Bone Metastases of Diverse Primary Origin Frequently Express the VDR (Vitamin D Receptor) and CYP24A1
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Collection
2.2. Sample Processing
2.3. Immunohistochemistry (IHC)
2.4. Evaluation
2.5. Statistical Evaluation/Data Analysis
3. Results
3.1. Baseline Characteristics of Participants
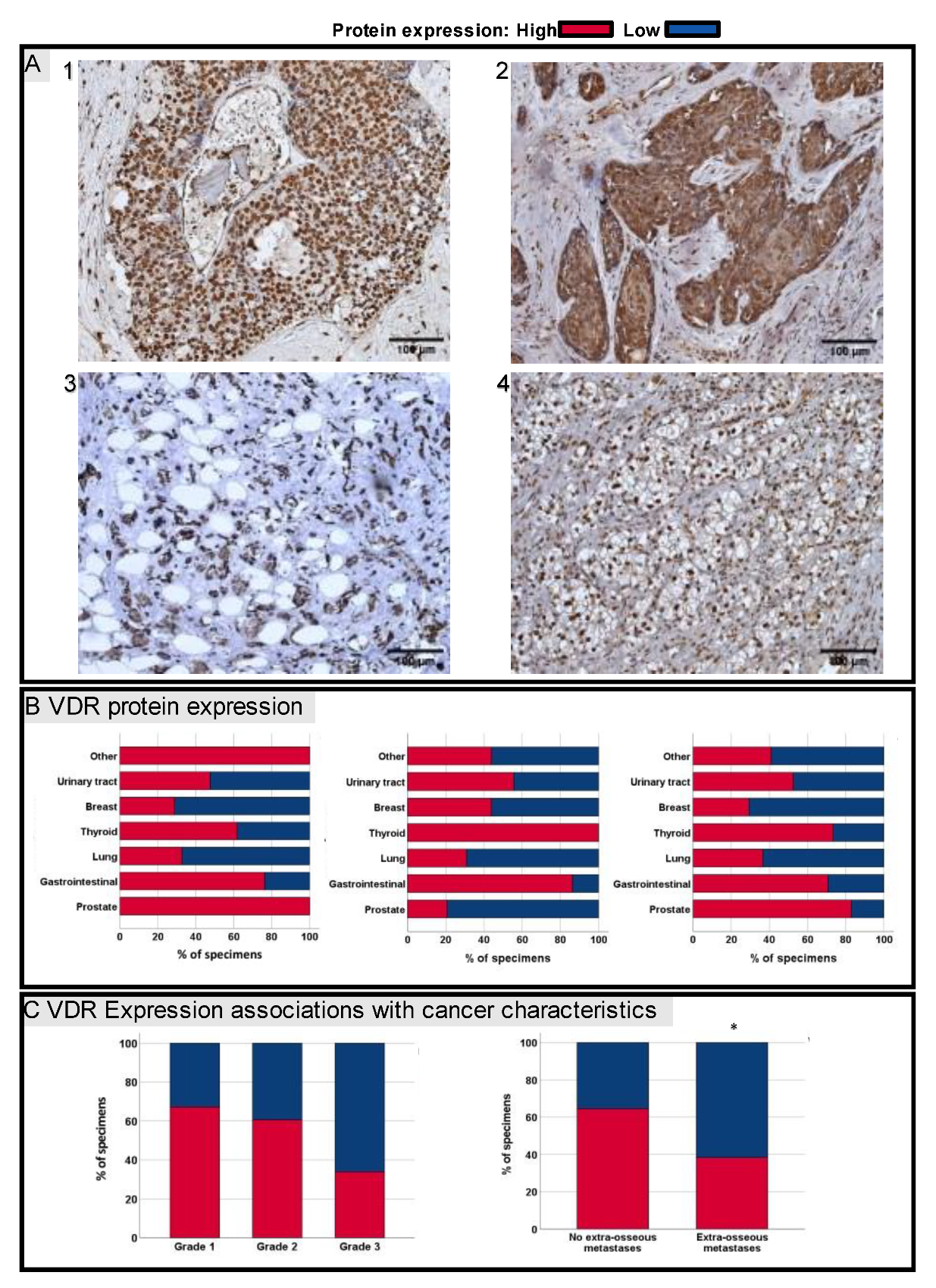
3.2. VDR Protein Expression in Bone Metastases
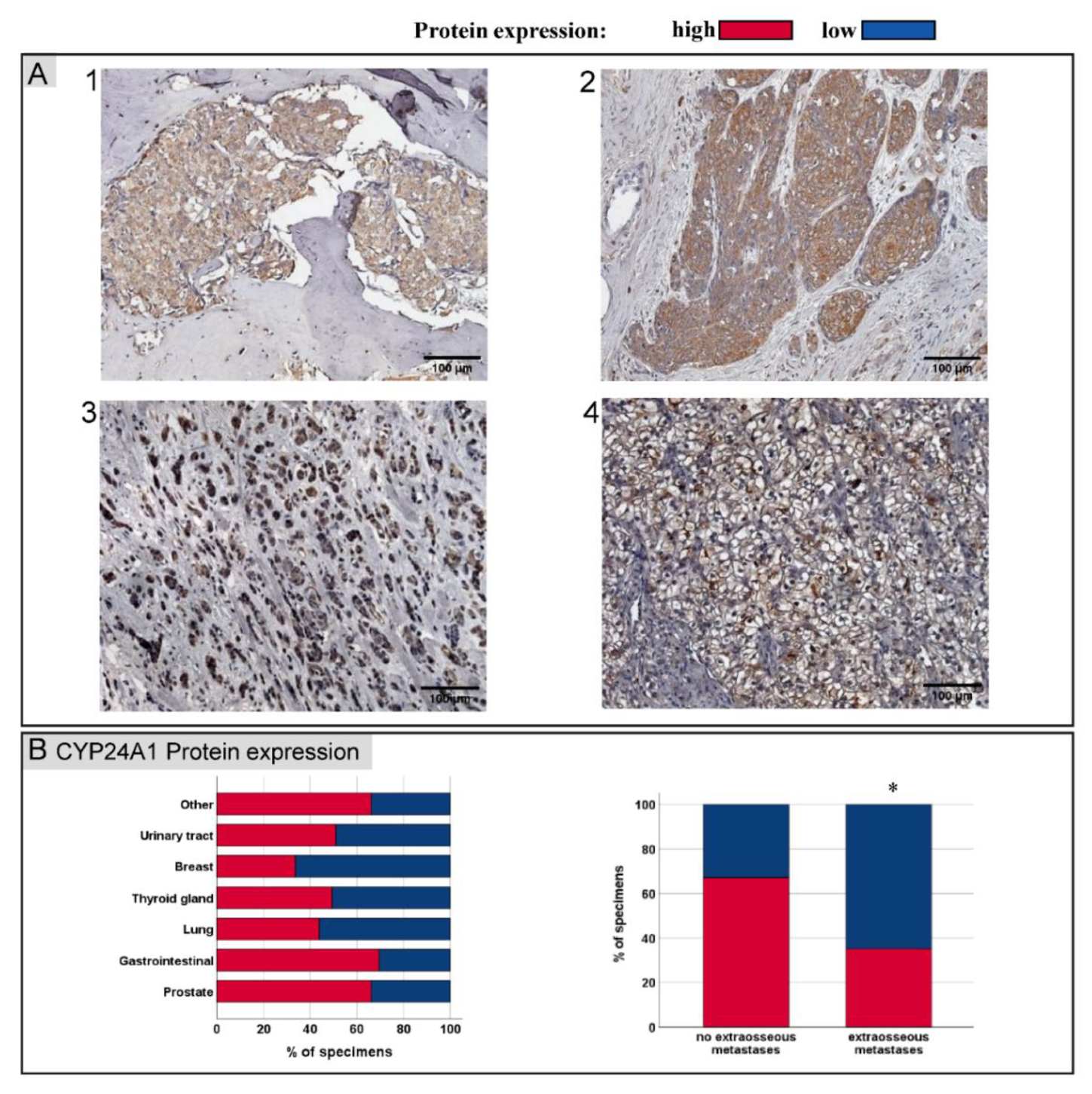
3.3. CYP24A1 Protein Expression in Bone Metastases
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Coleman, R.E.; Croucher, P.I.; Padhani, A.R.; Clezardin, P.; Chow, E.; Fallon, M.; Guise, T.; Colangeli, S.; Capanna, R.; Costa, L. Bone metastases. Nat. Rev. Dis. Prim. 2020, 6, 83. [Google Scholar] [CrossRef] [PubMed]
- Coleman, R.E. Clinical Features of Metastatic Bone Disease and Risk of Skeletal Morbidity. Clin. Cancer Res. 2006, 12, 6243s–6249s. [Google Scholar] [CrossRef] [PubMed]
- Yong, M.; Jensen, A.; Jacobsen, J.B.; Nørgaard, M.; Fryzek, J.P.; Sørensen, H.T. Survival in breast cancer patients with bone metastases and skeletal-related events: A population-based cohort study in Denmark (1999–2007). Breast Cancer Res. Treat. 2011, 129, 495–503. [Google Scholar] [CrossRef]
- Feldman, D.; Krishnan, A.V.; Swami, S.; Giovannucci, E.; Feldman, B.J. The role of vitamin D in reducing cancer risk and progression. Nat. Rev. Cancer 2014, 14, 342–357. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, A.V.; Trump, D.L.; Johnson, C.S.; Feldman, D. The role of vitamin D in cancer prevention and treatment. Endocrinol. Metab. Clin. N. Am. 2010, 39, 401–418, table of contents. [Google Scholar] [CrossRef]
- Spina, C.S.; Tangpricha, V.; Uskokovic, M.; Adorinic, L.; Maehr, H.; Holick, M.F. Vitamin D and cancer. Anticancer Res. 2006, 26, 2515–2524. [Google Scholar]
- Kim, Y.; Je, Y. Vitamin D intake, blood 25(OH)D levels, and breast cancer risk or mortality: A meta-analysis. Br. J. Cancer 2014, 110, 2772–2784. [Google Scholar] [CrossRef]
- Li, C.; Li, H.; Zhong, H.; Li, X. Association of 25-hydroxyvitamin D level with survival outcomes in female breast cancer patients: A meta-analysis. J. Steroid Biochem. Mol. Biol. 2021, 212, 105947. [Google Scholar] [CrossRef]
