Recent Trends in Diabetes-Associated Hospitalizations in the United States
Abstract
1. Introduction
2. Materials and Methods
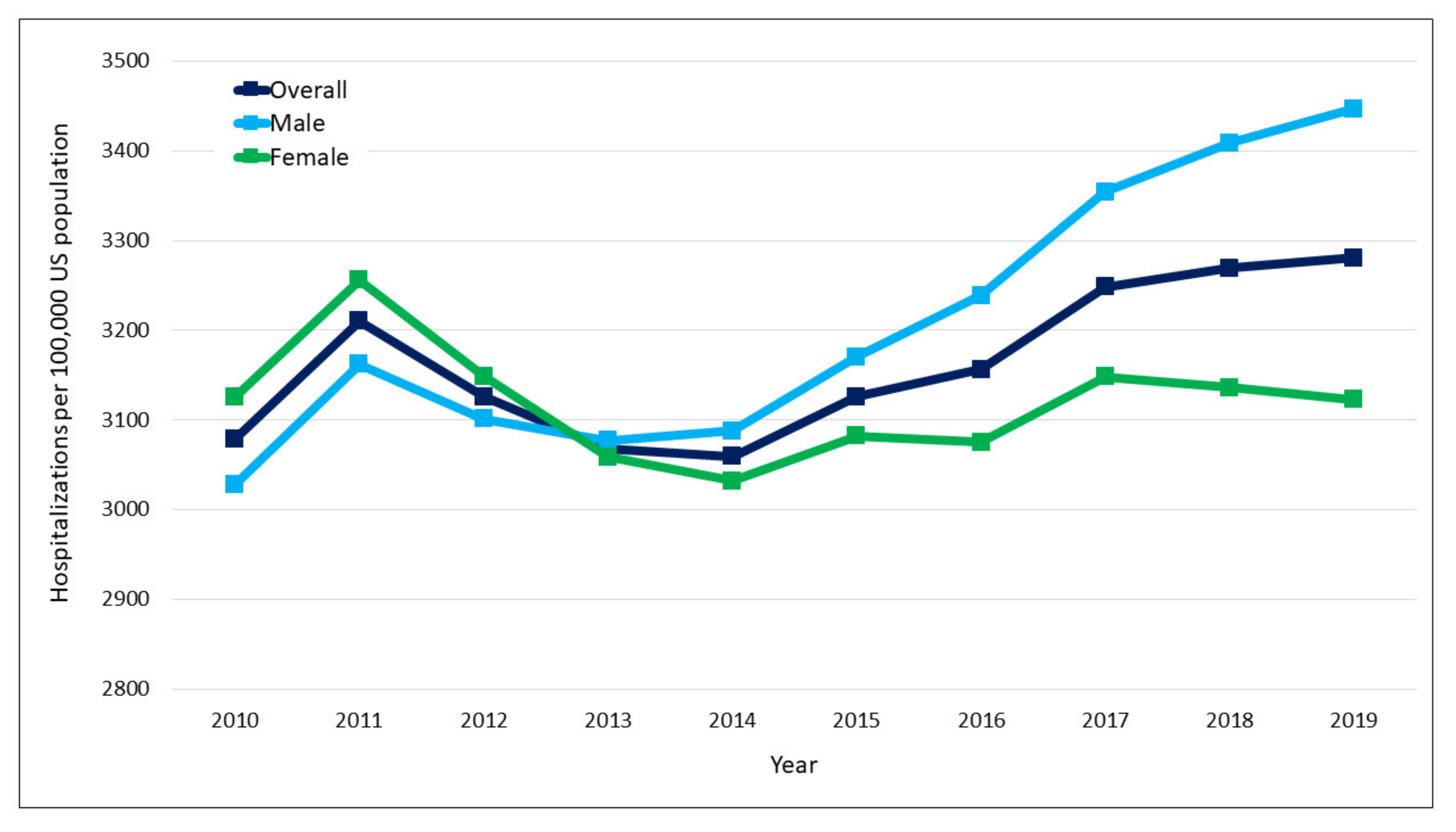
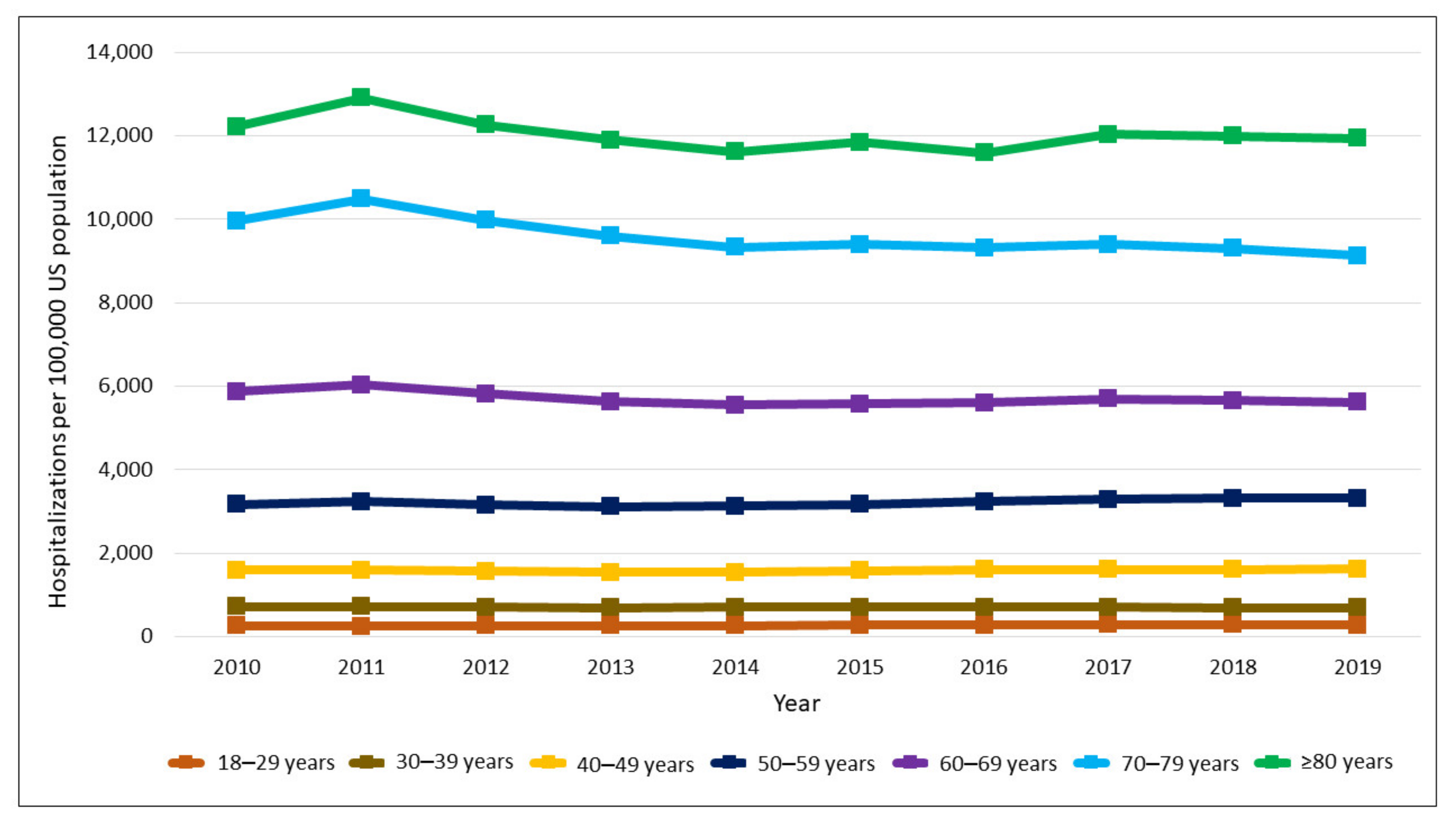
