Impact of the COVID-19 Pandemic on Solid Organ Transplant and Rejection Episodes in Brazil’s Unified Healthcare System
Abstract
1. Introduction
2. Methods
2.1. Population
2.2. Data Retrieved
2.3. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cristelli, M.P.; Ferreira, G.F.; Medina-Pestana, J. Global Perspective on Kidney Transplantation: Brazil. Kidney360 2021, 2, 2016–2018. [Google Scholar] [CrossRef] [PubMed]
- DATASUS—Ministério Da Saúde. Available online: https://datasus.saude.gov.br/ (accessed on 21 July 2022).
- Saldanha, R.d.F.; Bastos, R.R.; Barcellos, C. Microdatasus: A package for downloading and preprocessing microdata from Brazilian Health Informatics Department (DATASUS). Cad. Saude Publica 2019, 35, e00032419. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro Junior, M.A.F.; Costa, C.T.K.; Néder, P.R.; Aveiro, I.D.A.; Elias, Y.G.B.; Augusto, S.D.S. Impact of COVID-19 on the Number of Transplants Performed in Brazil during the Pandemic. Current Situation. Rev. Col. Bras. Cir. 2021, 48, e20213042. [Google Scholar] [CrossRef] [PubMed]
- Requião-Moura, L.R.; Sandes-Freitas, T.V.; Viana, L.A.; Cristelli, M.P.; Andrade, L.G.M.; Garcia, V.D.; Oliveira, C.M.C.; Esmeraldo, R.M.; Abbud Filho, M.; Pacheco-Silva, A.; et al. High Mortality among Kidney Transplant Recipients Diagnosed with Coronavirus Disease 2019: Results from the Brazilian Multicenter Cohort Study. PLoS ONE 2021, 16, e0254822. [Google Scholar] [CrossRef] [PubMed]
- Cristelli, M.P.; Sandes-Freitas, T.V.; Viana, L.A.; Requião-Moura, L.R.; Andrade, L.G.M.; Tedesco-Silva, H.; Medina-Pestana, J. Migratory Pattern of the Coronavirus Disease 2019 and High Fatality Rates among Kidney Transplant Recipients: Report from the Brazilian Multicenter Cohort Study. Braz. J. Nephrol. 2021, 44, 3. [Google Scholar] [CrossRef] [PubMed]
- Bigoni, A.; Malik, A.M.; Tasca, R.; Carrera, M.B.M.; Schiesari, L.M.C.; Gambardella, D.D.; Massuda, A. Brazil’s Health System Functionality amidst of the COVID-19 Pandemic: An Analysis of Resilience. Lancet Reg. Health Am. 2022, 10, 100222. [Google Scholar] [CrossRef] [PubMed]
- Castro, M.C.; Massuda, A.; Almeida, G.; Menezes-Filho, N.A.; Andrade, M.V.; de Souza Noronha, K.V.M.; Rocha, R.; Macinko, J.; Hone, T.; Tasca, R.; et al. Brazil’s Unified Health System: The First 30 Years and Prospects for the Future. Lancet Lond. Engl. 2019, 394, 345–356. [Google Scholar] [CrossRef]
- Paim, J.; Travassos, C.; Almeida, C.; Bahia, L.; Macinko, J. The Brazilian Health System: History, Advances, and Challenges. Lancet Lond. Engl. 2011, 377, 1778–1797. [Google Scholar] [CrossRef]
- Estimates of Resident Population for Municipalities and Federation Units | IBGE. Available online: https://www.ibge.gov.br/en/statistics/social/population/18448-estimates-of-resident-population-for-municipalities-and-federation-units.html?=&t=resultados (accessed on 21 July 2022).