- Chandler, P.D.; Chen, W.Y.; Ajala, O.N.; Hazra, A.; Cook, N.; Bubes, V.; Lee, I.M.; Giovannucci, E.L.; Willett, W.; Buring, J.E.; et al. Effect of Vitamin D3 Supplements on Development of Advanced Cancer: A Secondary Analysis of the VITAL Randomized Clinical Trial. JAMA Netw. Open 2020, 3, e2025850. [Google Scholar] [CrossRef]
- Ooi, L.L.; Zhou, H.; Kalak, R.; Zheng, Y.; Conigrave, A.D.; Seibel, M.J.; Dunstan, C.R. Vitamin D deficiency promotes human breast cancer growth in a murine model of bone metastasis. Cancer Res. 2010, 70, 1835–1844. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Zhou, H.; Ooi, L.L.; Snir, A.D.; Dunstan, C.R.; Seibel, M.J. Vitamin D deficiency promotes prostate cancer growth in bone. Prostate 2011, 71, 1012–1021. [Google Scholar] [CrossRef] [PubMed]
- Ooi, L.L.; Zheng, Y.; Zhou, H.; Trivedi, T.; Conigrave, A.D.; Seibel, M.J.; Dunstan, C.R. Vitamin D deficiency promotes growth of MCF-7 human breast cancer in a rodent model of osteosclerotic bone metastasis. Bone 2010, 47, 795–803. [Google Scholar] [CrossRef]
- Zheng, Y.; Zhou, H.; Dunstan, C.R.; Sutherland, R.L.; Seibel, M.J. The role of the bone microenvironment in skeletal metastasis. J. Bone Oncol. 2013, 2, 47–57. [Google Scholar] [CrossRef] [PubMed]
- Skowronski, R.J.; Peehl, D.M.; Feldman, D. Vitamin D and prostate cancer: 1,25 dihydroxyvitamin D3 receptors and actions in human prostate cancer cell lines. Endocrinology 1993, 132, 1952–1960. [Google Scholar] [CrossRef] [PubMed]
- Higashimoto, Y.; Ohata, M.; Nishio, K.; Iwamoto, Y.; Fujimoto, H.; Uetani, K.; Suruda, T.; Nakamura, Y.; Funasako, M.; Saijo, N. 1 alpha, 25-dihydroxyvitamin D3 and all-trans-retinoic acid inhibit the growth of a lung cancer cell line. Anticancer Res. 1996, 16, 2653–2659. [Google Scholar] [PubMed]
- Trivedi, T.; Zheng, Y.; Fournier, P.G.J.; Murthy, S.; John, S.; Schillo, S.; Dunstan, C.R.; Mohammad, K.S.; Zhou, H.; Seibel, M.J.; et al. The vitamin D receptor is involved in the regulation of human breast cancer cell growth via a ligand-independent function in cytoplasm. Oncotarget 2017, 8, 26687–26701. [Google Scholar] [CrossRef]
- Horas, K.; Zheng, Y.; Fong-Yee, C.; Macfarlane, E.; Manibo, J.; Chen, Y.; Qiao, J.; Gao, M.; Haydar, N.; McDonald, M.M.; et al. Loss of the Vitamin D Receptor in Human Breast Cancer Cells Promotes Epithelial to Mesenchymal Cell Transition and Skeletal Colonization. J. Bone Miner. Res. 2019, 34, 1721–1732. [Google Scholar] [CrossRef]