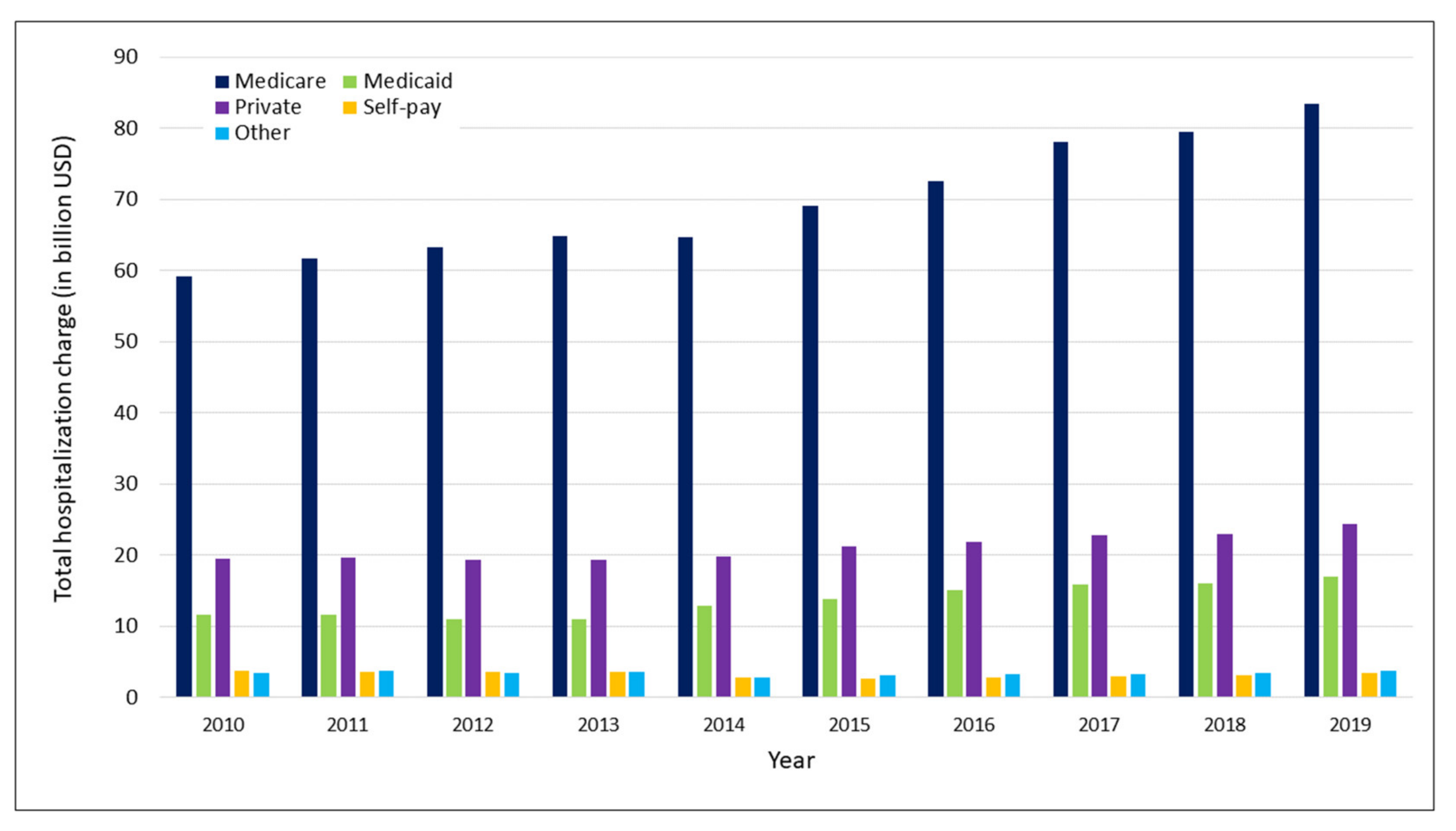
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Disease Control and Prevention (CDC). National and State Diabetes Trends. Diabetes Incidence and Prevalence. Available online: https://www.cdc.gov/diabetes/library/reports/reportcard/national-state-diabetes-trends.html#:~:text=Diabetes%20Incidence%20and%20Prevalence&text=About%2037.3%20million%20people%E2%80%94or,14.7%25%20of%20all%20US%20adults (accessed on 12 July 2022).