- Foresto, R.D.; Pestana, J.O.M.; Silva, H.T. Brasil: The Leading Public Kidney Transplant Program Worldwide. Rev. Assoc. Med. Bras. 2020, 66, 708–709. [Google Scholar] [CrossRef] [PubMed]
- Aubert, O.; Yoo, D.; Zielinski, D.; Cozzi, E.; Cardillo, M.; Dürr, M.; Domínguez-Gil, B.; Coll, E.; Da Silva, M.I.; Sallinen, V.; et al. COVID-19 Pandemic and Worldwide Organ Transplantation: A Population-Based Study. Lancet Public Health 2021, 6, e709–e719. [Google Scholar] [CrossRef]
- Nimmo, A.; Gardiner, D.; Ushiro-Lumb, I.; Ravanan, R.; Forsythe, J.L.R. The Global Impact of COVID-19 on Solid Organ Transplantation: Two Years Into a Pandemic. Transplantation 2022, 106, 1312–1329. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.; McAdams-DeMarco, M.A.; Massie, A.B.; Ahn, J.B.; Werbel, W.A.; Brennan, D.C.; Lentine, K.L.; Durand, C.M.; Segev, D.L. Early Changes in Kidney Transplant Immunosuppression Regimens During the COVID-19 Pandemic. Transplantation 2021, 105, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Moynihan, R.; Sanders, S.; Michaleff, Z.A.; Scott, A.M.; Clark, J.; To, E.J.; Jones, M.; Kitchener, E.; Fox, M.; Johansson, M.; et al. Impact of COVID-19 Pandemic on Utilisation of Healthcare Services: A Systematic Review. BMJ Open 2021, 11, e045343. [Google Scholar] [CrossRef] [PubMed]
- Aziz, F.; Muth, B.; Parajuli, S.; Garg, N.; Mohamed, M.; Mandelbrot, D.; Djamali, A. Unusually High Rates of Acute Rejection during the COVID-19 Pandemic: Cause for Concern? Kidney Int. 2020, 98, 513–514. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Lauber, C.; Spoden, M.; Huber, T.B.; Günster, C.; Grahammer, F. Increased Rejection Rates in Kidney Transplantations during the COVID-19 Pandemic. Transpl. Int. 2021, 34, 2899–2902. [Google Scholar] [CrossRef] [PubMed]
- Vásquez-Jiménez, E.; Moguel-González, B.; Soto-Abraham, V.; Flores-Gama, C. Risk of Acute Rejection in Kidney Transplant Recipients after COVID-19. J. Nephrol. 2022, 35, 367–369. [Google Scholar] [CrossRef] [PubMed]
- Imprensa Oficial. Available online: http://www.imprensaoficial.com.br/. (accessed on 21 July 2022).
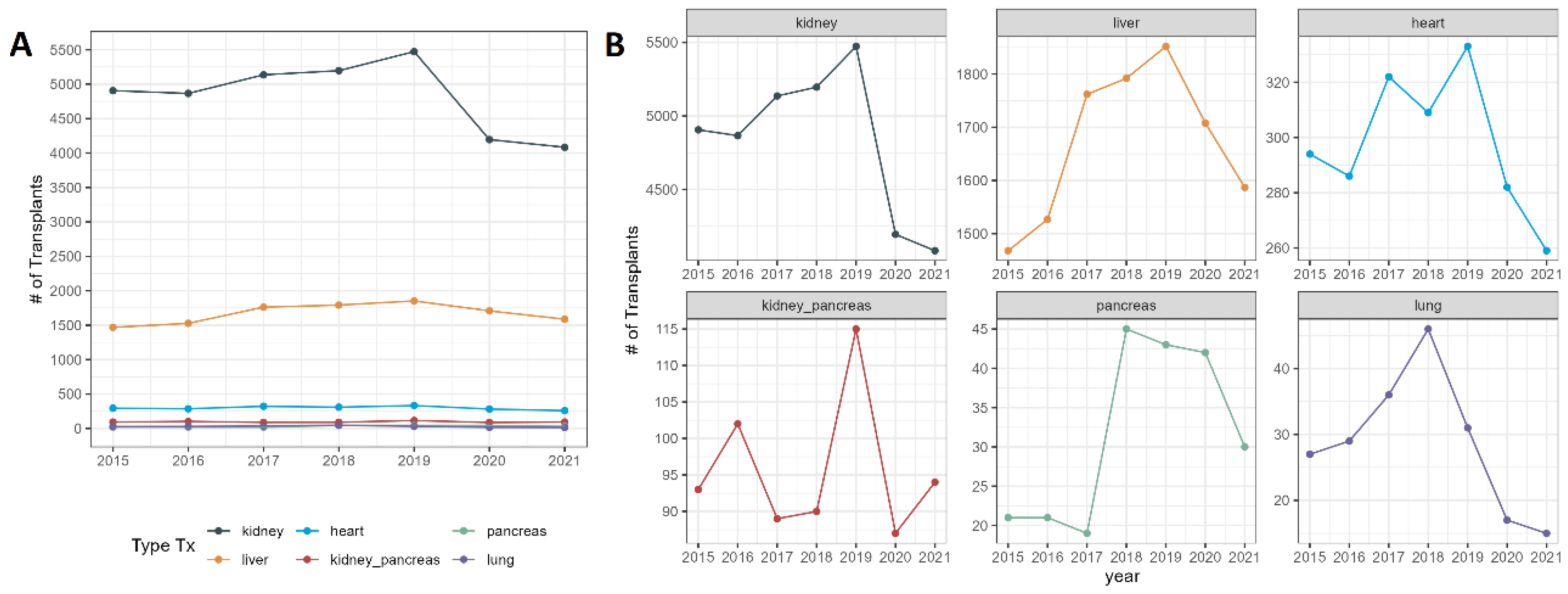