- Zheng, Y.; Trivedi, T.; Lin, R.C.; Fong-Yee, C.; Nolte, R.; Manibo, J.; Chen, Y.; Hossain, M.; Horas, K.; Dunstan, C.; et al. Loss of the vitamin D receptor in human breast and prostate cancers strongly induces cell apoptosis through downregulation of Wnt/β-catenin signaling. Bone Res. 2017, 5, 17023. [Google Scholar] [CrossRef]
- Podgorska, E.; Kim, T.K.; Janjetovic, Z.; Urbanska, K.; Tuckey, R.C.; Bae, S.; Slominski, A.T. Knocking out the Vitamin D Receptor Enhances Malignancy and Decreases Responsiveness to Vitamin D3 Hydroxyderivatives in Human Melanoma Cells. Cancers 2021, 13, 3111. [Google Scholar] [CrossRef]
- Shi, Q.; Han, X.P.; Yu, J.; Peng, H.; Chen, Y.Z.; Li, F.; Cui, X.B. Decreased vitamin D receptor protein expression is associated with progression and poor prognosis of colorectal cancer patients. Int. J. Clin. Exp. Pathol. 2020, 13, 746–755. [Google Scholar] [PubMed]
- Jóźwicki, W.; Brożyna, A.A.; Siekiera, J.; Slominski, A.T. Expression of Vitamin D Receptor (VDR) Positively Correlates with Survival of Urothelial Bladder Cancer Patients. Int. J. Mol. Sci. 2015, 16, 24369–24386. [Google Scholar] [CrossRef]
- Wang, K.; Dong, M.; Sheng, W.; Liu, Q.; Yu, D.; Dong, Q.; Li, Q.; Wang, J. Expression of vitamin D receptor as a potential prognostic factor and therapeutic target in pancreatic cancer. Histopathology 2015, 67, 386–397. [Google Scholar] [CrossRef] [PubMed]
- Huss, L.; Butt, S.T.; Borgquist, S.; Elebro, K.; Sandsveden, M.; Rosendahl, A.; Manjer, J. Vitamin D receptor expression in invasive breast tumors and breast cancer survival. Breast Cancer Res. BCR 2019, 21, 84. [Google Scholar] [CrossRef] [PubMed]
- Hendrickson, W.K.; Flavin, R.; Kasperzyk, J.L.; Fiorentino, M.; Fang, F.; Lis, R.; Fiore, C.; Penney, K.L.; Ma, J.; Kantoff, P.W.; et al. Vitamin D receptor protein expression in tumor tissue and prostate cancer progression. J. Clin. Oncol. 2011, 29, 2378–2385. [Google Scholar] [CrossRef] [PubMed]
- Al-Azhri, J.; Zhang, Y.; Bshara, W.; Zirpoli, G.; McCann, S.E.; Khoury, T.; Morrison, C.D.; Edge, S.B.; Ambrosone, C.B.; Yao, S. Tumor Expression of Vitamin D Receptor and Breast Cancer Histopathological Characteristics and Prognosis. Clin. Cancer Res. 2017, 23, 97–103. [Google Scholar] [CrossRef]
