Google Scholar] [CrossRef] [PubMed]
- Dossett, H.G.; Estrada, N.A.; Swartz, G.J.; LeFevre, G.W.; Kwasman, B.G. A randomised controlled trial of kinematically and mechanically aligned total knee replacements: Two-year clinical results. Bone Jt. J. 2014, 96, 907–913. [Google Scholar] [CrossRef] [PubMed]
- Calliess, T.; Bauer, K.; Stukenborg-Colsman, C.; Windhagen, H.; Budde, S.; Ettinger, M. PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: A prospective, randomized study. Knee Surg. Sport. Traumatol. Arthrosc. 2017, 25, 1743–1748. [Google Scholar] [CrossRef]
| KSS | WOMAC | |
|---|---|---|
| Pre-op | 53.5 ± 7.5 | 45.8 ± 9.8 |
| 6 weeks | 60.6 ± 10.0 | 22.9 ± 9.0 |
| 6 months | 89.3 ± 10.6 | 3.4 ± 5.4 |
| 12 months | 93.8 ± 4.5 | 0.9 ± 1.6 |
| 24 months | 93.8 ± 6.2 | 0.4 ± 1.3 |
| Predominantly Affected Compartment | Resection of Medial Posterior Condyle (mm) | Resection of Lateral Posterior Condyle (mm) | Medial Posterior Tibial Slope | Lateral Posterior Tibial Slope | Resected Posterior Tibial Slope | Cartilage Loss Medial | Cartilage Loss Lateral |
|---|---|---|---|---|---|---|---|
| lateral | 7 | 8.5 | 0 | 7.2 | 7 | 1/3 loss | to bone |
| lateral | 8 | 10 | 5 | 10 | 9 | 1/3 loss | to bone |
| lateral | 7 | 8 | 5 | 6 | 6 | no loss | 1/3 loss |
| lateral | 8 | 9 | 7 | 9 | 9 | no loss | 1/2 loss |
| medial | 9 | 7 | 7 | 4 | 7 | 1/3 loss | no loss |
| medial | 10 | 7 | 8.5 | 4 | 8 | to bone | no loss |
| medial | 12 | 10 | 10 | 7 | 9 | 1/2 loss | no loss |
| medial | 11 | 9 | 9 | 9 | 9 | 2/3 loss | no loss |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dlaska, C.; Ismailidis, P.; Doma, K.; Brandon, B.; Wilkinson, M.; Hazratwala, K. Femoral Component Rotation in Total Knee Arthroplasty Using a Tibia-First, Gap-Balancing, “Functional Alignment” Technique. J. Clin. Med. 2022, 11, 6680. https://doi.org/10.3390/jcm11226680
Dlaska C, Ismailidis P, Doma K, Brandon B, Wilkinson M, Hazratwala K. Femoral Component Rotation in Total Knee Arthroplasty Using a Tibia-First, Gap-Balancing, “Functional Alignment” Technique. Journal of Clinical Medicine. 2022; 11(22):6680. https://doi.org/10.3390/jcm11226680
Chicago/Turabian StyleDlaska, Constantin, Petros Ismailidis, Kenji Doma, Benjamin Brandon, Matthew Wilkinson, and Kaushik Hazratwala. 2022. "Femoral Component Rotation in Total Knee Arthroplasty Using a Tibia-First, Gap-Balancing, “Functional Alignment” Technique" Journal of Clinical Medicine 11, no. 22: 6680. https://doi.org/10.3390/jcm11226680
APA StyleDlaska, C., Ismailidis, P., Doma, K., Brandon, B., Wilkinson, M., & Hazratwala, K. (2022). Femoral Component Rotation in Total Knee Arthroplasty Using a Tibia-First, Gap-Balancing, “Functional Alignment” Technique. Journal of Clinical Medicine, 11(22), 6680. https://doi.org/10.3390/jcm11226680