| Characteristic | 2015, n = 6809 | 2016, n = 6831 | 2017, n = 7364 | 2018, n = 7478 | 2019, n = 7847 | 2020, n = 6331 | 2021, n = 6069 |
|---|---|---|---|---|---|---|---|
| Organ, n (%) | |||||||
| Kidney | 4906 (72) | 4866 (71) | 5136 (70) | 5196 (69) | 5473 (70) | 4195 (66) | 4084 (67) |
| Reduction * | - | - | - | - | - | 23.3% | 25.4% |
| Liver | 1468 (22) | 1527 (22) | 1762 (24) | 1792 (24) | 1852 (24) | 1708 (27) | 1587 (26) |
| Reduction * | - | - | - | - | - | 7.7% | 14.3% |
| Heart | 294 (4.3) | 286 (4.2) | 322 (4.4) | 309 (4.1) | 333 (4.2) | 282 (4.5) | 259 (4.3) |
| Reduction * | - | - | - | - | - | 15.3% | 22.2% |
| Kidney–pancreas | 93 (1.4) | 102 (1.5) | 89 (1.2) | 90 (1.2) | 115 (1.5) | 87 (1.4) | 94 (1.5) |
| Reduction * | - | - | - | - | - | 24.3% | 18.2% |
| Pancreas | 21 (0.3) | 21 (0.3) | 19 (0.3) | 45 (0.6) | 43 (0.5) | 42 (0.7) | 30 (0.5) |
| Reduction * | - | - | - | - | - | 2.3% | 30.2% |
| Lung | 27 (0.4) | 29 (0.4) | 36 (0.5) | 46 (0.6) | 31 (0.4) | 17 (0.3) | 15 (0.2) |
| Reduction * | - | - | - | - | - | 45% | 51.6% |
| Characteristic | Overall n = 48,729 | Pre-Pandemic n = 38,429 | COVID-19 n = 10,300 | p-Value |
|---|---|---|---|---|
| Age (years), Median (IQR) | 49 (36–58) | 49 (36–58) | 49 (37–59) | 0.066 |
| Sex, n (%) | 0.077 | |||
| Female | 18,280 (38) | 14,339 (37) | 3941 (38) | |
| Male | 30,449 (62) | 24,090 (63) | 6359 (62) | |
| Race, n (%) | 0.522 | |||
| White | 23,066 (57) | 18,364 (58) | 4702 (54) | |
| Black | 4008 (9.9) | 2913 (9.2) | 1095 (12) | |
| Mixed | 12,794 (32) | 9897 (31) | 2897 (33) | |
| Asian | 591 (1.5) | 518 (1.6) | 73 (0.8) | |
| Indigenous | 6 (<0.1) | 4 (<0.1) | 2 (<0.1) | |
| Not identified | 8264 | 6733 | 1531 | |
| Tx Organ, n (%) | <0.001 | |||
| Kidney | 33,856 (69) | 26,987 (70) | 6869 (67) | |
| Liver | 11,696 (24) | 8942 (23) | 2754 (27) | |
| Heart | 2085 (4.3) | 1637 (4.3) | 448 (4.3) | |
| Kidney–pancreas | 670 (1.4) | 512 (1.3) | 158 (1.5) | |
| Pancreas | 221 (0.5) | 170 (0.4) | 51 (0.5) | |
| Lung | 201 (0.4) | 181 (0.5) | 20 (0.2) | |
| Length of Stay (days), Median (IQR) | 10 (7–13) | 10 (7–13) | 9 (7–12) | <0.001 |