- Christakos, S.; Dhawan, P.; Verstuyf, A.; Verlinden, L.; Carmeliet, G. Vitamin D: Metabolism, Molecular Mechanism of Action, and Pleiotropic Effects. Physiol. Rev. 2016, 96, 365–408. [Google Scholar] [CrossRef]
- Tannour-Louet, M.; Lewis, S.K.; Louet, J.F.; Stewart, J.; Addai, J.B.; Sahin, A.; Vangapandu, H.V.; Lewis, A.L.; Dittmar, K.; Pautler, R.G.; et al. Increased expression of CYP24A1 correlates with advanced stages of prostate cancer and can cause resistance to vitamin D3-based therapies. FASEB J. 2014, 28, 364–372. [Google Scholar] [CrossRef]
- Parise, R.A.; Egorin, M.J.; Kanterewicz, B.; Taimi, M.; Petkovich, M.; Lew, A.M.; Chuang, S.S.; Nichols, M.; El-Hefnawy, T.; Hershberger, P.A. CYP24, the enzyme that catabolizes the antiproliferative agent vitamin D, is increased in lung cancer. Int. J. Cancer 2006, 119, 1819–1828. [Google Scholar] [CrossRef]
- Sun, H.; Wang, C.; Hao, M.; Sun, R.; Wang, Y.; Liu, T.; Cong, X.; Liu, Y. CYP24A1 is a potential biomarker for the progression and prognosis of human colorectal cancer. Hum. Pathol. 2016, 50, 101–108. [Google Scholar] [CrossRef]
- Höbaus, J.; Tennakoon, S.; Heffeter, P.; Groeschel, C.; Aggarwal, A.; Hummel, D.M.; Thiem, U.; Marculescu, R.; Berger, W.; Kállay, E. Impact of CYP24A1 overexpression on growth of colorectal tumour xenografts in mice fed with vitamin D and soy. Int. J. Cancer 2016, 138, 440–450. [Google Scholar] [CrossRef] [PubMed]
- Osanai, M.; Lee, G.H. CYP24A1-induced vitamin D insufficiency promotes breast cancer growth. Oncol. Rep. 2016, 36, 2755–2762. [Google Scholar] [CrossRef] [PubMed]
- Hu, N.; Zhang, H. CYP24A1 depletion facilitates the antitumor effect of vitamin D3 on thyroid cancer cells. Exp. Med. 2018, 16, 2821–2830. [Google Scholar] [CrossRef]
- Muindi, J.R.; Yu, W.-D.; Ma, Y.; Engler, K.L.; Kong, R.-X.; Trump, D.L.; Johnson, C.S. CYP24A1 inhibition enhances the antitumor activity of calcitriol. Endocrinology 2010, 151, 4301–4312. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhu, J.; DeLuca, H.F. Where is the vitamin D receptor? Arch. Biochem. Biophys. 2012, 523, 123–133. [Google Scholar] [CrossRef]
- Anderson, M.G.; Nakane, M.; Ruan, X.; Kroeger, P.E.; Wu-Wong, J.R. Expression of VDR and CYP24A1 mRNA in human tumors. Cancer Chemother. Pharmacol. 2006, 57, 234–240. [Google Scholar] [CrossRef]