- Wang, L.; Li, X.; Wang, Z.; Bancks, M.P.; Carnethon, M.R.; Greenland, P.; Feng, Y.-Q.; Wang, H.; Zhong, V.W.; Greenland, P. Trends in prevalence of diabetes and control of risk factors in diabetes among US adults, 1999–2018. JAMA 2021, 326, 704–716. [Google Scholar] [CrossRef] [PubMed]
- Gregg, E.W.; Sattar, N.; Ali, M.K. The changing face of diabetes complications. Lancet Diabetes Endocrinol. 2016, 4, 537–547. [Google Scholar] [CrossRef]
- Association, A.D. Economic costs of diabetes in the US in 2017. Diabetes Care 2018, 41, 917–928. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-S.; Chang, C.-C.; Lee, Y.-W.; Liu, C.-C.; Yeh, C.-C.; Chang, Y.-C.; Chuang, M.-T.; Chang, T.-H.; Chen, T.-L.; Liao, C.-C. Adverse outcomes after major surgeries in patients with diabetes: A multicenter matched study. J. Clin. Med. 2019, 8, 100. [Google Scholar] [CrossRef] [PubMed]
- Nirantharakumar, K.; Hemming, K.; Narendran, P.; Marshall, T.; Coleman, J.J. A prediction model for adverse outcome in hospitalized patients with diabetes. Diabetes Care 2013, 36, 3566–3572. [Google Scholar] [CrossRef] [PubMed]
- Rubens, M.; Saxena, A.; Ramamoorthy, V.; Khera, R.; Hong, J.; Veledar, E.; Nasir, K. Trends in diabetes-related preventable hospitalizations in the US, 2005–2014. Diabetes Care 2018, 41, e72–e73. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.M.; Okumura, M.J.; Freed, G.L.; Menon, R.K.; Davis, M.M. Trends in hospitalizations for diabetes among children and young adults: United States, 1993–2004. Diabetes Care 2007, 30, 3035–3039. [Google Scholar] [CrossRef][Green Version]
- Lee, J.M.; Davis, M.M.; Gebremariam, A.; Kim, C. Age and sex differences in hospitalizations associated with diabetes. J. Women’s Health 2010, 19, 2033–2042. [Google Scholar] [CrossRef]
- Agency for Healthcare Research and Quality. National (Nationwide) Inpatient Sample (NIS) Database Documentation. Available online: https://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp (accessed on 25 June 2022).
- O’Connor, P.J.; Rush, W.A.; Pronk, N.P.; Cherney, L.M. Identifying diabetes mellitus or heart disease among health maintenance organization members: Sensitivity, specificity, predictive value, and cost of survey and database methods. Am. J. Manag. Care 1998, 4, 335–342. [Google Scholar]
- Agency for Healthcare Research and Quality. Checklist for Working with the NIS. Available online: https://www.hcup-us.ahrq.gov/db/nation/nis/nischecklist.jsp (accessed on 21 July 2022).
- United States Inflation Calculator. United States Consumer Price Index. Available online: https://www.usinflationcalculator.com/inflation/consumer-price-index-and-annual-percent-changes-from-1913-to-2008/ (accessed on 18 June 2022).