| Death, n (%) | 2121 (4.4) | 1677 (4.4) | 444 (4.3) | 0.81 |
| Region | 2015, n = 6809 | 2016, n = 6831 | 2017, n = 7364 | 2018, n = 7478 | 2019, n = 7847 | 2020, n = 6331 | 2021, n = 6069 |
|---|---|---|---|---|---|---|---|
| Midwest | 218 | 248 | 290 | 440 | 465 | 424 | 409 |
| Reduction * | - | - | - | - | - | 8.8% | 12% |
| North | 165 | 188 | 173 | 188 | 230 | 121 | 137 |
| Reduction * | - | - | - | - | - | 47.3% | 40.4% |
| Northeast | 1313 | 1232 | 1422 | 1492 | 1557 | 1032 | 1165 |
| Reduction * | - | - | - | - | - | 33.7% | 25.2% |
| South | 1629 | 1872 | 1899 | 1924 | 1798 | 1464 | 1192 |
| Reduction * | - | - | - | - | - | 18.5% | 33.7% |
| Southeast | 3418 | 3172 | 3474 | 3434 | 3797 | 3290 | 3166 |
| Reduction * | - | - | - | - | - | 13.5% | 16.6% |
| Characteristic | Overall, n = 21,339 | Pre-Pandemic, n = 16,576 | COVID-19, n = 4763 | p-Value |
|---|---|---|---|---|
| Age (years), Median (IQR) | 46 (31–58) | 46 (32–58) | 45 (30–57) | 0.006 |
| Sex, n (%) | ||||
| Female | 8464 (40) | 6570 (40) | 1894 (40) | 0.87 |
| Male | 12,875 (60) | 10,006 (60) | 2869 (60) | |
| Race, n (%) | ||||
| White | 11,694 (68) | 9126 (69) | 2568 (64) | 0.435 |
| Black | 1287 (7.5) | 928 (7.1) | 359 (8.9) | |
| Mixed | 3998 (23) | 2946 (22) | 1052 (26) | |
| Asian | 198 (1.2) | 154 (1.2) | 44 (1.1) | |
| Indigenous | 2 (<0.1) | 2 (<0.1) | 0 (0) | |
| Not identified | 4160 | 3420 | 740 | |
| Type Rejection, n (%) | <0.001 | |||
| Rejection kidney | 13,424 (63) | 10,452 (63) | 2972 (62) | |
| Rejection liver | 5128 (24) | 3901 (24) | 1227 (26) | |
| Rejection heart | 2326 (11) | 1835 (11) | 491 (10) | |
| Rejection heart–lung | 63 (0.3) | 56 (0.3) | 7 (0.1) | |
| Rejection pancreas | 244 (1.1) | 193 (1.2) | 51 (1.1) | |
| Rejection lung | 154 (0.7) | 139 (0.8) | 15 (0.3) | |
| Length of stay (days), Median (IQR) | 6 (2–12) | 6 (3–12) | 5 (2–11) | <0.001 |
| Death, n (%) | 673 (3.2) | 491 (3.0) | 182 (3.8) | 0.003 |
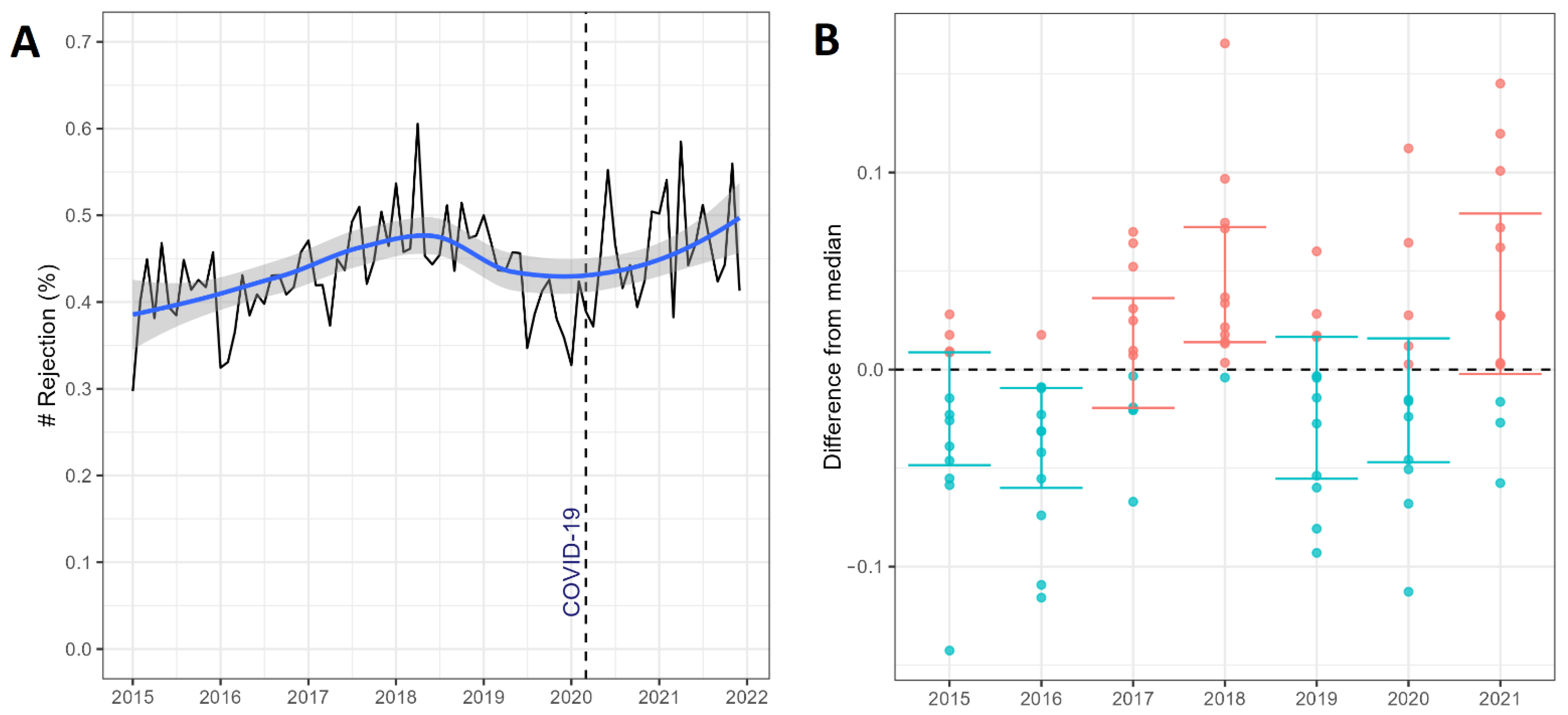
| Rejection * | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 |
|---|---|---|---|---|---|---|---|