- Campolina-Silva, G.H.; Maria, B.T.; Mahecha, G.A.B.; Oliveira, C.A. Reduced vitamin D receptor (VDR) expression and plasma vitamin D levels are associated with aging-related prostate lesions. Prostate 2018, 78, 532–546. [Google Scholar] [CrossRef]
- Lopes, N.; Sousa, B.; Martins, D.; Gomes, M.; Vieira, D.; Veronese, L.A.; Milanezi, F.; Paredes, J.; Costa, J.L.; Schmitt, F. Alterations in Vitamin D signalling and metabolic pathways in breast cancer progression: A study of VDR, CYP27B1 and CYP24A1 expression in benign and malignant breast lesions. BMC Cancer 2010, 10, 483. [Google Scholar] [CrossRef]
- Šutalo, N.; Tomić, S.; Bevanda, M.; Dragišić, V.; Marijanović, I.; Petričević, J.; Mikulić, I. Immunohystochemical Expression of Vitamin D Receptor in Development Stages of Colorectal Carcinoma. Psychiatr Danub 2017, 29 (Suppl. S4), 855–858. [Google Scholar]
- Srinivasan, M.; Parwani, A.V.; Hershberger, P.A.; Lenzner, D.E.; Weissfeld, J.L. Nuclear vitamin D receptor expression is associated with improved survival in non-small cell lung cancer. J. Steroid Biochem. Mol. Biol. 2011, 123, 30–36. [Google Scholar] [CrossRef]
- Ding, P.; Du, X.; Wan, L.; Zhao, X.; Zhang, D.; Huang, Z.; Cao, G.; Zhou, X.; Zheng, Y.; Cao, Y. Diagnostic Value of VDR in Bone Metastasis and Prognosis of Patients with Breast Cancer and Expression Correlation between Vitamin D Receptor and Hairless Protein. Oncol. Res. Treat. 2022, 45, 166–177. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Guo, Q.; Zhang, Z.; Bai, N.; Liu, Z.; Xiong, M.; Wei, Y.; Xiang, R.; Tan, X. VDR status arbitrates the prometastatic effects of tumor-associated macrophages. Mol. Cancer Res. 2014, 12, 1181–1191. [Google Scholar] [CrossRef] [PubMed]
- Yuan, L.; Jiang, R.; Yang, Y.; Ding, S.; Deng, H. 1,25-Dihydroxyvitamin D3 inhibits growth of the breast cancer cell line MCF-7 and downregulates cytochrome P4501B1 through the COX-2/PGE2 pathway. Oncol. Rep. 2012, 28, 2131–2137. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Liu, X.; Zhang, F.; Liao, S.; He, X.; Zhuo, D.; Huang, H.; Wu, Y. Vitamin D receptor suppresses proliferation and metastasis in renal cell carcinoma cell lines via regulating the expression of the epithelial Ca2+ channel TRPV5. PLoS ONE 2018, 13, e0195844. [Google Scholar] [CrossRef] [PubMed]