- Fang, M.; Wang, D.; Coresh, J.; Selvin, E. Trends in diabetes treatment and control in US adults, 1999–2018. N. Engl. J. Med. 2021, 384, 2219–2228. [Google Scholar] [CrossRef]
- Kazemian, P.; Shebl, F.M.; McCann, N.; Walensky, R.P.; Wexler, D.J. Evaluation of the cascade of diabetes care in the United States, 2005-2016. JAMA Intern. Med. 2019, 179, 1376–1385. [Google Scholar] [CrossRef] [PubMed]
- Group, A.C. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N. Engl. J. Med. 2008, 358, 2560–2572. [Google Scholar]
- Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive glucose lowering in type 2 diabetes. N. Engl. J. Med. 2008, 358, 2545–2559. [Google Scholar] [CrossRef]
- Duckworth, W.; Abraira, C.; Moritz, T.; Reda, D.; Emanuele, N.; Reaven, P.; Zieve, F.J.; Marks, J.; Davis, S.N.; Hayward, R.; et al. Glucose control and vascular complications in veterans with type 2 diabetes. N. Engl. J. Med. 2009, 360, 129–139. [Google Scholar] [CrossRef]
- Inzucchi, S.E.; Bergenstal, R.M.; Buse, J.B.; Diamant, M.; Ferrannini, E.; Nauck, M.; Peters, A.L.; Tsapas, A.; Wender, R.; Matthews, D.R. Management of hyperglycemia in type 2 diabetes: A patient-centered approach: Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2012, 35, 1364–1379. [Google Scholar] [CrossRef] [PubMed]
- Casagrande, S.S.; McEwen, L.N.; Herman, W.H. Changes in health insurance coverage under the Affordable Care Act: A national sample of US adults with diabetes, 2009 and 2016. Diabetes Care 2018, 41, 956–962. [Google Scholar] [CrossRef]
- Delevry, D.; Ho, A.; Le, Q.A. Association between processes of diabetes care and health care utilization in patients with diabetes: Evidence from a nationally representative US sample. J. Diabetes 2021, 13, 78–88. [Google Scholar] [CrossRef]
- Zhang, X.; Bullard, K.M.; Gregg, E.W.; Beckles, G.L.; Williams, D.E.; Barker, L.E.; Williams, D.E.; Barker, L.E.; Albright, A.L.; Imperatore, G. Access to health care and control of ABCs of diabetes. Diabetes Care 2012, 35, 1566–1571. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Diabetes Data and Statistics. Available online: https://www.cdc.gov/diabetes/data/index.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fdiabetes%2Fdata%2Findex.htm (accessed on 2 July 2022).
- Benoit, S.R.; Hora, I.; Pasquel, F.J.; Gregg, E.W.; Albright, A.L.; Imperatore, G. Trends in emergency department visits and inpatient admissions for hyperglycemic crises in adults with diabetes in the US, 2006–2015. Diabetes Care 2020, 43, 1057–1064. [Google Scholar] [CrossRef]
- Brierley, S.; Eiser, C.; Johnson, B.; Young, V.; Heller, S. Working with young adults with Type 1 diabetes: Views of a multidisciplinary care team and implications for service delivery. Diabetes Med. 2012, 29, 677–681. [Google Scholar] [CrossRef]
- Styles, E.; Kidney, R.S.; Carlin, C.; Peterson, K. Diabetes Treatment, Control, and Hospitalization Among Adults Aged 18 to 44 in Minnesota, 2013–2015. Prev. Chronic Dis. 2018, 15, E142. [Google Scholar] [CrossRef] [PubMed]
- Ness, M.M.; Saylor, J.L.; Ji, X.; Bell, A.; Habermann, B. Challenges experienced by parents of emerging young adults with type 1 diabetes mellitus during the transition to college. Diabetes Educator. 2020, 46, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Altman, D.; Frist, W.H. Medicare and Medicaid at 50 years: Perspectives of beneficiaries, health care professionals and institutions, and policy makers. JAMA 2015, 314, 384–395. [Google Scholar] [CrossRef]