| Prop, Median (IQR) | 0.42 (0.39–0.45) | 0.41 (0.38–0.43) | 0.45 (0.42–0.48) | 0.47 (0.45–0.51) | 0.43 (0.38–0.46) | 0.42 (0.39–0.46) | 0.47 (0.44–0.52) |
| Characteristic | IRR (95% CI) | p-Value |
|---|---|---|
| 2015 year (Reference) | ||
| 2016 | 0.97 (0.88 to 1.06) | 0.51 |
| 2017 | 1.10 (1.00 to 1.20) | 0.051 |
| 2018 | 1.18 (1.08 to 1.29) | <0.001 |
| 2019 | 1.03 (0.94 to 1.12) | 0.59 |
| 2020 | 0.92 (0.79 to 1.07) | 0.30 |
| 2021 | 0.99 (0.83 to 1.18) | 0.89 |
| Reference pre-pandemic | ||
| COVID-19 pandemic | 1.18 (1.01 to 1.37) | 0.040 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Andrade, L.G.M.; Barbosa, A.M.P.; da Rocha, N.C.; de Almeida Cardoso, M.M.; de Almeida, J.T.C.; Machado-Rugolo, J.; Arantes, L.F.; Pontes, D.F.S.; Ferreira, G.F. Impact of the COVID-19 Pandemic on Solid Organ Transplant and Rejection Episodes in Brazil’s Unified Healthcare System. J. Clin. Med. 2022, 11, 6581. https://doi.org/10.3390/jcm11216581
de Andrade LGM, Barbosa AMP, da Rocha NC, de Almeida Cardoso MM, de Almeida JTC, Machado-Rugolo J, Arantes LF, Pontes DFS, Ferreira GF. Impact of the COVID-19 Pandemic on Solid Organ Transplant and Rejection Episodes in Brazil’s Unified Healthcare System. Journal of Clinical Medicine. 2022; 11(21):6581. https://doi.org/10.3390/jcm11216581
Chicago/Turabian Stylede Andrade, Luis Gustavo Modelli, Abner Macola Pacheco Barbosa, Naila Camila da Rocha, Marilia Mastrocolla de Almeida Cardoso, Juliana Tereza Coneglian de Almeida, Juliana Machado-Rugolo, Lucas Frederico Arantes, Daniela Ferreira Salomão Pontes, and Gustavo Fernandes Ferreira. 2022. "Impact of the COVID-19 Pandemic on Solid Organ Transplant and Rejection Episodes in Brazil’s Unified Healthcare System" Journal of Clinical Medicine 11, no. 21: 6581. https://doi.org/10.3390/jcm11216581
APA Stylede Andrade, L. G. M., Barbosa, A. M. P., da Rocha, N. C., de Almeida Cardoso, M. M., de Almeida, J. T. C., Machado-Rugolo, J., Arantes, L. F., Pontes, D. F. S., & Ferreira, G. F. (2022). Impact of the COVID-19 Pandemic on Solid Organ Transplant and Rejection Episodes in Brazil’s Unified Healthcare System. Journal of Clinical Medicine, 11(21), 6581. https://doi.org/10.3390/jcm11216581