- Bennett, R.G.; Wakeley, S.E.; Hamel, F.G.; High, R.R.; Korch, C.; Goldner, W.S. Gene expression of vitamin D metabolic enzymes at baseline and in response to vitamin D treatment in thyroid cancer cell lines. Oncology 2012, 83, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Zinser, G.M.; McEleney, K.; Welsh, J. Characterization of mammary tumor cell lines from wild type and vitamin D3 receptor knockout mice. Mol. Cell. Endocrinol. 2003, 200, 67–80. [Google Scholar] [CrossRef]
- Maier, G.S.; Horas, K.; Kurth, A.A.; Lazovic, D.; Seeger, J.B.; Maus, U. Prevalence of Vitamin D Deficiency in Patients with Bone Metastases and Multiple Myeloma. Anticancer Res. 2015, 35, 6281–6285. [Google Scholar]
- Hofbauer, L.C.; Rachner, T.D.; Coleman, R.E.; Jakob, F. Endocrine aspects of bone metastases. Lancet. Diabetes Endocrinol. 2014, 2, 500–512. [Google Scholar] [CrossRef]
- Manson, J.E.; Cook, N.R.; Lee, I.M.; Christen, W.; Bassuk, S.S.; Mora, S.; Gibson, H.; Gordon, D.; Copeland, T.; D’Agostino, D.; et al. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. N. Engl. J. Med. 2019, 380, 33–44. [Google Scholar] [CrossRef]
- Chen, G.; Kim, S.H.; King, A.N.; Zhao, L.; Simpson, R.U.; Christensen, P.J.; Wang, Z.; Thomas, D.G.; Giordano, T.J.; Lin, L.; et al. CYP24A1 is an independent prognostic marker of survival in patients with lung adenocarcinoma. Clin. Cancer Res. 2011, 17, 817–826. [Google Scholar] [CrossRef]
- Cai, H.; Jiao, Y.; Li, Y.; Yang, Z.; He, M.; Liu, Y. Low CYP24A1 mRNA expression and its role in prognosis of breast cancer. Sci. Rep. 2019, 9, 13714. [Google Scholar] [CrossRef] [PubMed]
| Primary Cancer | T-Stage | N-Stage | Grading | |||||
|---|---|---|---|---|---|---|---|---|
| n | 1 to 2 | 3 to 4 | N0 | N+ | G1 | G2 | G3 | |
| Breast | 16 | 10 (62.5) | 6 (37.5) | 5 (31.3) | 11 (68.7) | 2 (12.5) | 6 (37.5) | 8 (50.0) |
| Urinary tract | 13 | 3 (27.3) | 8 (62.7) | 4 (50.0) | 4 (50.0) | 2 (15.4) | 7 (53.8) | 4 (30.7) |
| Lung | 11 | 1 (12.5) | 7 (87.5) | 2 (22.2) | 7 (77.7) | 0 (0) | 5 (45.5) | 6 (54.5) |
| Gastro-intestinal | 9 | 2 (25.0) | 6 (75.0) | 2 (25.0) | 6 (75.0) | 0 (0) | 8 (88.9) | 1 (11.1) |
| Prostate | 8 | 2 (50.0) | 2 (50.0) | 2 (40.0) | 3 (60.0) | Not applied | ||
| Thyroid cancer | 5 | 4 (80.0) | 1 (20.0) | 1 (100) | 0 (0) | |||
| Other | 4 | 0 (0.0) | 3 (100) | 1 (33.3) | 2 (66.6) | 1 (25.0) | 2 (50.0) | 1 (25.0) |
| Total | 22 (40.0) | 33 (60.0) | 16 (33.3) | 32 (66.6) | 5 (9.4) | 28 (52.8) | 20 (37.7) | |