- Kirkman, M.; Briscoe, V.; Clark, N.; Florez, H. Consensus development conference on diabetes and older adults. Diabetes in older adults: A consensus report. J. Am. Geriatr. Soc. 2012, 60, 2342–2356. [Google Scholar] [CrossRef] [PubMed]
| Variables | 2010 (n = 7,241,873) | 2019 (n = 8,373,830) | p Value |
|---|---|---|---|
| Age group, n (%) | <0.001 | ||
| 18–29 years | 135,882 (1.9%) | 151,790 (1.8%) | |
| 30–39 years | 290,512 (4.0%) | 308,500 (3.7%) | |
| 40–49 years | 692,250 (9.6%) | 652,305 (7.8%) | |
| 50–59 years | 1,334,476 (18.5%) | 1,403,455 (16.8%) | |
| 60–69 years | 1,731,351 (24.0%) | 2,136,320 (25.6%) | |
| 70–79 years | 1,659,355 (23.0%) | 2,161,665 (25.9%) | |
| ≥80 years | 1,380,572 (19.1%) | 1,541,200 (18.4%) | |
| Gender, n (%) | <0.001 | ||
| Males | 3,457,701 (47.8%) | 4,286,635 (51.2%) | |
| Females | 3,783,506 (52.2%) | 4,086,755 (48.8%) | |
| Race, n (%) | 0.433 | ||
| White | 4,108,081 (63.7%) | 5,181,249 (63.2%) | |
| Black | 1,247,733 (19.3%) | 1,493,565 (18.2%) | |
| Hispanic | 723,074 (11.2%) | 990,055 (12.1%) | |
| Asian or Pacific Islander | 152,989 (2.4%) | 238,210 (2.9%) | |
| Native American | 59,019 (0.9%) | 70,190 (0.9%) | |
| Other | 160,816 (2.5%) | 228,430 (2.8%) | |
| Insurance, n (%) | <0.001 | ||
| Medicare | 4,390,287 (60.2%) | 5,329,005 (63.3%) | |
| Medicaid | 835,050 (11.5%) | 1,094,935 (13.0%) | |
| Private | 1,512,996 (20.8%) | 1,486,175 (17.7%) | |
| Self-pay | 308,403 (4.2%) | 270,410 (3.2%) | |
| Other | 241,733 (3.3%) | 236,030 (2.8%) | |
| Income quartiles, n (%) | 0.542 | ||
| First quartile | 2,332,361 (33.1%) | 2,826,940 (34.3%) | |
| Second quartile | 1,876,330 (26.6%) | 2,154,509 (26.2%) | |
| Third quartile | 1,617,042 (22.9%) | 1,910,875 (23.2%) | |
| Fourth quartile | 1,223,970 (17.4%) | 1,340,491 (16.3%) | |
| Length of stay, median (IQR) | 3.1 (1.6–5.8) | 3.2 (1.6–6.0) | 0.526 |
| Diabetic retinopathy, n (%) | 731,429 (10.1%) | 820,635 (9.8%) | 0.072 |
| Diabetic nephropathy, n (%) | 1,636,663 (22.6%) | 1,758,504 (21.0%) | 0.085 |
| Diabetic neuropathy, n (%) | 1,911,854 (26.4%) | 2,152,074 (25.7%) | 0.092 |
| Lower-extremity amputations, n (%) | 79,660 (1.1%) | 83,738 (1.0%) | 0.081 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rubens, M.; Ramamoorthy, V.; Saxena, A.; McGranaghan, P.; McCormack-Granja, E. Recent Trends in Diabetes-Associated Hospitalizations in the United States. J. Clin. Med. 2022, 11, 6636. https://doi.org/10.3390/jcm11226636
Rubens M, Ramamoorthy V, Saxena A, McGranaghan P, McCormack-Granja E. Recent Trends in Diabetes-Associated Hospitalizations in the United States. Journal of Clinical Medicine. 2022; 11(22):6636. https://doi.org/10.3390/jcm11226636
Chicago/Turabian StyleRubens, Muni, Venkataraghavan Ramamoorthy, Anshul Saxena, Peter McGranaghan, and Elise McCormack-Granja. 2022. "Recent Trends in Diabetes-Associated Hospitalizations in the United States" Journal of Clinical Medicine 11, no. 22: 6636. https://doi.org/10.3390/jcm11226636
APA StyleRubens, M., Ramamoorthy, V., Saxena, A., McGranaghan, P., & McCormack-Granja, E. (2022). Recent Trends in Diabetes-Associated Hospitalizations in the United States. Journal of Clinical Medicine, 11(22), 6636. https://doi.org/10.3390/jcm11226636