| VDR Protein Expression | CYP24A1 Protein Expression | ||||||
|---|---|---|---|---|---|---|---|
| High | Low | p | High | Low | p | ||
| n | No. of Patients (%) | No. of Patients (%) | |||||
| T-Stadium | 55 | 0.57 + | 0.32 + | ||||
| T1–2 | 13 (59.1) | 9 (40.9) | 12 (54.5) | 10 (45.5) | |||
| T3–4 | 23 (69.7) | 10 (30.3) | 20 (60.6) | 13 (39.4) | |||
| Grading | 53 | 0.07 + | 0.58 + | ||||
| G1 | 4 (80.0) | 1 (20.0) | 1 (20.0) | 4 (80.0) | |||
| G2 | 21 (75.0) | 7 (25.0) | 16 (57.1) | 12 (42.9) | |||
| G3 | 9 (45.0) | 11 (55.0) | 11 (55.0) | 9 (45.0) | |||
| N-Stadium | 48 | 0.63 + | 0.33 + | ||||
| N0 | 12 (70.6) | 4 (29.4) | 12 (70.6) | 4 (29.4) | |||
| N+ | 18 (58.1) | 13 (41.9) | 16 (50.0) | 16 (50.0) | |||
| Multiple metastasised | 60 | 0.03+ | 0.01+ | ||||
| Positive | 18 (56.3) | 14 (43.7) | 14 (43.8) | 18 (56.2) | |||
| Negative | 5 (82.1) | 23 (17.9) | 22 (78.6) | 9 (21.4) | |||
| Years | Years | ||||||
| Age at diagnosis | 66 | 0.79 * | 0.54 * | ||||
| Mean | 62.1 | 61.1 | 61.2 | 62.7 | |||
| Time to metastasis | 66 | 0.41 * | 0.68 * | ||||
| Mean | 3.7 | 2.8 | 3.6 | 3.2 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seiler, J.; Ebert, R.; Rudert, M.; Herrmann, M.; Leich, E.; Weißenberger, M.; Horas, K. Bone Metastases of Diverse Primary Origin Frequently Express the VDR (Vitamin D Receptor) and CYP24A1. J. Clin. Med. 2022, 11, 6537. https://doi.org/10.3390/jcm11216537
Seiler J, Ebert R, Rudert M, Herrmann M, Leich E, Weißenberger M, Horas K. Bone Metastases of Diverse Primary Origin Frequently Express the VDR (Vitamin D Receptor) and CYP24A1. Journal of Clinical Medicine. 2022; 11(21):6537. https://doi.org/10.3390/jcm11216537
Chicago/Turabian StyleSeiler, Jonas, Regina Ebert, Maximilian Rudert, Marietta Herrmann, Ellen Leich, Manuela Weißenberger, and Konstantin Horas. 2022. "Bone Metastases of Diverse Primary Origin Frequently Express the VDR (Vitamin D Receptor) and CYP24A1" Journal of Clinical Medicine 11, no. 21: 6537. https://doi.org/10.3390/jcm11216537
APA StyleSeiler, J., Ebert, R., Rudert, M., Herrmann, M., Leich, E., Weißenberger, M., & Horas, K. (2022). Bone Metastases of Diverse Primary Origin Frequently Express the VDR (Vitamin D Receptor) and CYP24A1. Journal of Clinical Medicine, 11(21), 6537. https://doi.org/10.3390/jcm11216537







